Abstract
CONTEXT:
The care bundle approach is a set of evidence-based practices that when performed collectively and reliably have been shown to improve the patient outcome.
AIMS:
To evaluate the impact of the bundle care approach on reducing device-associated infections (DAIs).
SETTINGS AND DESIGN:
The study was conducted at a tertiary care hospital, South India. The study period was from January 2016 to September 2016 which was divided into three phases, each comprising 3 months.
SUBJECTS AND METHODS:
During the implementation phase, bundle care forms were implemented in all Intensive Care Units (ICUs) and the ICU staff were given a basic education on the importance of bundle care approach. The DAI rates (ventilator-associated pneumonia [VAP] rates, central line-associated bloodstream infection [CLABSI] rate, and catheter-associated urinary tract infection [CAUTI] rate) were calculated throughout the study period.
STATISTICAL ANALYSIS USED:
Statistical analysis was performed using SPSS 19 software.
RESULTS:
During preimplementation phase, the VAP rate, CLABSI rate, and CAUTI rate were 14.79, 4.98, and 4.86 per 1000 device days, respectively. Rates were reduced to 13.03, 3.98, and 3.39 per 1000 device days, respectively, during the implementation phase and further reduced into 11.91, 3.49, and 2.36 per 1000 device days during the postimplementation phase. The month-wise decreasing trend of DAI rates was significant for medical ICUs as compared to surgical and pediatric ICUs.
CONCLUSIONS:
The month-wise decreasing trend of VAP rate, CLABSI rate, and CAUTI rate was noted, which signifies that the use of care bundle approach has a great impact on reducing DAIs
Key words: Care bundle, catheter-associated urinary tract infection, central line-associated bloodstream infections, device-associated infections, ventilator-associated pneumonia
Introduction
The last decade has focused a spotlight on staggering numbers of hospital deaths due to medical errors and ways to reengineer our health-care system to improve quality, safety, and efficiency of health-care delivery.[1] A care bundle is a structural way of improving care and patient outcome. The care bundle involves grouping together key elements of care for procedures to provide a systematic method to improve and monitor the delivery of clinical care processes. In short, care bundles aim to ensure that all patients consistently receive the best care or treatment, all the time. This approach has been successfully applied to the management of device-associated infections (DAIs) in the critical care setting. It is a 3–5 set of evidence-based practices that when performed collectively and reliably have been shown to improve the patient outcome.[2]
DAI is a major global health problem, causing increased morbidity and mortality. Central line-associated bloodstream infections (CLABSIs), ventilator-associated pneumonia (VAP), and catheter-associated urinary tract infection (CAUTI) are the major DAIs.[3] From healthcare-associated infections (HAIs) surveillance data, it was observed that DAI rates are quite high in our setting compared to Centers for Disease Control and Prevention (CDCs) National Healthcare Safety Network (NHSN) data, 2012.[4] The aim of our study was to evaluate the impact of the bundle care approach on reducing DAIs.
Subjects and Methods
This study was conducted by the Hospital Infection Control Committee (HICC) of Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), a large tertiary care hospital in South India having 18 Intensive Care Units (ICUs) with nearly 300 beds. The study period was 9 months (January 2016–September 2016) which was divided into three phases, each comprising 3 months – preimplementation phase, implementation phase, and postimplementation phase.
During the preimplementation phase (January 2016–March 2016), the baseline DAI rates (i.e., CLABSI, CAUTI, and VAP rates) for all the 18 ICUs of the hospital were calculated as per the standard HAI surveillance guideline laid down by CDC's NHSN, 2016 followed under routine HAI surveillance protocol of the institute.[5,6]
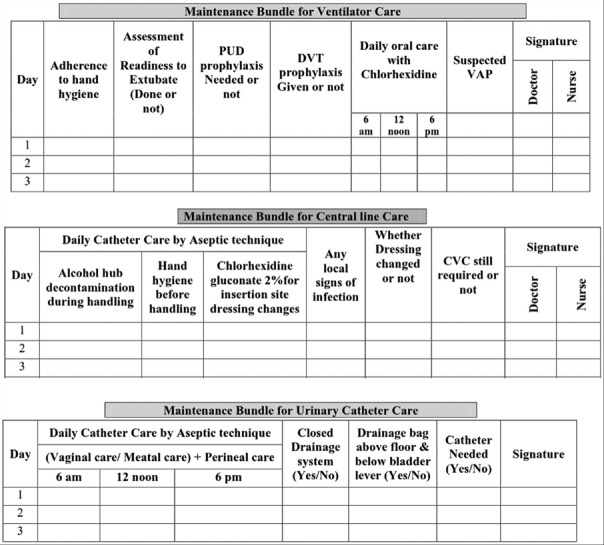
During the implementation phase (April 2016–June 2016), bundle care forms for three major DAIs, namely, CLABSI, CAUTI, and VAP, were made as per the standard guidelines of CDC and other references and also after considering opinions from ICU liaisons.[7,8,9] The components of the maintenance bundles are depicted in Figure 1. Then, the forms were distributed, and the concerned doctors and nurses of the ICUs were educated (both by mass lectures and bedside training) about the importance of adherence to the bundle care approach. The DAI rates of all the ICUs were determined under routine HAI surveillance of the institute.
Figure 1.
Bundle care forms for ventilator, central line, and urinary catheter. *PUD = Peptic ulcer disease, DVT = Deep vein thrombosis
During the postimplementation phase (July 2016–September 2016), the bundle care forms were continued to be used by the ICUs. The HAI surveillance was carried out to determine the DAI rates.
Statistical analysis was performed using SPSS 19 software (IBM Corporation, New York, United States). The HAI data of all the ICUs were analyzed as under three categories, namely, all medical, surgical, and pediatric ICUs.
Medical ICUs – Medicine, cardiac, medical oncology, step-down medical (adult), neuromedicine, and burns
Surgical ICUs – Surgery, plastic surgery, surgical oncology, cardiothoracic, trauma care, neurosurgery, critical care unit (adult), surgical gastroenterology, and urology
Pediatric ICUs – Pediatric medical, neonatal, and pediatric surgery.
Results
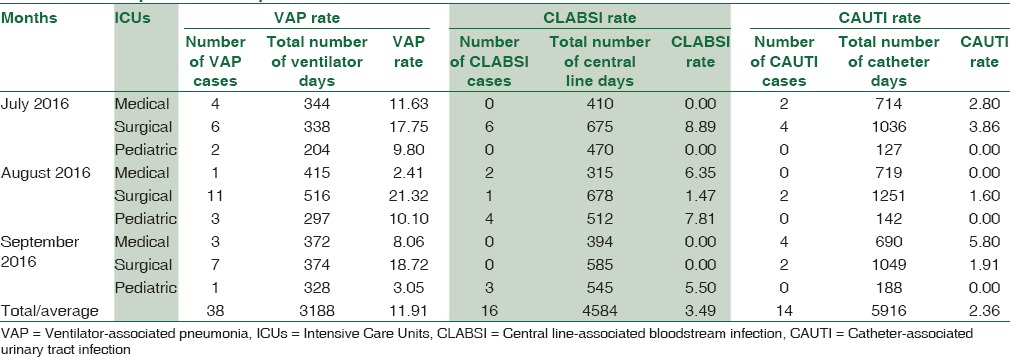
In the present study, an attempt was made to analyze the impact of care bundle approach on DAI rates. During preimplementation phase, the VAP rate, CLABSI rate, and CAUTI rate for all the ICUs taken together were 14.79/1000 ventilator days, 4.98/1000 central line days, and 4.86/1000 urinary catheter days, respectively [Table 1]. Rates were reduced to 13.03, 3.98, and 3.39 per 1000 device days, respectively, during implementation phase [Table 2]. However, during the postimplementation phase [Table 3], the rates were further reduced into 11.91, 3.49, and 2.36 per 1000 device days, respectively.
Table 1.
Preimplementation phase
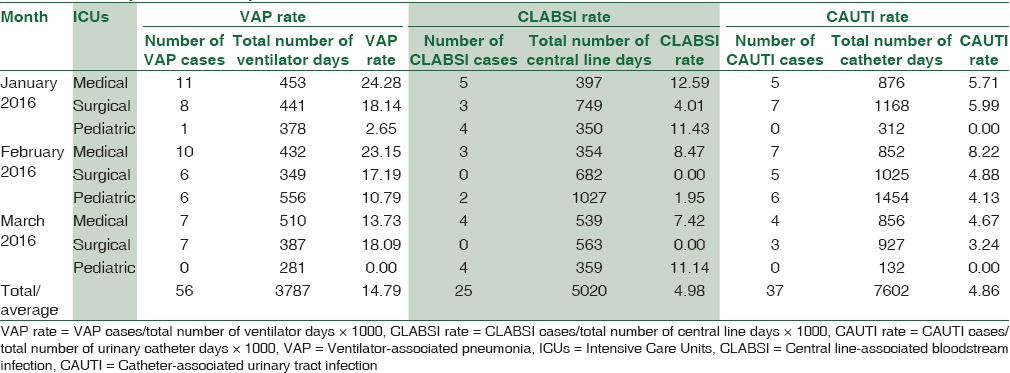
Table 2.
Implementation phase
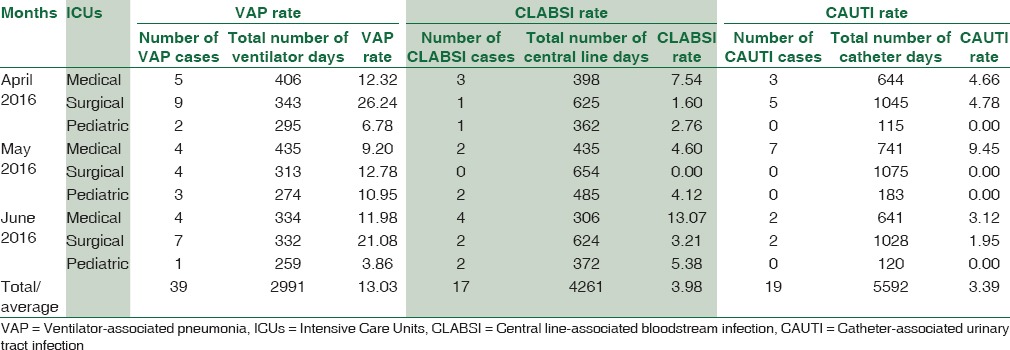
Table 3.
Postimplementation phase
There was a month-wise decreasing trend of VAP rate, CLABSI rate, and CAUTI rate during the study period. This signifies that the use of care bundle approach has a great impact on reducing DAIs [Figure 2]. Comparison of DAI rates between all medical, surgical, and pediatric ICUs showed that the declining trend was more pronounced in medical ICUs as compared to surgical and pediatric ICUs [Figures 3–5]. Effect of bundle care intervention on VAP (P < 0.001) and CAUTI (P = 0.001) was statistically significant whereas effect of implementation program of CLABSI, though was useful, was not statistically significant (P = 0.055) due to short period.
Figure 2.
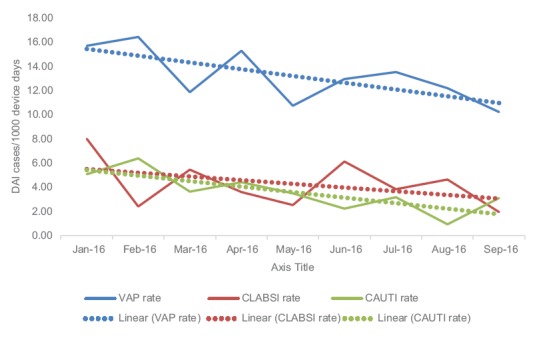
Month-wise trend of device-associated infection rates of all the Intensive Care Units taken together
Figure 3.
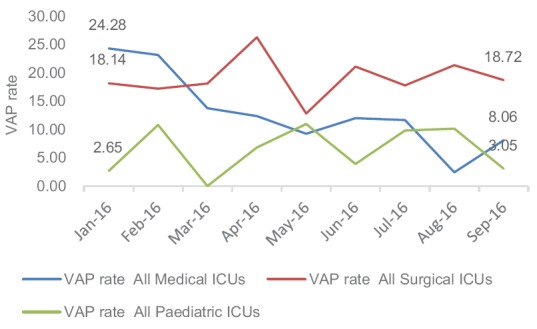
Month-wise trend of ventilator-associated pneumonia rate among all medical, surgical, pediatric Intensive Care Units
Figure 5.
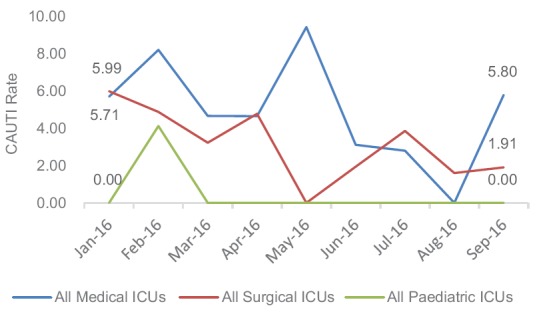
Month-wise trend of catheter-associated urinary tract infection rate among all medical, surgical, pediatric Intensive Care Units
Figure 4.
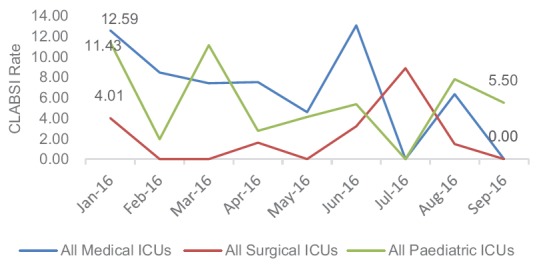
Month-wise trend of central line-associated bloodstream infection rate among all medical, surgical, pediatric Intensive Care Units
Discussion
Although the idea of a care bundle was originated by clinicians many years ago, the importance of compliance with each of the individual elements has been recognized relatively recently.[2] The bundles should act as a cohesive unit to ensure that all steps of care are reliably delivered and adequately documented. Failure of adherence to any one component makes the bundle compliance zero. This approach prevents avoidable patient morbidity and results in reduced length of hospital stay and improved patient outcome.[2] DAIs are major but preventable threat to patient safety and are strongly associated with the use of invasive devices which cause a mucosal breach or surface colonization, thus increasing evidence of HAIs. We evaluated the impact of implementation of the bundle care approach on the reduction of DAI rates.
There was a statistically significant steady decline of VAP rate by 19.0% from preimplementation to postimplementation phase (from 14.7 to 11.9 per 1000 ventilator days). Many studies documented similar decrease in VAP rate, following bundle implementation. Morris et al. showed a decrease of VAP rate from 32.0 to 12.0 cases per 1000 ventilator days following implementation of bundle.[10] The reduction was greater among patients requiring >6 days in ICU.[10] A multicentric survey conducted by Pogorzelska et al. demonstrated that among the ICUs with written policy on VAP bundle, only those who continuously monitored the compliance and achieved higher compliance were associated with a reduction in VAP.[7] They also observed that individual components of the bundle did not appear to be effective and the presence of a full-time hospital epidemiologist was associated with lower VAP rates.[7] Resar et al. reported 44.5% reduction of VAP rate in a data collected on ventilator bundle adherence and VAP rates.[11]
The CLABSI rate was brought down by 29.9% (4.98–3.49 per 1000 central line days) after implementation of bundles. Although the decrease was not statistically significant, it was clinically significant. Many studies revealed concurrent finding of decreasing CLABSI rate following bundle implementation (9.3–5.1 per 1000 central line days by Menegueti et al., 9.4–5.5 per 1000 central line days by Warren et al., and 3.9–0 per 1000 central line days by Longmate et al. at the USA).[12,13,14] A study conducted by Yilmaz et al. reported that the CLABSI rate decreased in the first 3 months after the postimplementation of bundle but up surged thereafter, emphasizing on the fact that a continuous regular educational program is needed to achieve a sustained impact of bundle.[15] Furuya et al. in 2011 reported that, according to the study done in 250 hospitals only when an ICU had a policy, monitored compliance, and had 95% compliance, CLABSI rates decreased.[16]
CAUTI is widely recognized as the most common HAI in the world, accounting for 40% of all HAIs.[17] We observed a statistically significant drop in the CAUTI rate by 51.4% (from 4.86 in preimplementation to 2.36 per 1000 catheter days in postimplementation phase). A quasi-experimental study by Blanck et al. reported a concordance finding of decrease in the CAUTI rate by 50% (8.4–4.3 per 1000 catheter days).[18] Davis et al. also reported a similar decline of 50% reduction in the mean monthly CAUTI rate in Philadelphia.[19] They further emphasized the importance of monitoring the bundle compliance in achieving a greater reduction of CAUTI. Karen Clarke et al. in 2013 reported that the CAUTI infection rate for the preintervention period was 5.2/1000. For the 7 months following the implementation of the interventions, the infection rate was 1.5/1000 catheter days, a significant reduction relative to the preintervention period (P = 0.03).[20]
In the present study, medical ICUs have shown to have a greater decrease in the DAI rates compared to surgical ICUs and pediatric ICUs. This was in discordance with the study conducted by Narang, which showed a reduction of VAP by 24.2% in the surgical patients compared to 12% reduction in the medical group following bundle implementation.[21] The route cause analysis was carried out and found that the compliance to bundle components was lower in surgical ICUs in postimplementation phase, which could be the reason for their lower decrease in DAI rates. In the pediatric ICUs, on the other hand, the infection control measures were much better than other ICUs even before implementation of bundles, and therefore, a reduction DAI was not noticed in postimplementation phase.
Limitation of the study
Certainly, care bundle is a powerful driver for improving the reliability of delivery of evidence-based care and patient outcome. Process indicators for bundle implementation such as assessment of knowledge of the health-care workers on the use of bundle and monitoring the compliance to individual components of bundle have a great impact to increase the bundle compliance and thereby reducing the DAI rates. However, we did not test the process indicators as the study period was less. Such studies in the future are warranted. The implementation of the insertion bundle was a difficult challenge in our study due to the reason that insertion of devices takes place in different locations (emergency, operation rooms, or sometimes in ICUs) in our institute. As a result, we could not implement the insertion bundle. A holistic approach to implement and to monitor the compliance to insertion bundle in addition to the maintenance bundle by taking the help of administrators would further improve the outcome indicator (i.e., the DAI rate).
Conclusions
Our result emphasizes the importance of implementation of the bundle care approach on reducing the occurrence of DAIs. Regular continuing education of the stakeholders and evaluation of bundle compliance by regular audits are the key elements to achieve a greater reduction of DAIs.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to acknowledge Dr. J. Balachander, Medical Superintendent of JIPMER, Dr. S. Sujatha, Head of Department of Microbiology and Member Secretary of HICC, JIPMER, for their constant support. We also like to give our gratitude to all the residents of Department of Microbiology, JIPMER, and most importantly, the infection control nurses of JIPMER (Ms. Rani Thamizharasan, Ms. Ruth Lilly, Ms. Djiva Azhwar, Mr. G. Thirumavarasu, Ms. Rajalakshmi Garnett, Ms. J. Radjalatchoumy, Ms. Lathika Gladson, Ms. V. Vijitha, Mr. Mohammad Aslam, Ms. Mehertaz Begum) for their immense help during data collection and Ms. Ilaveni for her contribution to data entry and analysis.
References
- 1.Zilberberg MD, Shorr AF, Kollef MH. Implementing quality improvements in the Intensive Care Unit: Ventilator bundle as an example. Crit Care Med. 2009;37:305–9. doi: 10.1097/CCM.0b013e3181926623. [DOI] [PubMed] [Google Scholar]
- 2.Cooke FJ, Holmes AH. The missing care bundle: Antibiotic prescribing in hospitals. Int J Antimicrob Agents. 2007;30:25–9. doi: 10.1016/j.ijantimicag.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 3.Salomao R, Rosenthal VD, Grimberg G, Nouer S, Blecher S, Buchner-Ferreira S, et al. Device-associated infection rates in Intensive Care Units of Brazilian hospitals: Findings of the international nosocomial infection control consortium. Rev Panam Salud Publica. 2008;24:195–202. doi: 10.1590/s1020-49892008000900006. [DOI] [PubMed] [Google Scholar]
- 4.Dudeck MA, Weiner LM, Allen-Bridson K, Malpiedi PJ, Peterson KD, Pollock DA, et al. National Healthcare Safety Network (NHSN) report, data summary for 2012, device-associated module. Am J Infect Control. 2013;41:1148–66. doi: 10.1016/j.ajic.2013.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weinstein RA, Darouiche RO. Device-associated infections: A macroproblem that starts with microadherence. Clin Infect Dis. 2001;33:1567–72. doi: 10.1086/323130. [DOI] [PubMed] [Google Scholar]
- 6. [Last accessed on 2016 Dec 02]. Available from: http://www.cdc.gov/nhsn/pdfs/pscmanual/2psc_identifyinghais_nhsncurrent.pdf .
- 7.Pogorzelska M, Stone PW, Furuya EY, Perencevich EN, Larson EL, Goldmann D, et al. Impact of the ventilator bundle on ventilator-associated pneumonia in Intensive Care Unit. Int J Qual Health Care. 2011;23:538–44. doi: 10.1093/intqhc/mzr049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. [Last cited on 2016 Dec 01]. Available from: https://www.cdc.gov/hai/pdfs/bsi/checklist-for-clabsi.pdf .
- 9.Catheter-associated Urinary Tract Infections (CAUTI) | HAI | CDC. [Last cited on 2016 Dec 01]. Available from: http://www.cdc.gov/hai/ca_uti/uti.html .
- 10.Morris AC, Hay AW, Swann DG, Everingham K, McCulloch C, McNulty J, et al. Reducing ventilator-associated pneumonia in intensive care: Impact of implementing a care bundle. Crit Care Med. 2011;39:2218–24. doi: 10.1097/CCM.0b013e3182227d52. [DOI] [PubMed] [Google Scholar]
- 11.Resar R, Pronovost P, Haraden C, Simmonds T, Rainey T, Nolan T. Using a bundle approach to improve ventilator care processes and reduce ventilator-associated pneumonia. Jt Comm J Qual Patient Saf. 2005;31:243–8. doi: 10.1016/s1553-7250(05)31031-2. [DOI] [PubMed] [Google Scholar]
- 12.Warren DK, Zack JE, Mayfield JL, Chen A, Prentice D, Fraser VJ, et al. The effect of an education program on the incidence of central venous catheter-associated bloodstream infection in a medical ICU. Chest. 2004;126:1612–8. doi: 10.1378/chest.126.5.1612. [DOI] [PubMed] [Google Scholar]
- 13.Longmate AG, Ellis KS, Boyle L, Maher S, Cairns CJ, Lloyd SM, et al. Elimination of central-venous-catheter-related bloodstream infections from the Intensive Care Unit. BMJ Qual Saf. 2011;20:174–80. doi: 10.1136/bmjqs.2009.037200. [DOI] [PubMed] [Google Scholar]
- 14.Menegueti MG, Ardison KM, Bellissimo-Rodrigues F, Gaspar GG, Martins-Filho OA, Puga ML, et al. The impact of implementation of bundle to reduce catheter-related bloodstream infection rates. J Clin Med Res. 2015;7:857–61. doi: 10.14740/jocmr2314w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yilmaz G, Caylan R, Aydin K, Topbas M, Koksal I. Effect of education on the rate of and the understanding of risk factors for intravascular catheter-related infections. Infect Control Hosp Epidemiol. 2007;28:689–94. doi: 10.1086/517976. [DOI] [PubMed] [Google Scholar]
- 16.Furuya EY, Dick A, Perencevich EN, Pogorzelska M, Goldmann D, Stone PW. Central line bundle implementation in US Intensive Care Units and impact on bloodstream infections. PLoS One. 2011;6:e15452. doi: 10.1371/journal.pone.0015452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hanchett M, Rn M. Preventing CAUTI: A patient-centered approach. Prevention. 2012;43:42–50. [Google Scholar]
- 18.Blanck AM, Donahue M, Brentlinger L, Dixon Stinger K, Polito C. A quasi-experimental study to test a prevention bundle for catheter-associated urinary tract infections. [Last cited on 2016 Nov 19];J Hosp Adm. 2014 3:101–8. Available from: http://www.sciedu.ca/journal/index.php/jha/article/view/4232 . [Google Scholar]
- 19.Davis KF, Colebaugh AM, Eithun BL, Klieger SB, Meredith DJ, Plachter N, et al. Reducing catheter-associated urinary tract infections: A quality-improvement initiative. Pediatrics. 2014;134:e857–64. doi: 10.1542/peds.2013-3470. [DOI] [PubMed] [Google Scholar]
- 20.Clarke K, Tong D, Pan Y, Easley KA, Norrick B, Ko C, et al. Reduction in catheter-associated urinary tract infections by bundling interventions. Int J Qual Health Care. 2013;25:43–9. doi: 10.1093/intqhc/mzs077. [DOI] [PubMed] [Google Scholar]
- 21.Narang S. Use of ventilator bundle to prevent ventilator associated pneumonia. Oman Med J. 2008;23:96–9. [PMC free article] [PubMed] [Google Scholar]