Abstract
The utilisation of robotic-assisted techniques is a novelty in the field of general surgery. Our intention was to examine the up to date available literature on the cost assessment of robotic surgery of diverse operations in general surgery. PubMed and Scopus databases were searched in a systematic way to retrieve the included studies in our review. Thirty-one studies were retrieved, referring on a vast range of surgical operations. The mean cost for robotic, open and laparoscopic ranged from 2539 to 57,002, 7888 to 16,851 and 1799 to 50,408 Euros, respectively. The mean operative charges ranged from 273.74 to 13,670 Euros. More specifically, for the robotic and laparoscopic gastric fundoplication, the cost ranged from 1534 to 2257 and 657 to 763 Euros, respectively. For the robotic and laparoscopic colectomy, it ranged from 3739 to 17,080 and 3109 to 33,865 Euros, respectively. For the robotic and laparoscopic cholecystectomy, ranged from 1163.75 to 1291 and from 273.74 to 1223 Euros, respectively. The mean non-operative costs ranged from 900 to 48,796 from 8347 to 8800 and from 870 to 42,055 Euros, for robotic, open and laparoscopic technique, respectively. Conversions to laparotomy were present in 34/18,620 (0.18%) cases of laparoscopic and in 22/1488 (1.5%) cases of robotic technique. Duration of surgery robotic, open and laparoscopic ranged from 54.6 to 328.7, 129 to 234, and from 50.2 to 260 min, respectively. The present evidence reveals that robotic surgery, under specific conditions, has the potential to become cost-effective. Large number of cases, presence of industry competition and multidisciplinary team utilisation are some of the factors that could make more reasonable and cost-effective the robotic-assisted technique.
Keywords: Costs, general surgery, healthcare economics, outcomes, robotics, training
INTRODUCTION
The evolution of robotic technology during the last decade has facilitated the realisation of a great variety of operations in various surgical fields.[1] The robotic-assisted technique has an important position among the other minimally invasive methods in general surgery. Several are the main advantages of robotic-assisted surgery, such as three-dimensional view of the operating field, low intraoperative blood loss, the precision of movements due to the elimination of surgeon tremor, utilisation of wristed instruments that improve dexterity and facilitate suturing, have made possible even the most complicate operations such as robotic pancreaticoduodenectomy.[2,3,4] In contrast to the above-mentioned advantages, the absence of tactile feedback of the surgeon and the cost are the main weak points of the robotic technique.
Nowadays, the only commercially available robotic equipment “(da Vinci®, Intuitive Surgical Inc.; CA, USA) is characterised by elevated cost, including the cost of acquisition, training, and equipment-instrument cost, as well as that of maintenance of the robotic system (with an annual service contract, over 100,000 US dollars). This high cost can explain the reasons that decreased the widespread use of robotic-assisted surgery.[4] According to van Dam et al., to amortise the initial capital for the acquisition of robotic devices, the technique should be applied on more than 300 surgical procedures per year for 7 years, equivalent to an amount of over 1000 Euros per patient.[4] As a result, it can be easily understood that the robotic technology refers exclusively to surgical centres with a large volume of patients to achieve the per case charges as low as possible. The robotic instrumentation that has increased the cost of acquisition (almost over 1500 Euros per instrument), as well as a limited number of use (10 uses per instrument), represent another financial burden.[5] Moreover, the reimbursement to the hospital for utilisation of the robot is in direct correlation with the type of health insurance and the health system itself, favouring the countries without universal health coverage.
The purpose of this review is to evaluate the till now available literature on the cost assessment of robotic technology in the field of general surgery.
METHODS
Data sources
A systematic search was held in PubMed (16 November 2015) and Scopus (16 November 2015) databases. The same search strategy was implemented in both PubMed and Scopus databases, consisted of a sequence of keywords: (Robot OR robotic OR telesurgery) AND (general surgery OR bariatric OR colorectal resection OR cholecystectomy OR appendicectomy OR pancreatectomy OR splenectomy OR fundoplication OR pancreaticoduodenectomy) AND (cost OR cost analysis). The references of each included study were also searched.
Study selection criteria
All comparative articles providing information regarding the cost evaluation of robotic technology in general surgery were regarded as valid for this review. Only articles published in English, German, French, Italian, Spanish and Greek were involved in this review. Abstracts, reviews, letters to the editor, short surveys, commentaries and editorials were not included in this review.
Definitions
Operative charges are constituted of the medical costs referred exclusively to operation (e.g. operating theatre, anaesthesia and surgical supply). Non-operative charges are constituted of all the costs not referred exclusively to the operation but to preoperative procedure and postoperative recuperation (e.g., postoperative medication, hospital stay, laboratory, and radiology). Total costs are constituted of the sum of operative and non-operative charges. All costs are calculated in Euros.
A total of 175 and 656 studies were retrieved, respectively, in PubMed and Scopus search among which 31 studies that have met the inclusion criteria of our systematic review.[6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36] Three additional studies were included through hand-searching of included references.[11,23,25] Figure 1 represents the followed search strategy (flow diagram).
Figure 1.
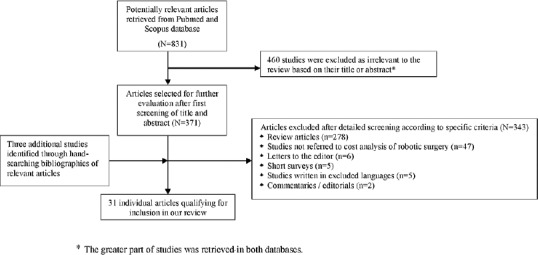
Flow diagram of the selection process of the included articles in the review
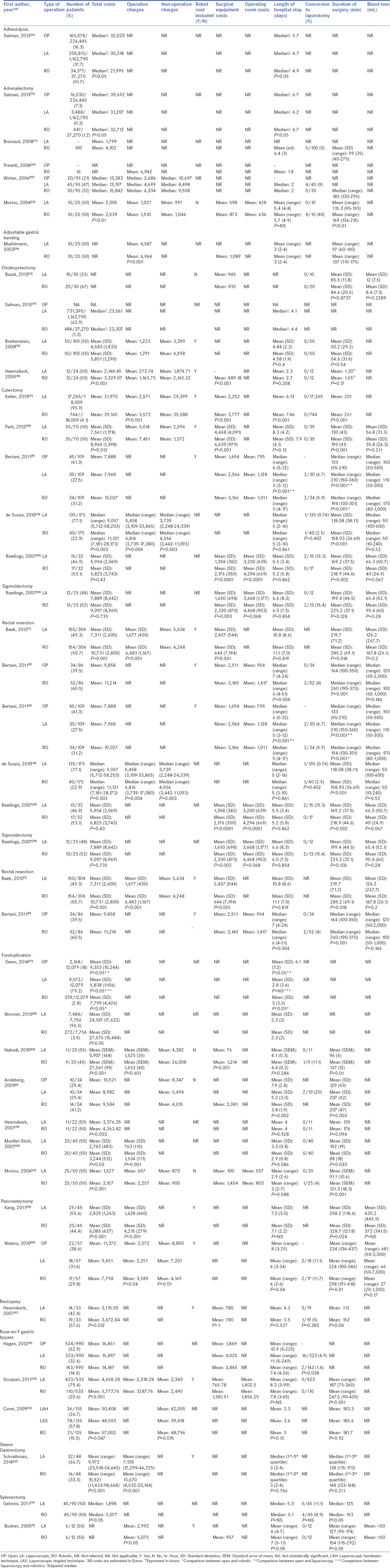
The principal characteristics of the included studies in our review (demographics, type of operation, number of patients, total costs, operative charges, non-operative charges, robot charges included to the total costs, surgical equipment costs, operating theatre costs, length of hospital stay, number of conversions to laparotomy, duration of the operation and blood loss) are presented in Table 1.
Table 1.
Robotics in general surgery: costs related to equipment and peri-operative outcomes†
Statistical considerations
Nonparametric statistical techniques were applied in this study. These methods are appropriate because the studies’ data did not present normal distributions. Kruskal–Wallis test was used to test the differences in the median between the three surgical techniques (OP, LA, and RO) applied in various types of operations. The value of P < 0.05 denoted statistical significance.
RESULTS
Among the 31 studies included, 7 referred to gastric fundoplication, 5 to adrenalectomy, 5 to colectomy, 4 to cholecystectomy, 3 to Roux-en-Y gastric bypass, 2 to pancreatectomy, 2 to rectal resection, 2 to splenectomy, 1 to positioning of adjustable gastric banding, 1 to sigmoidectomy, 1 to gastroenterostomy, 1 to rectopexy, 1 to sleeve gastrectomy and 1 to adhesiolysis. The median cost for adhesiolysis ranged from 21,995 to 32,020, and the weighted median average was 30,309.38 for 405,068 patients, regardless the type of operation. The median cost for adrenalectomy ranged from 13,197 to 32,712 and the weighted median average was 38.093,38 for 20.465 patients, regardless the type of operation. The median cost for cholecystectomy ranged from 23,307 to 23,561, and the weighted median average was 23,560.83 for 731,879 patients, regardless the type of operation. The median cost for splenectomy ranged from 1898 to 5077, and the weighted median average was 3487.50 for 90 patients, regardless the type of operation [Figure 2]. There was a significant different between adhesiolysis, adrenalectomy and cholecystectomy as well (P < 0.01). Seven studies had 3 arms comparing robotic to open to laparoscopic, 2 studies had 2 arms comparing robotic to open while 22 studies compared robotic with the laparoscopic technique. Of the 31 studies listed, 14 had no surgical equipment or operating room costs. Of these 14, further 7 were not analysing any operative charges or non-operative charges but only total costs. 184,431 patients were operated by the open method, 1,006,285 patients with laparoscopic and 37,814 with robotic. The mean cost for robotic, open and laparoscopic ranged from 2539 to 57,002, 7888 to 16,851 and 1799 to 50,408 Euros, respectively. The mean operative charges ranged from 273.74 to 13,670 Euros. For robotic and laparoscopic gastric fundoplication, the cost ranged from 1534 to 2257 and 657 to 763 Euros, respectively. For adrenalectomy, it ranged from 1510 to 6942 and 1027 to 4699 Euros, respectively. For robotic and laparoscopic colectomy, it ranged from 3739 to 17,080 and 3109 to 33,865 Euros, respectively. For robotic and laparoscopic cholecystectomy, it ranged from 1163.75 to 1291 and 273.74 to 1223 Euros, respectively. Regarding the Roux-en-Y gastric bypass, only one study mentioned the mean operative charges for a robotic and laparoscopic method which was 3287.76 and 2318.28 Euros, respectively. For robotic and laparoscopic pancreatectomy, it ranged from 3589 to 4215 and 1628 to 2251 Euros, respectively. Regarding rectal resection, only one study was retrieved in which the mean operative charges for the robotic and laparoscopic method was 6483 and 1677 Euros, respectively. The mean non-operative costs ranged from 900 to 48,796, from 8347 to 8800 and from 870 to 42,055 Euros, for robotic, open and laparoscopic technique, respectively. The mean operative costs for splenectomy was 5075 Euros for robotic technique and 2992 Euros for laparoscopic technique. In twelve studies, the robotic costs were included in the estimation of operative charges. Surgical equipment costs variated between 644 and 6639 Euros. Operating theatre costs ranged from 636 to 4468 Euros per surgical case. Regarding adhesiolysis, andrenalectomy and cholecystecomy, the weighted median average costs were 29,703.10 for operative charges, 25,703.10 for laparoscopic charges and 22,122.32 for robotic charges. There was a significant difference between these three types of operations P < 0.05 [Figure 2].
Figure 2.
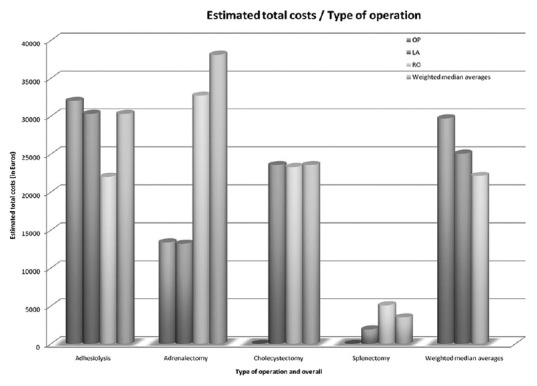
Estimated total costs in correlation of the surgical technique used in three types of operations
The mean hospital stay (in days) for robotic, open and laparoscopic techniques ranged from 1.8 to 51, from 3 to 220 and from 2.3 to 11, respectively. More specifically, in robotic, open and laparoscopic gastric fundoplication, it ranged from 2.3 to 4, 6.1 to 7.9 and 2.3 to 5.2 days, respectively. For robotic and laparoscopic adrenalectomy, it ranged from 1.8 to 6.4 and 2 to 6.2 (median) days, respectively. For robotic, open and laparoscopic colectomy, it ranged from 5.2 to 7.46, 5 to 32 and 5.5 to 8.3, respectively. For robotic and laparoscopic cholecystectomy, it ranged from 2.7 to 4.58 and 2.3 to 4.84, respectively. In Roux-en-Y gastric bypass, for robotic, open and laparoscopic technique, it ranged from 3 to 7.8, 5 to 220 and from 3.3 to 11, respectively. In pancreatectomy, it ranged from 4 to 7.1, 3 to 25 and 6 to 7.3, respectively. In rectal resection, it ranged from 4 to 51, 4 to 24 and 10.8 ± 8.6, respectively. In splenectomy, it ranged from 5 to 11 and 4 to 7, respectively for the robotic and the laparoscopic technique. Conversions to laparotomy were performed in 34/18,620 (0.18%) cases of laparoscopic and in 22/1488 (1.5%) cases of robotic technique. The mean duration of robotic, open and laparoscopic techniques ranged from 54.6 to 328.7, 129 to 234 and from 50.2 to 260 min, respectively. Blood loss in robotic, open and laparoscopic ranged from 8.4 to 279, from 120 to 681 and from 12 to 667 ml, respectively.
DISCUSSION
The introduction of innovative and less invasive technologies in surgical fields has been adopted with great difficulty from the health care systems as a consequence of the lack of data and of the high costs (acquisition and maintenance) of every novel equipment.[37] In the current finance situation, where a great portion of the world is facing difficulties to sustain the already present health structures, it would be considered scandalous to introduce new and highly expensive technique such as robotics as the new standard of care without the presence of strong evidence of significant cost-effectiveness and the comparison of minimally invasive methods to standard surgical techniques. Although cost related studies are complicated to be organised, it is essential that all parts involved, society and doctors should comprehend the impact of the cost of robotics.
Robotic-assisted surgery specifically requires equipment of elevated cost as a result of the novelty and the high specialisation of the utilised devices.[5,38] The high cost of acquisition (over 1 million Euros) as well the expensive maintenance costs (almost 150,000 Euros/year) are obstacles that should be overcome. van Dam et al. have suggested that the costs of robotic equipment could be amortised, if the health care systems permit the application of robotic equipment on elevated number of patients.[4] Furthermore, the absence of competition in the market of robotic equipment, especially after 2003, is one of the most important factors that maintain high the costs of robotic instrumentation.[39] More specifically, in 2003, the merge of the only two existed companies in the market of robotic devices was achieved, creating monopoly conditions.
The operating time is another essential reason that may cause great variations on the total surgical costs. Even though for private health structures, the length of the operating time is not an issue, for public health systems, which are financed by the government's budget, every penny must be carefully spent. The setup of the robotic equipment, which is significantly longer compared to either the laparoscopic or the open one can increase the cost. However, it was shown that this time can be substantially improved when the surgical team is well trained.[37] Furthermore, the operative time is related to the experience of the surgical team. The type of surgical operation, as well as the surgeon's capability and experience, are factors that influence considerably the learning curve.[4] In addition, the costs are in correlation with the learning curve and are considered an additional cost caused by the fact that surgeons already went through a training program for both laparoscopic and open technique.[40] Nevertheless, it should be mentioned that an effective way to decrease the costs related to learning curve is the presence of great volume of patients and the necessity of virtual reality simulators.[41,42] Minimal invasive techniques have revealed to have an edge over laparotomy for the management of patients in a wide spectrum of pathologies.[43,44] Keyhole incisions offer various advantages over the open surgical method, such as decrease of both postoperative pain and recovery time, less postoperative complications, reduced blood loss, and better cosmetic result. In particular, robotic techniques have a positive impact on specific patients’ categories, such as the reduction of operative costs and of hospital stay in elderly or morbidly obese patients. According to some studies, the total cost between both open and laparoscopic technique do not present statistically significant difference.[45,46]
The extent of hospital stay has an important influence on the total charges of hospitalisation. The limited hospital stay is a principal characteristic of both robotic and laparoscopic approach as it is expected in comparison to the open method.[5] Therefore, the decreased number of hospital days can amortise part of the increased operative costs of the minimally invasive techniques. Besides, the expenses of hospitalisation are also in strait correlation with the category of health care system and the type of health care structure.[4,47] Differences between countries, private or public sectors render complex any approach to evaluate those cost data. Regarding the comparison of robotic procedures to laparoscopy, several studies claim that over hospital stay the robotic surgery seems to have a slight financial advantage over the standard laparoscopy.[48] Nevertheless, currently, it appears that laparoscopy is a most economic approach among the other minimally invasive methods.
As presented in Table 1, the greater part of the studies referred to gastric fundoplication and showed that robotic is more expensive in comparison to laparoscopic technique. Despite the cost of acquisition the robotic devices, professional charges, operating theatre costs, surgical equipment costs present great variation in the included studies. Such a cost could be minimised if we also take into consideration the decrease of the hospital stay, the sooner return to normal patient's activities, the reduction of blood loss and the decrease on conversion rates to laparotomy. Furthermore, by improving the robotic training of all personnel, the surgical time could be further reduced and as consequence favour the use of minimally invasive techniques.
The utilisation of robotics in almost every surgical field could be thought, in the future, as a valuable tool in common surgical practice. To realise this fact, both operative costs and unnecessary charges should be eliminated. The formation of specialised robotic units operating on great number of cases per year, the reduction of operating time per procedure by specialised training on robotic approach, the decision for early discharge of the patients when that is possible and the minimisation of the number of instruments used per operation are some of the first steps that could be done in this direction. An additional proposal to minimise the cost is the multiple-use of the robotic equipment by multiple surgical specialties, good training of all the team members implicated while the acquisition of the robotic devices could be made through research funding or even charities.
Numerous limitations should be taken into consideration in the interpretation of the results of this review. The restricted number of the included studies and of the number of the included patients in these studies is in relation with the innovation of the technique. The study design, the volume of the surgical cases, the surgeon's experience as well as the different hospital suppliers among the various institutions and the different countries are factors that render difficult any comparison between the robotic-assisted and the other techniques. Due to the lack of available data, we limited to evaluate the weighted median average cost of only the types of operations. The “cost” calculation is also difficult to be evaluated due to the existence of multiple variables, such as presence of diverse health systems and the differences between private and public sector. Cost is a difficult parameter to obtain from hospitals. We refer to cost, even when discussing professional fees, however the majority of the literature typically reports hospital charges rather than cost. Thus, somebody could highlight that the stated purpose for the review might be better stated to compare hospital charges for performing robotic surgery to more traditional approaches (open and/or laparoscopically). Based on our literature search, robotic-assisted technique cost more in comparison with laparoscopic or open procedures, although it appears that when the initial acquisition costs for robotic equipment is left apart then robotic techniques are the most effective method regarding costs. Nevertheless, because of great heterogeneity of the included studies and the absence of all the above mentioned information (indirect, direct, total, fixed or variable cost of each included study), in our opinion, safe conclusions could not be extracted on cost-effectiveness of robotic use in general surgery, due to more recent studies including operations performed by more well trained surgical teams. In addition, the lack of studies that refer on long-term clinical outcomes, such as quality adjusted life-year gained, is an obstacle on the realisation of a real cost-effective analysis. The costs related to readmission are difficult to be retrieved and included in the data analysis. Last but not least, the diverse types of operations included have different costs as well as different cost of total surgical time. Regarding, the adopted search strategy which was previously mentioned, it could be defined as restricted as a result of the exclusion of various publication types (such as abstracts, short surveys, reviews, etc.) and the limitation on the written language of the included studies.
CONCLUSION
The implement of robotic technology in operations of general surgery represent a novelty that may influence both the surgical treatment of numerous pathologies and the postoperative outcomes. The robotic assisted surgery has serious possibilities to evolve in a cost-effective technique, especially in centres with large number of cases, in spite of the undeniable elevated costs of acquisition and maintenance. Having as intention to increase the use of this surgical technique, it should be utilised not only on clinical treatment of patients but as well for the surgical training of all residents. The possible future industry competition in correlation with the technological development may steadily reduce the cost of the robotic equipment, making robotics a more cost-effective and affordable technique.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Yu HY, Friedlander DF, Patel S, Hu JC. The current status of robotic oncologic surgery. CA Cancer J Clin. 2013;63:45–56. doi: 10.3322/caac.21160. [DOI] [PubMed] [Google Scholar]
- 2.Boggi U, Signori S, De Lio N, Perrone VG, Vistoli F, Belluomini M, et al. Feasibility of robotic pancreaticoduodenectomy. Br J Surg. 2013;100:917–25. doi: 10.1002/bjs.9135. [DOI] [PubMed] [Google Scholar]
- 3.Smith JA, Jr, Herrell SD. Robotic-assisted laparoscopic prostatectomy: Do minimally invasive approaches offer significant advantages? J Clin Oncol. 2005;23:8170–5. doi: 10.1200/JCO.2005.03.1963. [DOI] [PubMed] [Google Scholar]
- 4.van Dam P, Hauspy J, Verkinderen L, Trinh XB, van Dam PJ, Van Looy L, et al. Are costs of robot-assisted surgery warranted for gynecological procedures? Obstet Gynecol Int 2011. 2011:973830. doi: 10.1155/2011/973830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lotan Y. Is robotic surgery cost-effective: No. Curr Opin Urol. 2012;22:66–9. doi: 10.1097/MOU.0b013e32834d4d76. [DOI] [PubMed] [Google Scholar]
- 6.Anderberg M, Kockum CC, Arnbjornsson E. Paediatric robotic surgery in clinical practice: A cost analysis. Eur J Pediatr Surg. 2009;19:311–5. doi: 10.1055/s-0029-1233495. [DOI] [PubMed] [Google Scholar]
- 7.Baek SJ, Kim SH, Cho JS, Shin JW, Kim J. Robotic versus conventional laparoscopic surgery for rectal cancer: A cost analysis from a single institute in Korea. World J Surg. 2012;36:2722–9. doi: 10.1007/s00268-012-1728-4. [DOI] [PubMed] [Google Scholar]
- 8.Bertani E, Chiappa A, Biffi R, Bianchi PP, Radice D, Branchi V, et al. Assessing appropriateness for elective colorectal cancer surgery: Clinical, oncological, and quality-of-life short-term outcomes employing different treatment approaches. Int J Colorectal Dis. 2011;26:1317–27. doi: 10.1007/s00384-011-1270-0. [DOI] [PubMed] [Google Scholar]
- 9.Bodner J, Kafka-Ritsch R, Lucciarini P, Fish JH, 3rd, Schmid T. A critical comparison of robotic versus conventional laparoscopic splenectomies. World J Surg. 2005;29:982–5. doi: 10.1007/s00268-005-7776-2. [DOI] [PubMed] [Google Scholar]
- 10.Breitenstein S, Nocito A, Puhan M, Held U, Weber M, Clavien PA. Robotic-assisted versus laparoscopic cholecystectomy: Outcome and cost analyses of a case-matched control study. Ann Surg. 2008;247:987–93. doi: 10.1097/SLA.0b013e318172501f. [DOI] [PubMed] [Google Scholar]
- 11.Brunaud L, Ayav A, Zarnegar R, Rouers A, Klein M, Boissel P, et al. Prospective evaluation of 100 robotic-assisted unilateral adrenalectomies. Surgery. 2008;144:995–1001. doi: 10.1016/j.surg.2008.08.032. [DOI] [PubMed] [Google Scholar]
- 12.Buzad FA, Corne LM, Brown TC, Fagin RS, Hebert AE, Kaczmarek CA, et al. Single-site robotic cholecystectomy: Efficiency and cost analysis. Int J Med Robot. 2013;9:365–70. doi: 10.1002/rcs.1507. [DOI] [PubMed] [Google Scholar]
- 13.Curet MJ, Curet M, Solomon H, Liu G, Morton JM. Comparison of hospital charges between robotic, laparoscopic stapled, and laparoscopic handsewn Roux-en-Y gastric bypass. [Last accessed on 2016 May 13];J Robot Surg. 2009 3:75–8. doi: 10.1007/s11701-009-0143-9. Available from: http://link.springer.com/article/101007/s11701-009-0143-9 . [DOI] [PubMed] [Google Scholar]
- 14.deSouza AL, Prasad LM, Park JJ, Marecik SJ, Blumetti J, Abcarian H. Robotic assistance in right hemicolectomy: Is there a role? Dis Colon Rectum. 2010;53:1000–6. doi: 10.1007/DCR.0b013e3181d32096. [DOI] [PubMed] [Google Scholar]
- 15.Gelmini R, Franzoni C, Spaziani A, Patriti A, Casciola L, Saviano M. Laparoscopic splenectomy: Conventional versus robotic approach – A comparative study. J Laparoendosc Adv Surg Tech A. 2011;21:393–8. doi: 10.1089/lap.2010.0564. [DOI] [PubMed] [Google Scholar]
- 16.Hagen ME, Pugin F, Chassot G, Huber O, Buchs N, Iranmanesh P, et al. Reducing cost of surgery by avoiding complications: The model of robotic Roux-en-Y gastric bypass. Obes Surg. 2012;22:52–61. doi: 10.1007/s11695-011-0422-1. [DOI] [PubMed] [Google Scholar]
- 17.Heemskerk J, de Hoog DE, van Gemert WG, Baeten CG, Greve JW, Bouvy ND. Robot-assisted vs. conventional laparoscopic rectopexy for rectal prolapse: A comparative study on costs and time. Dis Colon Rectum. 2007;50:1825–30. doi: 10.1007/s10350-007-9017-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Heemskerk J, van Dam R, van Gemert WG, Beets GL, Greve JW, Jacobs MJ, et al. First results after introduction of the four-armed da Vinci Surgical System in fully robotic laparoscopic cholecystectomy. Dig Surg. 2005;22:426–31. doi: 10.1159/000091445. [DOI] [PubMed] [Google Scholar]
- 19.Heemskerk J, van Gemert WG, Greve JW, Bouvy ND. Robot-assisted versus conventional laparoscopic Nissen fundoplication: A comparative retrospective study on costs and time consumption. Surg Laparosc Endosc Percutan Tech. 2007;17:1–4. doi: 10.1097/01.sle.0000213756.76761.b7. [DOI] [PubMed] [Google Scholar]
- 20.Kang CM, Kim DH, Lee WJ, Chi HS. Conventional laparoscopic and robot-assisted spleen-preserving pancreatectomy: Does da Vinci have clinical advantages? Surg Endosc. 2011;25:2004–9. doi: 10.1007/s00464-010-1504-1. [DOI] [PubMed] [Google Scholar]
- 21.Keller DS, Senagore AJ, Lawrence JK, Champagne BJ, Delaney CP. Comparative effectiveness of laparoscopic versus robot-assisted colorectal resection. Surg Endosc. 2014;28:212–21. doi: 10.1007/s00464-013-3163-5. [DOI] [PubMed] [Google Scholar]
- 22.Morino M, Benincà G, Giraudo G, Del Genio GM, Rebecchi F, Garrone C. Robot-assisted vs laparoscopic adrenalectomy: A prospective randomized controlled trial. Surg Endosc. 2004;18:1742–6. doi: 10.1007/s00464-004-9046-z. [DOI] [PubMed] [Google Scholar]
- 23.Morino M, Pellegrino L, Giaccone C, Garrone C, Rebecchi F. Randomized clinical trial of robot-assisted versus laparoscopic Nissen fundoplication. Br J Surg. 2006;93:553–8. doi: 10.1002/bjs.5325. [DOI] [PubMed] [Google Scholar]
- 24.Mühlmann G, Klaus A, Kirchmayr W, Wykypiel H, Unger A, Höller E, et al. DaVinci robotic-assisted laparoscopic bariatric surgery: Is it justified in a routine setting? Obes Surg. 2003;13:848–54. doi: 10.1381/096089203322618632. [DOI] [PubMed] [Google Scholar]
- 25.Müller-Stich BP, Reiter MA, Wente MN, Bintintan VV, Köninger J, Büchler MW, et al. Robot-assisted versus conventional laparoscopic fundoplication: Short-term outcome of a pilot randomized controlled trial. Surg Endosc. 2007;21:1800–5. doi: 10.1007/s00464-007-9268-y. [DOI] [PubMed] [Google Scholar]
- 26.Nakadi IE, Mélot C, Closset J, DeMoor V, Bétroune K, Feron P, et al. Evaluation of da Vinci Nissen fundoplication clinical results and cost minimization. World J Surg. 2006;30:1050–4. doi: 10.1007/s00268-005-7950-6. [DOI] [PubMed] [Google Scholar]
- 27.Owen B, Simorov A, Siref A, Shostrom V, Oleynikov D. How does robotic anti-reflux surgery compare with traditional open and laparoscopic techniques: A cost and outcomes analysis. Surg Endosc. 2014;28:1686–90. doi: 10.1007/s00464-013-3372-y. [DOI] [PubMed] [Google Scholar]
- 28.Park JS, Choi GS, Park SY, Kim HJ, Ryuk JP. Randomized clinical trial of robot-assisted versus standard laparoscopic right colectomy. Br J Surg. 2012;99:1219–26. doi: 10.1002/bjs.8841. [DOI] [PubMed] [Google Scholar]
- 29.Prewitt R, Bochkarev V, McBride CL, Kinney S, Oleynikov D. The patterns and costs of the da Vinci robotic surgery system in a large academic institution. [Last accessed on 2016 May 13];J Robot Surg. 2008 2:17–20. doi: 10.1007/s11701-008-0075-9. Available from: http://link.springer.com/article/101007%2Fs11701-008-0075-9 . [DOI] [PubMed] [Google Scholar]
- 30.Rawlings AL, Woodland JH, Vegunta RK, Crawford DL. Robotic versus laparoscopic colectomy. Surg Endosc. 2007;21:1701–8. doi: 10.1007/s00464-007-9231-y. [DOI] [PubMed] [Google Scholar]
- 31.Salman M, Bell T, Martin J, Bhuva K, Grim R, Ahuja V. Use, cost, complications, and mortality of robotic versus nonrobotic general surgery procedures based on a nationwide database. Am Surg. 2013;79:553–60. [PubMed] [Google Scholar]
- 32.Schraibman V, Macedo AL, Epstein MG, Soares MY, Maccapani G, Matos D, et al. Comparison of the morbidity, weight loss, and relative costs between robotic and laparoscopic sleeve gastrectomy for the treatment of obesity in Brazil. Obes Surg. 2014;24:1420–4. doi: 10.1007/s11695-014-1239-5. [DOI] [PubMed] [Google Scholar]
- 33.Scozzari G, Rebecchi F, Millo P, Rocchietto S, Allieta R, Morino M. Robot-assisted gastrojejunal anastomosis does not improve the results of the laparoscopic Roux-en-Y gastric bypass. Surg Endosc. 2011;25:597–603. doi: 10.1007/s00464-010-1229-1. [DOI] [PubMed] [Google Scholar]
- 34.Waters JA, Canal DF, Wiebke EA, Dumas RP, Beane JD, Aguilar-Saavedra JR, et al. Robotic distal pancreatectomy: Cost effective? Surgery. 2010;148:814–23. doi: 10.1016/j.surg.2010.07.027. [DOI] [PubMed] [Google Scholar]
- 35.Winter JM, Talamini MA, Stanfield CL, Chang DC, Hundt JD, Dackiw AP, et al. Thirty robotic adrenalectomies: A single institution's experience. Surg Endosc. 2006;20:119–24. doi: 10.1007/s00464-005-0082-0. [DOI] [PubMed] [Google Scholar]
- 36.Wormer BA, Dacey KT, Williams KB, Bradley JF, 3rd, Walters AL, Augenstein VA, et al. The first nationwide evaluation of robotic general surgery: A regionalized, small but safe start. Surg Endosc. 2014;28:767–76. doi: 10.1007/s00464-013-3239-2. [DOI] [PubMed] [Google Scholar]
- 37.Heemskerk J, Bouvy ND, Baeten CG. The end of robot-assisted laparoscopy? A critical appraisal of scientific evidence on the use of robot-assisted laparoscopic surgery. Surg Endosc. 2014;28:1388–98. doi: 10.1007/s00464-013-3306-8. [DOI] [PubMed] [Google Scholar]
- 38.Turchetti G, Palla I, Pierotti F, Cuschieri A. Economic evaluation of da Vinci-assisted robotic surgery: A systematic review. Surg Endosc. 2012;26:598–606. doi: 10.1007/s00464-011-1936-2. [DOI] [PubMed] [Google Scholar]
- 39.Intuitive SIW, the Free Encyclopedia. [Last accessed on 2015 Sep 10]. Available from: http://www.enwikipedia.org/wiki/Intuitive_Surgical .
- 40.Steinberg PL, Merguerian PA, Bihrle W, 3rd, Seigne JD. The cost of learning robotic-assisted prostatectomy. Urology. 2008;72:1068–72. doi: 10.1016/j.urology.2007.11.118. [DOI] [PubMed] [Google Scholar]
- 41.Albani JM, Lee DI. Virtual reality-assisted robotic surgery simulation. J Endourol. 2007;21:285–7. doi: 10.1089/end.2007.9978. [DOI] [PubMed] [Google Scholar]
- 42.Iavazzo C, Papadopoulou EK, Gkegkes ID. Cost assessment of robotics in gynecologic surgery: A systematic review. J Obstet Gynaecol Res. 2014;40:2125–34. doi: 10.1111/jog.12507. [DOI] [PubMed] [Google Scholar]
- 43.Blackmore AE, Wong MT, Tang CL. Evolution of laparoscopy in colorectal surgery: An evidence-based review. World J Gastroenterol. 2014;20:4926–33. doi: 10.3748/wjg.v20.i17.4926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ng AT, Tam PC. Current status of robot-assisted surgery. Hong Kong Med J. 2014;20:241–50. doi: 10.12809/hkmj134167. [DOI] [PubMed] [Google Scholar]
- 45.Gorter RR, Heij HA, Eker HH, Kazemier G. Laparoscopic appendectomy: State of the art. Tailored approach to the application of laparoscopic appendectomy? Best Pract Res Clin Gastroenterol. 2014;28:211–24. doi: 10.1016/j.bpg.2013.11.016. [DOI] [PubMed] [Google Scholar]
- 46.Magrina JF. Outcomes of laparoscopic treatment for endometrial cancer. Curr Opin Obstet Gynecol. 2005;17:343–6. doi: 10.1097/01.gco.0000175350.18308.73. [DOI] [PubMed] [Google Scholar]
- 47.Schreuder HW, Verheijen RH. Robotic surgery. BJOG. 2009;116:198–213. doi: 10.1111/j.1471-0528.2008.02038.x. [DOI] [PubMed] [Google Scholar]
- 48.Seamon LG, Cohn DE, Henretta MS, Kim KH, Carlson MJ, Phillips GS, et al. Minimally invasive comprehensive surgical staging for endometrial cancer: Robotics or laparoscopy? Gynecol Oncol. 2009;113:36–41. doi: 10.1016/j.ygyno.2008.12.005. [DOI] [PubMed] [Google Scholar]


