Abstract
We have integrated preventive oral health measures into preventive care visits for children at a federally qualified health center in Boston, Massachusetts. The program, started in 2015, covers 3400 children and has increased universal caries risk screening in primary care to 85%, fluoride varnish application rates to 80%, and referrals to a dental home to 35%. We accomplished this by minimizing pressures on providers’ workflow, empowering medical assistants to lead the initiative, and utilizing data-driven improvement strategies, alongside colocated coordinated care.
Our goals were to integrate caries prevention into all well-child visits and increase the number of children who established a dental home at our federally qualified health center (FQHC). We therefore designed and implemented an Oral Health in Pediatric Primary Care program.
INTERVENTION
The intervention had three components, each conducted during preventive care visits, annually or more frequently: (1) universal caries risk screening and oral health education, (2) fluoride varnish application for all eligible children, and (3) expedited referrals to a colocated dental clinic for all children who did not have a dental home.
PLACE AND TIME
The program was implemented at The Dimock Center, a FQHC in the Roxbury neighborhood of Boston, Massachusetts, and was first funded in 2015 for children aged 0 to 6 years via a learning collaborative. Additional funding allowed further expansion in 2016 to patients aged 0 to 18 years. The program continues to operate successfully.
PERSON
The Dimock Center’s pediatric clinic serves approximately 3400 patients aged 0 to 18 years. All patients are offered the interventions described at the well-child visit. Almost 73% have public insurances (Medicaid, Medicaid managed care organizations, Health Safety Net, State Children’s Health Insurance Program [S-CHIP]), 2.75% are uninsured, and 25% have private insurance, which may not include dental coverage. A 2015 market survey commissioned by the Dimock Center indicates that across all age groups, 91% of our patients have incomes below 200% of the federal poverty level (according to the US Department of Health and Human Services) and 96% identify as ethnic or racial minorities. The pediatric population closely resembles Dimock’s overall patient population.
PURPOSE
Caries is the most prevalent chronic childhood disease in the United States, with low-income children and children of color aged 2 to 17 years affected disproportionately.1 In Massachusetts, Black and Hispanic children in kindergarten have a 1.7 times higher prevalence of caries compared with non-Hispanic White children. This disparity persists in the third and sixth grades.2 Although federal guidelines mandate that S-CHIP and Medicaid cover pediatric dental treatment, children with public insurances have lower rates of dental care utilization than their privately insured peers.3 Children have multiple well-child visits in early childhood, providing primary care providers frequent opportunities to offer anticipatory guidance, caries risk screening, and preventive treatment.
However, published literature suggests that these opportunities are infrequently utilized. Reasons included limited time during medical visits, lack of cross-training for primary care providers around caries prevention, and low reimbursement rates for fluoride varnish applications in the medical setting.4,5 Improved referral mechanisms between primary care providers and dentists could increase the number of children with a dental home, but lack of interoperability of electronic health records (EHRs) and competing priorities during the well-child visit have hindered these efforts.1 Our program offers caries prevention within the primary care setting and streamlined referrals to a colocated dental home to reduce oral health disparities in the children we serve.
IMPLEMENTATION
Patients complete risk screens on paper at each well-child visit to determine their caries risk and dental home status (Figure 1). The screen, adapted from the American Academy of Pediatrics Oral Risk Assessment Tool, is in English and Spanish.6 It was piloted by the clinic’s medical assistants, with changes incorporated on the basis of their suggestions. The medical assistant rooms the patient, hands out the screen at the beginning of each visit, and provides standardized oral health education. Primary care providers review completed screens, reinforcing anticipatory guidance. At the conclusion of the visit, the medical assistant provides fluoride varnish treatment to all eligible children aged 9 months to 6 years as an opt-out process, based on standing orders.
FIGURE 1—
Percentage of Pediatric Patients (Aged 9 Months to 6 Years) Who Completed Oral Health Risk Screen During Preventive Care Visits in the Dimock Pediatric Clinic: Boston, MA, 2015–2017
Customized templates in the EHR prompt primary care providers to record screening results and patient’s dental home status within trackable fields. Our medical and dental clinics share a common EHR, eClinicalWorks (e-ClinicalWorks, Westborough, MA).
Patients who report that they have no dental home are offered appointments at Dimock’s colocated dental clinic. Appointments are ordered by the primary care provider via the EHR to enable tracking and scheduled by a designated referral coordinator within 2 weeks of the medical visit. This system was implemented following patient interviews conducted in 2016 to identify barriers to dental care. Besides lack of dental insurance, the most frequent barriers cited were long phone waiting times when calling for appointments and appointments offered several months out. Fast-tracked appointments were made possible through strategic coordination between Dimock’s pediatric and dental clinics. To date, 107 children were referred for dental services. Outreach calls were made to all of them, and 56 appointments were successfully made (52%). Of the 56 appointments, 20 initial dental visits have been completed (36%).
The quality improvement analyst posts periodic reports in the pediatric clinic and reviews them at monthly staff meetings. Consensus is obtained to conduct appropriate improvement cycles to improve outcomes.
EVALUATION
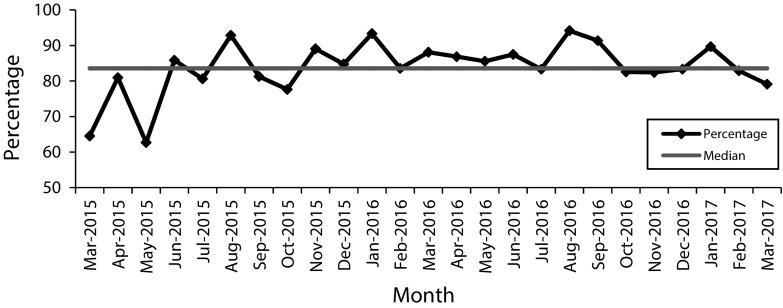
A total of 1840 out of 2163 eligible children have been screened since the start of the project. Since caries risk screenings were instituted in 2015, the monthly screening rate increased from 0 before starting the project to 60% in month 1 (40 children screened out of 62 eligible) and is now at approximately 85% (Figure 2). The proportion of all patients at high risk of caries according to screening results is 54% (994 at high risk out of 1840 screened). The proportion of patients with no dental home referred to the Dimock dental practice rose from 0% to 35% by month 6. The rate of fluoride varnish application for eligible children seen each month increased to more than 80% after 18 months and is currently at 79% (Figure 2).
FIGURE 2—
Percentage of Pediatric Patients (Aged 9 Months to 6 Years) Receiving Fluoride Varnish During Preventive Care Visits in the Dimock Pediatric Clinic: Boston, MA, 2015–2017
ADVERSE EFFECTS
Patients and staff report high program satisfaction. There is widespread acceptance of the EHR template changes and the utilization of medical assistants to lead this project. Risk screening, fluoride varnish application, and dental referral rates were very sensitive to continuous quality monitoring. All these rates dropped if the monthly reports and improvement cycles were delayed. Dental referral rates have increased more slowly than expected. This is likely related to parents’ assumption that dental screenings offered in schools and child care facilities are sufficient, and because we are unable to offer wide access to dental appointments for children younger than 2 years.
SUSTAINABILITY
Funding and technical support allowed us to develop operational efficiencies and infrastructure, ensuring sustainability of key activities. The medical assistants’ and quality improvement analyst’s roles are critical. Primary care providers participate enthusiastically, as program activities do not generate increased pressure on their workload. Strategic coordination and colocation of medical and dental services improved referrals. The main recurring cost incurred is quality improvement staff time. At Dimock, this position is incorporated into the operating budget with expenses distributed among several quality improvement projects, minimizing the cost impact on this program.
PUBLIC HEALTH SIGNIFICANCE
Poor oral health, while linked with racial and ethnic minority status, also correlates highly to disparities in dental care access. There is a nationwide shortage of dentists who accept Medicaid, possibly associated with poor reimbursement rates.7 In a 2012 survey, 1844 (42%) of Massachusetts dentists reported that they accepted Medicaid. Of these, almost half reported that Medicaid makes up less than less than 10% of their patient population. A 2016 market analysis conducted by Dimock confirmed the shortage of dentists accepting Medicaid in Dimock’s service area and the long wait times for dental care at FQHCs. We therefore anticipate that increasing the number of referrals for Medicaid-eligible children to dental homes will remain challenging. As a consequence, caries prevention in the medical setting assumes particular significance.
In conclusion, we have sustainably integrated preventive oral health measures into well-child visits by minimizing pressures on providers’ workflow, empowering medical assistants to lead the initiative, using data-driven improvement strategies, and leveraging the colocation of our medical and dental clinics. We continue to work to mitigate barriers to dental referrals.
ACKNOWLEDGMENTS
The authors would like to thank the Massachusetts League of Community Health Centers and the Harvard Medical School Center for Primary Care for funding, technical support, and leading the learning collaboratives that made it possible to implement this program.
They also would like to thank Marcel Flores for his contributions to the compilation of data.
HUMAN PARTICIPANT PROTECTION
This analysis, which was conducted to inform a public health program, used de-identified data and therefore was not classified as human participant research and was not subject to institutional review board review.
REFERENCES
- 1.Fisher-Owens SA, Isong IA, Soobader M-J et al. An examination of racial/ethnic disparities in children’s oral health in the United States. J Public Health Dent. 2013;73(2):166–174. doi: 10.1111/j.1752-7325.2012.00367.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.White BA, Monopoli MP, Souza BS. The oral health of Massachusetts’ children. Catalyst Institute. 2008. Available at: http://www.bu.edu/creedd/files/2009/05/Oral-Health-Of-Massachusetts-Children-2008.pdf. Accessed May 1, 2017.
- 3.Nasseh K, Vujicic M. Dental care utilization steady among working-age adults and children, up slightly among the elderly. American Dental Association Health Policy Institute. 2016. Available at: http://www.ada.org/∼/media/ADA/Science and Research/HPI/Files/HPIBrief_1016_1.pdf?la=en. Accessed May 1, 2017.
- 4.Isong IA, Silk H, Rao SR, Perrin JM, Savageau JA, Donelan K. Provision of fluoride varnish to Medicaid-enrolled children by physicians: the Massachusetts experience. Health Serv Res. 2011;46(6 pt 1):1843–1862. doi: 10.1111/j.1475-6773.2011.01289.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schroeder S. Fact sheet: Fluoride varnish application in primary care settings. Center for Rural Health, University North Dakota School of Medicine and Health Sciences. 2016. Available at: https://ruralhealth.und.edu/pdf/fluoride-varnish-application-primary-care.pdf. Accessed May 1, 2017.
- 6.American Academy of Pediatrics. Oral Health Risk Assessment Tool. Available at: http://www2.aap.org/oralhealth/docs/riskassessmenttool.pdf. Accessed July 25, 2017.
- 7.Nasseh K, Vujicic M, Yarbrough C. A ten-year, state-by-state, analysis of Medicaid fee-for-service reimbursement rates for dental care services. American Dental Association Health Policy Institute. 2014. Available at: http://www.aapd.org/assets/1/7/PolicyCenter-TenYearAnalysisOct2014.pdf. Accessed April 7, 2016.