Abstract
Benign multiple sclerosis is a retrospective diagnosis based primarily on a lack of motor symptom progression. Recent findings that suggest patients with benign multiple sclerosis experience non-motor symptoms highlight the need for a more prospective means to diagnose benign multiple sclerosis early in order to help direct patient care. In this study, we present optical coherence tomography and T cell neurotrophin gene analysis findings in a small number of patients with benign multiple sclerosis. Our results demonstrated that retinal nerve fiber layer was mildly thinned, and T cells had a distinct gene expression profile that included upregulation of interleukin 10 and leukemia inhibitory factor, downregulation of interleukin 6 and neurotensin high affinity receptor 1 (a novel neurotrophin receptor). These findings add evidence for further investigation into optical coherence tomography and mRNA profiling in larger cohorts as a potential means to diagnose benign multiple sclerosis in a more prospective manner.
Keywords: neurotensin high affinity receptor 1, benign multiple sclerosis, optical coherence tomography, interleukin 10, T cell, leukemia inhibitory factor, optic neuritis, neural regeneration
Introduction
Diagnosis of benign multiple sclerosis (BMS) is a clinical challenge. BMS diagnosis is primarily retrospective and is heavily weighted towards motor progression, and in particular depends on a condition that an Expanded Disability Status Scale (EDSS) ≤ 3 after at least 10 or 15 years of disease onset without disease modifying therapy (DMT) (Ramsaransing and De Keyser, 2006; Zimmermann et al., 2013). However, recent reports have demonstrated that BMS patients experience a range of non-motor symptoms including cognitive dysfunction, pain and depression (Hviid et al., 2011; Sayao et al., 2011; Correale et al., 2012). Thus, identifying a prospective means to diagnose BMS has significant implications for treatment and patient management as these symptoms can negatively impact quality of life. Investigating the plausibility of using newer technologies to diagnose BMS represents one approach to achieve this goal.
In this study, we reported a small case series of BMS patients with their clinical course, magnetic resonance imaging (MRI), optical coherence tomography (OCT) and T cell gene expression analysis in our study. We provide evidence that OCT and mRNA profiling represent plausible technologies to pursue in larger cohorts that aim to further differentiate BMS from progressive MS.
Subjects and Methods
Subjects
The study was conducted in compliance with the principles of the Declaration of Helsinki. The University of Vermont institutional review board reviewed and approved the study protocol (approval No. CHRMS09-092). All patients provided written informed consent. Three patients with BMS were recruited from the Multiple Sclerosis Center at the University of Vermont. The diagnosis of BMS was based on an Expanded Disability Status Scale (EDSS) ≤ 3 after at least 10 or 15 years of disease onset (Ramsaransing and De Keyser, 2006). Since disease modifying therapy (DMT) use/non-use was significantly associated with maintaining a benign disease state (Zivadinov et al., 2016) and also can modulate the loss of retinal nerve fiber layer (RNFL; Button et al., 2017), we focused on patients with BMS who maintain a non-progressive benign status without prior treatment with DMT.
OCT scanning
The OCT images were obtained using the time-domain Stratus device (TD-OCT, Carl Zeiss Meditec, Dublin, CA, USA). We performed ATON study and confirmed OCT scanning competence (Sergott et al., 2015). The whole OCT scanning protocol was performed according to a previous report (Sergott et al., 2015). Only good-quality scans defined as signal strength > 8 (maximum, 10), centered optic disc, and uniform brightness were used (Cruz-Herranz et al., 2016).
T cell isolation and culture
T cell isolation, activation and culture were performed according to a previous study by Soltys et al. (2014). Briefly, peripheral blood mononuclear cells (PBMCs) were obtained from the whole blood by standard Ficoll gradient centrifugation. T cells were isolated from this cell population using a Pan T cell isolation kit (Miltenyi Biotech Inc. Auburn, CA, USA) according to manufacturer protocol. In brief, non-T cells were bound with biotin conjugated antibodies against CD14, CD16, CD19, CD36, CD56, CD123, and glycophorin A. These cells were captured with anti-biotin microbeads and magnetically depleted by passing the cells through the column (negative selection) to produce a highly pure (90–97%) population of T cells. Cell purity was confirmed by flow cytometry using human T cell receptor (TCR) staining (FITC conjugated mouse anti-human TCR standard FiPharmingen). Isolated T cells were cultured in T cell complete media (RPMI media, 10% fetal calf serum, 2.5 g/L glucose, 2 nM glutamine, 10 μg/mL folate, 1 mM pyruvate, 50 μM 2-mercaptoethanol). Cultures were stimulated with human anti-CD3 and anti-CD28 monoclonal antibodies (5 μg/106 cells) and cultured for 48 hours, at 37°C and 5% CO2. Prior to RNA extraction, all cells were collected via centrifugation and the supernatants immediately frozen at –80°C for protein analysis.
mRNA isolation
mRNA isolation and profiling were described according to previous reports (Soltys et al., 2014; Wang et al., 2015). In brief, RNA was extracted from T cells using the RNeasy RNA Extraction Kit (Qiagen). RNA quality control and integrity were assessed with an Agilent 2100 Bioanalyzer (Agilent Technologies Inc. Santa Clara, CA, USA). Absence of genomic DNA contamination was confirmed by RT-qPCR. RNA samples were reverse transcribed to cDNA using the SuperArray RT2 First Strand Kit (Invitrogen, Thermo Fisher Scientific, Waltham, MA, USA), according to manufacturer protocol.
Gene array and real time-quantitative polymerase chain reaction (RT-qPCR)
RNA (200 ng) was reversed transcribed to cDNA using the SuperArray RT-2 First-Strand cDNA synthesis kit (SA Biosciences, QIAGEN Inc., Germantown, MD, USA). cDNA samples were run on the SuperArray plate “Neurotrophins and Receptors” (PAHS-31A, SABiosciences, QIAGEN Inc., Germantown, MD, USA) using Applied Biosystems 7900HT (Applied Biosystems Inc., Foster City, CA, USA), to analyze 84 neurotrophic factors and receptors, and 5 housekeeping genes.
Results were quantified using the 2-ample method and expressed as a fold difference with respect to the healthy control group (n = 5, 4 females and 1 male, aged 33 ± 12 years, recruited from the Multiple Sclerosis Center at the University of Vermont, USA). For all analysis, a Ct cutoff of > 35 was used to define a gene as undetectable. All prepared graphs and statistical analyses were run using GraphPad® Prism software (GraphPad Software Inc.). Analysis of variance and Benjamini-Hochberg post-test were used to determine significance. The candidate genes were further confirmed by RT-qPCR using Applied Biosystems 7500 (Thermo Scientific, Grand Island, NY, USA). RT-qPCR method was described in previous studies (Soltys et al., 2014; Wang et al., 2015). Amplification consisted of 40 cycles of 95°C for 15 seconds and 60°C for 1 minute with approximately 15 ng/μL cDNA. TaqMan Master Mix and specific primer pairs for leukemia inhibitory factor (LIF) and interleukin-10 (IL-10) were purchased from Applied Biosystems (assay on demands primers) (Applied Biosystems Inc., Foster City, CA, USA). RT-qPCR was performed using Taqman® Master Mix (Applied Biosystems Inc.,) and applied Biosystems 7500 Fast Software (Applied Biosystems Inc.).
Statistical analysis
SuperArray statistical analysis was done with the PCR Data Array Web Portal provided by SABiosciences. Pairwise comparisons between groups of experimental replicates were performed. A level of P < 0.05 was considered statistically significant. Analysis of variance and Benjamini-Hochberg post-test were used to determine significance. Data were exported and all prepared graphs and statistical analyses were run using GraphPad® Prism 6 software (GraphPad Software Inc., San Diego, CA, USA).
Results
Patient #1
The case was a 68-year-old female who experienced an episode of right optic neuritis at the age of 32 years. The symptoms of optic neuritis resolved over several weeks without treatment. Twenty-one years later, she developed left-sided numbness and Lhermitte’s phenomena. MRI at that time showed non-enhancing hyperintense lesions in the deep white matter of the brain; there were no cervical spine lesions. A diagnosis of MS was given at the age of 57. Repeat MRI in 2–3 years later showed no new lesions or progression. Her symptoms improved though there was some residual numbness in her left hand, which could be brought on by heat. She began to experience depressive symptoms 5 years later including fatigue and disinterest in physical activity which responded to Escitalopram (Lexapro). Nine years after diagnosis, MRI showed one new non-enhancing hyperintense signal in the left hemisphere with no other new change or progression. She developed bladder symptoms in the 11th year after diagnosis, but the MRI showed no new additional changes (Figure 1#1).
Figure 1.
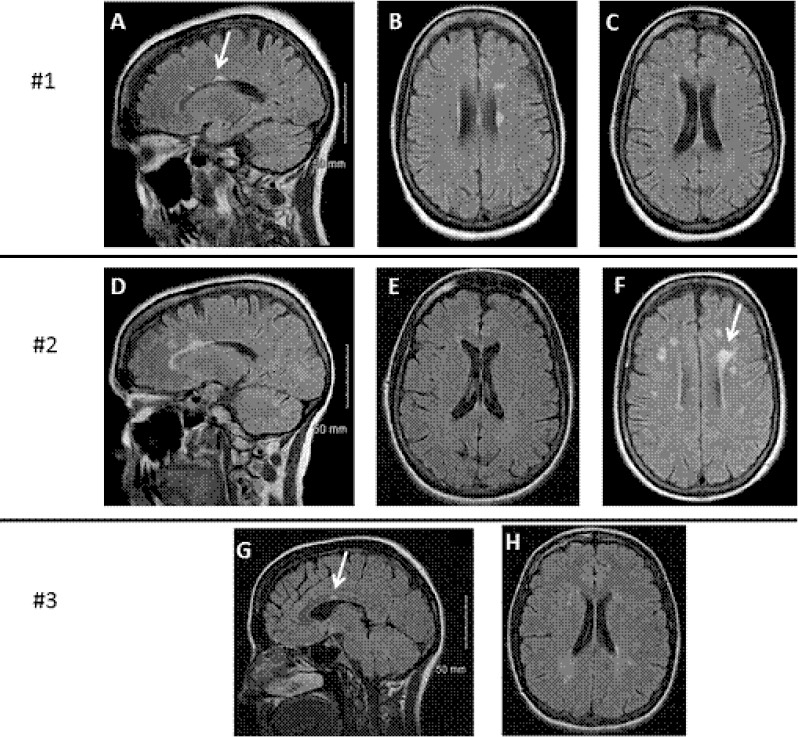
MRI findings in the brain of three patients with benign multiple sclerosis.
The most recent MRI findings of each patient are shown: Patient #1, A–C; patient #2, D–F; patient #3, G and H. Typical periventricular hyperintense signals (arrows) were seen on sagittal and axial fluid attenuation inversion recovery (FLAIR) sequences.
Patient #2
The case was a 63-year-old right-handed female. At the age of 35 years, she developed Lhermitte’s phenomena after recovering from a 2-month episode of viral myelitis. She then had bilateral trigeminal neuralgia (BTN) one year later. Her symptoms were well controlled with Carbamazepine (Tegretol). She was diagnosed with MS 3 years later at the age of 38 years. Her MRI at the diagnosis showed several hyperintense deep white matter foci in the brain without cervical spine lesions. Since the diagnosis, she has had only minor exacerbations of BTN, and the latest one was 5 years ago. Her physical exam 25 years after being diagnosed with MS showed decreased vibratory/proprioceptive sensation in both feet. Romberg was negative but she had a tendency to sway. Deep tendon reflexes were hyperactive. Repeat brain MRI at that time revealed several periventrical non-enhancing hyperintense signals (Figure 1#2). Follow-up has revealed no progression of neurologic deficit and her ambulation remains fully unrestricted.
Patient #3
The case was a 32-year-old female diagnosed with right optic neuritis at the age of 12 years. She experienced right-sided numbness for 4-5 weeks 5 years later at the age of 17 and was diagnosed with MS. The patient experienced bilateral internuclear ophthalmoplegia 7 years after diagnosis at the age of 24 years. She was treated with 3-day course of methylprednisolone (Solumedrol) but no other disease-modifying therapy (DMT). Since this episode, the patient has had no disease progression. Though she could not recall an episode of visual loss, based on her exam, she had subtle right relative afferent pupillary defect and temporal pallor in her right eye which was most likely due to past right optic neuritis. The only other bnormality was hyperreflexia in all extremities. The MRI of her brain showed two lesions in the corpus callosum, a small brain stem lesion, and a left frontal periventricular lesion (Figure 1#3).
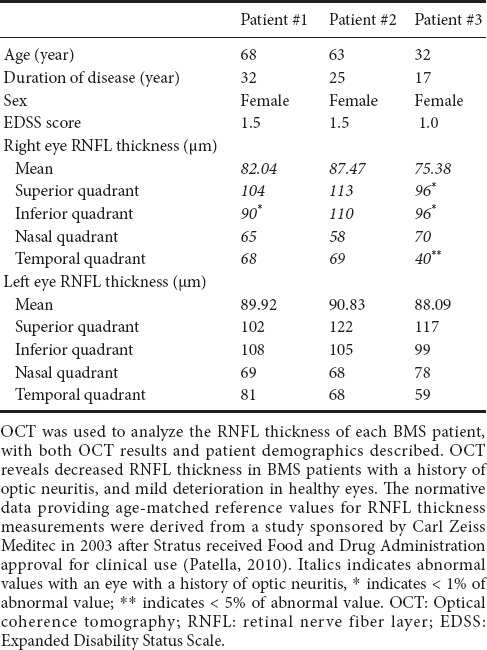
We performed OCT on each patient. Patient age, disease duration, EDSS at the time of OCT, and blood drawing (described below) are summarized in Table 1. Of note, in these patients, the EDSS was only 1.0–1.5 despite disease duration ranging from 17 to 32 years. The mean RNFL thickness was mildly decreased in the optic neuritis affected eyes while healthy non-optic neuritis eyes had relatively normal RNFL (Table 1).
Table 1.
Patient demographics and OCT data
We isolated T cells from peripheral blood samples of each patient and healthy control. T cell mRNA was extracted after 48 hours of culture with anti-CD3 and anti-CD28 antibodies. A SuperArray gene analysis using a “Neurotrophins and Receptors” plate (PAHS-31A, SABiosciences) was done to screen for potential genes of interests (Figure 2A). The fold changes were then confirmed using RT-qPCR against healthy controls (Figure 2C) (detailed methods see previous publication in Soltys et al., 2014). The mRNA levels of IL-10 and LIF were significantly increased in T cells of patients with BMS (Figure 2A).
Figure 2.
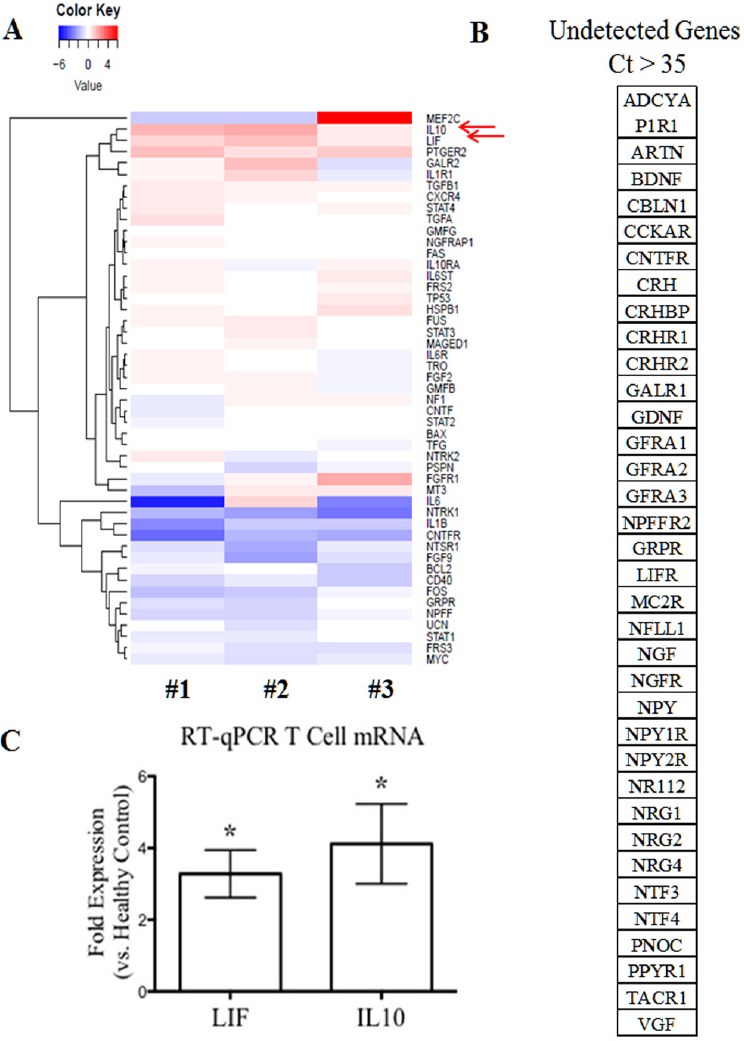
mRNA gene profiling of T cells isolated from each patient with benign multiple sclerosis.
T cells were isolated from peripheral blood mononuclear cells of each patient and cultured for 48 hours in the presence of anti-CD3/anti-CD28 antibodies. Then RNAs were extracted from T cells. “Neurotrophin and Receptor” SuperArray gene screening technology was used to screen for potential genes of interest. The results for each patient were expressed as the fold change of the specific gene as compared to healthy controls (n = 5). (A) Individual patient results with detected genes. (B) Undetected genes defined as Ct > 35. (C) The fold changes of interleukin-10 (IL-10) and leukemia inhibitory factor (LIF) were confirmed via real-time quantitative polymerase chain reaction as compared to healthy controls (n = 5). Graph showed average fold changes ± SD, *P < 0.05 (Mann-Whitney U test).
Discussion
Despite long-standing disease in our patients, there is minimal deterioration in healthy eyes. One hypothesis may be that a more benign clinical course can be predicted by a slower rate of RNFL deterioration in healthy eyes, compared to more aggressive forms of MS (Syc et al., 2012; Zimmermann et al., 2013; Galetta et al., 2015; Martinez-Lapiscina et al., 2016). Our data in Table 1 support the hypothesis that the non-ON eyes have normal values in BMS patients.
There have been reports of OCT findings in other MS presentations (Cettomai et al., 2008; Dörr et al., 2011; Saidha et al., 2011; Lange et al., 2013), including the observation that an increased thinning of RNFL correlates with disease severity in more aggressive subtypes (Oberwahrenbrock et al., 2012; Huang-Link et al., 2015). In this study, we showed that the utility of OCT might extend into and had applications in BMS as previously reported by Huang-Link et al. (2015). It is challenging to differentiate BMS from more progressive forms of MS based on clinical characteristics, neuroimaging, and cerebrospinal fluid tests. OCT allows quantification of retinal structures such as RNFL thickness to trace minor alterations and the progression of neurodegeneration. While overall neurologic impairment is mild in BMS, visual dysfunction is not well captured by the EDSS, but may account for a substantial degree of disability in BMS (Galetta et al., 2015). There is evidence that thinning of RNFL was less severe in patients with BMS than in patients with other MS in particular with secondary progressive MS (Balk et al., 2014). Despite great utility of OCT, RNFL thickness alone does not allow distinction between BMS patients and other types of MS (Balk et al., 2014).
We therefore attempted to identify molecular signatures of BMS. Recent evidence suggests that T cell-mediated inflammation may be beneficial and neuroprotective via altered neurotrophin production in MS (Correale and Villa, 2004; Soltys et al., 2014; Wang and Mao-Draayer, 2015; Johnson et al., 2016). To the best of our knowledge, the distinct neurotrophic factor/cytokine contributions from specific cell populations have not been studied in BMS. In this study, we isolated T cells, the key mediators of MS immunopathogenesis, from peripheral blood samples of three patients with benign MS. A SuperArray gene analysis was performed to screen for neurotrophin and neurtrophin receptor related genes. BMS patients demonstrate significantly elevated mRNA levels of IL-10 and LIF in T cells, which was consistent with previous studies showing that mRNA expression of IL-10 and LIF in peripheral blood mononuclear cells was elevated in patients with stable MS than in patients with active MS (Byskosh and Reder, 1996; Krakauer et al., 2008; Metcalfe et al., 2015). Furthermore, the mRNA levels of IL-6, novel neurotrophin receptor, and neurotensin high affinity receptor 1 were decreased in patients with BMS than in healthy controls. This supports our previous report that interferon-β treatment can induce the expression of anti-inflammatory cytokines and upregulate neurotensin high affinity receptor 1 in T cells (Soltys et al., 2014; Wang and Mao-Draayer, 2015). IL-6, secreted by T cells and macrophages during infection and trauma, acts mostly as pro-inflammatory cytokine in MS (Melamed et al., 2015). IL-6 together with transforming growth factor-β mediates Th17/Treg balances by promoting Th17 development and accelerating FoxP3 degradation (Kimura and Kishimoto, 2010). Therefore, decreased IL-6 in T cells from the BMS patients could be another surrogate marker for BMS. Although we cannot generalize the potential roles of these specific factors given our small sample size, our findings show that a more benign clinical course leads to a more distinct neurotrophin gene expression profile which in combination with OCT measurement could serve as biomarkers to aid the diagnosis of BMS. Further investigations with larger cohorts over time will allow us to extend our observation.
This study provides evidence that OCT and T cell neurotrophin mRNA gene expression profiling represents plausible technologies to help differentiate BMS from progressive MS. However, in this study, only three patients with benign MS were recruited. Therefore, OCT studies involving a larger cohort of patients with gene expression profile are needed to confirm our findings. Given the diverse presentations of clinical courses in BMS patients, it is likely that neither approach alone will suffice. A collaborative approach that correlates routine imaging findings (MRI, OCT) to blood and CSF biomarkers, EDSS and non-motor symptoms may best capture the range of benign clinical courses in a more prospective manner.
Additional file (31.8KB, pdf) : Open peer review report 1.
Open peer review report 1 on “Optical coherence tomography and T cell gene expression analysis in patients with benign multiple sclerosis”
Acknowledgments
We thank the Center of Biomedical Research Excellence (COBRE) at the University of Vermont for their support and equipment access, and the UVM Cancer Center DNA Analysis Facility for their assistance with our SuperArray assays. We thank our ophthalmology technician Jeffrey Abell for performing optical coherence tomography and Patricia Shea for helping with the case review.
Footnotes
Funding: This study was funded by an investigator-initiated, unrestricted research grant (to YMD) from Biogen Idec. YMD served as a consultant and/or received grant support from: Acorda, Bayer Pharmaceutical, EMD Serono, Genzyme, Novartis, Questor, Teva Neuroscience and Chugai Pharma. Dr. YMD is currently supported by grants from NIH NIAID Autoimmune Center of Excellence: UM1-AI110557; NIH NINDS R01-NS080821, Novartis and Chugai (to YMD).
Conflicts of interest: None declared.
Research ethics: The study was conducted in compliance with the principles of the Declaration of Helsinki. The University of Vermont institutional review board reviewed and approved the study protocol (approval No. CHRMS09-092).
Declaration of patient consent: The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Data sharing statement: The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Plagiarism check: Checked twice by iThenticate.
Peer review: Externally peer reviewed.
Open peer review report:
Reviewer: Chunjian Huang, National Jewish Health, USA.
Copyedited by Li CH, Song LP, Zhao M
References
- Balk L, Tewarie P, Killestein J, Polman C, Uitdehaag B, Petzold A. Disease course heterogeneity and OCT in multiple sclerosis. Mult Scler. 2014;20:1198–1206. doi: 10.1177/1352458513518626. [DOI] [PubMed] [Google Scholar]
- Button J, Al-Louzi O, Lang A, Bhargava P, Newsome SD, Frohman T, Balcer LJ, Frohman EM, Prince J, Calabresi PA, Saidha S. Disease-modifying therapies modulate retinal atrophy in multiple sclerosis: a retrospective study. Neurology. 2017;88:525–532. doi: 10.1212/WNL.0000000000003582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byskosh PV, Reder AT. Interferon beta-1b effects on cytokine mRNA in peripheral mononuclear cells in multiple sclerosis. Mult Scler. 1996;1:262–269. doi: 10.1177/135245859600100502. [DOI] [PubMed] [Google Scholar]
- Cettomai D, Pulicken M, Gordon-Lipkin E, Salter A, Frohman TC, Conger A, Zhang X, Cutter G, Balcer LJ, Frohman EM, Calabresi PA. Reproducibility of optical coherence tomography in multiple sclerosis. Arch Neurol. 2008;65:1218–1222. doi: 10.1001/archneur.65.9.1218. [DOI] [PubMed] [Google Scholar]
- Correale J, Villa A. The neuroprotective role of inflammation in nervous system injuries. J Neurol. 2004;251:1304–1316. doi: 10.1007/s00415-004-0649-z. [DOI] [PubMed] [Google Scholar]
- Correale J, Peirano I, Romano L. Benign multiple sclerosis: a new definition of this entity is needed. Mult Scler. 2012;18:210–218. doi: 10.1177/1352458511419702. [DOI] [PubMed] [Google Scholar]
- Cruz-Herranz A, Balk LJ, Oberwahrenbrock T, Saidha S, Martinez-Lapiscina EH, Lagreze WA, Schuman JS, Villoslada P, Calabresi P, Balcer L, Petzold A, Green AJ, Paul F, Brandt AU, Albrecht P. IMSVISUAL consortium (2016) The APOSTEL recommendations for reporting quantitative optical coherence tomography studies. Neurology. 86:2303–2309. doi: 10.1212/WNL.0000000000002774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dörr J, Wernecke KD, Bock M, Gaede G, Wuerfel JT, Pfueller CF, Bellmann-Strobl J, Freing A, Brandt AU, Friedemann P. Association of retinal and macular damage with brain atrophy in multiple sclerosis. PLoS One. 2011;6:e18132. doi: 10.1371/journal.pone.0018132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galetta SL, Villoslada P, Levin N, Shindler K, Ishikawa H, Parr E, Cadavid D, Balcer LJ. Acute optic neuritis: unmet clinical needs and model for new therapies. Neurol Neuroimmunol Neuroinflamm. 2015;2:e135. doi: 10.1212/NXI.0000000000000135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang-Link YM, Fredrikson M, Link H. Benign multiple sclerosis is associated with reduced thinning of the retinal nerve fiber and ganglion cell layers in non-optic-neuritis eyes. J Clin Neurol. 2015;11:241–247. doi: 10.3988/jcn.2015.11.3.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hviid LE, Healy BC, Rintell DJ, Chitnis T, Weiner HL, Glanz BI. Patient reported outcomes in benign multiple sclerosis. Mult Scler. 2011;17:876–884. doi: 10.1177/1352458511398370. [DOI] [PubMed] [Google Scholar]
- Johnson MC, Pierson ER, Spieker AJ, Nielsen AS, Posso S, Kita M, Buckner JH, Goverman JM. Distinct T cell signatures define subsets of patients with multiple sclerosis. Neurol Neuroimmunol Neuroinflamm. 2016;3:e278. doi: 10.1212/NXI.0000000000000278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimura A, Kishimoto T. IL-6: regulator of Treg/Th17 balance. Eur J Immunol. 2010;40:1830–1835. doi: 10.1002/eji.201040391. [DOI] [PubMed] [Google Scholar]
- Krakauer M, Sorensen P, Khademi M, Olsson T, Sellebjerg F. Increased IL-10 mRNA and IL-23 mRNA expression in multiple sclerosis: interferon-beta treatment increases IL-10 mRNA expression while reducing IL-23 mRNA expression. Mult Scler. 2008;14:622–630. doi: 10.1177/1352458507087136. [DOI] [PubMed] [Google Scholar]
- Lange AP, Zhu F, Sayao AL, Sadjadi R, Alkabie S, Traboulsee AL, Costello F, Tremlett H. Retinal nerve fiber layer thickness in benign multiple sclerosis. Mult Scler. 2013;19:1275–1281. doi: 10.1177/1352458512474706. [DOI] [PubMed] [Google Scholar]
- Martinez-Lapiscina EH, Arnow S, Wilson JA, Saidha S, Preiningerova JL, Oberwahrenbrock T, Brandt AU, Pablo LE, Guerrieri S, Gonzalez I, Outteryck O, Mueller AK, Albrecht P, Chan W, Lukas S, Balk LJ, Fraser C, Frederiksen JL, Resto J, Frohman T, et al. Retinal thickness measured with optical coherence tomography and risk of disability worsening in multiple sclerosis: a cohort study. Lancet Neurol. 2016;15:574–584. doi: 10.1016/S1474-4422(16)00068-5. [DOI] [PubMed] [Google Scholar]
- Melamed E, Levy M, Waters PJ, Sato DK, Bennett JL, John GR, Hooper DC, Saiz A, Bar-Or A, Kim HJ, Pandit L, Leite MI, Asgari N, Kissani N, Hintzen R, Marignier R, Jarius S, Marcelletti J, Smith TJ, Yeaman MR, et al. Update on biomarkers in neuromyelitis optica. Neurol Neuroimmunol Neuroinflamm. 2015;2:e134. doi: 10.1212/NXI.0000000000000134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metcalfe SM, Strom TB, Williams A, Fahmy TM. Multiple sclerosis and the LIF/IL-6 axis: use of nanotechnology to harness the tolerogenic and reparative properties of LIF. Nanobiomedicine. 2015;2:5. doi: 10.5772/60622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oberwahrenbrock T, Schippling S, Ringelstein M, Kaufhold F, Zimmermann H, Keser N, Young KL, Harmel J, Hartung HP, Martin R, Paul F, Aktas O, Brandt AU. Retinal damage in multiple sclerosis disease subtypes measured by high-resolution optical coherence tomography. Mult Scler Int. 2012;2012:530305. doi: 10.1155/2012/530305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patella VM. Stratus OCT: Establishment of normative reference values for retinal nerve fiber layer thickness measurements. Carl Zeiss Meditec Web site. 2010. [Accessed February 27, 2010]. Available at: http://www.meditec.zeiss.de/88256DE3007B-916B/0/55B63359D850E15D882575E7000AA4AE/$file/stratusoct5_en.pdf .
- Ramsaransing GS, De Keyser J. Benign course in multiple sclerosis: a review. Acta Neurol Scand. 2006;113:359–369. doi: 10.1111/j.1600-0404.2006.00637.x. [DOI] [PubMed] [Google Scholar]
- Saidha S, Syc SB, Durbin MK, Eckstein C, Oakley JD, Meyer SA, Conger A, Frohman TC, Newsome S, Ratchford JN, Frohman EM, Calabresi PA. Visual dysfunction in multiple sclerosis correlates better with optical coherence tomography derived estimates of macular ganglion cell layer thickness than peripapillary retinal nerve fiber layer thickness. Mult Scler. 2011;17:1449–1463. doi: 10.1177/1352458511418630. [DOI] [PubMed] [Google Scholar]
- Sayao AL, Bueno AM, Devonshire V, Tremlett H. The psychosocial and cognitive impact of longstanding ‘benign’ multiple sclerosis. Mult Scler. 2011;17:1375–1383. doi: 10.1177/1352458511410343. [DOI] [PubMed] [Google Scholar]
- Sergott RC, Bennett JL, Rieckmann P, Montalban X, Mikol D, Freudensprung U, Plitz T, van Beek J ATON Trial Group. ATON: results from a Phase II randomized trial of the B-cell-targeting agent atacicept in patients with optic neuritis. J Neurol Sci. 2015;351(1-2):174–178. doi: 10.1016/j.jns.2015.02.019. [DOI] [PubMed] [Google Scholar]
- Soltys J, Knight J, Scharf E, Pitt D, Mao-Draayer Y. IFN-β alters neurotrophic factor expression in T cells isolated from multiple sclerosis patients - implication of novel neurotensin/NTSR1 pathway in neuroprotection. Am J Transl Res. 2014;6:312–319. [PMC free article] [PubMed] [Google Scholar]
- Syc SB, Saidha S, Newsome SD, Ratchford JN, Levy M, Ford E, Crainiceanu CM, Durbin MK, Oakley JD, Meyer SA, Frohman EM, Calabresi PA. Optical coherence tomography segmentation reveals ganglion cell layer pathology after optic neuritis. Brain. 2012;135(Pt 2):521–533. doi: 10.1093/brain/awr264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q, Chuikov S, Taitano S, Wu Q, Rastogi A, Tuck SJ, Corey JM, Lundy SK, and Mao-Draayer Y. Dimethyl fumarate protects neural stem/progenitor cells and neurons from oxidative damage through Nrf2-ERK1/2 MAPK pathway. Int J Mol Sci. 2015;16:13885–13907. doi: 10.3390/ijms160613885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q, Mao-Draayer Y. Neuroprotective effect of IFN-β treatment is involved in neurotrophic factors and novel NT/NTSR1 pathway. Neural Regen Res. 2015;10:1932–1933. doi: 10.4103/1673-5374.169636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmermann H, Freing A, Kaufhold F, Gaede G, Bohn E, Bock M, Oberwahrenbrock T, Young KL, Dörr J, Wuerfel JT, Schippling S, Paul F, Brandt AU. Optic neuritis interferes with optical coherence tomography and magnetic resonance imaging correlations. Mult Scler. 2013;19:443–150. doi: 10.1177/1352458512457844. [DOI] [PubMed] [Google Scholar]
- Zivadinov R, Cookfair DL, Krupp L, Miller AE, Lava N, Coyle PK, Goodman AD, Jubelt B, Lenihan M, Herbert J, Gottesman M, Snyder DH, Apatoff BR, Teter BE, Perel AB, Munschauer F, Weinstock-Guttman B. Factors associated with benign multiple sclerosis in the New York State MS Consortium (NYSMSC) BMC Neurol. 2016;16:102. doi: 10.1186/s12883-016-0623-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Open peer review report 1 on “Optical coherence tomography and T cell gene expression analysis in patients with benign multiple sclerosis”


