Abstract
Here, we illustrate a 69-year old female admitting with weakness on left side of the face who firstly considered peripheral facial palsy in the forefront. However, detailed neurological examination and cranial MRI findings finally yielded the proper diagnosis of right hemisphere ischemic stroke. Via this remarkable presentation, we point out the clinical challenges in evaluation processes of patients with facial palsy in emergency practice and emphasize the importance of detailed examination for the proper diagnosis as well as initiation of appropriate treatment agents without delay.
Keywords: Facial paralysis, Stroke, Emergency department, Facial innervation, Pathophysiology
Abbreviations: HBS, House–Brackmann score; INR, International normalized ratio; MRC, Medical Research Council
1. Introduction
Peripheral facial nerve paralysis is an acute facial nerve affection which is encountered frequently in emergency medicine practice. Typically, the diagnosis can be made based on the weakness of all muscles innervated by the facial nerve branches. The discrimination between peripheral and central facial nerve palsies can be made according to whether the upper facial muscles are spared or not [1]. However, in contrast with common knowledge, upper facial weakness has also been reported to exist in patients with central facial palsy associated with unilateral stroke syndromes [2], [3]. From a distinct point of view, via the remarkable clinical follow-up of our patient, we point out challenges associated with clinical evaluation of patients presenting with facial palsy in emergency departments. We emphasize the importance of a detailed examination for the proper diagnosis as well as the initiation of appropriate treatment agents without delay.
2. Case report
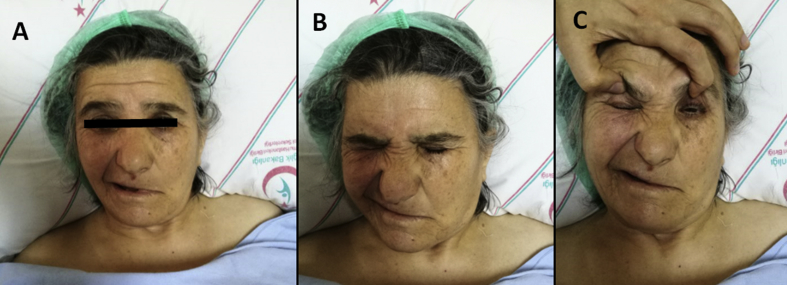
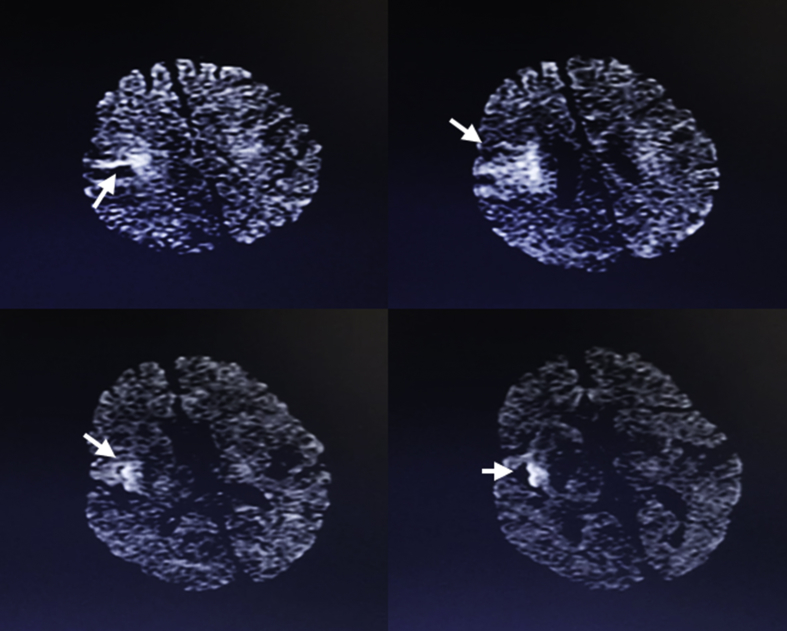
A-69-year old female patient with a medical history of diabetes mellitus and hypertension presented with a left facial weakness, which had started abruptly 4 hours prior to his admission to ED. A neurological examination revealed that both upper and lower parts of the face were involved in a grade 3 facial nerve palsy based on the HBS grading system (Fig. 1). Hence, a preliminary diagnosis of peripheral facial nerve palsy was made and an otorhinolaryngology consultation was requested. However, a reassessment of the patient revealed a left-sided hemiparesis (MRC grade 4) which had not been expressed by the patient's relatives. Taken together, a central nervous system disorder was considered at the forefront and a neurology consultation was requested. Based on a provisional diagnosis of stroke, a cranial MRI was performed which showed a right frontal lobe infarction corresponding to the territory of the superior division of the right middle cerebral artery (Fig. 2). Antiplatelet and anticoagulant therapies were started and the patient was admitted to the neurology ward. Further investigations, including computed tomography angiography of the brain and the neck, echocardiogram, electrocardiogram did not demonstrate any other abnormality. However, paroxysmal atrial fibrillation attacks were observed during HOLTER monitoring which led to the initiation of warfarin therapy. After the INR values within the target range were achieved, the patient was discharged with residual left sided peripheral-type facial paralysis and a moderate left hemiparesis.
Fig. 1.
Grade 3 upper and lower face paralysis according to HB grading system (A, B, C).
Fig. 2.
Diffusion weighted cranial MRI findings showing a right frontal lobe infarction corresponding to the superior division of the right middle cerebral artery (arrows).
3. Discussion
Here, we present an interesting patient diagnosed with central facial paralysis associated with unilateral cortical ischemic infarction whose diagnosis constituted a distractive experience in the emergency department. Findings of upper and lower facial weakness firstly suggested a diagnosis of peripheral facial palsy, however a detailed examination of the patient revealed a left sided hemiparesis, in addition to the facial weakness. Finally, cranial MRI findings enabled a proper diagnosis of right frontal lobe ischemic stroke in the MCA territory.
Facial paralysis is classically categorized as ‘upper motor neuron’ or ‘lower motor neuron’ types [4]. Upper motor neuron paralysis refers to ‘central’ paralysis, whereas lower motor neuron paralysis is known as ‘peripheral’ facial paralysis. Peripheral facial palsy can be defined as acute peripheral facial nerve affection, and can be classified as idiopathic or secondary to a number of conditions including infections, metabolic diseases, tumors, surgery, etc. Of note, rare cases of strokes associated with peripheral type facial paralysis have been reported in the literature [5], [6], [7]. However, in these reports, patients were diagnosed with brain stem infarcts and the responsible mechanisms were explained in the setting of lower motor neuron damage (facial nucleus). On the other hand, it is also a recognized fact that the weakness of upper facial muscles which is typically attributed to peripheral facial paralysis can be seen in association with central facial paralysis [2], [3]. In a study, it was reported to appear up to 6.6% of the patients with unilateral stroke and central facial paralysis [2]. Of note, right hemisphere involvement was suggested as a risk factor for upper facial weakness which was also the case in our patient [2]. Nonetheless, underlying pathophysiology and pathways of this atypical manifestation (peripheral-type facial paralysis) associated with upper motor neuron injury still remain to be clarified. Moreover, these discussions seem to be relatively underestimated in the literature. The basic knowledge states that upper facial muscles receive bilateral cortical innervation, but lower facial muscles are innervated by the contralateral cortex. However, currently, it is suggested that there may be some controversies regarding the mechanisms of facial innervation [8]. For example, studies conducted in adult rhesus monkeys using neuronal labelling techniques revealed that both upper and lower facial nucleus received bilateral cortical innervation which was in contrast to the classical knowledge, and remarkably, the upper facial nucleus received less cortical innervation than the lower facial nucleus [9], [10]. These conclusions have also been confirmed by post mortem anatomical studies in humans [11].
In the literature, this atypical manifestation of upper facial weakness has been stated in a limited number of reports and basically, clinical presentations, patient characteristics, prognosis and neuroimaging findings were the major points focused on in these studies [1], [3]. However, from a distinct point of view, our report may add substantial data pointing out clinical challenges in the differential diagnosis of facial paralysis associated with cortical stroke which mimics peripheral type, particularly in emergency departments. We emphasize the importance of a detailed evaluation to make a proper diagnosis and initiate appropriate treatments without delay. We believe that the presence of comorbidities (hypertension, diabetes mellitus, coronary disease etc.) or an abrupt clinical onset should lead the clinicians to be more careful while a complete neurological examination should be performed in all patients presenting with facial palsy, even in typical peripheral subtypes. In addition, we think that documentation of these atypical presentations in future reports of larger case series may further clarify the unknown mechanisms underlying innervation pathways of facial nerve, while these study results may add crucial data to the evaluation processes as well as treatment approaches in these atypical cases.
Conflict of interest
None.
Acknowledgements
None.
Footnotes
Peer review under responsibility of The Emergency Medicine Association of Turkey.
References
- 1.Finsterer J. Management of peripheral facial nerve palsy. Eur Arch Otorhinolaryngol. 2008;265(7):743–752. doi: 10.1007/s00405-008-0646-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lin J. Weakness of eye closure with central facial paralysis after unilateral hemispheric stroke predicts a worse outcome. J Stroke Cerebrovasc Dis. 2016 doi: 10.1016/j.jstrokecerebrovasdis.2016.10.029. [DOI] [PubMed] [Google Scholar]
- 3.Hagg M., Tibbling L. Four-quadrant facial function in dysphagic patients after stroke and in healthy controls. Neurol Res Int. 2014;2014:672685. doi: 10.1155/2014/672685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.G. H, editor. Anatomy of the human body. twentieth ed. Lea and Febiger; Philadelphia: 1918. [Google Scholar]
- 5.Ahn S.K. A rare case of pontomedullary infarction presenting with peripheral-type facial palsy. Auris Nasus Larynx. 2010;37(6):747–749. doi: 10.1016/j.anl.2010.03.010. [DOI] [PubMed] [Google Scholar]
- 6.Thomke F. Seventh nerve palsies may be the only clinical sign of small pontine infarctions in diabetic and hypertensive patients. J Neurol. 2002;249(11):1556–1562. doi: 10.1007/s00415-002-0894-y. [DOI] [PubMed] [Google Scholar]
- 7.Park J.H., Yoo H.U., Shin H.W. Peripheral type facial palsy in a patient with dorsolateral medullary infarction with infranuclear involvement of the caudal pons. J Stroke Cerebrovasc Dis. 2008;17(5):263–265. doi: 10.1016/j.jstrokecerebrovasdis.2008.02.007. [DOI] [PubMed] [Google Scholar]
- 8.Mahadevappa K. Facial paralysis: a critical review of accepted explanation. Med Hypotheses. 2010;74(3):508–509. doi: 10.1016/j.mehy.2009.10.010. [DOI] [PubMed] [Google Scholar]
- 9.Morecraft R.J. Cortical innervation of the facial nucleus in the non-human primate: a new interpretation of the effects of stroke and related subtotal brain trauma on the muscles of facial expression. Brain. 2001;124(Pt 1):176–208. doi: 10.1093/brain/124.1.176. [DOI] [PubMed] [Google Scholar]
- 10.Jenny A.B., Saper C.B. Organization of the facial nucleus and corticofacial projection in the monkey: a reconsideration of the upper motor neuron facial palsy. Neurology. 1987;37(6):930–939. doi: 10.1212/wnl.37.6.930. [DOI] [PubMed] [Google Scholar]
- 11.Kuypers H.G. Corticobular connexions to the pons and lower brain-stem in man: an anatomical study. Brain. 1958;81(3):364–388. doi: 10.1093/brain/81.3.364. [DOI] [PubMed] [Google Scholar]