Abstract
Though addictions to substances including alcohol are highly heritable, there have been no studies regarding the possible applicability of genetic counseling to this set of conditions. Adults (≥18 years old) with a personal and/or family history of alcohol addiction were recruited to participate in an online survey-based study comprising 43 questions about beliefs/concern about recurrence risk and etiology of alcohol addiction and its impact on childbearing decisions, and perceptions of potential utility of genetic counseling for alcohol addiction. We applied primarily descriptive statistics, but also tested the hypotheses that perceiving genetic counseling to be useful would be associated with: 1) increasing importance attributed to genetics in the etiology of alcohol addiction, and 2) greater concern about recurrence of alcohol addiction (in self and/or children). Overall, the 113 participants recognized the multifactorial nature of alcohol addiction but reported a wide range of estimated recurrence risks for first-degree relatives. Overall, 62% perceived genetic counseling for alcohol addiction to be potentially beneficial. Participants were more likely to perceive a benefit from genetic counseling if they were concerned about recurrence for themselves (p = .021) or perceived genetics to be etiologically important in alcohol addiction (p = .024). Future studies are warranted to evaluate the outcomes of genetic counseling for addictions with respect to patient understanding, lifestyle modifications and psychological adaptation.
Keywords: Alcoholism, Genetic Counseling, Alcohol Addiction, Substance Use
Introduction
Addictions to substances including alcohol are highly prevalent psychiatric conditions (“Comorbidity: Addiction and Other Mental Illnesses,” 2010) with alcohol use disorders (defined in the DSMV as a “problem pattern of alcohol use leading to clinically significant impairment or distress”, and includes both alcohol abuse and dependence (American Psychiatric Association, 2013)) affecting an estimated 7% of adults in the United States (National Institute of Alcohol Abuse and Alcoholism, 2015). Addictions can aggregate in families and are highly heritable with an estimated fourfold increase in risk for children of people with alcohol addiction to develop the addiction themselves (Agrawal & Lynskey, 2008; Heath et al., 1997; Kendler K., Heath A., Neale M., Kessler R., 1992; Russell, 1990; Verhulst, Neale, & Kendler, 2015). Like other common conditions, they are complex in etiology arising as a result of the combined effects of genetic and environmental factors. As such, addictions fall squarely within the theoretical scope of relevance for genetic counseling (defined as: “the process of assisting people to understand and adapt to the medical, psychological, and familial implications of genetic contributions to disease” (Resta et al., 2006)).
Though the concept of genetic counseling for psychiatric conditions has been discussed for decades (e.g. Tsuang, 1978), only recently has its practice been studied. Genetic counseling for psychiatric conditions is fundamentally no different from genetic counseling in other contexts – it is a psychotherapeutically oriented encounter in which patients are helped to understand, in a personalized manner, what is known from research about the etiology of the illness in the family and about probability of illness recurrence (if desired) (Austin & Honer, 2007; Biesecker, 2006; Resta et al., 2006). In the context of genetic counseling for psychiatric conditions, the understanding of etiology can be used as a framework to help patients to better understand how they can protect their mental health for the future. Addressing issues that arise relating to guilt, shame, and stigma is central to the process (Austin & Honer, 2008; Costain, Esplen, Toner, Hodgkinson, & Bassett, 2014). Genetic counseling for psychiatric conditions has been shown to significantly increase patient empowerment, knowledge, and self-efficacy, and decrease sense of stigma (Costain et al., 2014; Hippman et al., 2016; Inglis, Koehn, McGillivray, Stewart, & Austin, 2015).
Though studies have looked at the potential applicability and/or impact of genetic counseling for various psychiatric disorders, they have focused on psychotic and mood disorders rather than addictions (Austin & Honer, 2008; Costain et al., 2014; Hippman et al., 2016; Inglis et al., 2015, Andrighetti et al., 2015). To the best of our knowledge, published literature has not yet investigated the possible desire for or potential utility of genetic counseling for individuals with lived experience and/or a family history of addictions. An understanding of how members of this population perceive risk and etiology, and how addictions in a family history can affect childbearing decisions is important and may aid genetic counselors in providing service to people with addictions and their family members.
Materials and Methods
Participants and Recruitment
Between September 2015 and January 2016, we recruited individuals aged 18 or older with self-reported lived experience and/or family history (defined as having one or more first-degree relatives) of alcohol addiction. Participants were recruited from web-based forums (e.g. Reddit and Facebook) that focus on recovery and family support for alcoholism (see supplemental material for full list). Specifically, we posted an invitation to participate in the study and a link to the survey.
Survey Tool
We designed a survey (see supplemental material, created and hosted on www.surveymonkey.com) that included questions about demographics (including personal and family history of alcohol addiction and experience with genetic counseling) and participants’ beliefs about the causes of alcohol addiction, perception of risk for recurrence of alcohol addiction, level of concern associated with the possibility of recurrence (for self, children and siblings), impact of alcohol addiction on childbearing decisions, experience with and attitudes towards genetic counseling. Participants were then shown a brief video explaining addiction genetic counseling (for transcript, see supplemental material), followed by a question regarding perceptions of their own potential to benefit from genetic counseling for alcohol addiction.
Analysis
Given that this was the first study in this area, we applied primarily descriptive statistics, but we also tested two exploratory hypotheses. Specifically, guided by the literature (Maio et al 2013), we hypothesized that perceiving genetic counseling to be useful would be associated with 1) greater importance attributed to genetics in the etiology of alcohol addiction, and 2) greater concern about recurrence of alcohol addiction (for self and/or children). To test the hypotheses, mean scores for attribution and concern were derived from Likert type scale responses. An attribution score for importance of various factors (such as genetics) in etiology was derived as follows: 1 = does not contribute at all, 2 = a less important contributor, 3 = an important contributor, 4 = the only cause. A score for concern about recurrence was derived in the same way: 1 = Not concerned at all, 2 = somewhat concerned, 3 = moderately concerned, 4 = extremely concerned. The perceived benefit of genetic counseling in addiction was treated as a binary variable, with those indicating: “No, I don’t think I would benefit” in one group, and those responding that they would “extremely”, “moderately” or “somewhat” benefit from genetic counseling in another. Wording for all questions (e.g. whether participants had heard about genetic counseling, risk perception and family history decisions, etc) together with response options are provided in Supplemental Material.
We highlight findings at a nominal significance threshold of p=.05. Statistical testing of the hypotheses, including Spearman’s Rho for correlation analyses and independent sample t-tests were carried out using SPSS software, Version 23.
Results
Demographics
A total of 155 individuals began the online survey, and 113 surveys were completed (answers provided to all items) by eligible individuals (as described above) and were used in our analysis. Demographic data for participants are presented in Table 1.
Table 1.
Demographics Characteristics of Respondents
| Characteristic | All (n=113) respondents n (%) | Respondents (n=69) who perceived benefit of GC for addiction n (%) | Respondents (n=44) who perceived no benefit of GC for addiction n (%) |
|---|---|---|---|
| Gender | |||
| Male | 55 (49%) | 32 (46%) | 23 (52%) |
| Female | 58 (51%) | 37 (54%) | 31 (48%) |
| Highest Completed Education | |||
| High School | 20 (18%) | 12 (17%) | 8 (18%) |
| Associate’s Degree | 12 (11%) | 8 (12%) | 4 (9%) |
| Bachelor’s Degree | 53 (47%) | 31 (45%) | 22 (50%) |
| Postsecondary School | 28 (25%) | 18 (26%) | 10 (23%) |
| Race | |||
| Caucasian | 103 (91%) | 60 (87%) | 43 (98%) |
| African American | 1 (1%) | 0 (0%) | 1 (2%) |
| Asian | 2 (2%) | 2 (3%) | 0 (0%) |
| Hispanic | 2 (2%) | 2 (3%) | 0 (0%) |
| Native American | 1 (1%) | 1 (1%) | 0 (0%) |
| Other | 4 (4%) | 4 (6%) | 0 (0%) |
| Personal Experience of Alcohol Addiction | |||
| Yes | 71 (63%) | 45 (65%) | 26 (59%) |
| No | 42 (37%) | 24 (35%) | 18 (41%) |
| Family History of Alcohol Addiction | |||
| Yes | 98 (87%) | 60 (87%) | 38 (86%) |
| 1st Degree Relative | 60 (61%) | 37 (54%) | 23 (52%) |
| 2nd or 3rd Degree Relative | 82 (73%) | 53 (77%) | 29 (66%) |
| Spouse | 5 (4%) | 4 (6%) | 1 (2%) |
| No | 15 (13%) | 9 (13%) | 6 (14%) |
| Mental Health History* | |||
| Personal History | 55 (49%) | 30 (44%) | 25 (57%) |
| Family History (in Relative(s) with Alcohol Addiction) | 52 (46%) | 33 (48%) | 19 (43%) |
Reported mental health diagnoses include depression, anxiety, schizophrenia, bipolar disorder
Perceptions of Causes of Alcohol Addiction
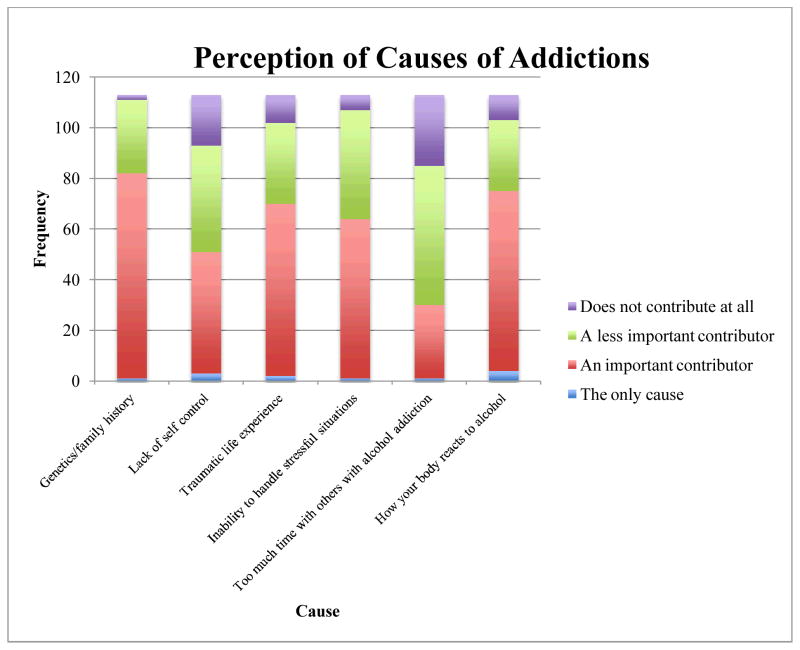
The large majority of respondents indicated more than one factor to be important in contributing to the development of alcohol addiction (see Figure 1, and Table 2).
Figure 1.
Attributions of Cause of Addictions
Table 2.
Attributions of Causes of Alcohol Addiction
| Cause | Mean attribution scores for causes of alcohol addiction* | ||
|---|---|---|---|
| All respondents (n=113) | Respondents (n=69) who perceived benefit of GC for addiction | Respondents (n=44) who perceived no benefit of GC for addiction | |
| Genetics/Family History | 2.72 | 2.80 | 2.59 |
| Lack of Self Control | 2.30 | 2.22 | 2.43 |
| Traumatic Life Experience | 2.54 | 2.48 | 2.64 |
| Inability to Handle Stressful Situations | 2.52 | 2.43 | 2.66 |
| Spending Too Much Time Around Others with Alcohol Addiction | 2.03 | 2.03 | 2.02 |
| How Your Body Reacts to Alcohol | 2.61 | 2.55 | 2.70 |
Scores range from 1–4, with higher scores reflecting greater perceived contributions
Perceptions of Risk for Recurrence
In total, 111 participants provided numeric estimates of risk for recurrence of alcohol addiction for children and siblings of someone with the condition (the remaining two participants indicated that they didn’t know). See Table 3.
Table 3.
Estimated probabilities of recurrence for relatives of people with alcohol addiction.
| Type of relative for whom chance of recurrence estimated | Estimated probability of recurrence | Estimated chance of ≥50% N(%) | Overestimated chance* N(%) | |||
|---|---|---|---|---|---|---|
| Min | Max | Mean | Mode | |||
| Children | 5 | 100 | 39 | 50 | 51(46) | 70(63) |
| Siblings | 5 | 80 | 30 | 50 | 30(27) | ---- |
Assuming a 28% chance for a child of a person with alcohol addiction to develop alcohol addiction themselves (based on the current population frequency of 7% for alcohol use disorders (National Institute of Alcohol Abuse and Alcoholism, 2015) and the reported four-fold increased risk for children of (Russell, 1990)
Concern Around Risk for Recurrence of Alcohol Addiction
Of the 68 participants who did not have an alcohol addiction, 63% (n = 43) reported some degree of concern for themselves to develop it in the future. Most participants (n = 81, 72%) were concerned to some degree about their children developing alcohol addiction, and 43% (n = 49) had similar concerns for their siblings. Overall mean concern scores were highest with respect to participants’ children and lowest with respect to their siblings (Table 4).
Table 4.
Concern About Risk of Alcohol Addiction
| Mean concern scores for risk of alcohol addiction* | |||
|---|---|---|---|
| All respondents^ | Respondents who perceived benefit of GC for Addiction | Respondents who perceived no benefit of GC for Addiction | |
| Concern for Self | 2.10 | 2.33 | 1.73 |
| Concern for Children | 2.27 | 2.39 | 2.09 |
| Concern for Siblings | 1.71 | 1.65 | 1.80 |
Scores range from 1–4 with higher scores indicating greater concern.
Mean scores for “concern for self” were calculated only for the 68 individuals who reported they did not already have a personal diagnosis of alcoholism (of these participants, 42 felt that genetic counseling would be helpful, and 26 felt it would not be useful). Mean scores for concern about siblings and children were calculated from all 113 participants (of whom 69 thought genetic counseling for addictions would be useful, and 44 thought it would not be helpful)
Effects of Alcohol Addiction on Childbearing Decisions
The majority of individuals (n = 71; 63%) reported that the presence of alcohol addictions in their personal or family history had not influenced their decisions about having children. Seven individuals (6%) reported that they were unaware that alcohol addiction was an issue when they were family planning. Six individuals (5%) reported that their decision had affected their family planning by either choosing to adopt children or to not have children. The remaining 29 respondents (26%) said that they were not sure if their personal/family history of alcohol addiction would influence their family planning, as they were not ready for children yet. The concern scores for these groups are shown in Table 5.
Table 5.
Concern About Risk for Alcohol Addiction Among Participants Who made Different Childbearing Decisions
| Effect of Personal/Family History of Alcohol Addiction on Childbearing Decisions | Mean Concern Score for Risk of Alcohol Addiction* | ||
|---|---|---|---|
| All Respondents | Respondents Who Perceived Benefit of GC for Addiction | Respondents Who Perceived No Benefit of GC for Addiction | |
| Adopting or not having children (n = 6) | 2.14 | 2.3 | 1.94 |
| No effect on decision to have children (n = 71) | 2.39 | 2.47 | 2.27 |
| Didn’t know this was an issue when having family (n = 7) | 2.86 | 3.33 | 2.5 |
| Unsure/not ready for children (n = 29) | 1.97 | 2.12 | 1.75 |
Scores range from 1–4 with higher scores indicating greater concern.
Personal Experience with, Attitudes Towards, and Perceptions of Genetic Counseling
Although 40% (n = 45) of respondents reported they had heard of genetic counseling before the survey, only 80% (n = 36) reported that they knew what it was upon further questioning. Only one individual had experienced genetic counseling (during a pregnancy, addictions were not addressed). When asked what healthcare providers they would consider consulting for alcohol addiction-related advice around things such as risk factors or risk-reducing strategies, 16 respondents (15%) said they would consider asking a genetic counselor, with the most common provider reported was a therapist or counselor (n = 82; 75%).
After viewing a description of genetic counseling for addictions (created from the definition of psychiatric genetic counseling and modified to fit addiction (see supplemental material)), 69 individuals (62%) felt that they would experience some degree of benefit from genetic counseling. Demographic data for those who felt that genetic counseling would and would not be useful are presented in Table 1 (for descriptive purposes only).
The greater the importance attributed to genetics in the etiology of alcohol addiction, the more likely participants were to perceive genetic counseling as potentially beneficial (ρ = .21, df = 111, p = .024). No significant correlations were found between perceived benefit of addiction genetic counseling and any other perceived causes.
An independent sample t-test assessing participants’ concern for their children and their perceptions of their potential to benefit from genetic counseling (Table 3) revealed no significant relationship between these variables (t = 1.51, df = 111, p = ns), however, an independent sample t-test did find a significant relationship between unaffected individuals’ concern level for themselves and their perceived benefit of genetic counseling (t = 2.37, df = 66, p = .021).
Discussion
This was the first study (to our knowledge) to explore causal attributions for and perceptions of risk for recurrence of alcohol addiction among people with lived experience and their family members. Participants generally appreciated the complex etiology of alcohol addiction, an understanding that has been observed in studies investigating perceived causes of other psychiatric conditions (Meiser, Mitchell, McGirr, Van Herten, & Schofield, 2005; Schulz et al., 1982). Also similar to many study findings in the context of other psychiatric disorders (Austin, Smith, & Honer, 2006; Costain et al., 2014; Quaid, Aschen, Smiley, & Nurnberger, 2001; Trippitelli, Jamison, Folstein, Bartko, & DePaulo, 1998), participants in this study tended to overestimate the chance for first degree relatives to develop the same condition as their affected relative. Despite most participants overestimating the chance of recurrence in the family, a wide range of probabilities was reported, with some participants grossly underestimating. This variability in perceptions has been observed for other conditions, such as breast and colon cancer (Bjorvatn et al., 2007; Lloyd et al., 1996).
Most participants indicated that their personal or family history of alcohol addiction had not influenced their childbearing decisions, but for 5% it had led to a decision not to have biological children. This is much lower than other studies have found when looking at the effect of other psychiatric illness, such as bipolar disorder or schizophrenia, in a family on childbearing decisions (Austin et al., 2006; Lyus, 2007; Meiser et al., 2007; Schulz et al., 1982). It was interesting to note that those who were unaware that alcohol addiction was a relevant issue when they were having children reported the highest relative levels of concern. A quarter of participants (26%) reported being unsure of how their decisions would be influenced, as they were not ready to start a family. This group reported a relatively lower average concern for their children to develop an alcohol addiction (See Table 5) – one potential explanation for this observation is that perhaps the lower concern was a result of recurrence risks being considered less salient for participants who self-identified as not being ready to start a family.
Less than one third of participants reported knowing what genetic counseling was, and the majority of participants had never heard of a genetic counselor before participating in this study. These findings closely mirror those of other studies that have explored awareness of genetic counseling in other populations (Maio, Carrion, Yaremco, & Austin, 2013; Riesgraf, McCarthy Veach, MacFarlane, & LeRoy, 2015, Goldberg et al., 2015).
Accordingly, despite the fact that genetic counseling is relevant to, and potentially beneficial for this population, none of our participants had received it. This gap in the delivery of clinical genetics services to individuals with psychiatric disorders and their families has been demonstrated previously in the context of schizophrenia (Hunter, Hippman, Honer, & Austin, 2010). However, our data extend previous work, showing that similar problems are encountered in the context of addictions.
Our data suggest that two subgroups of participants - those who felt that genetics/family history contributed highly to the development of alcohol addiction, and those with no personal history of alcohol addiction who were more concerned about chances for themselves to develop alcohol problems later on - may be more likely to perceive a benefit of genetic counseling. While this may be important information for genetic counselors and other healthcare providers to help identify who may be most interested in genetic counseling, the overall context for these findings was one where most participants perceived genetic counseling to be potentially beneficial to them.
In the context of alcohol addiction, genetic counseling could be implemented to help patients and their families to gain a better understanding of what we know from research regarding how genetic and environmental factors contribute to the development of alcohol addiction. This understanding can be used as a framework to help families to understand strategies that they can use (e.g. good quality regular sleep, good nutrition, exercise, social support) to protect mental health. Additionally, genetic counseling can help people to better understand the chances of recurrence of alcohol addiction in other family members. Genetic counselors can also work with individuals with lived experience of alcohol addiction and their families to uncover and address any psychological issues that can be associated with addiction such as guilt and shame (Bennett, 1995; Ehrmin, 2001; Meehan et al., 1996).
Limitations
The participants in this study were primarily Caucasian, well-educated and potentially highly motivated (as they were identified through alcohol addiction support resources). It is possible that a more diverse group of individuals (e.g. from different ethnic groups, cultural backgrounds, or having different levels of educational attainment) may feel differently about the benefit of genetic counseling for addiction and may have differing perceptions around the causes and recurrence of addiction. We did not provide a definition of addiction or alcoholism at the beginning of the survey and therefore it is possible that participants were working with different concepts of alcoholism. The component of the survey that addressed participants’ perceptions of causes was closed-ended, and though the options were derived from the authors’ collective experience of working with the study population, it is possible that other factors were perceived as potential causes. Last, all participants completed the questions regarding their level of concern for children and siblings to develop alcohol addiction. Therefore, assuming that some respondents would not have had these kinds of relatives, they may have been more likely to respond “not at all concerned” – so perhaps the real level of concern amongst those who actually do have children and siblings is higher than reported here.
Future directions
Future larger scale studies could provide more insight into possible factors that influence the perceived benefit of addiction genetic counseling. Pilot studies to explore the impact and outcome of genetic counseling for alcohol addiction could be implemented, together with investigations of attitudes towards and comfort with addiction genetic counseling among practicing genetic counselors in order to understand what education needs to be provided to the profession. Finally, education to this population regarding genetic counseling services would increase awareness and possibly uptake.
Conclusions
To our knowledge, this is the first study to explore the perceptions of risk for recurrence and etiology as well as the possible benefit of genetic counseling among individuals at risk for and with lived experience of alcohol addiction. While none of the participants had received genetic counseling for alcohol addiction, the majority of the participants felt that it could be beneficial. Genetic counseling for this population could help clarify their misconceptions about recurrence risk and facilitate a better understanding of the many causes of addictions. Genetic counseling may also lessen the impact of alcohol addiction on an individual and family by encouraging risk reduction strategies and reducing the psychological burden of the condition by addressing the guilt, shame, and stigma of addictions. Further research is warranted into the outcomes of genetic counseling for alcohol addiction and an increased effort for awareness of the availability of genetic counseling is needed for this population.
Supplementary Material
Acknowledgments
The authors would like to thank Janice Edwards and Peggy Walker for their feedback and edits, and Max Tiller for assistance with statistics and data analysis. The authors were grateful to receive funding support for this study through the National Society of Genetic Counselors (NSGC) Psychiatric Special Interest Group. JA was supported by the Canada Research Chairs program and BC Mental Health and Substance Use Services.
Footnotes
Human Studies and Informed Consent: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all individual participants included in the study. The study was approved by the University of South Carolina Ethics Review Board (Pro00047939).
Conflict of Interest Authors: FK, VV, TH, and JA declare that they have no conflict of interest
Animal Studies: No animal studies were carried out by the authors for this article
References
- Agrawal A, Lynskey MT. Are there genetic influences on addiction: Evidence from family, adoption and twin studies. Addiction. 2008 doi: 10.1111/j.1360-0443.2008.02213.x. http://doi.org/10.1111/j.1360-0443.2008.02213.x. [DOI] [PubMed]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Washington, DC: 2013. [Google Scholar]
- Andrighetti H, Semaka A, Stewart SE, Shuman C, Hayeems R, Austin J. Obsessive-Compulsive Disorder3: The Process of Parental Adaptation and Implications for Genetic Counseling. 2015 doi: 10.1007/s10897-015-9914-9. http://doi.org/10.1007/s10897-015-9914-9. [DOI] [PMC free article] [PubMed]
- Austin JC, Honer WG. The genomic era and serious mental illness: a potential application for psychiatric genetic counseling. Psychiatric Services (Washington, DC) 2007;58(2):254–261. doi: 10.1176/ps.2007.58.2.254. http://doi.org/10.1176/appi.ps.58.2.254. [DOI] [PubMed] [Google Scholar]
- Austin JC, Honer WG. Psychiatric genetic counselling for parents of individuals affected with psychotic disorders: A pilot study. Early Intervention in Psychiatry. 2008;2(2):80–89. doi: 10.1111/j.1751-7893.2008.00062.x. http://doi.org/10.1111/j.1751-7893.2008.00062.x. [DOI] [PubMed] [Google Scholar]
- Austin JC, Smith GN, Honer WG. The genomic era and perceptions of psychotic disorders: Genetic risk estimation, associations with reproductive decisions and views about predictive testing. American Journal of Medical Genetics. 2006;141B(8):926–928. doi: 10.1002/ajmg.b.30372. [DOI] [PubMed] [Google Scholar]
- Bennett L. Accountability for alcoholism in American families. Social Science & Medicine. 1995;40(1):15–25. doi: 10.1016/0277-9536(94)00123-b. [DOI] [PubMed] [Google Scholar]
- Biesecker BB. Genetic counseling for mental illness: Goals resemble counseling goals for other common conditions [1] Clinical Genetics. 2006;69(1):93–94. doi: 10.1111/j.1399-0004.2006.00554a.x. http://doi.org/10.1111/j.1399-0004.2006.00554a.x. [DOI] [PubMed] [Google Scholar]
- Bjorvatn C, Eide GE, Hanestad BR, Øyen N, Havik OE, Carlsson A, Berglund G. Risk perception, worry and satisfaction related to genetic counseling for hereditary cancer. Journal of Genetic Counseling. 2007;16(2):211–222. doi: 10.1007/s10897-006-9061-4. http://doi.org/10.1007/s10897-006-9061-4. [DOI] [PubMed] [Google Scholar]
- Comorbidity: Addiction and Other Mental Illnesses. National Institute on Drug Abuse; 2010. [Google Scholar]
- Costain G, Esplen MJ, Toner B, Hodgkinson Ka, Bassett AS. Evaluating Genetic Counseling for Family Members of Individuals with Schizophrenia in the Molecular Age. Schizophrenia Bulletin. 2014;40(1):88–99. doi: 10.1093/schbul/sbs124. http://doi.org/10.1093/schbul/sbs124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehrmin JT. Unresolved feelings of guilt and shame in the maternal role with substance-dependent African American women. Journal of Nursing Scholarship3: An Official Publication of Sigma Theta Tau International Honor Society of Nursing/Sigma Theta Tau. 2001;33:47–52. doi: 10.1111/j.1547-5069.2001.00047.x. http://doi.org/http://dx.doi.org/10.1111/j.1547-5069.2001.00047.x. [DOI] [PubMed] [Google Scholar]
- Goldberg D, Bocian M, Austin JC, Grody WW, Osann K, Singh K. Measuring Awareness and Identifying Misconceptions About Genetic Counseling Services and Utilizing Television to Educate. 2015. [Google Scholar]
- Heath A, Bucholz K, Madden P, Dinwiddie S, Slutske W, Bierut L, … Martin N. Genetic and environmental contributions to alcohol dependence risk in a national twin sample: cinsistency of findings in men and women. Psychological Medicine. 1997;27(6):1381–96. doi: 10.1017/s0033291797005643. [DOI] [PubMed] [Google Scholar]
- Hippman C, Ringrose A, Inglis A, Cheek J, Albert A, Remick R, … Austin JC. A pilot randomized clinical trial evaluating the impact of genetic counseling for serious mental illnesses. Journal of Clinical Psychiatry. 2016;77(2):e190–e198. doi: 10.4088/JCP.14m09710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter MJ, Hippman C, Honer WG, Austin JC. Genetic counseling for schizophrenia: A review of referrals to a provincial medical genetics program from 1968 to 2007. American Journal of Medical Genetics. 2010;152A(1):147–152. doi: 10.1002/ajmg.a.33193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inglis a, Koehn D, McGillivray B, Stewart SE, Austin J. Evaluating a unique, specialist psychiatric genetic counseling clinic: uptake and impact. Clinical Genetics. 2015;3:1–7. doi: 10.1111/cge.12415. http://doi.org/10.1111/cge.12415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler K, Heath A, Neale M, Kessler REL. A Population-Based Twin Study of Alcoholism in Women. Journal of the American Medical Association. 1992;268(14):1877–1882. [PubMed] [Google Scholar]
- Lloyd S, Watson M, Waites B, Meyer L, Eeles R, Ebbs S, Tylee a. Familial breast cancer: a controlled study of risk perception, psychological morbidity and health beliefs in women attending for genetic counselling. British Journal of Cancer. 1996;74(3):482–487. doi: 10.1038/bjc.1996.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyus VL. The importance of genetic counseling for individuals with schizophrenia and their relatives: Potential clients’ opinions and experiences. American Journal of Medical Genetics, Part B: Neuropsychiatric Genetics. 2007;144(8):1014–1021. doi: 10.1002/ajmg.b.30536. http://doi.org/10.1002/ajmg.b.30536. [DOI] [PubMed] [Google Scholar]
- Maio M, Carrion P, Yaremco E, Austin JC. Awareness of genetic counseling and perceptions of its purpose: a survey of the Canadian public. Journal of Genetic Counseling. 2013;22(6):762–770. doi: 10.1007/s10897-013-9633-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meehan W, O’Connor LE, Berry JW, Weiss J, Morrison a, Acampora a. Guilt, shame, and depression in clients in recovery from addiction. Journal of Psychoactive Drugs. 1996 doi: 10.1080/02791072.1996.10524385. http://doi.org/10.1080/02791072.1996.10524385. [DOI] [PubMed]
- Meiser B, Mitchell PB, Kasparian NA, Strong K, Simpson JM, Mireskandari S, … Schofield PR. Attitudes towards childbearing, causal attributions for bipolar disorder and psychological distress: a study of families with multiple cases of bipolar disorder. Psychological Medicine. 2007;37(11):1601–1611. doi: 10.1017/S0033291707000852. [DOI] [PubMed] [Google Scholar]
- Meiser B, Mitchell PB, McGirr H, Van Herten M, Schofield PR. Implications of genetic risk information in families with a high density of bipolar disorder: an exploratory study. Social Science & Medicine. 2005;60(1):109–118. doi: 10.1016/j.socscimed.2004.04.016. [DOI] [PubMed] [Google Scholar]
- National Institute of Alcohol Abuse and Alcoholism. Alcohol Facts and Statistics. 2015. [Google Scholar]
- Quaid Ka, Aschen SR, Smiley CL, Nurnberger JI. Perceived Genetic Risks for Bipolar Disorder in a Patient Population: An Exploratory Study. Journal of Genetic Counseling. 2001;10(1):41–51. http://doi.org/10.1023/A:1009403329873. [Google Scholar]
- Resta R, Biesecker BB, Bennett RL, Blum S, Hahn SE, Strecker MN, Williams JL. A new definition of genetic counseling: National Society of Genetic Counselors’ Task Force report. Journal of Genetic Counseling. 2006;15(2):77–83. doi: 10.1007/s10897-005-9014-3. http://doi.org/10.1007/s10897-005-9014-3. [DOI] [PubMed] [Google Scholar]
- Riesgraf RJ, McCarthy Veach P, MacFarlane IM, LeRoy BS. Perceptions and Attitudes About Genetic Counseling Among Residents of a Midwestern Rural Area. Journal of Genetic Counseling. 2015;24(4):565–579. doi: 10.1007/s10897-014-9777-5. [DOI] [PubMed] [Google Scholar]
- Russell M. Prevalence of alcoholism among children of alcoholics. Children of Alcoholics: Critical Perspectives. 1990:17. [Google Scholar]
- Schulz PM, Schulz SC, Dibble E, Targum SD, van Kammen DP, Gershon ES. Patient and family attitudes about schizophrenia: implications for genetic counseling. Schizophrenia Bulletin. 1982;8:504–513. doi: 10.1093/schbul/8.3.504. http://doi.org/10.1093/schbul/8.3.504. [DOI] [PubMed] [Google Scholar]
- Trippitelli CL, Jamison KR, Folstein MF, Bartko JJ, DePaulo JR. Pilot study on patients’ and spouses’ attitudes toward potential genetic testing for bipolar disorder. The American Journal of Psychiatry. 1998;155(7):899–904. doi: 10.1176/ajp.155.7.899. http://doi.org/10.1176/ajp.155.7.899. [DOI] [PubMed] [Google Scholar]
- Tsuang M. Genetic Counseling for Psychiatric Patients and Their Families. The American Journal of Psychiatry. 1978 Dec; doi: 10.1176/ajp.135.12.1465. [DOI] [PubMed] [Google Scholar]
- Verhulst B, Neale M, Kendler K. The heritability of alcohol use disorders: a meta-analysis of twin and adoption studies. 2015;45(5):1061–1072. doi: 10.1017/S0033291714002165. http://doi.org/10.14440/jbm.2015.54.A. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.