Abstract
Background:
A number of techniques are available for performing biceps tenodesis, the majority of which result in good or excellent outcomes. However, failure may result in pain and/or dissatisfying biceps deformity.
Purpose:
To compare the clinical failure rates of 2 methods of suture passage in subpectoral biceps tenodesis with suture anchors performed by the senior author.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
A retrospective chart review was conducted of patients who underwent biceps tenodesis under the care of the senior author. Operative notes were used to determine whether the procedure was performed with a BirdBeak (BB) suture passer or a free needle (FN). Each subsequent clinical follow-up note was used to determine participation in physical therapy and duration, follow-up duration, and whether clinical tenodesis failure had occurred. Biceps tenodesis failure was defined as either cosmetic deformity (“Popeye” sign), pain at the tenodesis site, or need for revision.
Results:
Overall, 163 patients met the inclusion criteria (BB, n = 112; FN, n = 51). Mean follow-up was 5.3 months and 4.1 months in the BB and FN groups, respectively. Significantly more tenodesis failures occurred in the BB group (BB, 12%; FN, 2%, P = .042). Among all BB patients, 10% experienced failure due to cosmetic deformity, 2% required revision, and 4% had postoperative pain at the tenodesis site by latest follow-up. The 1 patient in the FN group who experienced failure presented with cosmetic deformity postoperatively.
Conclusion:
Biceps tenodesis with the use of an FN to pass the suture resulted in a significantly lower clinical failure rate compared with the use of a BB suture passer.
Keywords: biceps, tenodesis, Popeye sign
The long head of the biceps (LHB) tendon may be affected by numerous pathologic processes that result in anterior shoulder pain, including tendinosis, partial tearing, complete rupture, subluxation, and dislocation.2 Biceps tenodesis is a procedure that involves detachment of the associated LHB from the supraglenoid tubercle and reattachment to a more distal location along the proximal humerus.2 This procedure has been performed in either an open, mini-open, or arthroscopic fashion.10 Partial tearing of the LHB and instability of the LHB are the most common indications for biceps tenodesis,2 although it is additionally now accepted as a safe and effective treatment for failed arthroscopic repair of superior labral anterior-posterior (SLAP) tears in an older athletic population.6 Thus, the number of biceps tenodesis procedures performed in the United States has increased in recent years.10,11
Excellent or good outcomes have been reported in 74% of biceps tenodesis cases overall and in 63% to 93% of cases in the setting of rotator cuff repair.9 However, failure of this procedure may result in pain or a cosmetic deformity known as the “Popeye” sign due to visible bulging of the biceps muscle at the distal humerus.9 For some patients, this deformity is dissatisfying and may warrant a revision procedure. The purpose of this study was to compare failure rates of 2 suture passage methods used during mini-open subpectoral biceps tenodesis performed by the senior author (J.T.B.). The authors hypothesized that biceps tenodesis using a free needle (FN) to pass suture through the LHB tendon would result in a significantly lower clinical failure rate compared with tenodesis using a BirdBeak (BB) suture passer (Arthrex Inc).
Methods
A retrospective chart review was conducted of patients who underwent biceps tenodesis under the care of the senior author (J.T.B.) from January 1, 2010, to May 23, 2016. Patients ages 18 to 89 years were approved to be included in this study; patients who underwent biceps tenodesis in the setting of shoulder arthroplasty were excluded. Operative notes were used to determine whether the biceps tenodesis procedure was performed with a BB suture passer or an FN technique. The senior surgeon had switched from BB to an FN approach in February 2015 due to concerns of a high failure rate when using the BB suture passer. Demographic data such as date of birth, sex, and arm dominance, as well as preoperative diagnosis/indications and concomitant procedures, were recorded. Clinical follow-up notes were used to determine physical therapy use and duration, follow-up duration, and tenodesis failure. Biceps tenodesis failure was defined as observation of biceps deformity, pain at the tenodesis site, a complete biceps tear, or need for revision at most recent follow-up visit. Minor biceps asymmetry was not considered a tenodesis failure.
Surgical Technique
Following diagnostic arthroscopy, a small anterior axillary fold incision was made at the inferior border of the pectoralis major tendon. This incision was approximately 3 cm in length and was carried down sharply through the skin and subcutaneous tissue. The pectoralis major was elevated superiorly, and subpectoral dissection was carried out to reveal the LHB tendon and bicipital groove. The groove was prepared, and a 1.9-mm SutureFix double-loaded suture anchor (Smith & Nephew) was placed. Then, either a 2.75-mm tip BB suture passer or a 1.09-mm taper FN was used to pass a Cobraid No. 2 suture through the tendon. When BB was used, the suture was passed in a “lasso loop” type configuration as described by Lafosse et al,5 with an additional locking Krackow stitch more proximal (Figure 1). With FN, a modified lasso loop or cow-hitch type suture configuration with an adjacent locking Krackow stitch was used (Figure 2). This method was used for both of the sutures in each double-loaded anchor. The other limb of each suture was passed in simple fashion, which allowed the suture to slide in the anchor, reducing the tendon to the anchor site when tied. Each strand was then tied, securing the tendon to the base of the bicipital groove in its anatomic resting tension. Importantly, the above steps were performed before the biceps was released from the supraglenoid tubercle, such that anatomic resting tension of the biceps was maintained at the time of tenodesis. The more proximal portion of the tendon was then clamped and cut (Figure 3). Another arthroscopic view was obtained, and the biceps was cut from the supraglenoid tubercle, with the cut portion of the biceps tendon removed from the inferior tenodesis wound.
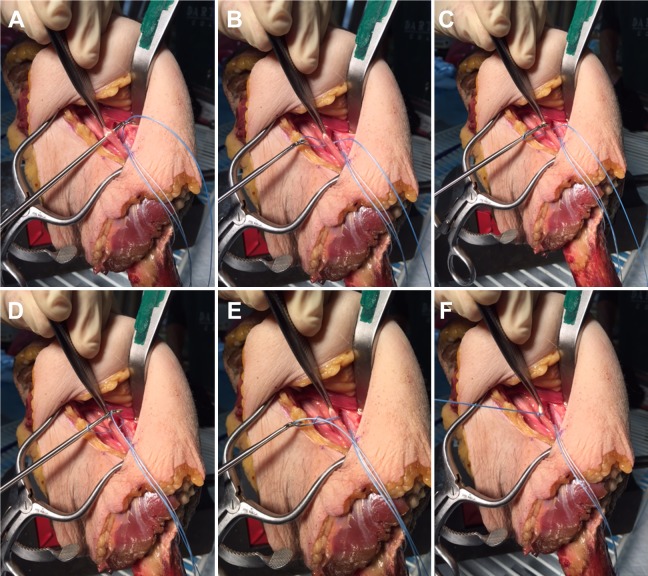
Figure 1.
BirdBeak (BB) suture passage technique. (A) Following suture anchor placement, the suture passer is brought through the long head of the biceps tendon, and (B) 1 suture is pulled through the tendon. (C) The BB is then passed through the loop, and (D-F) a second suture is then pulled through the loop to create a “lasso loop” configuration.
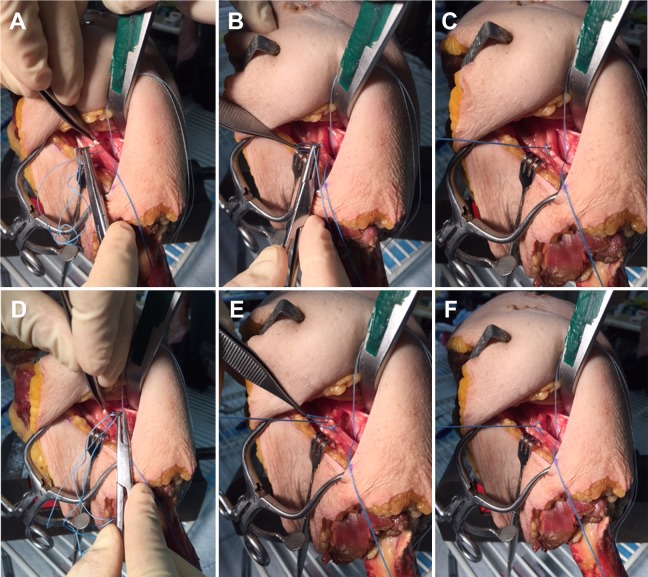
Figure 2.
Free needle (FN) suture passage technique. (A) An FN is placed through the long head of the biceps tendon. (B, C) The needle is then brought through the created loop and tied down. (D-F) The needle is brought deep to the tendon, out of the second created loop, and tied down to complete the cow-hitch configuration with an adjacent locking Krackow stitch.
Figure 3.
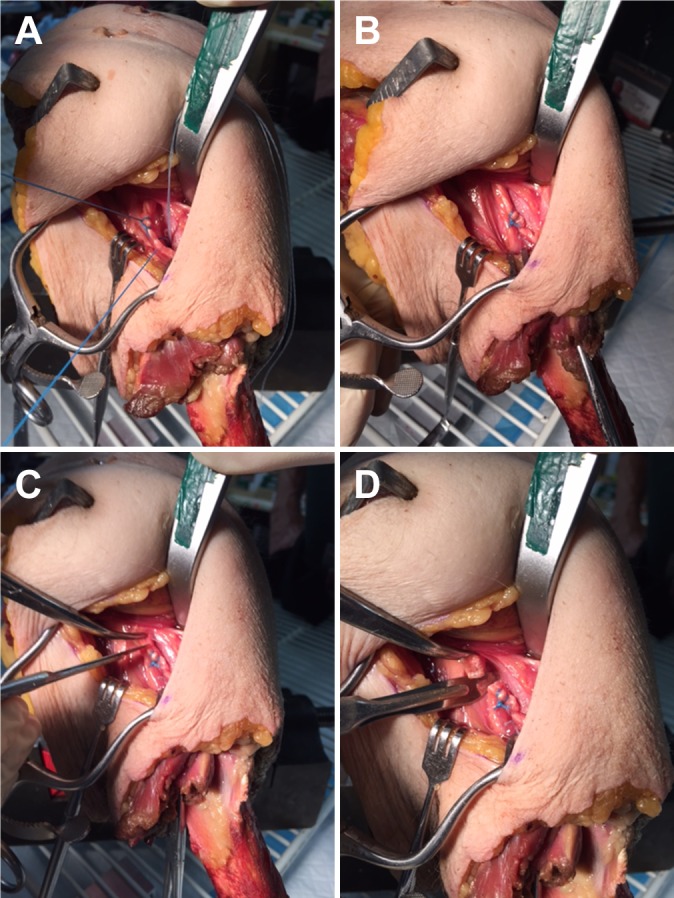
Final steps of biceps tenodesis procedure. (A) Regardless of technique, after both sutures are tied, the other limb of each suture is passed in simple fashion, which allows the suture to slide in the anchor, reducing the tendon to the anchor site. (B) Each strand is then tied, securing the tendon to the base of the bicipital groove in its anatomic resting tension. (C, D) The more proximal portion of the tendon is then clamped and cut.
Postoperative Rehabilitation
Postoperative rehabilitation consisted of sling immobilization in all cases for 4 weeks in the setting of isolated biceps tenodesis and for 6 weeks if concomitant rotator cuff repair was performed. A standardized rehabilitation protocol was used for all patients; gentle immediate passive range of motion was allowed, and a 5-lb lifting restriction of elbow flexion was in place for 6 weeks. Patients then progressed to active-assist range of motion and active resumption of activities at 6 weeks; return to full, unrestricted activity typically was allowed at a minimum of 12 weeks based on each patient's individual progress with physical therapy.
Follow-up Clinical Examinations
Clinical failure of biceps tenodesis was assessed at each clinical follow-up, clearly noted in the senior surgeon’s clinical documentation. Failure was indicated by cosmetic deformity, pain at the tenodesis site, or need for revision. If cosmetic deformity or pain had not resolved by the final follow-up, or if it was determined that the patient would require revision surgery, the tenodesis was determined to be a clinical failure.
Statistical Analysis
Chi-square statistical tests were used to determine significant differences in procedure side, preoperative diagnosis/indications, concomitant procedures, and failure rate between the 2 techniques. A Student t test was used to determine significant differences in mean age, therapy duration, and follow-up duration between the groups.
Results
A total of 163 patients met the inclusion and exclusion criteria for this study (BB: 112, FN: 51) (Table 1). Mean ± SD follow-up was significantly different between the 2 groups (BB, 5.3 ± 3.2 months; FN, 4.1 ± 2.5 months; P = .02). Every patient in both groups underwent either formal or home physical therapy, with no difference in physical therapy duration between groups (BB, 3.7 ± 2.6 months; FN, 4.2 ± 2.8 months; P = .27).
TABLE 1.
Demographic and Outcome Comparisons of 2 Biceps Tenodesis Techniquesa
| BirdBeak (n = 112) | Free Needle (n = 51) | P Value | |
|---|---|---|---|
| Age, y | 51 ± 13 | 48 ± 14 | .18 |
| Right side, % | 63 | 69 | .52 |
| Therapy duration, mo | 3.7 ± 2.6 | 4.2 ± 2.8 | .27 |
| Follow-up, mo | 5.3 ± 3.2 | 4.1 ± 2.5 | .02 |
| Concomitant preoperative diagnosis, % | |||
| Acromioclavicular arthrosis | 60 | 65 | .55 |
| Rotator cuff tear | 67 | 51 | .051 |
| Labral tear | 15 | 16 | .93 |
| Concomitant procedures, % | |||
| Rotator cuff repair | 40 | 37 | .72 |
| Debridement | 49 | 20 | <.001 |
| Distal clavicle resection | 48 | 57 | .31 |
| Subacromial decompression, bursectomy, acromioplasty | 70 | 61 | .27 |
| Overall failure rate, % | 12 | 2 | .042 |
| Deformity | 10 | 2 | <.0001 |
| Need for revision | 2 | 0 | .34 |
| Pain at tenodesis site | 4 | 0 | .13 |
aContinuous variables are presented as a mean ± SD. Bolded P values indicate statistically significant between-group difference (P < .05).
A significantly higher failure rate was found in the BB group compared with the FN group (12% vs 2%, P = .042). Cosmetic deformity was significantly higher in the BB group compared with the FN group (10% and 2%, respectively; P < .0001). Among BB patients, 2% needed biceps tenodesis revision surgery and 4% had pain at the tenodesis site, although this was not significantly higher than in FN patients (0% for both) (P = .34 and P = .13, respectively). The mean ± SD age of patients who experienced failure was 56 ± 11 years in the BB group and 53 ± 0 years in the FN group (P = .79). No postoperative infections or neurologic complications were observed in either group.
The primary diagnoses in the 1 FN failure were biceps tendinitis, labral tear, acromioclavicular arthrosis, and degenerative joint disease. Among patients in the BB group who experienced failure, 85% were diagnosed with biceps tendinitis, 77% with acromioclavicular arthrosis, 69% with rotator cuff tear, 23% with a labral tear, and 23% with a biceps tendon tear. Subacromial bursitis and degenerative joint disease each accounted for 15% of primary diagnoses among BB failures. One patient in the BB group had a loose body in the bicipital groove.
Among all patients, in addition to biceps tendinitis, the 3 most common concomitant preoperative diagnoses were acromioclavicular arthrosis, rotator cuff tear, and labral tear. The 4 most common concomitant procedures were rotator cuff repair, glenohumeral debridement (biceps stump, degenerative SLAP tear, etc), distal clavicle excision, and subacromial decompression with or without acromioplasty. Three subscapularis repairs were performed in the BB group, and none in the FN group. Arthroscopic debridement was performed in a significantly higher proportion of patients in the BB group. Otherwise, no significant differences were found between groups with regard to preoperative diagnosis or concomitant procedures.
Discussion
The results of the present study suggest that subpectoral mini-open biceps tenodesis results in a significantly lower clinical failure rate when performed with an FN suture passage technique compared with a BB suture passer. Furthermore, tenodesis with an FN results in a significantly lower rate of cosmetic deformity.
Biceps tenodesis is a common procedure performed for various pathologic conditions of the LHB tendon, including tendinosis, tenosynovitis, partial tearing, complete rupture, subluxation, dislocation, and SLAP tear.2 Failure of this procedure may result in a cosmetic deformity known as the “Popeye” sign due to bulging of the biceps muscle at the distal humerus. Based on a systematic review, Slenker et al9 demonstrated that biceps tenodesis results in an 8% rate of cosmetic deformity, compared with a 43% occurrence following biceps tenotomy (detachment of the biceps tendon origin without reattachment on the proximal humerus). Although the rate of cosmetic deformity occurrence is significantly lower after biceps tenodesis, this complication is dissatisfying for many patients, may produce biceps muscle belly cramping and supination weakness, and may warrant a revision procedure. Although bicipital pain may also result following biceps tenodesis/tenotomy, Slenker et al9 showed no significant difference in this outcome between the 2 procedures (tenodesis 24%, tenotomy 19%).
The complication rate of biceps tenodesis when an FN was used in this study was similar to that reported in other studies. Recently, Park et al8 performed a randomized controlled trial comparing outcomes of biceps tenodesis with interference screw (n = 33) versus suture anchor (n = 34) fixation. At a minimum 2-year follow-up, patient-reported outcomes had improved significantly in both groups, with no significant difference between groups. Tenodesis failures occurred in 7 interference screw patients and 2 suture anchor patients (P = .083). Multivariate logistic regression analysis showed that interference screw fixation was significantly associated with tenodesis failure (P = .003).
Nho et al7 reported on 353 patients undergoing subpectoral biceps tenodesis with interference screw fixation, with an overall complication rate of 2.0%. The most common complications were persistent bicipital pain (n = 2) and Popeye deformity due to failure of fixation (n = 2). In a case series of 102 patients undergoing open subpectoral biceps tenodesis with Krackow suture fixation for all causes of biceps tendon pathology, Kane et al4 described 3 postoperative complications due to the tenodesis procedure: 1 case of persistent bicipital groove pain, 1 infection at the tenodesis site requiring irrigation and debridement, and 1 case of cosmetic deformity resulting from loss of fixation. In a cohort study comparing all-arthroscopic suprapectoral versus open subpectoral biceps tenodesis using interference screw fixation, Gombera et al3 evaluated 23 patients in each group at a mean follow-up of 30.1 months. In the open biceps tenodesis group, 2 postoperative complications (8.7%) were reported, including 1 case of superficial erythema and 1 case of brachial plexopathy. Both complications resolved by final follow-up. Each of these studies describes various knot-tying techniques to secure the proximal LHB tendon, although none refers to the use of a BB suture passer. Finally, as mentioned above, Slenker et al9 performed a systematic review of biceps tenodesis versus tenotomy and found an 8% rate of cosmetic deformity following tenodesis.
To our knowledge, no published study has compared rates of clinical failure or complications following biceps tenodesis with a BB suture passer versus an FN. The higher rate of failure found in this study with the use of a BB may be related to less mechanical control over the site of suture passage through the biceps tendon. With more mechanical control using an FN, the surgeon can more accurately place the suture through the center of the tendon, thereby reducing the risk of postoperative failure due to suture cutting through the tendon. Additionally, the hole created with the FN (1.09-mm taper) is smaller than that of the BB (2.75-mm tip), which may have an effect on pull-out strength of the suture and ultimate failure observed. This has been examined previously with regard to rotator cuff repair.1 Based on a cadaveric study, Chokshi et al1 found that devices that create larger holes in the rotator cuff tendon, such as the BB and the Viper (Arthrex Inc), result in failure at lower forces of cyclic loading compared with devices that have smoother tips and thereby create smaller holes (No. 7 tapered Mayo needle; SutureLasso, Arthrex Inc). This same phenomenon likely applies to biceps tenodesis failure as well.
Additionally, to our knowledge, this is the first series in the available literature that reports biceps tenodesis outcomes in the setting of the particular sequence of the tenodesis procedure used in this series. In this cohort, tenodesis was performed and the tendon secured at its anatomic resting tension before the biceps root was released from the supraglenoid tubercle. We believe this helps to avoid any guesswork with regard to appropriate tensioning of the biceps during tenodesis and indeed may be at least partially responsible for the low rates of failure reported (specifically with regard to cosmetic deformity) when compared with other historical cohorts.
The strengths of this study include a large sample size over a 6-year duration. In addition, all procedures were performed by the senior surgeon (J.T.B.), thereby minimizing surgeon variability in surgical technique. The limitations of this study should also be noted. In particular, selection bias was involved in this study, as the senior author noted a high failure rate of biceps tenodesis with use of the BB and thus changed his technique to the use of an FN. In relation to this, surgeon technical improvement over time is an additional limitation, as all of the FN procedures were performed after the BB procedures. The lack of reported validated outcome scores in this cohort limits our ability to evaluate whether the differences observed between suture techniques have an effect on subjective outcomes. Another limitation is that cosmetic deformity does not always result in poor outcomes or poor patient satisfaction, although all nonminor deformities were counted as failures in this study. In addition, a significantly longer follow-up time occurred for patients undergoing biceps tenodesis with a BB suture passer. However, this is unlikely to be clinically significant (1.2-month difference on average) and is believed to represent an evolution of the surgical practice, where patients were typically released from routine care once they returned to full activity rather than being asked to return for a routine 6-month postoperative visit. However, it is unknown whether the difference in follow-up time between groups could additionally be explained by the BB cohort having a slightly higher rate of cosmetic deformity, pain at the tenodesis site, and need for revision, thereby necessitating longer clinical follow-up. Furthermore, data analysis was performed retrospectively, which may have created bias. Finally, detailed information about the biceps injury of each patient, such as the percentage of biceps tears or the types of biceps dislocation, was unavailable.
Conclusion
In this study, mini-open subpectoral biceps tenodesis with the use of an FN to pass suture through the LHB tendon resulted in a significantly lower clinical failure rate (as defined by cosmetic deformity, pain at the tenodesis site, or need for revision) compared with the use of a BB suture passer.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: J.T.B. is a paid consultant for DJ Orthopaedics and Smith & Nephew; receives financial/material support from Mitek, Smith & Nephew, and Stryker; receives royalties from Shukla Medical; is an unpaid consultant for Shukla Medical; and receives research support from Stryker.
Ethical approval for this study was obtained from the Colorado Multiple Institutional Review Board (protocol No. 16-0063).
References
- 1. Chokshi BV, Kubiak EN, Jazrawi LM, et al. The effect of arthroscopic suture passing instruments on rotator cuff damage and repair strength. Bull Hosp Jt Dis. 2006;63(3-4):123–125. [PubMed] [Google Scholar]
- 2. Creech MJ, Yeung M, Denkers M, Simunovic N, Athwal GS, Ayeni OR. Surgical indications for long head biceps tenodesis: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2016;24(7):2156–2166. [DOI] [PubMed] [Google Scholar]
- 3. Gombera MM, Kahlenberg CA, Nair R, Saltzman MD, Terry MA. All-arthroscopic suprapectoral versus open subpectoral tenodesis of the long head of the biceps brachii. Am J Sports Med. 2015;43(5):1077–1083. [DOI] [PubMed] [Google Scholar]
- 4. Kane P, Hsaio P, Tucker B, Freedman KB. Open subpectoral biceps tenodesis: reliable treatment for all biceps tendon pathology. Orthopedics. 2015;38(1):37–41. [DOI] [PubMed] [Google Scholar]
- 5. Lafosse L, Van Raebroeckx A, Brzoska R. A new technique to improve tissue grip: “the lasso-loop stitch.” Arthroscopy. 2006;22(11):1246.e1-3. [DOI] [PubMed] [Google Scholar]
- 6. McCormick F, Nwachukwu BU, Solomon D, et al. The efficacy of biceps tenodesis in the treatment of failed superior labral anterior posterior repairs. Am J Sports Med. 2014;42(4):820–825. [DOI] [PubMed] [Google Scholar]
- 7. Nho SJ, Reiff SN, Verma NN, Slabaugh MA, Mazzocca AD, Romeo AA. Complications associated with subpectoral biceps tenodesis: low rates of incidence following surgery. J Shoulder Elbow Surg. 2010;19(5):764–768. [DOI] [PubMed] [Google Scholar]
- 8. Park JS, Kim SH, Jung HJ, Lee YH, Oh JH. A prospective randomized study comparing the interference screw and suture anchor techniques for biceps tenodesis. Am J Sports Med. 2017;45(2):440–448. [DOI] [PubMed] [Google Scholar]
- 9. Slenker NR, Lawson K, Ciccotti MG, Dodson CC, Cohen SB. Biceps tenotomy versus tenodesis: clinical outcomes. Arthroscopy. 2012;28(4):576–582. [DOI] [PubMed] [Google Scholar]
- 10. Vellios EE, Nazemi AK, Yeranosian MG, et al. Demographic trends in arthroscopic and open biceps tenodesis across the United States. J Shoulder Elbow Surg. 2015;24(10):e279–e285. [DOI] [PubMed] [Google Scholar]
- 11. Werner BC, Brockmeier SF, Gwathmey FW. Trends in long head biceps tenodesis. Am J Sports Med. 2015;43(3):570–578. [DOI] [PubMed] [Google Scholar]