Abstract
Sections of paraffin embedded tissues are routinely used for studying tissue histology and histopathology. However, it is difficult to determine what the three-dimensional tissue morphology is from such sections. In addition, the sections of tissues examined may not contain the region within the tissue that is necessary for the purpose of the ongoing study. This latter limitation hinders histopathological studies of blood vessels since vascular lesions develop in a focalized manner. This requires a method that enables us to survey a wide area of the blood vessel wall, from its surface to deeper regions. A whole mount en face preparation of blood vessels fulfills this requirement. In this article, we will demonstrate how to make en face preparations of the mouse aorta and carotid artery and to immunofluorescently stain them for confocal microscopy and other types of fluorescence-based imaging.
Keywords: Basic Protocol, Issue 123, Aorta, carotid artery, endothelial cells, en face immunofluorescence preparation
Introduction
For histopathological studies by light microscopy, three dimensional pieces of biological tissues are routinely processed for paraffin embedment followed by sectioning and staining. A tissue sample that has been paraffin-embedded may be several millimeters in all three dimensions. However, for the purpose of light microscopy, it must be first sectioned so that light can pass through and then stained so that the thin section yields enough contrast for imaging. Because sectioned specimens are usually 5-10 µm in thickness, one sees only a very small fraction of the whole specimen in two dimensions at a time. It is possible to collect sequential sections and, after imaging each section individually, perform computer-assisted reconstruction of the 3D images, but this is a tedious job indeed. Histopathology of blood vessels, especially for studying the pathogenesis of atherosclerosis, presents unique problems. Atherosclerosis is a focalized disease that develops locally in areas where disturbed blood flow occurs. Furthermore, the disease is initiated within the intima, a thin tissue consisting of a monolayer of endothelial cells and extracellular matrix, of large arteries. For these reasons, it is a challenge to locate and study early lesions using sectioned blood vessels because one can easily miss sectioning the lesion. Even if a section does include a diseased area, one will see only a 5-10 µm portion containing endothelial cells and other vascular wall cells in the media and adventitia.
Whole mount en face (pronounced än ˈfäs) preparations allow us to survey a wide area of the blood vessel surface such as the entire aorta from the aortic root all the way down to the common iliac arteries. Using such a specimen stained with specific antibodies and other specific probes, one can pinpoint the location of lesions and also where various molecular events occur in endothelial cells in conjunction with atherogenesis such as changes in the expression, localization, and posttranslational modifications of proteins. In addition to studying atherogenesis, the endothelial cell shape observed in en face preparations is used as an indicator of the regional time-averaged blood flow pattern. Such data are important for studying mechanosignaling of endothelial cells in situ. For this purpose, routine histological cross-sectioned blood vessels are not useful. Thus, for vascular medicine and biology, it is especially important to acquire a technique for making en face preparations of blood vessels that allows one to observe a wide area of the vessel surface as well as the deeper subsurface areas of the vessel.
As reviewed by Jelev and Surchev1, vascular biologists have developed various methods to observe the lining of blood vessels en face. Some ingenious methods were developed in the 1940's and 1950's. Using these methods, they were able to study the fundamental organization of endothelial cells that line the inner surface of blood vessels. However, because of the way these en face preparations are prepared (the so-called Hautchen method2,3,4 or peeling off of the vessel surface5) and the way the specimen was stained, it was not always possible to obtain uninterrupted morphological information from the vessel surface into the deeper areas of the blood vessel wall. Whole mount en face vessel preparation combined with immunofluorescence staining allowed us to not only study endothelial cell morphology and protein expression and localization in these cells, but also to extend such studies to the subendothelial region of the vessel wall. Early studies using blood vessel en face preparations stained immunoflurescently began to appear in the 1980's6,7. With the advent of laser scanning confocal microscopy and more recently multiphoton microscopy, one can now obtain clear in-focus images of the blood vessel wall structure in immunofluorescently stained en face vessel samples as well as the vascular network in live animals8,9,10,11. These computer-based imaging techniques create in-focus optical sectioned images, and by stacking up such images, one can obtain reconstructed 3D images of the vessel wall and the vascular network in tissues. In addition, one can generate images of a section made along the Z-axis of the reconstructed image12,13.
In this article, we will illustrate a method for preparing en face preparations of the mouse aorta and the carotid artery for immunofluorescent staining. En face preparations can be made even after these vessels have been experimentally manipulated. For example, a carotid artery may be partially ligated and then an en face preparation made after such a surgery. For this reason, we will also describe in this article how we do a partial ligation on the carotid artery. Compared with making similar preparations from larger animals such as rats, rabbits, and humans, mouse vessels are small in size and more fragile, thus requiring added care for handling during surgical isolation of vessels and preparing them for antibody staining and microscopy. Because the most commonly used animal model for genetic modification is the mouse, it becomes critical for many investigators to handle mouse vessels without damaging them. In this manuscript, we will describe how to handle mouse blood vessels when making en face preparations of the mouse aorta and carotid artery. For the purpose of demonstration, we will use wild type C57/b6 mice.
Protocol
The protocols for the mouse partial carotid artery ligation and isolation of the mouse aorta and carotid artery for en face immunostaining are approved by the Institutional Animal Care and Use Committee (IBT 2014-9231).
1. Left Partial Carotid Artery Ligation
Prepare the surgical space by placing a 12 inch x 14 inch heating pad on the table and cover the pad and table top with a large clean surgical drape. Adjust the arm of the boom stand so that the stereomicroscope's field of view is in the center area of the heating pad.
- Turn on the heating pad on the table and set the 3-setting control dial to the medium heat level. At this temperature setting, the surgical board surface (see 1.6.1) will be 38-40 °C.
- Place a clean cage on another heating pad. Turn the heating pad on as above. This cage will be used for recovery after surgery (see 1.16) as well as housing.
On the surgical table, place an autoclaved sterilization pouch containing iris scissors (1 pair), tissue forceps (1 pair), super grip forceps (2 pairs), spring scissors (1 pair), blunt retractor (1 pair; 2.5 mm wide), round handled needle holder (1), sterilized 6-0 silk suture, cotton tipped applicators, mini cotton tipped applicators, surgical drapes, and 2" x 2" gauze sponges. Also place a squeeze bottle containing 70% ethanol and another containing chlorhexidine surgical scrubon the surgical table.
Weigh a mouse. The body weight is needed to determine the appropriate amount of analgesia, which will be administered immediately before surgery.
Place a mouse into the induction chamber.
- Turn on the oxygen tank and the anesthetic vaporizer in order to anesthetize the mouse in the induction chamber. Maintain the isoflurane level at 2%. It takes 3-5 min before the mouse stops moving.
- While the mouse is being anesthetized, place a smaller piece of sterile surgical drape (24 inch x 24 inch) under the stereomicroscope to create a surgical surface. Then place an acrylic surgical board (which has been cleaned with 70% alcohol) on the draped surface. The surgical board should therefore be on the heating pad but separated by two layers of surgical drapes.
When the mouse stops moving in the induction chamber, transfer the mouse to a pre-surgical preparation area and position its nose into the nose-cone connected to the vaporizer (2% isoflurane). Remove the hair around the cervical area using an electric trimmer or hair remover lotion. We recommend hair removing lotion because this method will not produce loose hair pieces, which are difficult to completely remove from the surgical area.
- With the nose-cone in place, move the mouse to the surgical board.
- Tape down the right and left fore-paws to the surgical board. Tape down both hind legs together on the right side of the mouse. This causes a slight rotation of the mouse body such that the left side of the neck area of the mouse becomes better positioned for surgery.
Disinfect the incision area with 70% alcohol, chlorhexidine surgical scrub, and again with 70% alcohol. Cover the mouse with a sterilized surgical drape except for the cervical incision area.
Confirm by toe pinch that the mouse is fully anesthetized and give analgesia (Caprofen 3-5 mg/kg) via intraperitoneal or subcutaneous injection.
Under the dissecting microscope, make a ventral midline incision around the cervical area using either a scalpel or iris scissors. NOTE: We use scissors because the working distance of the stereomicroscope is limited, which makes it difficult to use a scalpel.
Expose the left common carotid artery (LCCA) by pushing aside and repositioning the salivary glands that cover the blood vessels to the left side of the animal.
Identify all the blood vessels in the surgical field (Figure 1). The LCCA bifurcates into the left internal carotid artery (ICA) and the left external carotid artery (ECA). The superficial thyroid artery (STA) arises from the ECA on the medial side. The occipital artery (OA) usually arises from the ECA, but in some mice it arises from the ICA.
- Ligate all artery branches except the OA using sterilized 6-0 silk suture. To achieve this, make the following two ligations.
- Gently remove the connective tissue around and below the left internal carotid artery (ICA). Grab a piece of precut 6-0 silk suture (~2.5 cm) with forceps and pass it under the artery. Using another pair of forceps, pull the suture roughly 1/3 of its length and ligate the artery.
- Remove the connective tissue around the left external carotid artery (ECA) in the same way described above and make a ligation proximal to the left superior thyroid artery (STA) (Figure 1). Be careful not to damage nerve fibers that run within the surgical field.
When these ligations have been made, return the salivary glands to the original position and hydrate the surgical field by placing 2-3 drops of sterile saline. Close the skin using 6-0 coated vicryl sutures.
After the surgery, place the mouse in the pre-warmed cage (see 1.2.1). The mouse should wake up within 5 min and begin to walk around. Once confirmed that the mouse behaves normally, bring the cage to the animal housing room.
Observe the mouse daily for the first 3 days of recovery. The mouse can be kept as long as the experiment requires under the various conditions that the experimental protocol calls for. En face preparations may be made at any time after the surgery.
2. En Face Immunostaining
Euthanize a mouse with CO2 by inhalation overdose.
Tape the mouse in a supine (belly side up) position onto a dissecting board.
Expose the abdominal cavity by making a midline incision using iris scissors.
Expose the thoracic cavity by cutting the ribs laterally to the sternum.
Make a nick in the vena cava or cut one of the femoral arteries for draining blood.
Insert a 26 G needle attached to a gravity perfusion setup (120 cm water pressure) into the apex of the left ventricle and perfuse the circulatory system with saline solution containing heparin (40 U/mL). Continue the perfusion until the saline flowing out from the cut becomes clear.
Switch the perfusion system from saline to the fixation solution containing 4% paraformaldehyde in PBS (phosphate buffered saline), and continue perfusing for 5 more min.
Harvest the aorta and both left and right carotid arteries using blunt-end scissors and forceps, and place in a 50 mL conical tube containing the fixative on ice.
Transfer the vessel into a Petri dish containing PBS under a dissecting microscope, and carefully remove the fat and connective tissues attached to the aorta and carotid arteries. Separate and split the aorta and carotid arteries longitudinally to expose the endothelium (Figure 2).
Transfer each vessel separately to a well of a 12-well plate containing 0.5 mL of a permeabilizing solution (0.1% Triton X-100 in PBS) per well. Permeabilize blood vessels for 10 min with rocking at room temperature (RT).
Wash briefly with PBS.
To block non-specific antibody binding sites, incubate blood vessels in 10% normal serum from the animal species in which the secondary antibodies have been made, in TTBS (Tris-buffered saline (TBS) with 2.5% Tween 20) for 30 min with rocking at RT.
Incubate vessels with the primary antibodies appropriately diluted in TTBS with 10% normal serum (as described above) overnight with rocking at 4 °C. The level of dilution must be determined for each antibody.
- Perform the following control staining.
- Incubate vessels with TTBS instead of a primary antibody followed by incubation with a secondary antibody.
- Incubate vessels with TTBS containing non-immune (or pre-immune) serum or Ig of the same animal (species) in which primary antibodies have been made, followed by incubation with a secondary antibody.
- Omit the incubation with a secondary antibody. These control specimens must be handled in the same manner and at the same time when staining with specific antibodies is performed.
Wash blood vessels 3 times with TTBS for 10 min each with rocking at RT.
Incubate with fluorescently labeled secondary antibodies diluted appropriately in TTBS with 10% normal serum (as described above) for 1 h with rocking at RT. Nuclear staining with DAPI (4',6-diamidino-2-phenylindole) may be simultaneously performed at this stage by adding 1/5,000 by volume of a DAPI stock solution which contains 5 mg/mL of DAPI in H2O.
Wash 3 times with TTBS for 10 min each with rocking at RT.
Rinse briefly in PBS.
Place one drop of the anti-fade reagent on a cover glass (22 mm x 50 mm) and place a blood vessel on the cover glass with the endothelium facing down.
Place a slide glass (22 mm x 75 mm) on the blood vessel while avoiding trapping bubbles.
Place the slide on a clean laboratory wipe (e.g. Kimwipe) and cover the slide with two pieces of laboratory wipe. Gently place 3.5 kg of weight (e.g. use a bottle of water on a thick book.) on the slide for a maximum of 5 min to flatten the en face blood vessel sample.
Remove the weight and wipe off excess solution from around the coverslip.
Apply nail polish at the 4 corners of the coverslip, place the slides in a slide box, coverslip side up, and keep in the dark at RT (or 4 °C) overnight. This process flattens the tissue further and makes it easier to do microscopy at high magnifications.
Seal the coverslip completely using nail polish.
Perform microscopy as soon as the nail polish is dry.
If needed, store slides at -20 °C.
Representative Results
A typical en face immunofluorescence image of the endothelium is shown in Figure 3. This image shows a single optical section of a mouse aorta taken near the opening of an intercostal artery (the large dark egg-shaped area). The aorta was double-stained with anti-VE-cadherin (green) and anti-VCAM-1 (vascular cell adhesion molecule-1) (red). Each endothelial cell is outlined with a green linear staining at the adherens junction. Due to minor unevenness of the specimen, some adherens junctions are outside of this optical section. Anti-VCAM-1 staining is stronger at the opening of the intercostal artery where disturbed blood flow is known to occur. Figure 4 shows en face staining of carotid arteries with anti-VE-cadherin (green), anti-VCAM-1 (red), and DAPI (purple). The left carotid artery (LCA) was partially ligated while the right carotid artery (RCA) was untouched. The vessel specimens were made 1 day after the surgery and stained. Note increased anti-VCAM-1 staining in the ligated vessel. Specimens stained immunofluorescently with various antibodies can be used to investigate the expression level of proteins of interest, the extent of posttranslational modifications of target proteins, and of course, the pattern of localization of various proteins inside endothelial cells as well as in other cells within the blood vessel wall10,11.
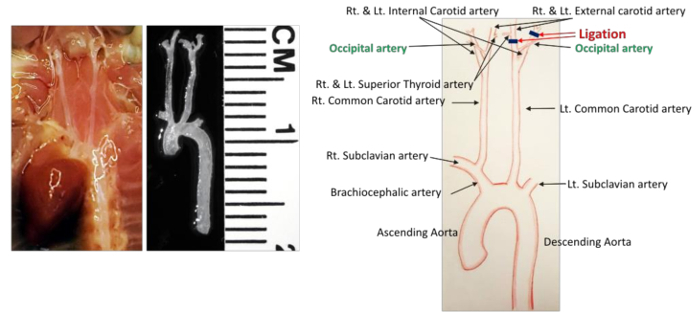 Figure 1: Detailed Vessel Anatomy in the Mouse Cervical Area. The vascular network before and after dissection is shown on the left. All the arteries are identified in the diagram shown on the right. Black lines indicate ligations. Scale: 1 division = 1 mm. Please click here to view a larger version of this figure.
Figure 1: Detailed Vessel Anatomy in the Mouse Cervical Area. The vascular network before and after dissection is shown on the left. All the arteries are identified in the diagram shown on the right. Black lines indicate ligations. Scale: 1 division = 1 mm. Please click here to view a larger version of this figure.
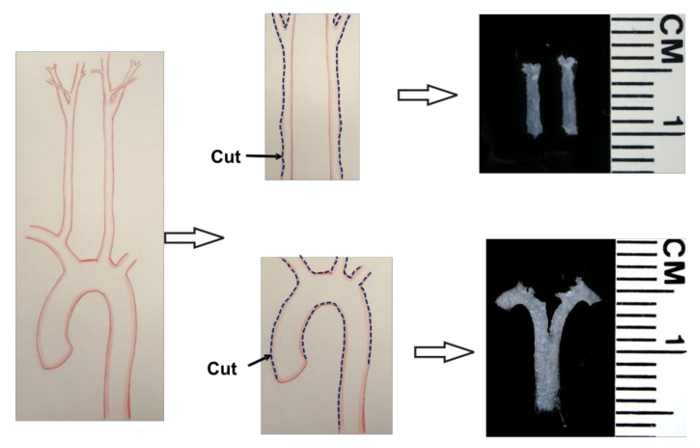 Figure 2: Diagram Showing How Carotid Arteries and Aorta are Made into En Face Preparations. Dotted lines along the vessel wall indicate cuts to be made to open up the vessels. The colored micrographs show actual en face preparations. Scale: 1 division = 1 mm. Please click here to view a larger version of this figure.
Figure 2: Diagram Showing How Carotid Arteries and Aorta are Made into En Face Preparations. Dotted lines along the vessel wall indicate cuts to be made to open up the vessels. The colored micrographs show actual en face preparations. Scale: 1 division = 1 mm. Please click here to view a larger version of this figure.
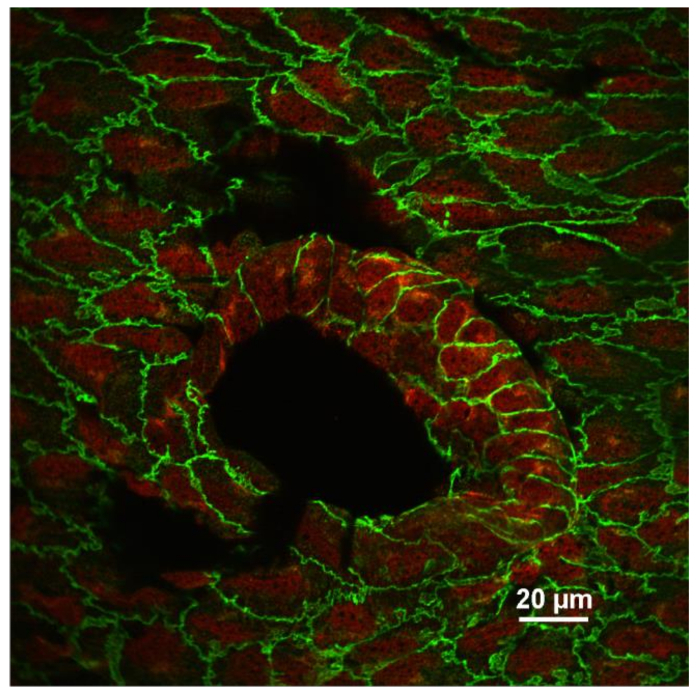 Figure 3: An En Face Image of the Endothelium Stained with Anti-VE-cadherin (Green) and Anti-VCAM-1 (Red). A confocal single optical section of endothelial cells near an intercostal opening is shown. Note that VCAM-1 expression is increased in endothelial cells located at the vessel branch point where blood flow is non-laminar. The image was recorded using a 60X (N.A. 1.4, oil) objective lens. Scale bar = 20 µm. Please click here to view a larger version of this figure.
Figure 3: An En Face Image of the Endothelium Stained with Anti-VE-cadherin (Green) and Anti-VCAM-1 (Red). A confocal single optical section of endothelial cells near an intercostal opening is shown. Note that VCAM-1 expression is increased in endothelial cells located at the vessel branch point where blood flow is non-laminar. The image was recorded using a 60X (N.A. 1.4, oil) objective lens. Scale bar = 20 µm. Please click here to view a larger version of this figure.
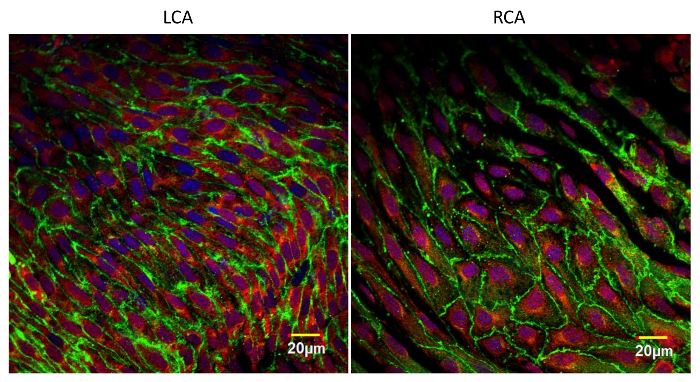 Figure 4: En Face Images of the Left and Right Carotid Arteries Stained with Anti-VE-cadherin (Green), Anti-VCAM-1 (Red), and DAPI (Purple). The left carotid artery was partially ligated and the right carotid was left intact. These en face preparations were made 24 h after the surgery. Increased expression of VCAM-1 on the ligated side compared to the intact vessel is evident. These images were taken near the bifurcation of common carotid arteries by using a laser scanning confocal microscope with a 60X (N.A. 1.4, oil) objective lens. Scale bars = 20 µm. Please click here to view a larger version of this figure.
Figure 4: En Face Images of the Left and Right Carotid Arteries Stained with Anti-VE-cadherin (Green), Anti-VCAM-1 (Red), and DAPI (Purple). The left carotid artery was partially ligated and the right carotid was left intact. These en face preparations were made 24 h after the surgery. Increased expression of VCAM-1 on the ligated side compared to the intact vessel is evident. These images were taken near the bifurcation of common carotid arteries by using a laser scanning confocal microscope with a 60X (N.A. 1.4, oil) objective lens. Scale bars = 20 µm. Please click here to view a larger version of this figure.
Discussion
When handling mouse blood vessels, it is important to remember that the endothelium is fragile and that any excessive mechanical force will damage endothelial cells. For example, endothelial cells break or detach from the vessel wall if the vessel is perfused too forcefully, which can easily happen when the vasculature is perfused using a hand-operated syringe.
To obtain constant perfusion pressure, we use a gravity perfusion system with a 120 cm water column pressure. It has been reported that the mean arterial pressure of a mouse, which differs by strain, ranges between 130 and 170 cm H2O14. Thus, the perfusion pressure we use is slightly less than the measured arterial pressure. When we perfusion-fixed rat aorta, 90 cm H2O column pressure was used6.
In situ endothelial cells are also damaged if the vessel is stretched during harvesting, cleaning, longitudinal splitting, immunostaining, and mounting. In fact, mechanical damage is one of the common causes of losing endothelial cells in en face preparations. Vessel stretching can occur at any step during the procedure, but most commonly, it occurs at the time of harvesting the vessel. It is also easy to stretch the vessel when removing the adipose tissue attached to the adventitia.
En face preparations are made by cutting a vessel longitudinally along its entire length. This is done usually using sharp ophthalmic scissors. However, the tip of scissors may be too large if the inner diameter of the target vessel is small. In such a case, one may use a fractured thin disposable razor blade to make a cut. We have used this technique to make en face preparations of chick mesenteric artery15.
After fixation, en face preparations are permeabilized. Usually, PBS containing Triton X-100 is used for this purpose, but it is possible to use other permeabilization reagents such as Tween-20, Nonidet P-40, saponin, digitonin, and Leucomerm. Ideally, the permeabilization condition should be optimized in each lab. For the mouse aorta and carotid arteries, we treat them with PBS containing 0.1% Triton X-100 for 10 min at RT, and this treatment is sufficient to permeabilize all the cells within the vessel wall. Permeabilized samples are then sequentially treated first with a primary antibody and then a secondary antibody which is fluorescently labeled. For staining mouse vessels, it is critical that the primary antibody is not made in mouse because the mouse vascular tissue will contain mouse IgG which will be labeled by the fluorescently-labeled secondary anti-mouse IgG, causing high background staining. For microscopy, the specimen should be as flat as possible. We press slides for 5 min with 3.5 kg of weight. This specific weight was determined empirically.
When en face preparations are labeled immunofluorescently, they can be studied by using an ordinary epifluorescence microscope, a laser scanning confocal microscope, and a multiphoton microscope. Confocal microscopy is best to obtain images of the endothelium and the subendothelial region up to 50 µm or so from the vessel surface while deep penetration of the excitation light achieved by the multiphoton mode of illumination enables one to obtain in-focus images from the depth of up to 2 mm from the vessel wall surface. In addition, multiphoton microscopy can be used for second harmonic imaging, most typically to study collagen fiber organization in the vessel wall. En face preparations are large, allowing us to survey a large vascular area such as the entire length of the aorta. These are some of the advantages of using immunofluorescently stained en face blood vessel preparations. There are, however, some disadvantages of this technique. First of all, the method is limited to the availability of specific antibodies and other fluorescently-labeled reagents such as fluorescent phalloidin, DAPI, and DiI-Ac-LDL (Acetylated Low Density Lipoprotein labeled with 1,1'-dioctadecyl - 3,3,3',3'-tetramethyl-indocarbocyanine perchlorate). Since imaging is based on fluorescence, non-fluorescent parts of specimens cannot be imaged. The whole mount specimens in general exhibit autofluorescence, and elastin fibers found in large blood vessels fluoresce in green. This fluorescence is especially problematic when using an epifluorescence microscope; thus, imaging by a confocal microscope is highly recommended. However, interference of this green autofluorescence can be significantly reduced by using secondary antibodies labeled with a red fluorescent dye. Finally, since en face specimens are thick, imaging by transmitted illumination is not possible.
Commercial confocal and multiphoton microscopes come with image analysis software including one for quantitatively analyzing fluorescent intensity of images. Quantified data are more reliable if comparisons are made within the same slide. This is so because all the conditions for immunostaining are the same for the specimen. If staining intensities must be compared between different slides (for instance, normal vs diseased vessels), the only way to validate the data is to increase sample numbers so that both technical and biological variations can be averaged. In general, intensity measurements on confocal images obtained near the surface of vessels are more reliable. Fluorescent intensities of images obtained from deeper regions of tissue tend to be more variable because of different degrees of scattering and absorption of both excitation and emitted fluorescent light. In general, one must be careful in interpreting subtle intensity differences detected in the deep areas of specimens. To improve imaging ability from deeper regions of tissue, attempts are being made to make tissues translucent, and some impressive images have been obtained (for example, see a recent article by Neckel et al.16 and papers cited by these authors). Although it is possible that the treatments used to make tissues translucent may extract certain antigens and/or denature certain epitopes, this method may be used to get more reproducible fluorescent signals from deeper regions of tissue.
The use of en face preparations is not limited to imaging by fluorescence microscopy. Using a stereo microscope, en face vessel preparations can be used to study the extent of atherosclerotic plaque formation after staining them with Oil Red O. En face vessel preparations can be made aseptically. Such preparations can be kept in culture and may be used as an ex vivo system to study leukocyte-endothelial cell interaction.
Disclosures
None
Acknowledgments
The research activities of the authors are supported by grants from the National Institute of Health to Dr. Abe (HL-130193, HL-123346, HL-118462, HL-108551).
References
- Jelev L, Surchev L. A novel simple technique for en face endothelial observations using water-soluble media -'thinned-wall' preparations. J Anat. 2008;212(2):192–197. doi: 10.1111/j.1469-7580.2007.00844.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neill JF. The effect on venous endothelium of alterations in blood flow through the vessels in vein walls, and the possible relation to thrombosis. Ann Surg. 1947;126(3):270–288. [PubMed] [Google Scholar]
- Rogers KA, Kalnins VI. A method for examining the endothelial cytoskeleton in situ using immunofluorescence. J Histochem Cytochem. 1983;11(11):1317–1320. doi: 10.1177/31.11.6352798. [DOI] [PubMed] [Google Scholar]
- Poole JCF, Sanders AG, Florey HW. The regeneration of aortic endothelium. J Pathol Bacteriol. 1958;75:133–143. doi: 10.1002/path.1700750116. [DOI] [PubMed] [Google Scholar]
- Sade RM, Folkman J. En face stripping of vascular endothelium. Microvasc Res. 1972;4:77–80. doi: 10.1016/0026-2862(72)90018-0. [DOI] [PubMed] [Google Scholar]
- White GE, Gimbrone MA, Jr, Fujiwara K. Factors influencing the expression of stress fibers in vascular endothelial cells in situ. J Cell Biol. 1983;97(2):416–424. doi: 10.1083/jcb.97.2.416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim DW, Gotlieb AI, Langille BL. In vivo modulation of endothelial F-actin microfilaments by experimental alterations in shear stress. Arteriosclero. 1989;9:439–445. doi: 10.1161/01.atv.9.4.439. [DOI] [PubMed] [Google Scholar]
- Haka A, Potteaux S, Fraser H, Randolph G, Maxfield F. Quantitative analysis of monocyte subpopulations in murine atherosclerotic plaques by multiphoton microscopy. Plos ONE. 2012;7(9):244823e. doi: 10.1371/journal.pone.0044823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chèvre R, et al. High-Resolution imaging of intravascular atherogenic inflammation in live mice. Circ Res. 2014;114:770–779. doi: 10.1161/CIRCRESAHA.114.302590. [DOI] [PubMed] [Google Scholar]
- Heo K-S, et al. Disturbed flow-activated p90RSK kinase accelerates atherosclerosis by inhibiting SENP2 function. J Clin Invest. 2015;125(3):1299–1310. doi: 10.1172/JCI76453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le N-T, et al. A crucial role for p90RSK-mediated reduction of ERK5 transcriptional activity in endothelial dysfunction and atherosclerosis. Circ. 2013;127:486–499. doi: 10.1161/CIRCULATIONAHA.112.116988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kano Y, Katoh K, Masuda M, Fujiwara K. Macromolecular composition of stress fiber-plasma membrane attachment sites in endothelial cells in situ. Circ Res. 1996;79:1000–1006. doi: 10.1161/01.res.79.5.1000. [DOI] [PubMed] [Google Scholar]
- Nigro P, et al. Cyclophilin A is an inflammatory mediator that promotes atherosclerosis in apolipoprotein E-dependent mice. J Exp Med. 2011;208(1):53–66. doi: 10.1084/jem.20101174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattson DL. Comparison of arterial blood pressure in different strains of mice. Am J Hypertens. 2001;14(5):405–408. doi: 10.1016/s0895-7061(00)01285-1. [DOI] [PubMed] [Google Scholar]
- Jinguji Y, Fujiwara K. Stress fiber dependent axial organization of fibronectin fibrils in the basal lamina of the chick and mesenteric artery. Endothelium. 1994;2:35–47. [Google Scholar]
- Neckel PH, Mattheus U, Hirt B, Lust L, Mack AF. Large-scale tissue clearing (PACT): Technical evaluations and new perspectives in immunofluorescence, histology, and ultrastructure. Sci Rep. 2016;6:34331. doi: 10.1038/srep34331. [DOI] [PMC free article] [PubMed] [Google Scholar]


