Abstract
Background
Financial barriers to adult vaccination are poorly understood. Our objectives were to assess among general internists (GIM) and family physicians (FP) shortly after Affordable Care Act (ACA) implementation: 1) proportion of adult patients deferring or refusing vaccines because of cost and frequency of physicians not recommending vaccines for financial reasons; 2) satisfaction with reimbursement for vaccine purchase and administration by payer type; 3) knowledge of Medicare coverage of vaccines; and 4) awareness of vaccine-specific provisions of the ACA.
Methods
We administered an Internet and mail survey from June to October 2013 to national networks of 438 GIMs and 401 FPs.
Results
Response rates were 72% (317/438) for GIM and 59% (236/401) for FP. Among physicians who routinely recommended vaccines, up to 24% of GIM and 30% of FP reported adult patients defer or refuse certain vaccines for financial reasons most of the time. Physicians reported not recommending vaccines because they thought the patient’s insurance would not cover it (35%) or the patient could be vaccinated more affordably elsewhere (38%). Among physicians who saw patients with this insurance, dissatisfaction (‘very dissatisfied’) was highest for payments received from Medicaid (16 % vaccine purchase, 14 % vaccine administration) and Medicare Part B (11 % vaccine purchase, 11 % vaccine administration). Depending on the vaccine, 36–71% reported not knowing how Medicare covered the vaccine. Thirty-seven percent were ‘not at all aware’ and 19% were ‘a little aware’ of vaccine-specific provisions of the ACA.
Conclusions
Patients are refusing and physicians are not recommending adult vaccinations for financial reasons. Increased knowledge of private and public insurance coverage for adult vaccinations might position physicians to be more likely to recommend vaccines and better enable them to refer patients to other vaccine providers when a particular vaccine or vaccines are not offered in the practice.
Introduction
Most deaths from vaccine preventable disease in the U.S are among adults, yet adult vaccination rates for most recommended vaccines remain low.1 National stakeholders in adult immunization have voiced concerns about gaps in financing for adult vaccines2 being one source of the problem and prior research3,4 suggests physicians view financial barriers as key contributors to low adult immunization rates. Comparatively, the U.S. pediatric vaccination program has been much more successful5 and benefits from the financial infrastructure of the Vaccines for Children program (VFC).6 Financial barriers to pediatric vaccination7–11 have been well-explored, but there has been little in-depth research of these barriers in the adult immunization program.
The current U.S. system for financing adult vaccine delivery is a mixture of public and private sector efforts, similar to the pediatric program, although there is not a comparable program to VFC for adults. Some of the provisions of the Affordable Care Act (ACA) aimed to address financial barriers to vaccination, but holes remain in the financial framework for adult vaccine delivery. The ACA mandates that non-grandfathered private health insurance plans cover Advisory Committee on Immunization Practices (ACIP) recommended vaccines without a copay when administered by an in-network provider, thus decreasing a financial barrier for patients. However, the law does not address payment to providers for vaccine purchase and administration.2 The ACA temporarily increased Medicaid reimbursement for vaccine administration to Medicare level ($21)11 which may have decreased physicians’ financial barriers to providing vaccines to Medicaid patients. However, the ACA did not mandate State Medicaid agencies do so and several State Medicaid agencies do not cover all ACIP recommended adult vaccines.12 The ACA did not affect vaccination coverage benefits in Medicare, the primary payer for adult vaccines for seniors.
Seasonal influenza vaccines, pneumococcal vaccines, hepatitis B vaccine for patients with certain conditions, and vaccines directly related to the treatment of an injury or direct exposure to a disease are covered by Medicare Part B. Over 90% of Medicare beneficiaries have Medicare Part B coverage.13 Vaccines not covered by Medicare Part B, must be covered by Medicare Part D plans and are subject to deductibles and copays for each individual vaccine. Not all Medicare beneficiaries have a Part D plan to cover these other vaccines; in 2015, 71% of seniors had Medicare Part D coverage.14
Little is known about physician awareness of Medicare coverage of vaccines or of the vaccine-specific provisions of the ACA. While physicians have reported concerns about reimbursement for adult vaccine delivery, this has not been assessed by payer type. Given the important role financial barriers may play in patient and provider behaviors related to adult vaccine delivery, we conducted a survey to determine among general internists and family physicians nationally soon after ACA implementation: 1) the proportion of adult patients who defer or refuse vaccines because of cost and the frequency of physicians not recommending vaccines for financial reasons; 2) satisfaction with payment for vaccine administration and purchase by payer type; 3) knowledge of Medicare coverage of vaccines; and 4) awareness of vaccine-specific provisions of the ACA.
Methods
Study Setting
From June – October 2013, we administered a survey to a national network of physicians who spent at least half their time practicing primary care. The human subjects review board at the University of Colorado Denver approved this study as exempt research not requiring written informed consent.
Study Population
The Vaccine Policy Collaborative Initiative15, a survey mechanism to assess physician attitudes about vaccine issues in collaboration with the Centers for Disease Control and Prevention (CDC), conducted the survey. We developed a network of primary care physicians for this program by recruiting general internists (GIM) and family physicians (FP) from the memberships of the American College of Physicians (ACP) and the American Academy of Family Physicians (AAFP). We conducted quota sampling16 to ensure that networks of physicians were similar to the ACP and AAFP memberships with respect to region, urban versus rural location, and for GIM only, practice setting. We previously demonstrated that survey responses from network physicians compared to those of physicians randomly sampled from American Medical Association physician databases were similar with respect to reported demographic characteristics, practice attributes, and attitudes about vaccination issues.16
Survey Design
We developed the survey collaboratively with the CDC. We used 4-point Likert scales for assessing frequency of not recommending vaccines for financial reasons (‘Never’ to ‘Frequently’), for satisfaction (‘Very satisfied’ to ‘Very dissatisfied’) with insurance payment for vaccine and administration fees for each payer type, and for whether physicians had considered stopping providing vaccines to patients with specific insurance types (‘never considered,’ ‘considered, but not seriously,’ ‘seriously considered or discussed,’ ‘already stopped providing all vaccines.’) Private payer types included fee for service (FFS), preferred provider organizations (PPO), and managed care (MCO) or health maintenance organizations (HMO). Public payer types included Medicaid and Medicare Parts B and D. We provided respondents with information about vaccine-specific provisions of the ACA and asked questions regarding their prior awareness of these provisions and whether these provisions would result in their practices changing stocking patterns of adult ACIP routinely recommended vaccines. A national advisory panel of GIM (n=3) and FP (n=4) pre-tested the survey, which we modified based on their feedback. We pilot-tested the survey among 50 GIM and 15 FP nationally and further modified based on their feedback.
Survey Administration
Based on physician preference, we sent the survey over the Internet17 or through the U.S. Postal Service. We sent the Internet group an initial e-mail with up to 8 e-mail reminders, and we sent the mail group an initial mailing and up to 2 additional reminders. Non-respondents in the Internet group were also sent a mail survey in case of problems with e-mail correspondence. We patterned the mail protocol on Dillman’s tailored design method.18
Statistical analysis
We pooled Internet and mail surveys for analyses because other studies have found that physician attitudes are similar when obtained by either method18–20. We compared respondents with non-respondents on all available characteristics using Wilcoxon and chi-square analyses; characteristics of non-respondents were obtained from the recruitment survey for the sentinel networks. We compared GIM and FP responses using Mantel-Haenszel chi square and Fisher’s Exact tests. With the exception of reported proportion of patients who defer or refuse vaccines for financial reasons and reported satisfaction with reimbursement by payer type, responses between specialties were similar and are, therefore, presented together. For comparisons between public (Medicaid, Medicare Parts B & D) and private insurance (HMO/MCO, PPO, FFS) we compared the proportion who responded ‘very dissatisfied’ to any payer in that group using chi-square analyses. Analyses were performed using SAS software, version 9.4 (SAS Institute, Cary, North Carolina).
Results
Survey response and characteristics of respondents
Response rates were 72% for GIM (317/438) and 59% for FP (236/401). Respondents and non-respondents did not differ significantly by age, region, practice location, or practice setting. Among GIM physicians, males were less likely to respond (p=0.02). Characteristics of respondents, their practices and their patient populations are shown in Table 1. Of those who responded, 19 (9 GIM and 10 FP) reported they do not give immunizations to adult patients and were excluded from further analysis leaving a final cohort of 534 (308 GIM, 226 FP).
Table 1.
Respondent and Non-Respondent Characteristics
| Characteristic | GIM | FP | ||
|---|---|---|---|---|
| Respondents (n=317) |
Non-Respondents (n=121) |
Respondents (n=236) |
Non-Respondents (n=165) |
|
| Age in years, mean (SD) | 52.9 (8.8) | 52.0 (9.5) | 52.9 (9.9) | 50.9 (10.1) |
| Male, % | 62* | 74* | 56 | 61 |
| Region, % | ||||
| Midwest | 19 | 27 | 31 | 26 |
| Northeast | 27 | 23 | 16 | 16 |
| South | 32 | 34 | 30 | 41 |
| West | 23 | 16 | 23 | 18 |
| Location of Practice, % | ||||
| Urban | 46 | 40 | 25 | 24 |
| Suburban | 41 | 46 | 46 | 51 |
| Rural | 13 | 15 | 29 | 25 |
| Setting, % | ||||
| Private practice | 80 | 79 | 7 | 74 |
| Hospital/clinic | 17 | 18 | 24 | 20 |
| HMO | 4 | 3 | 6 | 6 |
| # of physicians in your practice, % | ||||
| 1 | 15 | 21 | ||
| 2–4 | 27 | 39 | ||
| 5–10 | 29 | 25 | ||
| ≥10 | 29 | 14 | ||
| Physicians providing vaccines to adults, % | 97 | 96 | ||
| Proportion of patients ≥ 65,% | ||||
| <10% | 4 | 12 | ||
| 10–24% | 17 | 36 | ||
| 25–49% | 45 | 37 | ||
| ≥50% | 34 | 14 | ||
| Patients with Medicare Part B,% | ||||
| <10% | 7 | 16 | ||
| 10–24% | 18 | 31 | ||
| 25–49% | 42 | 35 | ||
| ≥50% | 24 | 10 | ||
| Don’t know | 10 | 7 | ||
| Patients with Medicare Part D,% | ||||
| <10% | 9 | 19 | ||
| 10–24% | 26 | 34 | ||
| 25–49% | 30 | 22 | ||
| ≥50% | 20 | 6 | ||
| Don’t know | 15 | 19 | ||
p<0.05 for comparison of respondents and non-respondents
Proportion of adults who defer or refuse vaccines for financial reasons
Figure 1 shows, among physicians who recommended each vaccine, the percentage of physicians who reported patients deferring or refusing vaccines because of out-of-pocket costs or insufficient insurance coverage in a typical month. Zoster, hepatitis B, and HPV vaccines were most commonly reported as deferred or refused.
Figure 1. Among Physicians Who Routinely Recommend Each Vaccine, Reported Proportion of Patients Who Defer/Refuse Vaccination due to Financial Reasons in a Typical Month*.

The following proportions of physicians for GIM and FP, respectively, were excluded from the analysis for the vaccines he/she did not recommend: Zoster (GIM-1%, FP-3%), Hepatitis B (18%, 16%), Tdap (2%, 1%), Hepatitis A (27%, 28%), HPV (22%, 7%), Meningococcal (26%, 14%), Varicella (39%, 17%), Td (6%, 10%), PCV13 (17%, 17%), PPSV23 (3%, 2%), MMR (30%, 16%).
+p<0.05 for difference in reported vaccination defer/refusal due to financial reasons between GIM and FP, Mantel-Haenszel χ2 Square.
GIM = general internists; FP = family medicine physicians; Tdap = tetanus, diphtheria, acellular pertussis; HPV = Human Papillomavirus; Td = tetanus, diphtheria; PCV13 = Pneumococcal conjugate vaccine; PPSV23 = pneumococcal polysaccharide vaccine; and MMR = measles, mumps, rubella
Vaccine prices were obtained from the CDC Vaccine Price List for the private sector: http://www.cdc.gov/vaccines/programs/vfc/awardees/vaccine-management/price-list/index.html.
Frequency of physicians not recommending an adult vaccine for financial reasons
Figure 2 demonstrates the frequency within the last year that physicians have reported not recommending a vaccine to an adult for various financial reasons. Over one-third of physicians reported they had not recommended vaccines ‘frequently’ or ‘sometimes’ because they either thought the patient’s insurance would not cover it or that the patient could receive the vaccine more affordably elsewhere; nearly one-quarter had not recommended vaccination believing that the patient could not afford it.
Figure 2. Frequency of Not Recommending Vaccination for Financial Reasons in the Past Year (GIM, n=308 and FP, n=226)*.

*No significant differences found comparing specialties using Mantel-Haenszel chi-squared test.
GIM = General Internal Medicine; FP = Family Practice
Satisfaction with Insurance Payment
Physicians’ level of satisfaction with insurance payment for vaccine purchase and vaccine administration by insurance type is shown in Figure 3. Almost half of the physicians were not knowledgeable about their level of satisfaction with payment by payer. However, across all payers, 6 to 16 % were ‘very dissatisfied’ with payment for vaccine purchase and 5 to 14 % were ‘very dissatisfied’ with payment for vaccine administration. There were 402/534 physicians (75%) who saw all insurance types and had non-missing values for satisfaction for vaccine purchase. Of those, 19% (n=75) reported being ‘very dissatisfied’ with any public payer, compared to 7% (n=28, p<.0001) who reported being ‘very dissatisfied’ with any private payer. There were 401/534 (75%) who saw all insurance types and had non-missing values for satisfaction for vaccine administration. Of those, 16% (n=66) reported being ‘very dissatisfied’ with any public payer, compared to 6% (n=23, p<.0001) who reported being ‘very dissatisfied’ with any private payer. Of physicians seeing patients with each specific insurance type, 12% (48/417), 11% (49/455), 11% (52/467) and 7% (32/485) had seriously considered stopping to provide all vaccines to patients with Medicaid, Medicare Part D, Medicare Part B and private insurance, respectively, due to vaccine cost, administration fee, and/or reimbursement issues in the past twelve months. Less than 5% of physicians had actually stopped providing vaccines for any payment type.
Figure 3. Satisfaction with Payment for Vaccine Purchase and Administration by Payer, (n=499)+.
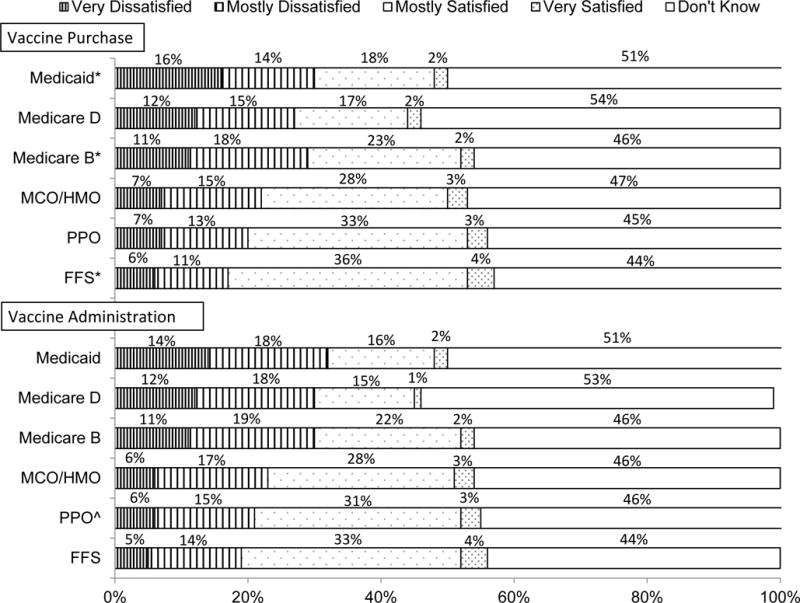
+4.5–14.6% of respondents indicated that they do not see patients in this group or do not bill this insurance, and therefore are not included in the figure.
*Comparison between specialties, with GIM more likely to report dissatisfaction with payment for vaccine purchase than FP for Medicaid (p=0.01), Medicare Part B (p=0.03), and FFS (p=0.04) by X2 analysis.
ˆComparison between specialties with GIM more likely to report dissatisfaction with payment for vaccine administration than FP for PPO (p=0.02) by X2 analysis.
MCO/HMO = managed care organization/health maintenance organization; PPO = preferred provider organization; FFS = fee for service.
Knowledge of Medicare coverage of vaccines
Eighty-three (n=425/512) percent of respondents reported their practice had a contractual relationship with Medicare. Of these respondents, 41% reported billing, 29% reported not billing, and 29% reported they ‘do not know’ if their practices bill Medicare Part D for adult vaccines provided in the practice. Only 9% of these respondents were aware of TransactRx-a web portal through which practices can electronically submit claims for reimbursement for Medicare Part D vaccines and administration. Of those who were aware of it, only 46% (n=16) reported being members of TransactRx. Physicians who reported having a contractual relationship with Medicare were also asked, as of January 2013, through what parts of Medicare various vaccines are reimbursed for beneficiaries (see Table 2). Large proportions, and often the majority of physicians, were not knowledgeable about Medicare coverage for vaccines. They were most knowledgeable about Medicare coverage for seasonal influenza, PPSV23, and zoster vaccines.
Table 2.
Among Providers Accepting Medicare, Knowledge of Medicare Coverage of Vaccines (n=425)*
| Vaccine | Medicare Coverage | Correct (%) | Incorrect (%) | Didn’t Know (%) |
|---|---|---|---|---|
| Seasonal influenza | Part B | 59 | 5 | 36 |
| PPSV23 | Part B | 54 | 5 | 41 |
| Zoster | Part D | 51 | 5 | 43 |
| PCV13 | Part B | 40 | 5 | 55 |
| Td | Part B | 36 | 10 | 54 |
| Hepatitis B | Part B | 27 | 8 | 66 |
| Tdap | Part D | 17 | 26 | 58 |
| Hepatitis A | Part D | 8 | 21 | 71 |
Tdap = tetanus, diphtheria, acellular pertussis; HPV = human papillomavirus; Td = tetanus, diphtheria; PCV13 = pneumococcal conjugate; and PPSV23 = pneumococcal polysaccharide
No significant differences found comparing specialties using Mantel-Haenszel chi-squared test.
Awareness of and anticipated changes as a result of vaccine specific provisions of the Affordable Care Act
Eleven percent of physicians were ‘very aware,’ 33% were ‘somewhat aware,’ 19% were ‘a little aware,’ and 37% were ‘not at all aware’ of the vaccine specific provisions of the Affordable Care Act. As a result of the ACA provisions, 71% of physicians reported their practice would not change, 8% would increase, and 1% would decrease the number of ACIP recommended adult vaccines their practice stocks. Twenty percent ‘did not know’ how these ACA provisions would affect their practice’s adult vaccine stocking patterns.
Discussion
While previous studies have documented physician reported financial barriers to adult vaccination,3,4 ours is the first to describe the implications of these financial barriers in practice. Many physicians reported not recommending vaccinations to their adult patients and patients frequently refusing vaccines for financial reasons. Physician satisfaction with reimbursement for delivering adult vaccines had not been previously reported. Although almost half of physicians were not knowledgeable about reimbursement, up to one-third of the knowledgeable physicians were dissatisfied with insurance payment for both vaccine purchase and vaccine administration across payer types. Physicians were most dissatisfied with public sector payers, primarily Medicaid followed by Medicare Parts B and D. Finally, we found that physicians lacked knowledge about coverage of adult vaccinations under Medicare and had limited awareness of vaccine-specific provisions of the ACA.
Physician recommendation is critical to patient receipt of vaccines,21–25 yet we found that physicians are not recommending vaccines to adults for financial reasons. Regardless of actual insurance coverage, if physicians perceive that vaccines are not covered, they may not recommend them. We are not certain why physicians would not recommend vaccines because patients could receive them more affordably elsewhere. This might relate to vaccines covered by Medicare Part D being more easily being billed for by pharmacists26 or that patients might receive vaccines at no charge by public health departments using federal funds for the underserved to fund the vaccination. According to National Vaccine Advisory Committee standards for adult immunization,27 providers should strongly recommend vaccines regardless of where they might be received.
Since the first US adult immunization schedule was published in 200228, several vaccines have been added, substantially increasing the complexity of the schedule and increasing the cost of obtaining all ACIP recommended vaccines for adults.29–36
Newly recommended vaccines are generally more expensive,10,37 and, in this study, physicians perceived that some of the new, more expensive vaccines, zoster and HPV vaccine, were deferred or refused by more patients than other vaccines for financial reasons. While PCV13 and meningococcal vaccine are also expensive, there are reasons physicians may have perceived these vaccines being refused by less patients. The PCV13 vaccine recommendation at the time of this study was new and targeted certain immunocompromised individuals less than sixty-five years-old, potentially a small proportion of a physician’s patient population. Similarly, the adult meningococcal vaccine recommendation targets certain high-risk adults that might not have accounted for many patients in the practice. It is notable physicians reported very few patients declining seasonal influenza or PPSV-23 vaccines for financial reasons as both of these vaccine are covered by Medicare Part B under which patients are not subject to copays. The fact that physicians perceive that several patients are refusing zoster and HPV vaccines for financial reasons implies that either patients are uninsured or that patient cost-sharing for vaccines can be substantial even when a patient is insured. The ACA has expanded health insurance coverage for millions of Americans38 and thus expanded coverage to recommended vaccines. However, patients covered by some grand-fathered private health insurance plans, some State Medicaid programs, and Medicare Part D may still be experiencing incomplete coverage and/or prohibitive beneficiary cost-sharing. With new vaccines under development like the new zoster vaccine,39 it could be helpful to consider how patient insurance coverage and cost to procure a vaccine will impact vaccine delivery.
While almost the majority of physicians reported they were not knowledgeable about their satisfaction with reimbursement, those that were knowledgeable reported dissatisfaction across payer types, but mostly with public insurance. Some physicians had stopped or had seriously considered stopping to provide vaccines to patients with these insurance types. Medicaid topped the list for both dissatisfaction with vaccine purchase and administration. A prior study evaluating pediatric vaccines also found higher levels of dissatisfaction with Medicaid payment for administration fees.11 Before the temporary increase in Medicaid vaccine administration fees to Medicare levels brought on by the ACA, Medicaid vaccine administration fees were as low as $2.40 It is unclear if physician respondents were aware of or changed their practice as a result of the temporary increased vaccine administration fee for Medicaid patients; this survey launched in the first year of increased payment so physicians may not have been aware of the increase and physicians were generally unaware of the vaccine-specific provisions of the ACA. However, physicians were almost equally dissatisfied with vaccine administration payment through Medicare Part B and D despite Medicare paying considerably more for vaccine administration than many state Medicaid programs,41 so this time-limited increase in payment might have been inconsequential. The Infectious Diseases Society of America has suggested that the Centers for Medicare and Medicaid Services (CMS) should work to assure physician billing codes adequately cover the full costs of providing immunizations42,43 and to do this CMS may require updated information about how much it actually costs to immunize an adult.2
Dissatisfaction with reimbursement for vaccines covered by Medicare Part B has not been previously reported. Previous research did not ask specifically about satisfaction with reimbursement by payer type, but did find that perceiving a higher financial burden from delivering adult vaccines was correlated with having a higher proportion of Medicare Part D patients.4 The only way a physician can bill for a Medicare Part D vaccine is through TransactRx,44 a web-portal which physicians’ can use for billing purposes. Although 41% of physicians reported billing Medicare Part D for vaccines, only 9% were aware of Transact Rx. This finding could be explained by respondents not being fully aware of details of vaccine billing processes. Also, physician knowledge of Medicare coverage for vaccines was poor and therefore physicians might not have accurately distinguished Medicare Part B and D in their responses. The Infectious Diseases Society of America45 and the Medicare Payment Advisory Commission,46 have suggested that all adult vaccines recommended for Medicare beneficiaries be moved to Medicare Part B; however, this may not be feasible due to the significant implications for the U.S government’s budget. Having some vaccines covered under Medicare Part D allows patients to share in the cost of vaccines through deductibles and copays. Increased knowledge of Medicare coverage and billing would help physicians determine which vaccines they can make available to their patients and, when this is not possible, where they should refer patients for vaccination.
Our study has strengths and limitations. Results were generated from general internists and family physicians from across the nation and we achieved an excellent response rate for a physician survey.47 Although the sample of sentinel physicians surveyed was designed to be representative of ACP and AAFP memberships, the attitudes, experiences, and practices of sentinel physicians may not be fully generalizable. Non-respondents may have held different views than respondents. The survey relied on self-report of practice rather than observation of practice. Respondents may have been too unfamiliar with vaccine financing in their practice to respond accurately.
Physicians perceive financial barriers to adult vaccination that are interfering with vaccine delivery and need more guidance on Medicare coverage of vaccines. Our data indicate that lack of understanding regarding Medicare coverage for vaccines and vaccine-relevant provisions of the ACA may be affecting physicians’ strength of recommendation and where they refer patients for vaccination; thus jeopardizing widespread adoption of National Vaccine Advisory Committee adult immunization standards to assess immunizations at every visit, strongly recommend needed vaccines and either administer or refer patients for vaccines.27 Even with the ACA vaccine-specific provisions, gaps remain in the financial infrastructure of adult vaccines in terms of prohibitive costs to patients and perceived insufficient reimbursement for physicians, particularly from public sector payers. Efforts to address these gaps will require further investigation into the perceived barriers created by Medicaid and Medicare reimbursement and physician costs to provide adult vaccines.
Acknowledgments
Funding Source: Centers for Disease Control and Prevention, grant 5U48DP001938. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
CONFLICT OF INTEREST: None of the authors has any conflict of interests.
Bibliography
- 1.Williams WW, Lu PJ, O’Halloran A, et al. Surveillance of Vaccination Coverage Among Adult Populations - United States, 2014. MMWR Surveill Summ. 2016;65(1):1–36. doi: 10.15585/mmwr.ss6501a1. [DOI] [PubMed] [Google Scholar]
- 2.Shen AK, Sobzcyk E, Buchanan A, Wu L, Duggan-Goldstein S. Second National Immunization Congress 2010: addressing vaccine financing for the future in the US. Hum Vaccin. 2011;7(1):12–18. doi: 10.4161/hv.7.1.13949. [DOI] [PubMed] [Google Scholar]
- 3.Hurley LP, Lindley MC, Harpaz R, et al. Barriers to the use of herpes zoster vaccine. Ann Intern Med. 2010;152(9):555–560. doi: 10.7326/0003-4819-152-9-201005040-00005. [DOI] [PubMed] [Google Scholar]
- 4.Hurley LP, Bridges CB, Harpaz R, et al. U.S. Physicians’ perspective of adult vaccine delivery. Ann Intern Med. 2014;160(3):161. doi: 10.7326/M13-2332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. National, State, and Selected Local Area Vaccination Coverage Among Children Aged 19-35 Months - United States 2014. MMWR - Morbidity & Mortality Weekly Report. 2014;64(33):889–896. doi: 10.15585/mmwr.mm6433a1. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Benefits from Immunization During the Vaccines for Children Program Era - United States, 1994–2013. MMWR - Morbidity & Mortality Weekly Report. 2014;63(16):352–255. [PMC free article] [PubMed] [Google Scholar]
- 7.Freed GL, Clark SJ, Konrad TR, Pathman DE. Variation in patient charges for vaccines and well-child care 8. Arch Pediatr Adolesc Med. 1996;150(4):421–426. doi: 10.1001/archpedi.1996.02170290087014. [DOI] [PubMed] [Google Scholar]
- 8.Freed GL, Cowan AE, Clark SJ. Primary care physician perspectives on reimbursement for childhood immunizations. Pediatrics. 2008;122(6):1319–1324. doi: 10.1542/peds.2008-2033. [DOI] [PubMed] [Google Scholar]
- 9.Freed GL, Cowan AE, Gregory S, Clark SJ. Variation in provider vaccine purchase prices and payer reimbursement. Pediatrics. 2008;122(6):1325–1331. doi: 10.1542/peds.2008-2038. [DOI] [PubMed] [Google Scholar]
- 10.Lindley MC, Shen AK, Orenstein WA, Rodewald LE, Birkhead GS. Financing the delivery of vaccines to children and adolescents: challenges to the current system. Pediatrics. 2009;124(Suppl 5):S548–S557. doi: 10.1542/peds.2009-1542O. [DOI] [PubMed] [Google Scholar]
- 11.O’Leary ST, Allison MA, Lindley MC, et al. Vaccine financing from the perspective of primary care physicians. Pediatrics. 2014;133(3):367–374. doi: 10.1542/peds.2013-2637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stewart AM, Lindley MC, Chang KH, Cox MA. Vaccination benefits and cost-sharing policy for non-institutionalized adult Medicaid enrollees in the United States. Vaccine. 2014;32(5):618–623. doi: 10.1016/j.vaccine.2013.11.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Medicare and Medicaid Services. Medicare Enrollment Data by State and Age as of July 1, 2012. 2012 https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/MedicareEnrpts/Downloads/Sageall12.pdf Accessed February 24, 2016.
- 14.Centers for Medicare and Medicaid Services. On its 50th anniversary, more than 55 million Americans covered by Medicare. 2015 https://www.cms.gov/Newsroom/MediaReleaseDatabase/Press-releases/2015-Press-releases-items/2015-07-28.html Accessed February 24, 2016.
- 15.University of Colorado. Vaccine Policy Collaborative Initiative. 2016 http://www.ucdenver.edu/academics/colleges/medicalschool/programs/outcomes/childrensoutcomesreserach/VaccinePolicyCollaborativeInitiative/Pages/default.aspx. Accessed August 10, 2015.
- 16.Crane LA, Daley MF, Barrow J, et al. Sentinel physician networks as a technique for rapid immunization policy surveys. Eval Health Prof. 2008;31(1):43–64. doi: 10.1177/0163278707311872. [DOI] [PubMed] [Google Scholar]
- 17.Vovici Feedback [computer program] Melville, NY: Verint Systems Inc; 2015. [Google Scholar]
- 18.Dillman DA, Smyth J, Christian LM. Internet, Mail and Mixed-Mode Surveys: The Tailored Desgin Method. 3rd. 3rd. New York, NY: John Wiley Co; 2009. [Google Scholar]
- 19.Atkeson LR, Adams AN, Bryant LA, Zilberman L, Saunder KL. Considering Mixed Mode Surveys for Questions in Political Behavior: Using the Internet and Mail to Get Quality Data at Reasonable Costs. Political Behavior. 2011;33(1):161–178. [Google Scholar]
- 20.McMahon SR, Iwamoto M, Massoudi MS, et al. Comparison of e-mail, fax, and postal surveys of pediatricians. Pediatrics. 2003;111(4 Pt 1):e299–e303. doi: 10.1542/peds.111.4.e299. [DOI] [PubMed] [Google Scholar]
- 21.Nichol KL, Lofgren RP, Gapinski J. Influenza vaccination. Knowledge, attitudes, and behavior among high-risk outpatients. Arch Intern Med. 1992;152(1):106–110. doi: 10.1001/archinte.152.1.106. [DOI] [PubMed] [Google Scholar]
- 22.Nichol KL, Mac Donald R, Hauge M. Factors associated with influenza and pneumococcal vaccination behavior among high-risk adults. Journal of general internal medicine. 1996;11(11):673–677. doi: 10.1007/BF02600158. [DOI] [PubMed] [Google Scholar]
- 23.Armstrong K, Berlin M, Schwartz JS, Propert K, Ubel PA. Barriers to influenza immunization in a low-income urban population. Am J Prev Med. 2001;20(1):21–25. doi: 10.1016/s0749-3797(00)00263-4. [DOI] [PubMed] [Google Scholar]
- 24.Winston CA, Wortley PM, Lees KA. Factors associated with vaccination of medicare beneficiaries in five U.S. communities: Results from the racial and ethnic adult disparities in immunization initiative survey, 2003. J Am Geriatr Soc. 2006;54(2):303–310. doi: 10.1111/j.1532-5415.2005.00585.x. [DOI] [PubMed] [Google Scholar]
- 25.Ding H, Black CL, Ball S, et al. Influenza Vaccination Coverage Among Pregnant Women–United States, 2014–15 Influenza Season. MMWR Morb Mortal Wkly Rep. 2015;64(36):1000–1005. doi: 10.15585/mmwr.mm6436a2. [DOI] [PubMed] [Google Scholar]
- 26.U.S. Government Accountability Office. Medicare: many factors, including administrative challenges, affect access to Part D vaccinations. 2011 http://www.gao.gov/products/GAO-12-61. Accessed February 24, 2016.
- 27.National Vaccine Advisory Committee. Recommendations from the National Vaccine Advisory committee: standards for adult immunization practice. Public Health Rep. 2014;129(2):115–123. doi: 10.1177/003335491412900203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Centers for Disease C, Prevention. Recommended adult immunization schedule–United States, 2002–2003. MMWR Morb Mortal Wkly Rep. 2002;51(40):904–908. [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention. Use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine for adults with immunocompromising conditions: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Morb Mortal Wkly Rep. 2012;61(40):816–819. [PubMed] [Google Scholar]
- 30.Tomczyk S, Bennett NM, Stoecker C, et al. Use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine among adults aged >/=65 years: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Morb Mortal Wkly Rep. 2014;63(37):822–825. [PMC free article] [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention. Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine (Tdap) in pregnant women–Advisory Committee on Immunization Practices (ACIP), 2012. MMWR Morb Mortal Wkly Rep. 2013;62(7):131–135. [PMC free article] [PubMed] [Google Scholar]
- 32.MacNeil JR, Rubin L, Folaranmi T, Ortega-Sanchez IR, Patel M, Martin SW. Use of Serogroup B Meningococcal Vaccines in Adolescents and Young Adults: Recommendations of the Advisory Committee on Immunization Practices, 2015. MMWR Morb Mortal Wkly Rep. 2015;64(41):1171–1176. doi: 10.15585/mmwr.mm6441a3. [DOI] [PubMed] [Google Scholar]
- 33.Cohn AC, MacNeil JR, Clark TA, et al. Prevention and control of meningococcal disease: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2013;62(RR-2):1–28. [PubMed] [Google Scholar]
- 34.Kretsinger K, Broder KR, Cortese MM, et al. Preventing tetanus, diphtheria, and pertussis among adults: use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccine recommendations of the Advisory Committee on Immunization Practices (ACIP) and recommendation of ACIP, supported by the Healthcare Infection Control Practices Advisory Committee (HICPAC), for use of Tdap among health-care personnel. MMWR Recomm Rep. 2006;55(RR-17):1–37. [PubMed] [Google Scholar]
- 35.Markowitz LE, Dunne EF, Saraiya M, et al. Human papillomavirus vaccination: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2014;63(RR-05):1–30. [PubMed] [Google Scholar]
- 36.Harpaz R, Ortega-Sanchez IR, Seward JF, Advisory Committee on Immunization Practices Centers for Disease Control and Prevention Prevention of herpes zoster: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2008;57(RR-5):1–30. quiz CE32–34. [PubMed] [Google Scholar]
- 37.Centers for Disease Control and Prevention. CDC Vaccine Price List. 2015 [Google Scholar]
- 38.RAND Corporation. Health Coverage Grows Under Affordable Care Act. 2016 http://www.rand.org/news/press/2015/05/06.html. Accessed March 2, 2016.
- 39.Lal H, Cunningham AL, Heineman TC. Adjuvanted Herpes Zoster Subunit Vaccine in Older Adults. N Engl J Med. 2015;373(16):1576–1577. doi: 10.1056/NEJMc1508392. [DOI] [PubMed] [Google Scholar]
- 40.Stewart AM, Lindley MC, Cox MA. Medicaid provider reimbursement policy for adult immunizations. Vaccine. 2015;33(43):5801–5808. doi: 10.1016/j.vaccine.2015.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Centers for Medicare and Medicaid Services. License for Use of Current Procedural Terminology. (Fourth) (“CPT®”). https://www.cms.gov/apps/physician-fee-schedule/license-agreement.aspx. Accessed March 30, 2016.
- 42.Immunization Work Group of the N, Global Public Health Committee of the Infectious Diseases Society of A. Actions to strengthen adult and adolescent immunization coverage in the United States: policy principles of the Infectious Diseases Society of America. Clin Infect Dis. 2007;44(12):e104–108. doi: 10.1086/519541. [DOI] [PubMed] [Google Scholar]
- 43.Immunization Work Group of the N, Global Public Health Committee of the Infectious Diseases Society of A. Executive summary–Actions to strengthen adult and adolescent immunization coverage in the United States: policy principles of the Infectious Diseases Society of America. Clin Infect Dis. 2007;44(12):1529–1531. doi: 10.1086/519542. [DOI] [PubMed] [Google Scholar]
- 44.TransactRx. Medical Billing Company. 2014 http://www.transactrx.com/
- 45.Orenstein WA, Mootrey GT, Pazol K, Hinman AR. Financing immunization of adults in the United States. Clin Pharmacol Ther. 2007;82(6):764–768. doi: 10.1038/sj.clpt.6100401. [DOI] [PubMed] [Google Scholar]
- 46.Medicare Payment Advisory Commission. Issues in Medicare coverage of drugs; Report to the Congress: Promoting Greater Efficiency in Medicare. 2007:157–186. Available at: www.medpac.gov/chapters/Jun07_Ch07.pdf. Accessed December 27, 2012.
- 47.Hickner J, Thompson PJ, Wilkinson T, et al. Primary care physicians’ challenges in ordering clinical laboratory tests and interpreting results. J Am Board Fam Med. 2014;27(2):268–274. doi: 10.3122/jabfm.2014.02.130104. [DOI] [PubMed] [Google Scholar]


