Abstract
Purpose
To explore the mobility-related preferences among stroke survivors and caregivers following post-acute rehabilitation at inpatient or skilled nursing facilities.
Methods
In this cross-sectional study; semi-structured, qualitative interviews of stroke survivors (n=24) and informal caregivers (n=15) were conducted. The participants were recruited from the community.
Results
Comparative content analysis was used to identify themes by two independent coders. The survivors (68 years) and caregivers (58 years) mentioned mobility related consequences including inability to walk, balance, drive, and transfer; and increased falls. The survivors (63%) and caregivers (73%) also mentioned the use of assistive devices. The common rehabilitation activities included: walking (62%); followed by standing and mobility; strength and balance; and wheelchair skills. Some stroke survivors were dissatisfied as their rehabilitation was not patient-centered. Frequently mentioned outcome preferences by survivors were ability to walk (88%), move, and balance. They also wanted to acquire assistive devices to move independently. Caregivers were concerned with the survivor’s safety and wanted them to drive (53%), prevent falls, have home accommodations, and transfer independently. Caregivers (40%) also expressed the importance of receiving realistic information.
Conclusions
This study suggests a need to consider the stroke survivors’ and caregivers’ mobility outcome preferences to improve the patient-centered rehabilitation care.
Keywords: mobility, caregivers, rehabilitation, qualitative research, patient-centered, stroke
Introduction
Annually, around 7 million Americans are affected by post-stroke disability. The majority of stroke survivors live in the community with prolonged long-term disability [1]. Hospitalizations, including nursing home admissions, are associated with a rapid decline in mobility and function [2]. Mobility typically includes the ability to walk, stand, and transfer from one place to another [3]. Mobility also encompasses the ability to participate in the community [4]. Mobility limitations among adults with stroke hinder their ability to effectively perform their activities of daily living [5]. Most individuals with stroke have decreased levels of community ambulation, which significantly reduces their quality of life [6,7].
The American Heart Association’s 2016 Heart Disease and Stroke Statistics Update reported that much of the long-term disability after stroke may be preventable [8]. Participation in rehabilitation is known to reduce disability and improve management of post-stroke limitations [9]. Although person-centered care is emphasized in many health care environments, this is often difficult to accomplish during busy clinical practice. Quantitative outcome measures used in studies to assess mobility and regain function may not always capture the patient-centered outcome preferences [10]. One way to better explore these needs is through semi-structured, open-ended qualitative interviews that help researchers, clinicians, and policy makers address the outcomes most important to the patient [11,12].
Studies have indicated the significance of post-acute discharge destination in developing an optimal patient-centered rehabilitation program. For instance, for individuals with stroke; rehabilitation in skilled nursing facilities is known to increase the rates of institutionalizations than those who received rehabilitation in inpatient facilities or were discharged home [13]. In addition, patients with acute-onset of disabilities undergoing inpatient rehabilitation have different preferences to prioritize the functional recovery compared to their clinicians caring for them [14]. The patients were more concerned to be independent in their physical functional recovery, including eating, grooming, and toileting activities; whereas their rehabilitation clinicians were focused on improving patient’s comprehension and expression. Engaging the patients and caregivers will represent an “insider’s perspective” of their desired preferences based on their unique characteristics, which will help inform decisions and enhance patient-centered care [15]. Previous studies have not explored the mobility outcome preferences of stroke survivors who received post-acute rehabilitation, and their caregivers. Since most of the stroke care research do not necessarily include the patient’s or caregiver’s opinions or desired needs, it is essential to identify the outcomes that matter and are prioritized by them.
The objective of the current study was to understand the mobility-related post-stroke consequences, rehabilitation activities, and outcome preferences of stroke survivors who received post-acute rehabilitation in inpatient rehabilitation or skilled nursing facilities, and their informal caregivers.
Methods
Study design
This is a cross-sectional study that utilized convenience sampling technique [16] for enrolling stroke survivors and their informal caregivers. This study is part of a larger Patient-Centered Outcomes Research in the Elderly (PCOR-E) study that explored the post-stroke experiences of stroke survivors and their caregivers. Approval for this study was obtained from the University’s Institutional Review Board. All participants provided written informed consent.
Participants and recruitment
For the PCOR-E study, participants were recruited from stroke support groups, skilled nursing facilities, and retirement living centers from the Houston and Galveston area. The stroke survivors were included if they self-identified to be 18 years or older, with diagnosis of stroke. Caregivers were included if they cared for the survivors and assisted them with their activities of daily living. Participants were excluded if they did not speak English. The stroke survivors identified most of their informal caregivers; others were recruited through stroke support groups. Not all caregivers identified by individuals with stroke were willing to participate. Similarly, some stroke survivors did not want to participate in this study but their caregivers participated. Before commencing the interviews, the interviewers stated their clinical and academic backgrounds, affiliations, and the purpose of the study to the participants. For the current study to determine the person-centered mobility outcome preferences, participants were included only if they received rehabilitation from inpatient or skilled nursing facilities or cared for the survivor who received rehabilitation in either of these facilities (n=39).
Data collection
To understand the participants’ outcome preferences following stroke, semi-structured, open-ended, face-to-face interviews were conducted from November 2013 to July 2015. The interviews were conducted separately for stroke survivors and their informal caregivers, at the participant’s preferred location (home or a meeting room in the facility). Two senior researchers in the team with expertise in stroke rehabilitation, interviewing and data collection were involved in developing semi-structured guide. The semi-structured, open-ended interviews allowed us to discover spontaneous responses, obtain a diversified set of responses spread beyond the original question, and avoided participant response bias [17]. This format allowed us to move around these domains and probe further based on the participants’ responses [18].The participants were asked to describe the stroke event, their hospitalization and rehabilitation experiences. In case of multiple strokes, the participants were asked to elaborate on the event that was followed with rehabilitation in either of the facilities. The list of semi-structured questions included, therapy and services received, goals in rehabilitation, what was most important, what would have been helpful, what do you wish was done looking back. The participants were asked to comment on the activities performed during rehabilitation, and advice they would want to share with others in a similar situation.
As the interviewers analyzed the transcripts iteratively, the interview guide was refined, and participants were probed on various aspects as the themes emerged [19–21]. The guide was refined during the initial stages to make sure all individuals probed on themes/concepts as they emerged in the previous interviews. This process allows researchers to further explore new topics based on emerging themes [21,22]. Probing helped us clarify and explore the participant’s response in greater detail [21]. The participants were probed with a series of follow-up questions, depending upon their responses to the semi-structured questions. For example, participants who mentioned mobility related limitations, were further probed on specific aspects of mobility such as balance, transfers etc. to further understand their preferences related to mobility. To obtain in-depth answers to on mobility related limitations the participants were probed and asked “can you give an example of that” or “could you tell me more about activities related to mobility during rehabilitation”. In addition, if the individual mentioned difficulty performing a mobility related activity the interviewers probed these individuals on “use of any assistive device” and “mobility related goals moving forward”. The interviewers discussed these probes as a team.
To probe individuals with aphasia and understand their preferences they were given cue cards with pictures along with other supportive conversation to ensure their comprehension provide them a means to respond [23]. Some questions were rephrased so that they could point out to yes/no cue cards so that they could point out and prioritize their preferred ones using the card sorting method [24]. Field notes were documented for these individuals with aphasia, to record their responses since most of the times the audio could not capture their responses. The verbatim from the field notes were analyzed in a similar manner as the other interviews.
The interviews were conducted independently by three rehabilitation therapists; licensed physical (SK) and occupational (TR, CH) therapists. These interviews were audio recorded and transcribed using a professional service. The interviewers on an average had over 15 years of experience in neurological rehabilitation. None of the interviewers had clinical or working relationships with the participants. In addition, all researchers in the team had extensive experience performing qualitative research (2–22 years). The interviews lasted for 31 minutes on an average.
Data analysis
Stroke survivors and their caregivers discussing any mobility needs such as moving in a space for their activities of daily living, or limitations that restricted the individual’s mobility were coded. The qualitative comparative method of content analysis was used to identify the themes and subthemes using inductive, line-by-line coding to systematically analyze the text [11]. Interviews of the stroke survivor and caregiver were coded independently by two primary coders (SK and TR) for various themes related to mobility.
The first stage involved reading of the transcripts and independently coding themes and subthemes related to mobility. The primary coders met weekly to discuss the consensus of the codes. Thematic saturation occurred by the end of the 12th stroke survivor and caregiver interview, following which no new concepts was generated.
The second stage involved entering the themes and subthemes into NVivo 10.a NViVo is a qualitative software used for data management and coding. This software also allowed us to update and maintain precise record of the coding decisions for specific themes and subthemes in a systematic manner [25]. As the themes were developed and entered a codebook was created.
The third stage involved evaluating the final list of themes for trustworthiness, including credibility, transferability, dependability, and confirmability [26,27]. All quotations under each theme and subtheme were appraised, and their quality was examined by the primary coders (SK and TR) and MP. In addition, parts of the coded interviews were quality checked by SW. The use of multiple coders with various backgrounds (physical therapist, occupational therapist, social work/health specialist, and social science expert) having qualitative and quantitative expertise ensured reliability and credibility in coding, reducing personal biases [11]. The researchers met weekly to review the final list of themes and subthemes. The disagreements in coding were resolved via discussion, and the finalized themes and subthemes were modified in NVivo.
The final stage involved grouping these themes and subthemes into meta-themes. To create the meta-themes, similarities and differences between themes were compared among the interviews [11]. The themes and subthemes were grouped into categories in NVivo. All the team members (male and female) reconciled various subthemes to form three major themes. Subgroup analyses by age, type of facility, or gender were not conducted as the data collection for this study was not stratified by these factors.
Results
All stroke survivors were community dwelling. The stroke survivors were roughly between 1 to 30 years post their stroke event. Table 1 lists the key characteristics of all participants. Out of the 39 participants included in the current study to explore patient-centered mobility outcome preferences: 24 stroke survivors received rehabilitation from inpatient rehabilitation or skilled nursing facilities, and 15 informal caregivers cared for the stroke survivors who received rehabilitation from either facility. Most of the participants received inpatient rehabilitation (71%) or cared for a survivor receiving inpatient rehabilitation (67%). Two of the stroke survivors had aphasia. The average age of the stroke survivors was 68 years, and that of caregivers was 58 years. Most of the survivors were men (67%), and most of the caregivers were women (80%). The caregivers were mostly spouses (73%) of stroke survivors. Most of the participants were Non-Hispanic Whites (69%), table 2.
Table 1.
Demographics of participants enrolled in this study (n=39)
| ID | Age (y) | Sex | Race/Ethnicity | Facility type | Relationship |
|---|---|---|---|---|---|
| ss02 | Unknown | M | White, Non-Hispanic | IRF | NA |
| ss03 | 61 | F | White, Non-Hispanic | SNF | NA |
| ss08 | 85 | F | White, Non-Hispanic | SNF | NA |
| ss11 | 72 | M | White, Non-Hispanic | IRF | NA |
| ss12 | 73 | F | Hispanic | SNF | NA |
| ss14 | 82 | M | White, Non-Hispanic | SNF | NA |
| ss15 | 82 | F | African American | SNF | NA |
| ss16 | 86 | M | African American | SNF | NA |
| ss17 | 71 | F | African American | IRF | NA |
| ss20 | 55 | M | White, Non-Hispanic | IRF | NA |
| ss21 | 56 | M | White, Non-Hispanic | IRF | NA |
| ss22 | Unknown | M | African American | IRF | NA |
| ss23 | 74 | F | White, Non-Hispanic | IRF | NA |
| ss24 | 68 | M | White, Non-Hispanic | IRF | NA |
| ss26 | 70 | M | White, Non-Hispanic | IRF | NA |
| ss29 | 91 | M | White, Non-Hispanic | SNF | NA |
| ss30 | 62 | M | White, Non-Hispanic | IRF | NA |
| ss31 | 72 | F | White, Non-Hispanic | IRF | NA |
| ss35 | 50 | M | Hispanic | IRF | NA |
| ss36 | 44 | M | African-American | IRF | NA |
| ss39 | 61 | M | Asian-American | IRF | NA |
| ss40 | 50 | M | White, Non-Hispanic | IRF | NA |
| ss41 | 69 | M | Hispanic | IRF | NA |
| ss42 | 67 | F | White, Non-Hispanic | IRF | NA |
| c01 | 65 | F | White, Non-Hispanic | IRF | Wife |
| c03 | 23 | M | African American | SNF | Nephew |
| c06 | 53 | F | White, Non-Hispanic | SNF | Daughter |
| c07 | 75 | M | White, Non-Hispanic | IRF | Husband |
| c08 | 47 | F | Hispanic | SNF | Daughter |
| c12 | 67 | F | White, Non-Hispanic | SNF | Wife |
| c13 | 54 | F | White, Non-Hispanic | IRF | Wife |
| c14 | 24 | F | White, Non-Hispanic | IRF | Daughter |
| c15 | 48 | F | Asian-American | IRF | Wife |
| c16 | 69 | F | White, Non-Hispanic | IRF | Wife |
| c19 | 59 | F | White, Non-Hispanic | SNF | Wife |
| c21 | 89 | F | White, Non-Hispanic | IRF | Wife |
| c23 | 75 | M | White, Non-Hispanic | IRF | Husband |
| c24 | 68 | F | African American | IRF | Wife |
| c25 | 59 | F | White, Non-Hispanic | IRF | Wife |
ss = stroke survivor, c = caregiver, IRF = inpatient rehabilitation facility, SNF = skilled nursing facility, M = male, F = female, NA = not applicaple, y = years
Table 2.
Demographics of participants enrolled in this study (n=39).
| Demographics | Stroke Survivors (n=24) | Caregivers (n=15) |
|---|---|---|
| Age (years) | ||
| Mean±SEM | 68.2±2.7 | 58.3±4.7 |
| Range | 44 – 91 | 23 – 89 |
| Sex | ||
| Male | 16 (66.7%) | 3 (20%) |
| Female | 8 (33.3%) | 12 (80%) |
| Race/Ethinicity | ||
| White, Non Hispanic | 15 (62.5%) | 11 (73.3%) |
| African American | 5 (20.8%) | 2 (13.3%) |
| Hispanic | 3 (7.7%) | 1 (6.7%) |
| Asian | 1 (4.2%) | 1 (6.7%) |
| Facility type | ||
| IRF | 17 (70.8%) | 10 (66.7%) |
| SNF | 7(29.2%) | 5 (33.3%) |
| Relationship with SS | NA | |
| Wife | 9 (60%) | |
| Husband | 2 (13.2%) | |
| Daughter | 3 (20%) | |
| Nephew | 1 (6.7%) | |
SS= stroke survivor, IRF = inpatient rehabilitation facility, SNF = skilled sursing facility, NA = not applicable
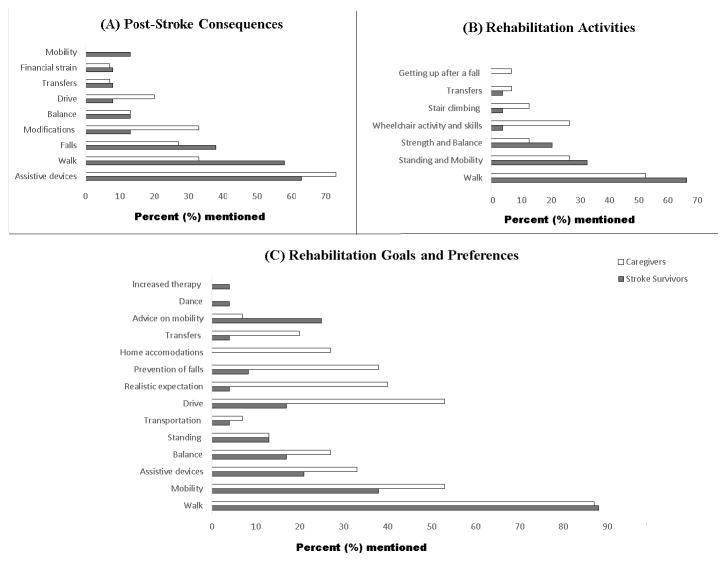
The mobility related themes that emerged from this study were: (a) Post-stroke consequences; (b) Rehabilitation activities and gains; and (c) Outcome preferences and advice to other stroke survivors. Figure 1 indicates the percentages of the participants’ preferences for each meta-theme.
Figure 1.
Themes related to mobility outcomes from stroke survivor and caregiver interviews (A) Post-stroke consequences, (B) Rehabilitation activities, and (C) Rehabilitation goals and preferences.
a) Post-stroke consequences
Thirty-two participants: 88% stroke survivors, and 73% caregivers mentioned at least one consequence related to mobility post-stroke. Table 3 consists of the prototypical quotations from the participants. The inability to walk was the most common limitation mentioned by 58% survivors and 33% caregivers, followed by an increased incidence of falls. Stroke survivors most often fell while getting in and out of a vehicle, or in the bathroom. To maximize the survivors’ independence and decrease the burden on caregiving, 63% of the survivors and 73% of the caregivers reported survivors’ utilization of some form of assistive device, such as wheelchair, walker, cane and orthoses; 33% of caregivers reported accommodated their home with some form of modification, including tilt bed, shower bench, toilet seat, or vehicle modifications. It is important to note that inability to walk was mentioned mostly by survivors than caregivers (58% vs. 33%), whereas having home or vehicle modifications were mentioned mostly by caregivers than survivors (33% vs. 13 %). Other post-stroke consequences related to mobility included the inability to drive, transfer, or balance, and increasing financial burden – figure 1(A).
Table 3.
Quotations related to post-stroke mobility consequences from stroke survivor and caregiver interviews (n=39).
| Consequences | Stroke survivors (n=24) | Caregivers (n=15) | Protypical quotations |
|---|---|---|---|
| Assistive devices | 15 (63%) | 11 (73%) | “I…got me fitted for the leg brace.” (ss36);“ She has this fantastic Quantum high end chair” (c6) |
| Walk | 14 (58%) | 5 (33%) |
“When I woke up I went to get out bed, I couldn’t walk or nothing.” (ss15); “Then suddenly, he can’t walk.”(c13) |
| Falls | 9 (38%) | 4 (27%) |
“I had started falling.” (ss39); “Many times he fell in the bathroom.” (c24) |
| Modifications | 3 (13%) | 5 (33%) |
“I had to make some modifications because I was in a wheelchair for a while and the house is not exactly wheelchair accessible.” (ss36); “We have a tilt bed. One of those beds you can raise. She used to be able to get in and out of that by herself and sit up with the back of the bed, pull into her fancy chair.” (c06) |
| Balance | 3 (13%) | 2 (13%) |
“My balance is not good.” (ss23); “Very bad balance.” (c16) |
| Drive | 2 (8%) | 3 (20%) |
“ They told me I couldn’t drive.” (ss42); “Initially he couldn’t drive, so I had to drive him everywhere.” (c15) |
| Transfers | 2 (8%) | 1 (7%) |
“Initially, the transfers were very, very difficult.” (ss22); “I had to physically get him out and physically get him in the bathtub.” (c16) |
| Financial strain | 2 (8%) | 1 (7%) |
“I don’t have it anymore because insurance ran out.”(ss35); “He needs Botox treatments, to be able to walk better, and I can’t afford to do it.” (c12) |
| Mobility | 3 (13%) | 0 | “When I was discharged from the inpatient I did not have any movement in my left leg. I took me three to four months to... As the movement returned, it just returned to the knee and hip first and still hasn’t returned to the ankle or toes.”(ss16) |
ss = stroke survivor, c = caregiver
b) Rehabilitation activities and gains
Rehabilitation activities performed by the stroke survivors to regain their mobility during their stay at inpatient or skilled nursing facilities and prototypical quotations are listed in table 4. The most common activities mentioned by participants were walking (62%), standing and mobility (31%), strength and balance (18%), and stair climbing (8%). However, the largest difference between the survivors and the caregivers’ response appeared to be on practicing wheelchair skills as a method for mobility (4% vs. 27%). Only participants who went through inpatient rehabilitation mentioned training for transfers and getting up after a fall -- figure 1(B). Eighteen participants (46%): 10 stroke survivors (42%), and 8 caregivers (53%) mentioned that the survivor was able to re-gain the mobility related outcomes following rehabilitation. Walking was the most common outcome that the survivors re-gained following rehabilitation, followed by the ability to drive, transfer, stand, and climb stairs. Three stroke survivors were frustrated and dissatisfied by the entire process of rehabilitation as they were not able to walk or accomplish their mobility-related outcomes. They also highlighted that their rehabilitation process was not patient-centered, stating that their therapists did not have the same mindset-set as them.
Table 4.
Quotations related to rehabilitation activities from stroke survivor and caregiver interviews (n=39).
| Activities | Inpatient rehabilitation (ss = 17, c = 10) | Skilled nursing (ss = 7, c = 5) |
|---|---|---|
|
Walk ss = 16 (67%) c = 8 (53%) |
“got me up to walk with a walker.” (ss11); “..they wanted her to do a lot of walking.” (c7) |
“Well we worked on the walking.” (ss3); “I know a lot of it was getting her to walk.” (c6) |
|
Standing and mobility ss = 8 (33%) c = 4 (27%) |
“They performed activities that deal with the leg.” (ss22); “..moving the leg, that kind of thing.”(c13) |
“I know they had me in bed move my legs up and down.” (ss8); Those goals were just getting him up to a certain level of movement.” (c12) |
|
Strength and Balance ss = 5 (21%) c = 2 (13%) |
“Because I had a lot of problems with my balance, we focused a lot on gaining on helping me find my center again.” (ss36); “..mostly just building strength” (c13). |
“They were trying to get my right leg stronger.” (ss8); “He did balance, strengthening.” (c12) |
|
Wheelchair and skills ss = 1 (4%) c = 4 (27%) |
Were any wheelchair skills taught to you when you were in rehab? “I was just told to do it and I did it.”(ss21); “They had created a wheelchair just for him for his weight.” (c21) |
“Taught her how to use her wheelchair, driving it and everything, worked with her arm.” (c06) |
|
Stair climbing ss = 1 (4%) c = 2 (13%) |
“..or climbed.” (ss22); “They did the standard climbing up.” (c13) |
“He did stair climbing.” (c12) |
|
Transfers ss = 1 (4%) c = 1 (7%) |
“When I was an in-patient we practiced transfers, for example, to the toilet.”(ss20); “Taught him how to transfer himself from the wheelchair to the car.” (c16) |
None mentioned |
|
Getting up after a fall ss = 0 c = 1 (7%) |
“They did some stuff where if you happen to fall off the bed, here’s how you can get back up, or fall out of a chair, those kind of things.” (c13) | None mentioned |
ss = stroke survivor; c = caregiver
c) Outcome preferences and advice to other stroke survivors
The mobility outcomes most important to stroke survivors and the caregivers with relevant quotations are listed in table 5. The ability to walk independently was the most preferred outcome among all participants (77%), followed by the ability to move (44%), drive (31%), balance (21%), and stand (13%). Most of them also highlighted the need to acquire an assistive device to move independently wanted transportation in the community (26%). Among assistive devices, participants wanted wheelchairs along with the skills to maneuver the wheelchair (10%), followed by walkers (5%), gait belt, orthoses, scooters, and cane (3% each). However, compared to the stroke survivors, the caregivers more often emphasized the need for the survivors to drive (17% vs. 53%). The caregivers were also concerned for the survivor’s safety, and felt the need to prevent falls (8% vs. 33%), have appropriate home accommodations (0% vs. 27%), and help the survivor to transfer independently (4% vs. 20%). Many caregivers (40%) wanted realistic information on post-stroke mobility prognosis. The stroke survivors also provided various suggestions to those in a similar situation as them: they highlighted the importance of rehabilitation to improve the mobility related outcomes (25%), and encouraged other stroke survivors to utilize wheelchairs to maintain independence. A few stroke survivors also wished for more therapy, and wanted to dance – figure 1(C).
Table 5.
Outcome preferences related to mobility of patients and caregivers and relevant quotations.
| Goals | Inpatient Rehabilitation Facility | Skilled Nursing Facility |
|---|---|---|
|
Walk ss = 21 (88%) c = 13 (87%) |
“I wanted to learn how to walk.” (ss17); “I want him to walk.” (c01) |
“I wish I could walk better.” (ss03); “Getting her up walking.” (c06) |
|
Movement/mobility ss = 9 (38%) c = 8 (53%) |
“My main goal when I went there to rehab was to get up.” (ss23); “I want to get him out of his wheelchair.” (c13) |
“move around more freely.” (ss30); “My goals were just to keep him motivated and mobile.” (c12) |
|
Assistive devices ss = 5 (21%) c = 5 (33%) |
“I haven’t gotten a scooter, which I could really use.” (ss26); “he needs a wheelchair.” (c13) |
“I recommend power chairs as a primary vehicle for outreach.” (ss29); “she gets her[a] good chair or we get her a new one, she’s a lot more self-sufficient.” (c06) |
|
Balance ss = 4 (17%) c = 4 (27%) |
“To have good balance while walking.” (ss31); “To get more balance.” (c16) |
“You really need to balance one side with the other side.”(ss29);“The balancing.” (c08). |
|
Standing ss = 3 (13%) c = 2 (13%) |
“Was to stand properly.” (ss21); “I wanted him to stand up.” (c15) |
“If everybody stands up, she’d like to be also doing that.” (c06) |
|
Transportation ss = 1 (4%) c = 1 (7%) |
“Sometimes I think of something to do at the last minute and I can’t call Metro. If I call somebody, they’ll say, ‘Yeah, I’ll be down to take you,’ and they don’t show up. That stuff hurts.” (ss39) | “He can’t go anywhere by himself, at all. He has to have a ride.” (c12) |
|
Drive ss = 4 (17%) c = 8 (53%) |
“I wanna drive.” (ss02); “it was driving first.” (c16) | “back to driving.” (c03) |
|
Information on mobility/ Realistic expectation ss = 1 (4%) c = 6 (40%) |
“I kind of wished I had known how long it would take. When I used to ask questions to doctors about how long is it likely to take before I get some of my sensation back and muscle movements, they always were not able to answer the questions.” (ss20); “My level of expectation was, and this is probably unrealistic as I look back at it, that she’s going to be able to walk out of the hospital the way she was before.” (c07) |
None mentioned |
|
Prevention of falls ss = 2 (8.3%) c = 5 (33%) |
“I don’t want maybe I fall.” (ss41); “That’s one of the things that I worry about all the time, falling.” (c07) |
“she falls in the bathroom..that was our biggest worry.” (c06) |
|
Home accomodations ss = 0 c = 4 (27%) |
“Some houses are upstairs which is very risky for somebody like them to be going upstairs all the time. And then some houses don’t have ramps.” (c24) | “..in the shower, in the bathrooms.” (c12) |
|
Transfers ss = 1 (4%) c = 3 (20%) |
“Transferring for yourself, is that a goal? Yes.” (ss31); “transferring ... as a caregiver, that was the big thing.” (c23) |
“It’s really a more ... just being to get ... transfer from one place to another.” (c06) |
|
Advice on mobility ss = 6 (25%) c = 1 (7%) |
“One advice I would like to give is that it does not take a short time to recover from stroke…There are certain things which are there…For example, my stroke was in April 2014, up to now I still cannot walk properly. It means it take more than a year.”(ss22) |
“You know if it was walking or their hand you know or their talking you know, tell them to work on that you know and then work on the others.” (ss03); “Depending on their situation as far as if they’re mobile.” (c19) |
|
Increased therapy ss = 1 (4%) c = 0 |
“I wanted more walking therapy than anybody else in the world.” (ss24) | None mentioned |
|
Dance ss = 1 (4%) c = 0 |
“I want to dance with my wife.” (ss35) | None mentioned |
ss = stroke survivor; c = caregiver
Discussion
To our knowledge, this is the first study conducted in the United States to specifically explore stroke survivors’ and their informal caregivers’ mobility-related outcome preferences following rehabilitation in either inpatient or skilled nursing facilities. In this sample, 87% of the participants indicated at least one mobility related limitation post-stroke. Although mobility was their greatest concern, emphasis on aspects of mobility was different between the groups. While discussing the post-stroke consequences, most of the survivors mentioned the inability to walk, whereas the caregivers mentioned having various accommodations. These two subthemes seem to emphasize the perceptions of these two groups. Most of the participants (97%) mentioned their mobility-related outcome preferences. Walking, and acquiring assistive devices to independently move were the preferred by all the participants. The caregivers were mostly concerned with the stroke survivors’ safety and wanted to prevent falls, have suitable home and vehicle accommodations, transfer and drive independently. They also highlighted the need for provision of realistic information by the clinicians.
In spite of evidence supporting a multidisciplinary patient-centered approach, physicians may influence the practices in rehabilitation facilities, and the outcomes they pursue may not be patient-centered [14]. Increase in the utilization of hospitalists contributes to insufficient communication between patients and their clinicians following acute care discharge [28]. To design an appropriate patient-centered transition in care by involving patients and their caregivers enhances their communication with their clinicians [28].
Similar to this study, previous studies have indicated that most of the individuals with stroke and their caregivers evaluate their recovery and prognosis in the context of mobility and function [29,30]. Stroke survivors who actively walked before the event usually express an increasing need to be able to walk [31]. Mobility in the community, including transportation and driving was another prioritized outcome expressed by the participants. Studies have indicated that individuals with stroke have difficulty using public transportation increasing their dependency [32]; similar to the outcomes reported in this study. Very rarely do rehabilitation professionals teach the skills needed to use public transportation, which may be due to shorter length of stay resulting in individuals being discharged home prior to obtaining the functional abilities needed for community ambulation and the use of public transportation. As a result, they are left to learn these skills by themselves.
Caregivers in the study reported the need for appropriate home accommodations, and prevent falls. The use of home accommodations and assistive devices to prevent falls among stroke survivors is known to decrease the caregiver burden [33]. Only those who went through inpatient rehabilitation mentioned practicing transfer related activities, and getting up correctly after a fall; this does not necessarily mean that those who went through skilled nursing rehabilitation were not taught these activities.
Individuals with stroke and their families prefer to be actively involved in the rehabilitative process, rather than allowing the clinicians making judgments on their behalf based solely on functional status assessments [34]. It is also important to note that the outcome preferences of stroke survivors and their families may evolve as their clinical and financial situations change [14]. Hence, the health care professionals must consider involving them during all stages of care. The unique contributions from this study provide information to guide clinicians and researchers in developing patient-centered measures post-stroke. The use of a qualitative approach increased our understanding of the mobility outcome preferences of stroke survivors and their caregivers [18,35].
The discussions with patients and their caregivers surrounding the “goal-setting” process require considerable time and effort and can be demanding [36]. If the clinician is not able to involve individuals with aphasia or dysphasia in the “goal-setting process”[37], it is important to resort to other means such as involving their families, or using card sorting [23,24]. The disconnect between the expectations of clinicians and stroke survivors and their caregivers can be attributed to the patient complexities including, patient’s personal characteristics, availability of support, social determinants, and health system factors geared towards discharging patients sooner from the hospital [38]. One way to address this disconnect could be by incorporating an interdisciplinary approach including all stakeholders (stroke survivors, families, stroke management team, physicians, social worker, discharge care team, and rehabilitation therapists) to incorporate the patient-centered needs. The clinicians may also tend to believe that patients usually focus on eventual outcomes and not the specific limitations that needs to be worked on to regain these outcomes making them hesitant to involve the patient; in such cases, it may be important to educate and train the stroke survivors and caregivers on the specific limitations that needs to be worked on that aligns with their preferred outcomes [39]. Future research must be implemented to understand the factors that can decrease the potential disconnect between the expectations of stroke survivors and the clinicians.
Increased therapy time and provision of services for the patients could be challenging because of limited time and insurance. In some cases the physicians may be able to write a letter to the insurance company to override the cap for patients who show continued improvement. It is also important to educate the stroke survivors to continue the rehabilitation interventions at home during the temporary cut in therapy. Increasing community-based rehabilitation services can help manage long-term stroke patients [40]. It is also important to train and educate the caregivers during rehabilitation, so that they can provide therapy once the patient is discharged from rehabilitation. The recent advances in the use of technology including, telerehabilitation, brain gaming, activity monitors, could serve as a possible solution to improve recovery in these individuals [41].
The National Institutes of Health Roadmap Initiative, the Patient Reported Outcomes Measurement Information System (PROMIS) is directed towards establishing a resource for clinicians to measure patient-reported outcome measures, and is being validated in stroke population [42]. Once additional PROMIS projects establish the validity of this scale, we can compare the mobility outcomes from this study with the mobility domains of the PROMIS – physical function scale.
Limitations
It is important to note that participants were probed on various mobility related outcomes, only when they indicated any mobility related consequences or preferences. Also, the sample size for those who went through skilled nursing rehabilitation was relatively small. As the stroke survivors and the caregivers were recruited from the community with varying lengths of time from stroke, the results of this study should be interpreted cautiously. It is also possible that the participants might not have mentioned all the activities that were taught or practiced during their rehabilitation stay, because of the open-ended interviews. The open-ended interviews may have been cognitively challenging for the participants [17], however, it is a preferred method for obtaining richer data and gain greater insight on various topics from a smaller sample. In addition, since most of the participants were recruited from the community we did not have information on their stroke severity.
As the individuals with aphasia were probed using cue cards, we may not have been able to completely explore their needs and preferences. In future, we plan to investigate the most appropriate method to conduct qualitative interviews to probe individuals with aphasia. Future studies with baseline levels of function among stroke survivors will further help us interpret the importance of these person-centered preferences. In spite of these limitations, the results of this study can be transferred to similar population and settings which can help develop effective intervention tailored to the individual’s preferences.
Conclusions
Stroke survivors and their informal caregivers tend to differ in their outcome preferences. It is important to understand the person-centered needs of stroke survivors and their caregivers to prescribe appropriate interventions. The most preferred outcome preferences for the participants were to walk, move, and balance. They also wanted to acquire appropriate assistive devices to move independently. The caregivers expressed greater concern for transfers, driving, fall prevention, home modifications, and wished for realistic information related to mobility from the clinicians.
Acknowledgments
Funding Sources: Supported with funding from the National Institute of Health, NICHD (K01-H0055929); Agency for Health Care Research and Quality (R24 HS022134 and R01-HS024711); National Institute on Disability and Rehabilitation Research (90AR5009); UTMB Institute for Translational Sciences support by an NIH Clinical & Translational Science Award (UL1RR029876); UTMB Claude D. Pepper Older Americans Independence Center NIH/NIA (P30 AG024832).
Footnotes
Suppliers: NVivo 10 for Windows, QSR International.
Conflicts of Interest:
The authors declare that no conflicts exist in connection with this paper. Preliminary results were presented at the American Congress Rehabilitation Medicine in Chicago. Illinois, November 2, 2016.
References
- 1.Minino AM, Murphy SL, Xu J, Kochanek KD. Deaths: final data for 2008. Natl Vital Stat Rep. 2011;59:1–126. [PubMed] [Google Scholar]
- 2.Gill TM, Gahbauer EA, Murphy TE, Han L, Allore HG. Risk factors and precipitants of long-term disability in community mobility: a cohort study of older persons. Ann Intern Med. 2012;156:131–40. doi: 10.1059/0003-4819-156-2-201201170-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kneafsey R, Clifford C, Greenfield S. What is the nursing team involvement in maintaining and promoting the mobility of older adults in hospital? A grounded theory study. Int J Nurs Stud. 2013;50:1617–29. doi: 10.1016/j.ijnurstu.2013.04.007. [DOI] [PubMed] [Google Scholar]
- 4.Barker DJ, Reid D, Cott C. The experience of senior stroke survivors: factors in community participation among wheelchair users. Can J Occup Ther. 2006;73:18–25. doi: 10.2182/cjot.05.0002. [DOI] [PubMed] [Google Scholar]
- 5.Andrenelli E, Ippoliti E, Coccia M, Millevolte M, Cicconi B, Latini L, Lagalla G, Provinciali L, Ceravolo MG, Capecci M. Features and predictors of activity limitations and participation restriction 2 years after intensive rehabilitation following first-ever stroke. Eur J Phys Rehabil Med. 2015;51:575–85. [PubMed] [Google Scholar]
- 6.Robinson CA, Shumway-Cook A, Matsuda PN, Ciol MA. Understanding physical factors associated with participation in community ambulation following stroke. Disabil Rehabil. 2011;33:1033–42. doi: 10.3109/09638288.2010.520803. [DOI] [PubMed] [Google Scholar]
- 7.Park HJ, Oh DW, Choi JD, Kim JM, Kim SY, Cha YJ, Jeon SJ. Action observation training of community ambulation for improving walking ability of patients with post-stroke hemiparesis: A randomized controlled pilot trial. Clin Rehabil. 2016 doi: 10.1177/0269215516671982. [DOI] [PubMed] [Google Scholar]
- 8.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Despres JP, Fullerton HJ, et al. Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. Circulation. 2016;133:e38–e360. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 9.Bowden MG, Woodbury ML, Duncan PW. Promoting neuroplasticity and recovery after stroke: future directions for rehabilitation clinical trials. Curr Opin Neurol. 2013;26:37–42. doi: 10.1097/WCO.0b013e32835c5ba0. [DOI] [PubMed] [Google Scholar]
- 10.Goins RT, Jones J, Schure M, Rosenberg DE, Phelan EA, Dodson S, Jones DL. Older Adults’ Perceptions of Mobility: A Metasynthesis of Qualitative Studies. Gerontologist. 2015;55:929–42. doi: 10.1093/geront/gnu014. [DOI] [PubMed] [Google Scholar]
- 11.Bernard HR, Ryan GW. Analyzing qualitative data: Systematic approaches. SAGE publications; 2009. [Google Scholar]
- 12.Garces JPD, Lopez GJP, Wang Z, Elraiyah TA, Nabhan M, Campana JPB, Boehmer K, Hasan R, Firwana B, Shippee N. A report prepared for the Patient-Centered Outcomes Research Institute. Rochester: Mayo Clinic; 2012. Eliciting patient perspective in patient-centered outcomes research: a meta narrative systematic review. [Google Scholar]
- 13.Buntin MB, Colla CH, Deb P, Sood N, Escarce JJ. Medicare spending and outcomes after post-acute care for stroke and hip fracture. Med Care. 2010;48:776. doi: 10.1097/MLR.0b013e3181e359df. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stineman MG, Rist PM, Kurichi JE, Maislin G. Disability meanings according to patients and clinicians: imagined recovery choice pathways. Qual Life Res. 2009;18:389–98. doi: 10.1007/s11136-009-9441-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xian Y, O’Brien EC, Fonarow GC, Olson DM, Schwamm LH, Hannah D, Lindholm B, Maisch L, Lytle BL, Greiner MA, et al. Patient-Centered Research into Outcomes Stroke Patients Prefer and Effectiveness Research: Implementing the patient-driven research paradigm to aid decision making in stroke care. Am Heart J. 2015;170:36–45. e1–11. doi: 10.1016/j.ahj.2015.04.008. [DOI] [PubMed] [Google Scholar]
- 16.Portney LG, Watkins MP. Foundations of clinical research: applications to practice. Prentice Hall; Upper Saddle River, NJ: 2000. [Google Scholar]
- 17.Reja U, Manfreda KL, Hlebec V, Vehovar V. Open-ended vs. close-ended questions in web questionnaires. Developments in applied statistics. 2003;19:159–77. [Google Scholar]
- 18.Brod M, Tesler LE, Christensen TL. Qualitative research and content validity: developing best practices based on science and experience. Qual Life Res. 2009;18:1263–78. doi: 10.1007/s11136-009-9540-9. [DOI] [PubMed] [Google Scholar]
- 19.Rabionet SE. How I learned to design and conduct semi-structured interviews: An ongoing and continuous journey. The Qualitative Report. 2011;16:563. [Google Scholar]
- 20.Adams WC. Handbook of Practical Program Evaluation. 2010. Conducting semi-structured interviews; p. 365. [Google Scholar]
- 21.Taylor SJ, Bogdan R, DeVault M. Introduction to qualitative research methods: A guidebook and resource. John Wiley & Sons; 2015. [Google Scholar]
- 22.Miles MB, Huberman AM, Saldana J. Qualitative data analysis: A methods sourcebook. SAGE Publications; 2013. Incorporated. [Google Scholar]
- 23.Johansson MB, Carlsson M, Sonnander K. Communication difficulties and the use of communication strategies: from the perspective of individuals with aphasia. Int J Lang Commun Disord. 2012;47:144–55. doi: 10.1111/j.1460-6984.2011.00089.x. [DOI] [PubMed] [Google Scholar]
- 24.Kerr J, Hilari K, Litosseliti L. Information needs after stroke: What to include and how to structure it on a website. A qualitative study using focus groups and card sorting. Aphasiology. 2010;24:1170–96. [Google Scholar]
- 25.QSR International Pty Ltd. NVivo Qualitative Data Analysis Software.(Version 10) QSR International Pty Ltd; Doncaster,, Vic, Australia: 2012. [Google Scholar]
- 26.Shenton AK. Strategies for ensuring trustworthiness in qualitative research projects. Education for information. 2004;22:63–75. [Google Scholar]
- 27.Schwandt TA, Lincoln YS, Guba EG. Judging interpretations: But is it rigorous? Trustworthiness and authenticity in naturalistic evaluation. New directions for evaluation. 2007;2007:11–25. [Google Scholar]
- 28.Arora VM, Prochaska ML, Farnan JM, D’Arcy MJt, Schwanz KJ, Vinci LM, Davis AM, Meltzer DO, Johnson JK. Problems after discharge and understanding of communication with their primary care physicians among hospitalized seniors: a mixed methods study. J Hosp Med. 2010;5:385–91. doi: 10.1002/jhm.668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kristensen HK, Tistad M, Koch L, Ytterberg C. The Importance of Patient Involvement in Stroke Rehabilitation. PLoS One. 2016;11:e0157149. doi: 10.1371/journal.pone.0157149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.O’Brien EC, Xian Y, Fonarow GC, Olson DM, Schwamm LH, Hernandez AF. Clinical commentary on “Certain uncertainty: life after stroke from the patient’s perspective”. Circ Cardiovasc Qual Outcomes. 2014;7:970. doi: 10.1161/CIRCOUTCOMES.114.001484. [DOI] [PubMed] [Google Scholar]
- 31.Barnsley L, McCluskey A, Middleton S. What people say about travelling outdoors after their stroke: a qualitative study. Aust Occup Ther J. 2012;59:71–8. doi: 10.1111/j.1440-1630.2011.00935.x. [DOI] [PubMed] [Google Scholar]
- 32.Ing MM, Vento MA, Nakagawa K, Linton KF. A Qualitative Study of Transportation Challenges Among Intracerebral Hemorrhage Survivors and Their Caregivers. Hawai’i Journal of Medicine & Public Health. 2014;73:353–7. [PMC free article] [PubMed] [Google Scholar]
- 33.Skolarus LE, Burke JF, Freedman VA. The role of accommodations in poststroke disability management. J Gerontol B Psychol Sci Soc Sci. 2014;69(Suppl 1):S26–34. doi: 10.1093/geronb/gbu117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hannah D, Lindholm B, Maisch L. Certain uncertainty: life after stroke from the patient’s perspective. Circ Cardiovasc Qual Outcomes. 2014;7:968–9. doi: 10.1161/CIRCOUTCOMES.114.001315. [DOI] [PubMed] [Google Scholar]
- 35.Hammel J, Magasi S, Heinemann A, Gray DB, Stark S, Kisala P, Carlozzi NE, Tulsky D, Garcia SF, Hahn EA. Environmental barriers and supports to everyday participation: a qualitative insider perspective from people with disabilities. Arch Phys Med Rehabil. 2015;96:578–88. doi: 10.1016/j.apmr.2014.12.008. [DOI] [PubMed] [Google Scholar]
- 36.Lloyd A, Roberts AR, Freeman JA. ‘Finding a balance’ in involving patients in goal setting early after stroke: a physiotherapy perspective. Physiother Res Int. 2014;19:147–57. doi: 10.1002/pri.1575. [DOI] [PubMed] [Google Scholar]
- 37.Plant SE, Tyson SF, Kirk S, Parsons J. What are the barriers and facilitators to goal-setting during rehabilitation for stroke and other acquired brain injuries? A systematic review and meta-synthesis. Clinical Rehabilitation. 2016;30:921–30. doi: 10.1177/0269215516655856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nelson ML, Hanna E, Hall S, Calvert M. What makes stroke rehabilitation patients complex? Clinician perspectives and the role of discharge pressure. Journal of Comorbidity. 2016;6:35–41. doi: 10.15256/joc.2016.6.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Leach E, Cornwell P, Fleming J, Haines T. Patient centered goal-setting in a subacute rehabilitation setting. Disabil Rehabil. 2010;32:159–72. doi: 10.3109/09638280903036605. [DOI] [PubMed] [Google Scholar]
- 40.Mohd Nordin NA, Aziz NA, Abdul Aziz AF, Ajit Singh DK, Omar Othman NA, Sulong S, Aljunid SM. Exploring views on long term rehabilitation for people with stroke in a developing country: findings from focus group discussions. BMC Health Serv Res. 2014;14:118. doi: 10.1186/1472-6963-14-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Saposnik G. Ischemic Stroke Therapeutics. Springer; 2016. Virtual Reality in Stroke Rehabilitation; pp. 225–33. [Google Scholar]
- 42.Katzan IL, Fan Y, Uchino K, Griffith SD. The PROMIS physical function scale: A promising scale for use in patients with ischemic stroke. Neurology. 2016;86:1801–7. doi: 10.1212/WNL.0000000000002652. [DOI] [PubMed] [Google Scholar]