Abstract
Background
Timely access to orthopedic trauma surgery is essential for optimal outcomes. Regionalization of some types of surgery has shown positive effects on access, timeliness and outcomes. We investigated how the consolidation of orthopedic surgery in 1 Canadian health region affected patients requiring hip fracture surgery.
Methods
We retrieved administrative data on all regional emergency department visits for lower-extremity injury and all linked inpatient stays from January 2010 through March 2013, identifying 1885 hip-fracture surgeries. Statistical process control and interrupted time series analysis controlling for demographics and comorbidities were used to assess impacts on access (receipt of surgery within 48-h benchmark) and surgical outcomes (complications, in-hospital/30-d mortality, length of stay).
Results
There was a significant increase in the proportion of patients receiving surgery within the benchmark. Complication rates did not change, but there appeared to be some decrease in mortality (significant at 6 mo). Length of stay increased at a hospital that experienced a major increase in patient volume, perhaps reflecting challenges associated with patient flow.
Conclusion
Regionalization appeared to improve the timeliness of surgery and may have reduced mortality. The specific features of the present consolidation (including pre-existing interhospital performance variation and the introduction of daytime slates at the referral hospital) should be considered when interpreting the findings.
Abstract
Contexte
En traumatologie, l’accès rapide à la chirurgie orthopédique est essentiel pour l’obtention de résultats optimaux. La régionalisation de certains types de chirurgie a eu des effets positifs sur l’accès aux soins, leur rapidité et leurs résultats. Nous avons vérifié l’effet qu’a eu la consolidation des soins chirurgicaux orthopédiques dans une région sanitaire canadienne sur les patients qui ont eu recours à la chirurgie pour une fracture de la hanche.
Méthodes
Nous avons obtenu les données administratives concernant toutes les consultations dans les services d’urgence régionaux pour des blessures aux membres inférieurs et nous les avons corrélées avec les séjours hospitaliers de janvier 2010 à mars 2013. Nous avons ainsi recensé 1885 chirurgies pour fracture de la hanche. Nous avons utilisé la maîtrise statistique des procédés et le modèle chronologique interrompu et nous avons tenu compte des caractéristiques démographiques et des comorbidités pour évaluer les impacts sur l’accès aux interventions (attente limite de 48 h pour obtenir la chirurgie) et leurs résultats (complications, mortalité perhospitalière à 30 j et durée des séjours).
Résultats
On a noté une augmentation significative de la proportion de patients traités par chirurgie à l’intérieur des délais. Les taux de complications n’ont pas varié, mais il semble y avoir eu une certaine diminution de la mortalité (significative à 6 mois). La durée des séjours a augmenté dans un hôpital qui a connu un accroissement majeur de sa clientèle, témoignant peut-être de difficultés liées à l’afflux de patients.
Conclusion
La régionalisation a semblé améliorer l’accès rapide à la chirurgie et pourrait avoir réduit la mortalité. Il faut tenir compte des caractéristiques spécifiques de la présente consolidation (y compris la variation préexistante du rendement interhospitalier et la création de listes de jour à l’hôpital de référence) avant d’interpréter ces conclusions.
Hip fractures are an important source of morbidity and mortality among older adults in Canada and elsewhere. Studies have shown that timely access to hip fracture surgery decreases mortality and may have positive impacts on length of stay (LOS) in hospital and surgical complications.1–4 The Canadian Institute for Health Information has set a national benchmark for hip fracture repair to 48 hours from time of admission to hospital.3
Consolidation or regionalization of surgical care is common in many Western countries and is widely considered to be best practice.5–7 In particular, the regionalization of trauma care has been shown to reduce mortality.8,9 Moreover, there is consistent evidence that high-volume surgeons/hospitals achieve superior outcomes to low-volume surgeons/hospitals (e.g., reduced mortality, adverse events, and/or LOS).5,10–13
On the other hand, regionalization has not shown universally positive outcomes. An American study of various consolidations at 19 hospitals found that complications decreased for 2 procedures (including total hip replacement), increased for 3, and remained unchanged for 2.6 A Canadian study found that the consolidation of acute care surgery increased wait times owing to the time required to transfer patients who presented at nonreferral hospitals.14
There is a lack of evidence on the impacts of consolidating orthopedic trauma surgery. In one Canadian health region, the consolidation of all high-acuity procedures at designated hospitals was associated with reduced LOS and no increase in mortality; however, this consolidation was not specific to orthopedic surgery and, furthermore, was accompanied by other major changes, such as a dramatic alteration to the nurse staffing model.15 Another study described the consolidation of orthopedic trauma surgery in a different Canadian region; however, that study investigated only impacts on residents, not patients.16 Accordingly, it was important to investigate how such a consolidation affected access and outcomes with respect to hip fractures.
The Winnipeg Regional Health Authority (WRHA) is a Canadian regional health system whose 6 hospitals serve a population of approximately 700 000. Prior to 2012, orthopedic trauma surgery had already been consolidated at 4 sites (hospitals A, B, C and D). In January 2012, a further consolidation saw orthopedic trauma patients redistributed from hospital B to hospital A; the 2 facilities are about 16 km apart. Hospital C remained the site for all complex trauma surgery and for out-of-province patients; hospital D continued to provide orthopedic trauma surgery as before. Concurrently, hospitals B and D became the primary locations for elective hip and knee replacements. The consolidation was accompanied by the introduction of daytime surgical slates at hospital A in order to enable it to accommodate a greater volume of surgeries. Daytime slates already existed 2 days per week at hospital D, and this did not change during the study period. The initiative was intended to promote a better match between bed capacity and demand, improve patient flow, minimize disruptions to elective slates from emergency needs, and improve patient outcomes by ensuring that surgeons could perform a high volume of the same type of surgery.
The 2012 consolidation built on a multicomponent intervention that the WRHA had introduced in 2008 to redress 7 identified sources of delay to hip fracture surgery; components included several changes to facilitate the transfer of patients from and back to rural hospitals, creation of daytime orthopedic trauma slates at 1 hospital, elimination of mandatory internal medicine consultations before surgery, clarification of standards regarding patients on clopidogrel, and provider education about the importance of timely surgery.4 The proportion of patients receiving surgery within the 48-hour benchmark rose from 67% before 2008 to 85% after 2008, with concomitant decreases in LOS and mortality.4 It should be noted that the 2008 intervention was well established before the present study’s “preintervention” period began.
The objective of this study was to investigate the impact of consolidation on patients requiring hip fracture surgery, in terms of access (receipt of surgery within the 48-hr benchmark) and surgical outcomes (complications, inhospital/30-day mortality, and LOS). The preintervention period extended from January 2010 through December 2011; the postintervention period was from January 2012 through March 2013.
Methods
Data sources
We retrieved data on all regional emergency department (ED) visits for lower-extremity injuries and all linked inpatient hospital visits from Jan. 1, 2010, through Mar. 31, 2013; inpatient records were also linked to data on date/time of surgery and 30-day mortality. The ED and inpatient data came from regional administrative databases, the operative log data came from electronic files provided by each hospital, and the mortality data came from Vital Statistics.
Among the inpatient admissions we identified were patients with hip fracture diagnoses (ICD-10 S72 codes) and patients having hip surgery. There was considerable overlap between these 2 categories; of all patients with a diagnosis of hip fracture, 94% received hip surgery. We considered hip fracture surgery patients to be those who fit into both categories. We were unable to identify patients who may have had orthopedic trauma surgery without being admitted or who presented with a condition other than lower-extremity injury.
In keeping with our methodology in a prior study,14 we defined the patient journey as beginning with the first presentation to a WRHA ED (time of registration) and including the index ED visit, any ED attendances occurring within 24 hours of this visit, the first subsequent inpatient admission to any WRHA hospital and any subsequent acute care admissions reflecting inpatient transfers (transfer noted in the “transfer-to” field and/or admission occurring within 6 h of the previous discharge). We did not include transfers to rehabilitation units or facilities, as there were some concerns about data quality.
Complications (adverse events) were defined as the receipt of an ICD-10 T code that was not identified as a preadmission comorbidity (T codes are assigned for infection, hemorrhage, mechanical complications and “other complications” of procedures or devices). Our measure of mortality combined in-hospital and 30-day mortality (i.e., 30 d from inpatient admission). We included the commonly studied outcome of LOS for completeness, much as we recognize that LOS is affected by numerous factors unrelated to surgical outcomes.
This study was part of a broader evaluation that also assessed (but did not detect significant change in) rates of admission and readmission to institutions, and included some analyses of nonoperative patients; details are available from the authors.
Statistical analysis
Patient outcomes were analyzed with statistical process control and interrupted time series analysis. Statistical process control involves plotting the data on a control chart to evaluate the timing and magnitude of any changes.17 Results are tested for significance according to rules that include 1 data point outside the upper and lower control limits, 6 consecutive data points ascending or descending, and 9 consecutive data points above or below the mean.
Interrupted time series analysis enabled us to test the significance of intervention effects (measured at 6 and 12 mo) and any changes in trend, while controlling for patient characteristics (age, sex, out-of-region origin, Charlson comorbidity score). As a sensitivity analysis, we subsequently included type of procedure (internal fixation v. arthroplasty); however, this variable was not statistically significant in any of the models and did not affect the direction or significance of other effects.
Multiple linear regression was used for continuous variables (after log-transforming those with skewed distributions), and logistic regression for binary variables. Before choosing this method, we used the Durbin–Watson test to check for autocorrelation of errors in all continuous data.18 These tests did not show significant results (the Durbin–Watson statistic was near 2), indicating that it was unnecessary to use a procedure, such as autoregressive integrated moving average, that controls for autocorrelation.
Results
We identified 4595 inpatient admissions; of these, 1855 fit our definition of hip fracture surgery patients. We determined that an additional 31 hip-fracture surgery patients whose hospital stays extended beyond March 2013 were missing from the inpatient data set. Of these, 22 had presented in March 2013, and no more than 3 had presented in any prior month. Accordingly, we excluded all patients who presented in March 2013 from the analysis, leaving a sample size of 1854 patients.
Characteristics of the sample
As intended, hospital B ceased to provide hip fracture surgery, and most of the patients it would otherwise have served were absorbed by hospital A (Table 1). Patient demographic characteristics (sex and age) remained constant pre- and postconsolidation, but there was some increase in the proportion of patients with comorbidities, especially multiple comorbidities (Mantel–Haenszel χ2 = 4.09, p = 0.043). There was also a significant increase in the proportion of patients who were transferred in from an out-of-region hospital (odds ratio [OR] 1.86, p < 0.001); this was not logically related to the consolidation and may reflect the provincial amalgamation of certain health regions in mid-2012 or coincidental orthopedic shortages in some regions. The proportion of within-region transfers for surgery also increased significantly postconsolidation (OR 1.73 p = 0.007); specifically, more patients were transferred from hospital B to hospital A. However, such transfers remained relatively uncommon, as most hip-fracture patients travel to the ED by ambulance and are triaged to the appropriate site by paramedics. The frequency of hip-fracture presentations and surgeries did not show clear time trends or seasonality, although there appeared to be some increase in the operative rate following the consolidation (data not shown).
Table 1.
Sample characteristics
| Characteristic | Group; no. (%) | |
|---|---|---|
| Preintervention (n = 1145) | Postintervention (n = 709) | |
| Hospital of admission | ||
| A | 331 (28.9) | 369 (52.0) |
| B | 309 (27.0) | 0 (0) |
| C | 182 (15.9) | 139 (19.6) |
| D | 323 (28.2) | 201 (28.4) |
| Sex | ||
| Male | 307 (26.8) | 205 (28.9) |
| Female | 838 (73.2) | 504 (71.1) |
| Age, yr | ||
| 0–17 | 4 (0.3) | 5 (0.7) |
| 18–64 | 137 (12.0) | 90 (12.7) |
| 65–79 | 261 (22.8) | 172 (24.3) |
| ≥ 80 | 743 (64.9) | 442 (62.3) |
| No. of comorbidities | ||
| 0 | 682 (59.6) | 398 (56.1) |
| 1 | 351 (30.7) | 219 (30.9) |
| ≥ 2 | 112 (9.8) | 92 (13.0) |
| Origin | ||
| WRHA | 1107 (96.7) | 658 (92.8) |
| Non-WRHA site | 38 (3.3) | 51 (7.2) |
| Transferred for surgery | ||
| No | 1081 (94.4) | 645 (91.0) |
| Yes | 64 (5.6) | 64 (9.0) |
WRHA = Winnipeg Regional Health Authority.
Patient access
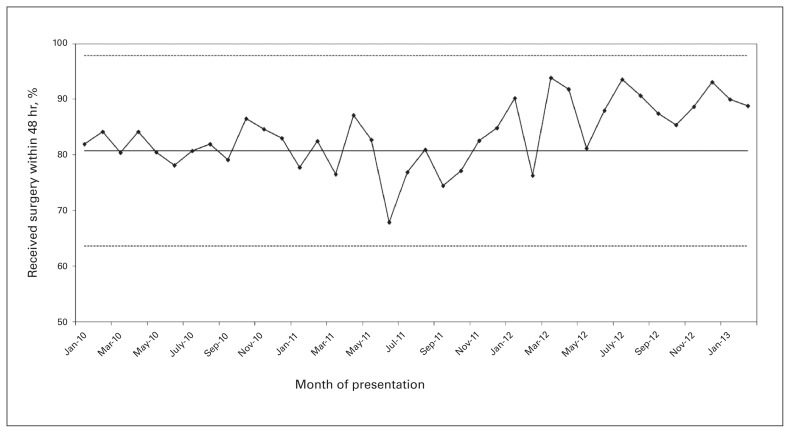
Time to surgery was defined as time from first registration at any WRHA ED to receipt of first surgical intervention on the hip. The proportion of patients receiving surgery within the 48-hour benchmark increased significantly (Fig. 1), rising from 80.8% to 88.4%. Regression modelling, controlling for patient sex, age, out-of-region origin and comorbidities, confirmed this result (Appendix 1, Table A-1, available at canjsurg.ca/000517-a1). The change detected was immediate; there was no indication of an ongoing increase or decrease.
Fig. 1.
Receipt of hip fracture surgery within 48 h. The solid line represents the mean, and the dotted lines represent the upper and lower control limits, all calculated based on the preintervention period.
The consolidation, of course, entailed that patients who would have otherwise had surgery at hospital B instead had it at hospital A. This may have affected the timeliness of surgery, as hospital A had the best performance on the 48-hour benchmark (91.9%), and hospital B had the worst (68.9%; notably, hospital B was also a site for emergency general surgery, which competed with orthopedic trauma for operating room time). When we controlled for hospital in the analysis, the intervention effect only approached significance at 6 and 12 months (data not shown).
As noted earlier, the consolidation was accompanied by the introduction of daytime surgical slates for orthopedic trauma. Post hoc analyses (data not shown) showed that the proportion of patients receiving surgery during the day shift (7:30 am to 4:30 pm) increased significantly. Including time of day in the prediction of time to surgery did not negate the intervention effect; however, the availability of daytime slates may have improved the timeliness of surgery in general by preventing backlogs. The relative contribution of daytime slates versus consolidation per se could not be assessed, as the 2 were introduced concurrently.
Surgical outcomes
Statistical process control analyses (not shown) detected no postconsolidation trend in the rate of surgical complications or in-hospital/30-day mortality. However, regression analysis with controls, while also finding no significant change in complications, suggested a decrease in mortality that was significant at 6 months but that only approached significance at 12 months (Appendix 1, Table A-2, available at canjsurg.ca/000517-a1).
Regression modelling showed that LOS had been falling before the consolidation and began to rise thereafter, with a significant increase apparent at 6 and 12 months (Appendix 1, Table A-3, available at canjsurg.ca/000517-a1). Statistical process control analysis did not detect a region-wide intervention effect, but did find that LOS at hospital A rose markedly at the time of consolidation, remaining well above its preintervention mean and typically above the preintervention mean for hospitals A and B combined (data not shown).
Discussion
The consolidation succeeded in providing patients with more timely hip-fracture surgery: there was a significant increase in the proportion of patients receiving surgery within 48 hours. This increase seems to be at least partially attributable to the redirection of patients from one specific hospital to another; it also seems plausible that the introduction of daytime slates was an important factor in allowing hospital A to maintain its short wait times while absorbing a large increase in volume. The increased timeliness of surgery may have translated into reduced mortality; no impact on the rate of complications was observed.
Length of stay showed some increase, specifically at hospital A; this seems more likely to have reflected changes in patient flow (efficiency) rather than changes in patient outcomes (quality/safety). It is plausible that at hospital A, the changes in bed allocation and patient mix put increased strain on rehabilitation beds and/or discharge-planning resources, resulting in longer stays. It should also be noted that following the consolidation many nurses left hospital A, resulting in bed closures; it is unclear how this may have affected bed utilization.
This study’s findings contrast with those of an analysis of the consolidation of acute care surgery in the same region.14 In the latter case, consolidation was associated with longer time to surgery; although the efficiency of within-hospital processes appeared to increase, any time savings were more than offset by the time required to transfer patients from nonreferral to referral hospitals. In the present study, consolidation reduced time to surgery, and few transfers occurred. The divergent findings can be explained in terms of the different surgical populations involved. Patients with hip fracture almost always present to hospital by ambulance, and emergency medical services staff can ensure that all patients with lower-extremity injuries are taken to a referral hospital. Indeed, as part of the consolidation, the WRHA implemented an algorithm to facilitate this. In contrast, about one-third of the acute care surgery patients who resided within the region did not call an ambulance, but instead presented directly to hospital; when this turned out to be a nonreferral hospital, their surgery was delayed owing to the need for a transfer. These contrasting findings suggest that surgical consolidation is more likely to improve access when it can be reliably ensured that patients with relevant symptoms present to a referral hospital.
Limitations
This study has certain limitations. We could not identify patients who may have presented with a condition other than lower-extremity injury (e.g., lower-extremity pain, major trauma). The range and specificity of patient characteristics and outcomes studied were limited by the variables present in administrative databases; clearly, each studied outcome is affected by multiple patient factors, of which we could control only a few. Also, the aggregate nature of the data used made it impossible to highlight unique outcomes (positive or negative) that some patients may have experienced. We were unable to measure the segment of the patient journey before presentation at an ED; thus, although it seems highly likely that patients were better off travelling an extra 16 km to take advantage of a 92% rather than a 69% rate of within-benchmark surgery, our analyses did not factor in the length of the ambulance trip. Lack of randomization was also an important limitation, but was offset by the long interrupted time series design; a randomized controlled trial of this complex, multihospital intervention would have been impracticable. The unequal length of the pre- and postintervention periods (24 v. 15 mo) might have introduced a seasonality effect, although this seems unlikely, as no seasonal pattern could be detected.
Perhaps the study’s greatest limitation was its inability to distinguish the impacts of the consolidation per se, the specific hospitals involved, and the addition of daytime slates. Although the change we studied had fewer components than the intervention package introduced in 2008, it was nonetheless composite and, moreover, built upon prior measures that had already improved timeliness and related outcomes.4 This inhibits generalization of the findings to other potential consolidations of orthopedic surgery. However, it is important to recognize that the regionalization of surgery is never a simple, single-component intervention. Regionalization necessarily involves moving patients from certain hospitals to others (thus, its outcomes will inevitably be affected by any pre-existing performance variation) and increases the volume of the relevant type of surgery at the referral hospital (thus, there needs to be some mechanism to ensure that this hospital’s operating rooms can manage the new referrals). The present study suggests that it is probably beneficial to redistribute patients from a hospital with longer wait times to one with shorter wait times, that daytime slates may help a referral hospital absorb increased volume, and that an increased contingent of hip-fracture patients may pose challenges associated with patient flow. Such considerations are integral to the implementation of surgical consolidation and must be addressed by any region contemplating a similar intervention. In general, it is important to consider the unintended impacts that consolidation might bring to programs involved in pre- and postsurgical components of the patient journey (e.g., emergency medical services, EDs, rehabilitation/geriatric services) and to all affected locations (particularly when one urban region serves multiple rural areas).
Conclusion
To our knowledge, this is the first study to investigate how the consolidation of orthopedic trauma surgery affects patients. We found a positive impact on the timeliness of surgery and a potential improvement in mortality, but were unable to determine the relative contribution of interlinked intervention components and contextual factors to these results. Thus, although our findings were broadly supportive of regionalization, regions undertaking such an enterprise should ensure that mechanisms are in place to fully evaluate its impacts on patient access and outcomes.
Acknowledgements
We are most grateful to Miroslava Svitlica for her assistance with data acquisition and linkage.
Footnotes
Competing interests: None declared.
Contributors: S. Kreindler and C. Metge designed the study. S. Kreindler acquired the data, which all authors analyzed. S. Kreindler wrote the article which all authors reviewed and approved for publication.
References
- 1.Simunovic N, Devereaux PJ, Bhandari M. Surgery for hip fractures: Does surgical delay affect outcomes? Indian J Orthop. 2011;45:27–32. doi: 10.4103/0019-5413.73660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bottle A, Aylin P. Mortality associated with delay in operation after hip fracture: observational study. BMJ. 2006;332:947–51. doi: 10.1136/bmj.38790.468519.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brener S. Optimal timing of hip fracture surgery: a rapid review. Toronto, ON: Health Quality Council; 2013. [Google Scholar]
- 4.Bohm E, Loucks L, Wittmeier K, et al. Reduced time to surgery improves mortality and length of stay following hip fracture: results from an intervention study in a Canadian health authority. Can J Surg. 2015;58:257–63. doi: 10.1503/cjs.017714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dy CJ, Marx RG, Ghomrawi HM, et al. The potential influence of regionalization strategies on delivery of care for elective total joint arthroplasty. J Arthroplasty. 2015;30:1–6. doi: 10.1016/j.arth.2014.08.017. [DOI] [PubMed] [Google Scholar]
- 6.Chang V, Blackwell RH, Yau RM, et al. Variable surgical outcomes after hospital consolidation: implications for local health care delivery. Surgery. 2016;160:1155–61. doi: 10.1016/j.surg.2016.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Healy DA, McCartan DP, Grace PA, et al. The impact of regional reconfiguration on the management of appendicitis. Ir J Med Sci. 2014;183:351–5. doi: 10.1007/s11845-013-1015-x. [DOI] [PubMed] [Google Scholar]
- 8.Lansink KW, Leenen LP. Do designated trauma systems improve outcome? Curr Opin Crit Care. 2007;13:686–90. doi: 10.1097/MCC.0b013e3282f1e7a4. [DOI] [PubMed] [Google Scholar]
- 9.Celso B, Tepas J, Langland-Orban B, et al. A systematic review and meta-analysis comparing outcome of severely injured patients treated in trauma centers following the establishment of trauma systems. J Trauma. 2006;60:371–8. doi: 10.1097/01.ta.0000197916.99629.eb. [DOI] [PubMed] [Google Scholar]
- 10.Liang TJ, Liu SI, Mok KT, et al. Associations of volume and thyroidectomy outcomes: a nationwide study with systematic review and meta-analysis. Otolaryngol Head Neck Surg. 2016;155:65–75. doi: 10.1177/0194599816634627. [DOI] [PubMed] [Google Scholar]
- 11.Mowat A, Maher C, Ballard E. Surgical outcomes for low-volume vs high-volume surgeons in gynecology surgery: a systematic review and meta-analysis. Am J Obstet Gynecol. 2016;215:21–33. doi: 10.1016/j.ajog.2016.02.048. [DOI] [PubMed] [Google Scholar]
- 12.Phillips P, Poku E, Essat M, et al. Procedure volume and the association with short-term mortality following abdominal aortic aneurysm repair in European populations: a systematic review. Eur J Vasc Endovasc Surg. 2016;53:77–88. doi: 10.1016/j.ejvs.2016.10.007. [DOI] [PubMed] [Google Scholar]
- 13.Hata T, Motoi F, Ishida M, et al. Effect of hospital volume on surgical outcomes after pancreaticoduodenectomy: a systematic review and meta-analysis. Ann Surg. 2016;263:664–72. doi: 10.1097/SLA.0000000000001437. [DOI] [PubMed] [Google Scholar]
- 14.Kreindler SA, Zhang L, Metge CJ, et al. Impact of a regional acute care surgery model on patient access and outcomes. Can J Surg. 2013;56:318–24. doi: 10.1503/cjs.007012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hamilton SM, Johnston WC, Voaklander DC, et al. Outcomes after the regionalization of major surgical procedures in the Alberta Capital Health Region (Edmonton) Can J Surg. 2001;44:51–8. [PMC free article] [PubMed] [Google Scholar]
- 16.Martins S, Johnston G. Impact of orthopedic trauma consolidation on resident education. Can J Surg. 2009;52:495–9. [PMC free article] [PubMed] [Google Scholar]
- 17.Hark MK, Hart RF. Statistical process control for health care. Pacific Grove (CA): Wadsworth Group; 2002. [Google Scholar]
- 18.Durbin J, Watson GS. Testing for serial correlation in least squares regression, II. Biometrika. 1951;38:159–78. [PubMed] [Google Scholar]