The United States has produced nearly 40 years of prevention and disparities research initiatives and public health programs aimed at eliminating inequities and the unfair burden of illness in society. These efforts have yielded a vast body of information regarding the large gaps in specific health and health care hardships suffered by large segments of the US population, and interventions for remediation. It remains unclear how much progress has been made in eliminating health inequities. If we use life expectancy as a gauge, we would have to judge the effort as a highly deficient one. Thirty years ago, life expectancy in the United States was five years longer for the upper quintile of income than for the lowest quintile.1 Today, that difference is 12 years for men and 14 years for women. Worse yet, life spans have not improved for lower-income people, and marginal loss of longevity has occurred for women. This reality check points out the importance of recognizing the towering role of growing income differences in the United States, and begs the pertinent question: “How much can we improve population health without a commensurate effort in closing income gaps?”
NOT INCOME STATUS PER SE
The challenge of recognizing fundamental causes, such as income differentials as a primary cause of poor health outcomes for predisposing subpopulations, provokes different modes of inquiry and analysis compared with targeting specific disease conditions, one at a time, in research and interventions. Health risk is a societally imbedded issue, and progress toward health equity requires reducing economic inequality.2 Although public health is axiomatically “upstream” in its strategic approach to eliminating contributory risks to health, often its actions are rooted in “downstream” disease causal models. The result is negation of the ecological model according to which pathways to health or disease and functional decline are influenced by the environmental conditions fostered and reinforced by economic inequality. This disjunction ultimately undermines progress toward elimination of health inequities.3
It is not income status per se that predisposes to disease; rather, income inequality creates a propensity to disease pathways over the course of human development through environmental exposures and learned behavior in specific social contexts.4 Krieger warns of the fallacy of treating causes of disease-attributed risk as if they add up to 100%. A logical extension of this critique is that the production of health equity involves accounting for the direct effects of economic inequality on opportunity structures and interactive influences on other putative risk factors associated with adverse life-course circumstances.5 Doubtless it is possible to point to critically important areas of positive health gains made by public health interventions, such as HIV infection and tobacco-use reduction. Yet there is only weak evidence of any elimination of “unfair and unjust” differences in overall health, functional status, or mortality between major social demographic subgroups based on national indices.
THE HEALTH EQUITY DILEMMA
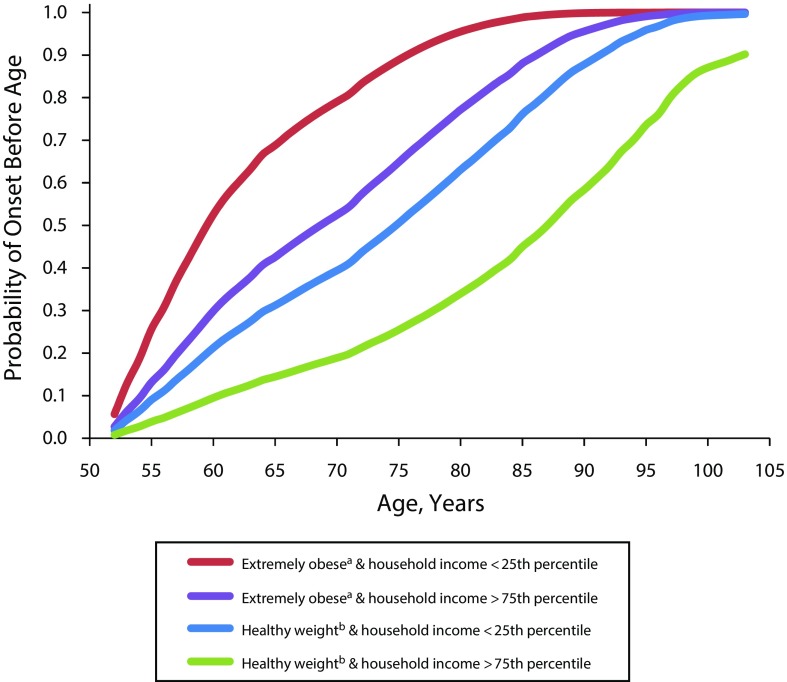
In Figure 1, we use the Health and Retirement Survey of the US population to illustrate the synergistic relationship between healthy functioning and income distribution for one major health and mortality threat, extreme obesity, among persons in the United States older than 50 years.6 Results are from Cox regressions (proportional hazards models) of the outcome “any limitations in activities of daily living” using an average of seven Health and Retirement Survey data points per respondent. We examine transitions as persons go from no deficits to any deficit. We exclude from the analysis persons with any deficit at their first survey. “Time” in the Cox models is age, and curves are “failure” curves from the Cox models—that is, the probability of “failure” (any deficit) occurring prior to the age shown. In the figure, we compare four subsamples—healthy and extremely obese for highest and lowest quartiles of income (P < .001)—for all differences, controlling for current smoking, gender, and living with a spouse or partner.
FIGURE 1—
Association of Body Mass Index With Age of First Onset of Functional Limitations, by Income Group: Health and Retirement Survey, United States, 2015
aExtremely obese defined as body mass index ≥ 40 kg/m2.
bHealthy weight defined as body mass index 18.5–25.0 kg/m2.
Low-income obese persons are progressing to dysfunction much more rapidly than high-income people. In their age of onset trajectory to deficits in activities of daily living, healthy-weight persons who are low income are similar to extremely obese higher-income persons rather than to healthy-weight higher-income persons. These findings suggest that total disease burden borne by people at the lower end of income distribution is greater irrespective of any specific medical condition. We conclude from this illustration that life-course risk for poor health and dysfunction is cumulative over the life span and is greatly exacerbated by growing income inequality, and that elimination of health disparities in the United States will not be accomplished relying solely on current public health or medical care approaches focused on individual diseases or dysfunctions and corresponding interventions.
LONG-RANGE PUBLIC POLICIES NEEDED
Population health outcomes can be improved without relying solely on changes in income distribution, as shown by the historic drop in cardiovascular mortality over the past two decades. However, these positive outcomes are limited because they are moderated by income resulting in greater health and mortality gains for the highest-income ranks. Policies designed to reduce income inequality and inordinate wealth differentials are required or, as a society, we will continue to expend significant resources and yet fall short of eliminating health disparities in the United States. We need more powerful solutions. The Robert Wood Johnson Foundation’s “Culture of Health” is a leading example of wide-angle thinking, but approaches to improve health for the lowest-income ranks necessitate wider coordination of public and private resources supported by long-range public policies aimed at establishing a balance between income and health equity.7
ACKNOWLEDGMENTS
Our thanks to Donald Lloyd for his assistance in reading and commenting on drafts of the manuscript.
REFERENCES
- 1.National Academies of Sciences, Engineering, and Medicine. The Growing Gap in Life Expectancy by Income: Implications for Federal Programs and Policy Responses. Washington, DC: National Academies Press; 2015. [PubMed] [Google Scholar]
- 2.Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A. 2015;112(49):15078–15083. doi: 10.1073/pnas.1518393112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bronfenbrenner U. Developmental ecology through space and time: a future perspective. In: Moen PO, Elder GHG Jr, editors; Lüscher K, editor. Examining Lives in Context: Perspectives on the Ecology of Human Development. Washington, DC: American Psychological Association; 1995. pp. 619–647. [Google Scholar]
- 4.Marmot M, Wilkinson RG. Psychosocial and material pathways in the relation between income and health: a response to Lynch et al. BMJ. 2001;322(7296):1233–1236. doi: 10.1136/bmj.322.7296.1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Krieger N. Health equity and the fallacy of treating causes of population health as if they sum to 100% Am J Public Health. 2017;107(4):541–549. doi: 10.2105/AJPH.2017.303655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Health and Retirement Study, public use data set. 2015. Available at: http://www.rand.org/labor/aging/dataprod/hrs-data.html. Accessed October 2, 2015.
- 7.Bor J, Cohen GH, Galea S. Population health in an era of rising income inequality: USA, 1980–2015. Lancet. 2017;389(10077):1475–1490. doi: 10.1016/S0140-6736(17)30571-8. [DOI] [PubMed] [Google Scholar]