Abstract
Background:
Laparoscopic cholecystectomy (LC) has many advantages as compared to open cholecystectomy. However, vasculobiliary injuries still continue to be a matter of concern despite advances in laparoscopic techniques. Misidentification and misperception of vasculobiliary structures is considered to be a pivotal factor leading to injuries. Although many studies since time immemorial have stressed on the importance of anatomy, an insight into laparoscopic anatomy is what essentially constitutes the need of the hour.
Objective:
To assess the frequency and the relevance of anatomical variations of extrahepatic biliary system in patients undergoing LC.
Materials and Methods:
The present study is an observational study performed for a period of 2 years from August 2014 to August 2016. It included all diagnosed patients of cholelithiasis undergoing routine LC performed by a single surgeon by achieving a critical view of safety. During dissection, vascular and ductal anomalies were noted and assessed for their relevance in LC.
Results:
Seven hundred forty cases of cholelithiasis, irrespective of pathology, comprising 280 (37.83%) men and 460 (62.16%) females with a mean age of 39.85 ± 18.82 years were included in the study. Photodocumentation and operative recordings were available in 93% of cases. Operative findings revealed 197 (26.62%) vascular anomalies and 90 (12.16%) ductal anomalies. A single cystic artery was seen in 340 cases, and a normal cystic duct was seen in 650 cases. Variations in ductal anatomy were fewer than variations in vascular anatomy.
Conclusion:
Extra-biliary anatomy relevant to LC is unpredictable and varies from patient to patient. Vascular anomalies are more frequent than the ductal anomalies, and surgeon should be alert regarding their presence.
Keywords: Cystic artery, cystic duct, extrahepatic biliary anatomy, laparoscopic cholecystectomy
INTRODUCTION
Laparoscopic cholecystectomy (LC) has gained acceptance as a gold standard method of treating gallstone disease.[1] However, there is still concern about the most serious complication of this procedure, the iatrogenic injury of the bile duct (0.3%–0.5%).[1,2,3] The incidence of bile duct injuries (BDIs) seems to have decreased compared with earlier periods. However, several studies showed a persistent higher rate and complexity of BDI compared to open cholecystectomy (0.3%–0.6% vs. 0.2%).
The unpredictability of extra-biliary anatomy combined with inflammation and fibrosis at times distorts the existing anatomy to get the surgeon into an ‘error trap’ of misidentification and misperception of biliary structures and is the frequent cause of BDI.[2]
To overcome the dilemma of ‘misidentification’ surgeons should be aware of the arrangement of vasculobiliary structures in the Calot's region. Till date, the knowledge of vasculobiliary anatomy is by way of cadaveric dissections, laparoscopic ultrasonography and various types of intraoperative cholangiography. However, the figures quoted in the literature are variable; keeping the surgeon in a dilemma of unpredictability.
Knowledge of these variants is important before LC. However, pre-operative assessment of the existing biliary anatomy is available only in those cases where magnetic resonance cholangiopancreatography/endoscopic retrograde cholangiopancreatography (MRCP/ERCP) had been done for some other pathology and that too does not provide any information regarding the vascular arrangements.
Thus, the only way out is to dissect and delineate each and every vascular and ductal structure in a given patient irrespective of anatomy and anomalies. To do that, one needs to have the knowledge of ‘laparoscopic anatomy’ relevant to LC before proceeding for dissection.
Critical view of safety (CVS) as advocated by Strasberg and Brunt[4] is based on the concept of thorough dissection and delineation of the vasculo-ductal structures (VDSs) and provides the limits of dissection for safe LC. Hence, this method was adopted in the present study to know the clinical arrangement of VDSs encountered during LC, rather than having a fixed mindset based on theoretical knowledge.
Objectives
The purpose of the present study is to analyse the clinical arrangement and surgical relevance of intra-operative vasculo-biliary anatomy for execution of safe LC.
MATERIALS AND METHODS
The present study was a prospective study carried out for a period of 2 years from December 2014 to December 2016, after approval from Ethical and Research Committee, comprising 800 cases of cholelithiasis. All the included patients underwent LC by achieving all three components of CVS i.e., first, the triangle of Calot must be cleared of fat and fibrous tissue. It does not require that the common bile duct be exposed. The second requirement is that the lowest part of the gallbladder be separated from the cystic plate, the flat fibrous surface to which the non peritonealized side of the gallbladder is attached. The cystic plate, which is sometimes referred to as the liver bed of the gallbladder, is part of the plate/sheath system of the liver. The third requirement is that 2 structures, and only 2, should be seen entering the gallbladder.[4]
During dissection, the arrangement of vascular and biliary structures was noted, doublet photographed and/or video recorded. The available operative videos/photographs were reviewed and confirmed for the presence of anatomy. To minimise bias, the reviewing surgeon (two senior surgeons from other units of Department of Minimally Invasive Surgery) was blinded at the time of reviewing the photographs/videos.
OBSERVATIONS AND RESULTS
Out of 800 cases, there were 740 valid LC reports. No documentation was available for rest of sixty cases due to technical difficulties of recording errors and was excluded from the study.
The present study included 280 (37.83%) males and 460 (62.16%) females. The age range was 18–79 years with a mean age as 41.2 years. About 118 (15.94%) were complicated cholelithiasis (difficult LC), 97 (82.2%) were of acute cholecystitis, 17 (14.4%) were of empyema GB, 2 (1.6%) were gangrenous GB and 2 (1.6%) were Mirizzi's syndrome. Two independent surgeons independently reviewed the videos/photographs over a period of 2 months. The photographs were retrieved in 720 patients, video recording was retrieved in 610 cases and operation notes were available in all 740 cases. The photographs of inadequate quality were not considered for the study; instead, their videos were assessed for the achievement of CVS. Hence, in total, 740 patients were available for data analysis.
Vascular and ductal arrangements observed clinically were as follows:
DISCUSSION
A major impediment to the safe conclusion of cholecystectomy is the inability to identify clearly the location of the extrahepatic bile ducts and to access their relationship to the GB when the hepatoduodenal anatomy is obscured by the phlegmonous transformation or dense fibrosis.[5] Laparoscopic surgeons chose the approachable real living patients who undergo LC with its advantage of magnifying technology. The incidences of anomalies in the laparoscopic observational studies are higher and are more realistic than that of radiological or cadaveric dissection. In the present study, VDS was delineated in as many as 94% of cases in all types of GB disease i.e., complicated as well as uncomplicated. It was observed that in the majority of the cases, there was normal anatomy [Tables 1 and 2].
Table 1.
Variations in cystic artery and other vascular anomalies
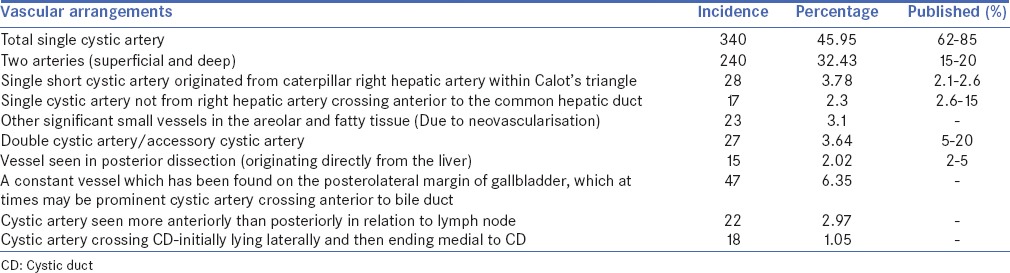
Table 2.
Variations in cystic duct anatomy and other ductal anomalies
Variations in ductal anatomy
Single cystic duct
A normal single cystic duct (CD) was observed in 650 cases which is in accordance with the fact that the CD variations are few compared to vascular. This observation has a lot of bearing as most of the classic injuries are related to the CD in one way or the other [Figure 1]. Primary entities involving the CD include calculous disease, Mirizzi's syndrome, CD-duodenal fistula, biliary obstruction, neoplasia and primary sclerosing cholangitis. Al Helli et al. reported an incidence of 62.5% of single CD in their case studies (125 cases).[6]
Figure 1.
Single cystic duct. One end is entering the gallbladder and the other end is entering the common bile duct
Long cystic duct
The most common ductal anomaly observed was long CD in 22 (7.02%) cases [Table 2]. Similar observation of 8.6% incidence has been seen by Benson and Page.[1] However, a very high incidence of 23% was observed by Hayes et al. in 1958. Al Helli et al. reported an incidence of 12.6% in their study.[6] Relatively less incidence of long CD in the present study could be because we did not define the CD-common bile duct (CBD) junction or locate the parallel course of CD until its insertion into common hepatic duct/right hepatic duct (RHD).
Long CD is of advantage to the surgeon as it allows easy manipulation and ensures that structure being handled is the CD only by its ending into the infundibulum. However, a long, parallel and spiral CD could be dangerous as its ending cannot be ascertained. Ligation of the CD too close to the common hepatic duct may result in stricture of the latter. Similarly, mistaking the CD for the bile duct can result in iatrogenic injury such as inadvertent ligation or transection of the extrahepatic bile duct.[7] In addition, an unusually long CD remnant (up to 6 cm in length) may be left after cholecystectomy. Approximately 10% of repeat surgeries performed after cholecystectomy are attributable to complications associated with the CD remnant (e.g., post-operative bile leakage, stricture and fistula formation). An enlarged or long CD remnant may be associated with inflammatory changes and formation of calculi, resulting in post-cholecystectomy syndrome, a cause of persistent or recurrent biliary symptoms in affected patients. A rare post-operative complication is a CD mucocele, in which the remnant becomes distended with mucus. CD may be overlapping the CBD in a spiral course when the CD is joining on the lateral side, then CBD runs behind the CD partially in parallel and joins it medially, thereby lifting it, leading to inadvertent injury to CBD.
Short cystic duct
In the present study, short CD was encountered in 17 (2.66%) cases, whereas Khan[8] has reported an almost similar incidence of 2.33%. In inflammatory conditions, it gets fused with the RHD/CBD, giving a false impression of infundibulum. Excessive traction on the GB brings CBD/RHD in line with the CD resulting in misidentification of CBD as CD and leading to inadvertent injury [Figure 2].
Figure 2.
Short cystic duct with stones
Variations in cystic duct insertion
In the present study, there were 8 cases of Type A (1.02%) i.e., CD joining the anterior sectorial duct, 11 cases of Type R (1.49%) i.e., CD joining the RHD and 6 cases of Type P (2.2%) i.e., CD joining the posterior sectorial duct [Table 2]. Buddingh KT et al.[9] reported an incidence of 0.6% of Type A, 1.4% of Type R and 1.2% of Type P. Prinz et al. and Daseler et al. reported 1% incidence of the CD joining the RHD.
For anatomic Types A, R and P, there is a high probability that a wrong duct may be cut. In Type R, one of the causes of injury is misidentification of the CD coming into the RHD. For Types A and P, one cause of injury is a failure to recognise that the CD enters onto a segmental duct. A surgeon may be highly likely to cut a wrong duct if he fails to distinguish the CD from the other bile duct.
Low medial insertion of the cystic duct
Low medial insertion of the CD deserves special attention because this anatomic variant may lead to misdiagnosis on imaging studies. Superimposition of the CD on the extrahepatic bile duct is commonly seen with this anatomic variant. CD stones in a low, medially inserting CD that joins the CBD at the ampulla may be mistaken for stones in the distal bile duct or may result in bile duct obstruction or gallstone pancreatitis. Retrograde filling of the low, medially inserting CD at ERCP may mimic the CBD or pancreatic duct, particularly if the CD is incompletely filled.
It is worth mentioning here that it is not important to know which duct it is, in fact what is important is that we have to isolate the CD from rest of the structures.
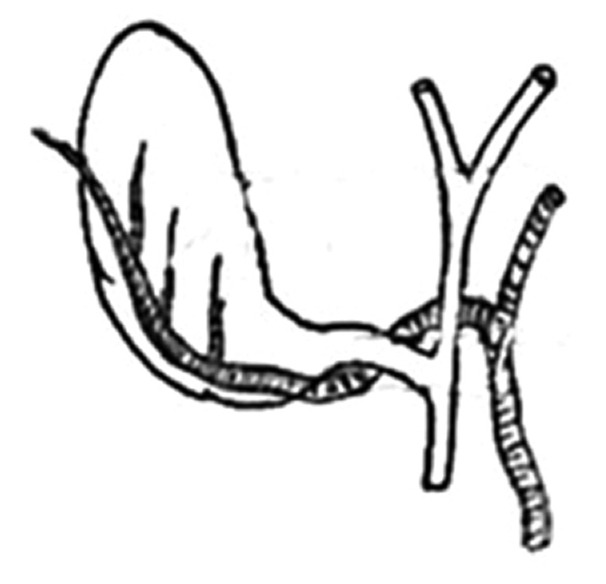
Subvesical ducts
In 1863, Lushka described a small, superficial duct located in the region of the GB and observed that these ducts drained into the major hepatic ducts. These ducts were named as ducts of Luschka or subvesical ducts.[2]
Subvesical ducts are present on both sides of the margins of the GB where the peritoneum is reflected onto the liver. Healey and Schroy[10] recorded an incidence of 15%, 35% and 50% in their study. In the present study, five cases of subvesical ducts [Figure 3] were observed (0.68%) [Table 2]. Although they may not drain any liver parenchyma, they can be a source of a bile leak or biliary peritonitis after cholecystectomy. Injury to these ducts can be avoided by giving adequate traction to the GB away from the liver edge.
Figure 3.
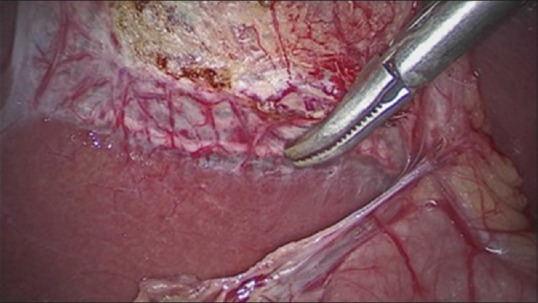
Subvesical duct draining into the biliary ductal system in close relationship to the gallbladder
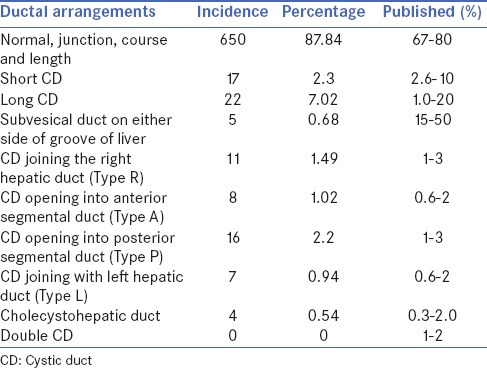
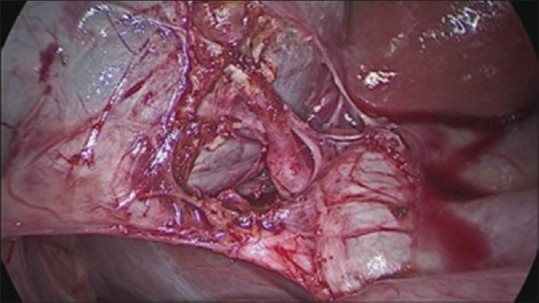
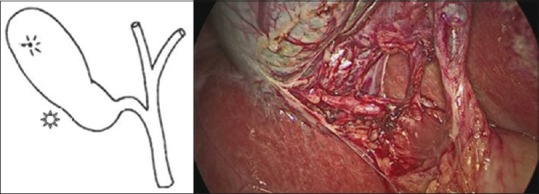
Cholecystohepatic ducts
Cholecystohepatic ducts were observed in four cases [Figure 4] while lifting GB from the cystic plate. Many studies have shown an incidence of 0.2%–2.3% of cholecystohepatic ducts. Although one cannot make out exactly the existence of these small ducts, one is sure to get a biliary fistula if they are injured. Only occasionally may they be seen by pre-operative endoscopic cholangiography or MRCP. Most of these ducts are too small to be delineated. This anatomic variant creates a risk of inadvertent ligation or transection of the aberrant duct near the CD insertion at cholecystectomy.
Figure 4.
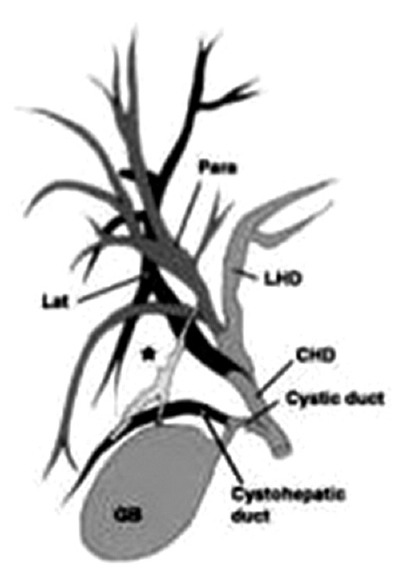
Diagram showing the cholecystohepatic duct
Variations in vascular anatomy
Variations in the vascular supply of the extrahepatic biliary tree are more common than variations in the ductal anatomy [Table 2]. Anatomic variations of the hepatic and cystic arteries are present in approximately 50% of individuals. A similar pattern of a higher number of vascular anomalies (384 out of 740 patients) was observed in the present study [Table 1].
Cystic artery bleeding is a troublesome complication during LC, which increases the rate of conversion to open surgery. The reported incidence of conversion to open surgery because of blood vessel injuries is approximately 0%–1.9% during LC and its mortality is about 0.02%. Safe LC demands a good knowledge of the anatomy of the cystic artery and its variations.
Classic single cystic artery
Cystic artery is a branch of the right hepatic artery and is usually given off in Calot's triangle. It usually gives off an anterior or superficial branch and a posterior or deep branch. This branching usually takes place near the GB. In addition, cystic artery gives a direct branch to the CD also, which usually comes across when dissection is made between duct and artery. A single cystic artery was seen in 340 cases in the present study [Figure 5 and Table 1].
Figure 5.
Classical single cystic artery
Accessory/double cystic artery
In the present study, there were 27 cases [Figure 6], in which double cystic artery was seen (2.64%); both were originating from the right hepatic artery within Calot's triangle [Table 1]. Benson and Page[1] described three surgically important variations in the arterial anatomy based on anatomic dissection. An accessory or double cystic artery being the most common anomaly occurred in 15%–20% of individual in their study. Al Helli et al. have reported an incidence of 3.50% (7 cases) in their study.[6]
Figure 6.
Double cystic artery
Caterpillar hump
The right hepatic artery occasionally forms a sinuous tortuosity called as caterpillar hump or Moynihan's hump, which occupies a major portion of the Calot's triangle. In the present study, there were 28 cases of caterpillar hump (3.78%). Benson and Page reported an incidence of 5%–15% in their study.[1] Due to variant course, right hepatic artery comes in proximity to the CD and GB, resulting in the formation of a short cystic artery. Hence, the right hepatic artery may be mistaken as cystic artery and inadvertently ligated resulting in torrential bleeding, and later on necrosis of the right lobe of the liver. Furthermore, since the cystic artery arising from the caterpillar hump is short, it can easily get avulsed from the hepatic artery [Figure 7].
Figure 7.
Cystic artery arising from caterpillar hump (right hepatic artery)
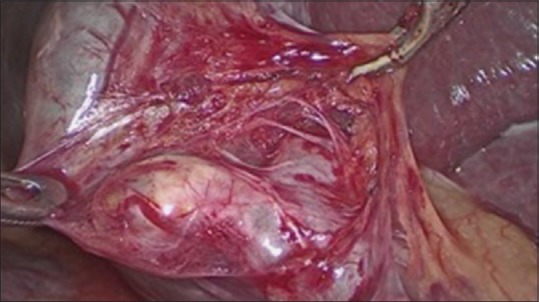
Two vessels (anterior and posterior)
When approaching the GB, the cystic artery is divided into deep and superficial branches at the neck of the GB. The superficial branch proceeds along the left side of the GB. The deep branch runs through the connective tissues between the GB and liver parenchyma. The deep branch gives rise to tiny branches to supply the GB, which anastomose with the superficial branches. According to the literature, this type is found in 70%–80% of cases. In the present study, these were seen in 240 cases [Figure 8].
Figure 8.
Two vessels (anterior and posterior)
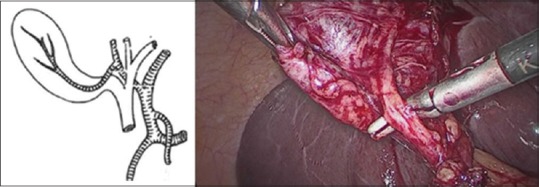
Cystic artery with an uncertain origin (Gastroduodenal artery, superior pancreaticoduodenal, celiac trunk, right gastric artery)
This was seen in seven cases [Figure 9 and Table 1]. This type of cystic artery is also called low-lying cystic artery, which does not pass through Calot's triangle but approaches the GB beyond it. In conventional open cholecystectomy, it is seen as inferior to the CD, while it usually localises superficially and anterior to the CD from a laparoscopic viewpoint. Its terminal segment as it approaches the GB is important for laparoscopic surgeons. Because it not only must be manipulated at first but also it is susceptible to injury and haemorrhage during dissection of the peritoneal folds that connect the hepatoduodenal ligament to Hartmann's pouch of the GB or to the CD. Ding et al. reported an incidence of 7.5% of this variation in their study.[11]
Figure 9.

Cystic artery originating from gastroduodenal artery
Vessels due to neovascularisation
In the present study, these were seen in 13 cases, cystic artery coming from below and crossing anterior to bile duct in 47 patients, seen more anteriorly than posteriorly in relation to lymph node in 22 patients and crossing the CD, initially lying laterally and then ending medial to CD, in 18 patients. These vessels need careful dissection to avoid bleeding [Table 1].
Cystic artery with late origin from right hepatic artery
Another relevant vascular anomaly has been a vessel with late origin from the right hepatic artery entering the GB at the level of cystic plate, which was observed in 11 patients. [Table 1] Although this variation is very less common, surgically important to be missed and can get injured with a torrential bleeding in the process of taking off the GB after ligating CD and artery.
Cystic artery originating from the variant right hepatic artery
This anatomic variation was found in 18 patients (3%) in the present study [Figure 10 and Table 1]. Anatomic variation of the right hepatic artery usually originates from the superior mesenteric artery or aorta. It enters Calot's triangle behind the portal vein and runs parallel to the CD on its passage through the triangle. It can be completely covered by the CD of the GB. It yields multiple small branches to supply the GB at its body, and it is often completely covered by the GB. We should be cautious of this right hepatic artery variation. From the laparoscopic viewpoint, it looks like a single large artery. Ding et al. have reported this anatomic variation in 18 patients (3%) in their study.[11]
Figure 10.
Cystic artery originating from variant right hepatic artery
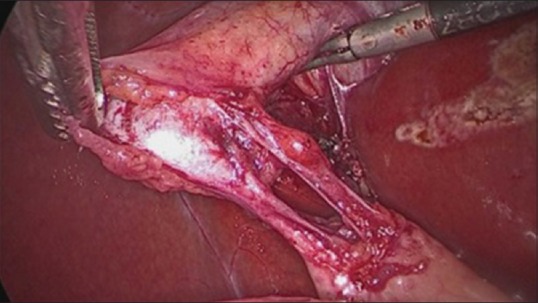
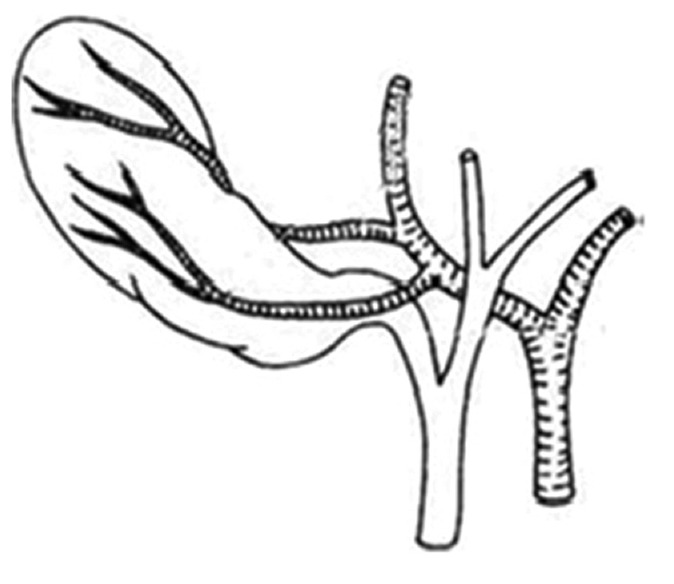
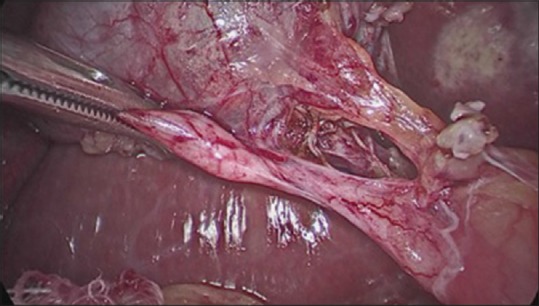
Vessel seen in posterior dissection (originating directly from the liver Parenchyma)
This variation was seen in 15 cases (2.02%). This vessel pierces the hepatic parenchyma approaching the bladder from the GB bed [Figure 11 and Table 1]. It usually situated in the right lateral border of GB body and bottom. However, a few are situated in the centre of the GB bed or situated left lateral of GB bottom. This vessel is observed during posterior dissection and is difficult to explore and requires careful dissection. Ding et al. found it in 15 patients (2.5%) in their study.[11]
Figure 11.
Vessel seen during posterior dissection
CONCLUSION
The use of laparoscopy for gallstone disease with high resolution and magnification reveals the clear anatomy of the biliary tree as compared to open cholecystectomy. Therefore, extrahepatic biliary system can easily be assessed for its anatomical variations and congenital anomalies during LC.
Introduction of LC and its unprecedented VD complications has led to newer insight into anatomy and surgeon's approach and concept of looking at this region. Congenital anomalies and anatomical variations of extrahepatic biliary tree though are not common but can be of clinical importance and surprise if present. Hence, every surgeon should assess for these anomalies during LC to prevent inadvertent ductal clipping, ductal injuries, strictures and bleeding problems. Awareness of these anomalies will decrease morbidity, conversion and re-exploration in these patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
Our thanks to all the staff of Department of Surgery and Operation Theatre. Last but not the least, we express our deep sense of obligation to all my patients who cooperated with me and silently made their invaluable contribution to the medical science.
REFERENCES
- 1.Benson EA, Page RE. A practical reappraisal of the anatomy of the extrahepatic bile ducts and arteries. Br J Surg. 1976;63:853–60. doi: 10.1002/bjs.1800631105. [DOI] [PubMed] [Google Scholar]
- 2.Suhocki PV, Meyers WC. Injury to aberrant bile ducts during cholecystectomy: A common cause of diagnostic error and treatment delay. AJR Am J Roentgenol. 1999;172:955–9. doi: 10.2214/ajr.172.4.10587128. [DOI] [PubMed] [Google Scholar]
- 3.Lamah M, Karanjia ND, Dickson GH. Anatomical variations of the extrahepatic biliary tree: Review of the world literature. Clin Anat. 2001;14:167–72. doi: 10.1002/ca.1028. [DOI] [PubMed] [Google Scholar]
- 4.Strasberg SM, Brunt LM. Rationale and use of the critical view of safety in laparoscopic cholecystectomy. J Am Coll Surg. 2010;211:132–8. doi: 10.1016/j.jamcollsurg.2010.02.053. [DOI] [PubMed] [Google Scholar]
- 5.Hand BH. Anatomy and function of the extrahepatic biliary system. Clin Gastroenterol. 1973;2:3–29. [PubMed] [Google Scholar]
- 6.Al Helli A, Al Taee M, Al Khafaji M. Laparoscopic surgical anatomy of Calot's triangle. Karbala J Med. 2011;4:1–6. [Google Scholar]
- 7.Singh K, Ohri A. Anatomic landmarks: Their usefulness in safe laparoscopic cholecystectomy. Surg Endosc. 2006;20:1754–8. doi: 10.1007/s00464-005-0528-4. [DOI] [PubMed] [Google Scholar]
- 8.Khan AH, Zaheer M. Frequency of extra hepatic biliary tree anomalies seen during cholecystectomy. Ann Pak Inst Med Sci. 2008;4:198–200. [Google Scholar]
- 9.Buddingh KT, Nieuwenhuijs VB, van Buuren L, Hulscher JB, de Jong JS, van Dam GM. Intraoperative assessment of biliary anatomy for prevention of bile duct injury: A review of current and future patient safety interventions. Surg Endosc. 2011;25:2449–61. doi: 10.1007/s00464-011-1639-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Healey, Schroy PC. Anatomy of the bile ducts within the human liver. Arch Surg. 1953;66:599–616. doi: 10.1001/archsurg.1953.01260030616008. [DOI] [PubMed] [Google Scholar]
- 11.Ding YM, Wang B, Wang WX, Wang P, Yan JS. New classification of the anatomic variations of cystic artery during laparoscopic cholecystectomy. World J Gastroenterol. 2007;13:5629–34. doi: 10.3748/wjg.v13.i42.5629. [DOI] [PMC free article] [PubMed] [Google Scholar]


