Abstract
An elderly diabetic farmer presented with chronic nonhealing ulcer over the left foot, multiple liver abscesses, and right-sided pleural effusion. The patient developed septicemia and multiorgan failure. The pus grew pigment producing Chromobacterium violaceum. He was treated successfully with ciprofloxacin for a total duration of 15 days. This case is reported for its rare clinical presentation and resemblance with melioidosis. Of the 200 C. violaceum cases reported across the globe, this is the 14th case from India and the oldest in the literature.
Key words: Chromobacterium violaceum, foot ulcer, liver abscess, sepsis
Introduction
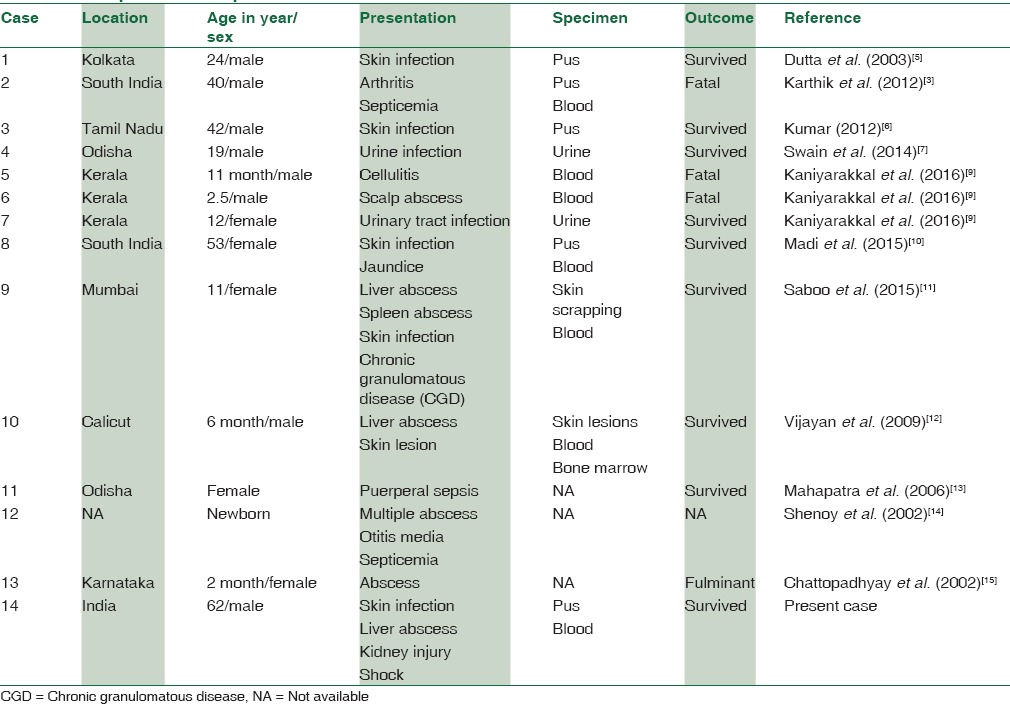
Chromobacterium violaceum is a Gram-negative bacillus producing violacein pigment.[1] Nonpigment-producing pathogenic species do exist but are rare and difficult to identify. Taxonomically, it is included in class-Betaproteobacteria, order-Neisseriales, family-Neisseriaceae, Genus-Chromobacterium, species-violaceum. Provide some more taxonomic and bacteriological details. The first human pathogenicity was found way back in 1925 in Malaysia. Since then about 200 cases have been described from around the globe (Vietnam, Taiwan. Japan, United States, Brazil, Argentine, Australia, Senegal, India, Korea, Srilanka, and Nepal). The most common established route of entry is through broken skin coming in contact with contaminated soil and water. Till now, the various clinical presentations that have been reported are skin and subcutaneous infections, liver abscess, parotid and ear discharge, urinary and gastrointestinal infections, septic arthritis, meningitis, and sepsis.[2] Pediatric and young adults seem to be the most vulnerable age group. The mortality rate has been up to 57% in the United States and about 80% in India.[2,3] There are only 7 cases aged more than 20 years, documented in global literature [Table 1]. A total 13 number of cases are documented from India before this case, most of which are southern part of India [Table 2]. We present oldest ever reported case of C. violaceum- induced subcutaneous ulcer, liver abscess, pleural effusion, and sepsis with a brief review of literature.
Table 1.
Details of reported cases of Chromobacterium violaceum cases in adults and their outcome
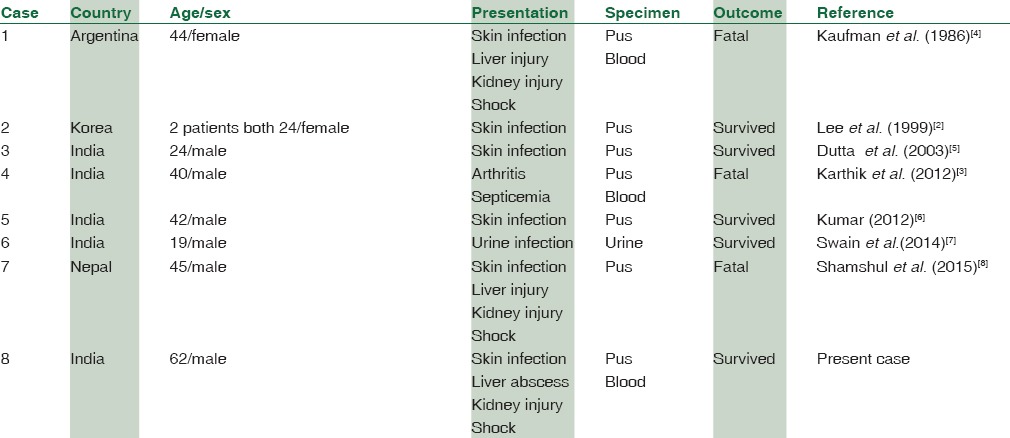
Table 2.
Comparison of reported cases of Chromobacterium violaceum cases from India
Case Report
A 62-year-male farmer from, Balasore district of Odisha, presented with a nonhealing ulcer on dorsum of the left foot for 2 months, pain in the right upper abdomen for 5 days and incoherent talk for 6 h. He was a diabetic for 6 years. Physical examination revealed; temperature 100°F, pulse – 110/min, blood pressure – 80/50 mmHg, and respiratory rate – 20/min. The ulcer was 5 cm × 7 cm in size, nontender, with a necrotic base [Figure 1]. There was tender hepatomegaly and reduced vesicular breath sound in the right mammary area. Point-of-care blood sugar was 280 mg/dl, hemoglobin A1c – 9.8%, and urine ketones were negative. Bedside sonography revealed hepatic size of 22 cm with 3 focal ill-defined hypoechoic lesion in the right lobe of liver with anechoic center, largest being 3.4 cm × 3.6 cm suggesting bacterial abscess with minimal pleural effusion on the right side [Figure 2]. The pus sample was inoculated on nutrient agar, blood agar, and MacConkey agar. Either Staphylococcal bacteremia or melioidosis is was suspected, and the patient was shifted to Intensive Care Unit.
Figure 1.

Ulcer (5 cm × 7 cm) over dorsum of the foot with necrotic base and surrounding edema
Figure 2.
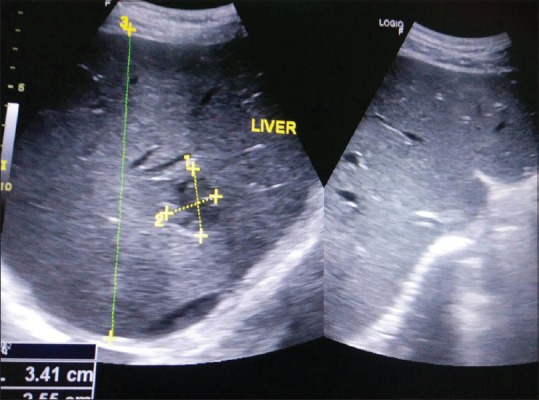
Ultrasonography of liver showing focal ill-defined hypoechoic lesion with anechoic center in the right lobe of liver
He was treated with bolus intravenous fluids, (IV) insulin at 10 units/h, ceftriaxone 1 g IV 12 hourly, and vancomycin 1 g 8 hourly. At 2 h, noradrenalin was started at 0.5 mcg/kg/min, and insulin rate was decreased to half. At 6 h, noradrenalin was titrated up to 2 mcg/kg/min. At 10 h, noradrenalin was further up-titrated to 3 mcg/kg/min, and the following laboratory results were obtained. Hemoglobin – 92 g/L, total leukocyte count – 10.2 × 109/L (polymorphs – 80%), total bilirubin – 4.5 mg/dL, direct bilirubin – 1.8 mg/dL, antibiotic susceptibility testing (AST) – 70 U/L, alanine aminotransferase – 96 U/L, alkaline phosphatase – 46 U/L, albumin – 2.2 g/dL), blood urea nitrogen – 56 mmol/L, creatinine – 3.8 μmol/L, sodium – 142 mEq/L, potassium – 4.6 mEq/L). The patient was clinically better on day 2 and allowed clear oral fluids while continuing the same dose of inotropes and antibiotics (with renal modification of dose).
On day 3, kidney function deteriorated (blood urea nitrogen-140 mmol/L, creatinine-5.8 μmol/L, sodium-136 mEq/L, and potassium-mEq/L) and hemodialysis was started. The microbiological report was obtained on the same day. A pure growth of violet-colored colonies with 2–3 mm diameter was seen on the nutrient agar [Figure 3]. Similar beta hemolytic colonies were seen on blood agar. In MacConkey agar, nonlactose fermenting colonies were isolated. The organism was Gram-negative bacillus, motile, catalase, and oxidase positive which fermented glucose with acid. It was negative for indole, methyl red, VogesPrausker, and mannitol was not fermented. It utilized citrate and produced nitrate. On triple sugar iron agar, alkaline slant with acidic butt (K/A) without gas and with H2S production was seen. Only arginine was decarboxylated. On incubating the plates anaerobically, there was no pigment production, and violet-colored colonies reappeared on aerobic incubation at 37°C for 6–8 h. With these phenotypic characteristics, the isolate was identified as C. violaceum.
Figure 3.

Pigmented colonies of Chromobacterium violaceum on Nutrient agar and antimicrobial susceptibility testing
AST was done by standard Kirby–Bauer disc diffusion method. Antibiotic sensitivity test (AST) interpretations were done based on Clinical and Laboratory Standards Institute document M45 – Methods for antimicrobial dilution and disk susceptibility testing of infrequently isolated or fastidious Bacteria. The organism was found to be sensitive to ciprofloxacin, gentamicin, amikacin, tetracycline, gatifloxacin, netilmicin, ceftazidime, cefepime, piperacillin-tazobactam, and imipenem. It showed resistance to ampicillin, amoxicillin-clavulanate, and cefotaxime [Figure 3]. We switched over to IV ciprofloxacin with adequate insulin to maintain the capillary sugar of 120 mg/dL.
On 4th day, the mean arterial pressure gradually improved, and noradrenalin was down titrated. On day 5, organism isolated from blood culture demonstrated similar phenotypic characteristics and susceptibility pattern. On the same day, the patient was shifted to high dependency unit. On 7th day, the patient was shifted to general ward, and oral ciprofloxacin was continued. The patient was discharged on 12th day with an advice to continue ciprofloxacin for a total duration of 15 days. The patient was seen 15 days after discharge and was doing fine. The patient was last seen 7 months after the incidence without any complications.
Discussion
Nearly 200 cases of C. violaceum have been described around the globe (Vietnam, Taiwan. Japan, United States, Brazil, Argentine, Australia, Senegal, India, Korea, Srilanka, and Nepal).[16] Atleast 13 cases have been reported earlier from India [Table 2]. Pediatric population and young children are the most vulnerable group.[3,17] In a case series from the United States, 11 out of 12 patients had a mean age of 15 years.[17] There have been only 7 cases in the global literature beyond the age of 20. Lee et al. have reported 2 girls of 24 years with infection of the skin and soft tissue after an airplane accident who survived almost a fatal course.[2] Kaufman et al. from Argentina and Shamshul et al. from Nepal have reported cases in their 40s and both the cases were fatal.[4,8] Our case is the eldest ever (62 years) reported case to the best of our knowledge. Similar to our cases, skin infection and multiorgan dysfunction in adults have been described by Kaufman et al. from Argentina and Shamshul et al. from Nepal.[4,8] Probably, this is the first-ever case of additional finding of liver abscess along with the skin and subcutaneous infection which prompted us to think of melioidosis which is not uncommon in coastal belt of India.[18] Our patient who had uncontrolled diabetes may be considered as immunocompromised akin to the earlier report of Karthik et al. in a patient of systemic lupus erythematosus and in the case series by Macher et al.[3,17] Various antibiotic regimens have been used by various authors, however, ciprofloxacin, co-trimoxazole, gentamicin, and carbapenems have been sensitive in all cases, and ampicillin/amoxicillin have been resistant in almost all cases.[2,3,4,5,9]
Conclusion
C. violaceum infections in humans are rare. Increasing case reports from South East Asian region suggest that it is an emerging pathogen. Although the initial case reports were predominantly from pediatric age group, present case shows that no age has a bar.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Davis ES. Chromobacterium. In: Braude AI, Davis CE, Fierer J, editors. Infectious diseases and medical microbiology. 2nd ed. Philadelphia: WB Saunders; 1986. pp. 358–61. [Google Scholar]
- 2.Lee J, Kim JS, Nahm CH, Choi JW, Kim J, Pai SH, et al. Two cases of Chromobacterium violaceum infection after injury in a subtropical region. J Clin Microbiol. 1999;37:2068–70. doi: 10.1128/jcm.37.6.2068-2070.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Karthik R, Pancharatnam P, Balaji V. Fatal Chromobacterium violaceum septicemia in a South Indian adult. Infect Dev Ctries. 2012;6:751–5. doi: 10.3855/jidc.1866. [DOI] [PubMed] [Google Scholar]
- 4.Kaufman SC, Ceraso D, Schugurensky A. First case report from Argentina of fatal septicemia caused by Chromobacterium violaceum. J of Clin Microbiol. 1986;23:956–8. doi: 10.1128/jcm.23.5.956-958.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dutta S, Dutta SK. Multidrug resistant Chromobacterium violaceum: An unusual bacterium causing long standing wound abscess. Indian J Med Microbiol. 2003;21:217–8. [PubMed] [Google Scholar]
- 6.Kumar MR. Chromobacterium violaceum: A rare bacterium isolated from a wound over the scalp. Int J Appl Basic Med Res. 2012;2:70–2. doi: 10.4103/2229-516X.96814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Swain B, Otta S, Sahu KK, Panda K, Rout S. Urinary tract infection by Chromobacterium violaceum. J Clin Diagn Res. 2014;8:DD01–2. doi: 10.7860/JCDR/2014/9230.4703. doi: 10.7860/jcdr/2014/9230.4703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shamshul Ansari, Pramod Paudel, Kishor Gautam, Sony Shrestha, Sangita Thapa, Rajendra Gautam. Chromobacteriumviolaceum Isolated from a Wound Sepsis: A Case Study from Nepal. Case Rep Infect Dis. 2015;2015:181946. doi: 10.1155/2015/181946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kaniyarakkal V, Orvankundil S, Lalitha SK, Thazhethekandi R, Thottathil J. Chromobacterium violaceum Septicaemia and Urinary Tract Infection: Case Reports from a Tertiary Care Hospital in South India. Case Rep Infect Dis. 2016;22:2016. doi: 10.1155/2016/6795743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Madi DR, Vidyalakshmi K, Ramapuram J, Shetty AK. Successful treatment of Chromobacterium violaceum sepsis in a South Indian adult. Am J Trop Med Hyg. 2015;93:1066–7. doi: 10.4269/ajtmh.15-0226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Saboo AR, Vijaykumar R, Save SU, Bavdekar SB. A rare nonfatal presentation of disseminated Chromobacterium violaceum sepsis. J Microbiol Immunol Infec. 2015;48:574–7. doi: 10.1016/j.jmii.2012.11.002. [DOI] [PubMed] [Google Scholar]
- 12.Vijayan AP, Anand MR, Remesh P. Chromobacterium violaceum sepsis in an infant. Indian Pediatr. 2009;46:721–2. [PubMed] [Google Scholar]
- 13.Mahapatra A, Roy D, Poddar N, Panda R, Sarangi G, Mallick B, et al. Chromobacterium violaceum: A case report of an unusual bacterium causing puerperal sepsis. Indian J Pathol Microbiol. 2006;49:450–2. [PubMed] [Google Scholar]
- 14.Shenoy S, Baliga S, Wilson G, Kamath N. Chromobacterium violaceum septicemia. Indian J Pediatr. 2002;69:363–4. doi: 10.1007/BF02723225. [DOI] [PubMed] [Google Scholar]
- 15.Chattopadhyay A, Kumar V, Bhat N, Rao PL. Chromobacterium violaceum infection: A rare but frequently fatal disease. J Pediatr Surg. 2002;37:108–10. doi: 10.1053/jpsu.2002.29439. [DOI] [PubMed] [Google Scholar]
- 16.Ray P, Sharma J, Marak RS, Singhi S, Taneja N, Garg RK, et al. Chromobacterium violaceum septicaemia from north India. Indian J Med Res. 2004;120:523–6. [PubMed] [Google Scholar]
- 17.Macher AM, Casale TB, Fauci AS. Chronic granulomatous disease of childhood and Chromobacterium violaceum infections in South eastern United States. Ann Intern Med. 1982;97:51–5. doi: 10.7326/0003-4819-97-1-51. [DOI] [PubMed] [Google Scholar]
- 18.Karuna T, Khadanga S, Dugar D. Melioidosis: Indian perspective. Int J Med Res Rev. 2014;2:243–248. [Google Scholar]


