Abstract
People with severe mental illness (schizophrenia, bipolar disorder or major depressive disorder) die up to 15 years prematurely due to chronic somatic comorbidities. Sedentary behavior and low physical activity are independent yet modifiable risk factors for cardiovascular disease and premature mortality in these people. A comprehensive meta‐analysis exploring these risk factors is lacking in this vulnerable population. We conducted a meta‐analysis investigating sedentary behavior and physical activity levels and their correlates in people with severe mental illness. Major electronic databases were searched from inception up to April 2017 for articles measuring sedentary behavior and/or physical activity with a self‐report questionnaire or an objective measure (e.g., accelerometer). Random effects meta‐analyses and meta‐regression analyses were conducted. Sixty‐nine studies were included (N=35,682; 39.5% male; mean age 43.0 years). People with severe mental illness spent on average 476.0 min per day (95% CI: 407.3‐545.4) being sedentary during waking hours, and were significantly more sedentary than age‐ and gender‐matched healthy controls (p=0.003). Their mean amount of moderate or vigorous physical activity was 38.4 min per day (95% CI: 32.0‐44.8), being significantly lower than that of healthy controls (p=0.002 for moderate activity, p<0.001 for vigorous activity). People with severe mental illness were significantly less likely than matched healthy controls to meet physical activity guidelines (odds ratio = 1.5; 95% CI: 1.1‐2.0, p<0.001, I2=95.8). Lower physical activity levels and non‐compliance with physical activity guidelines were associated with male gender, being single, unemployment, fewer years of education, higher body mass index, longer illness duration, antidepressant and antipsychotic medication use, lower cardiorespiratory fitness and a diagnosis of schizophrenia. People with bipolar disorder were the most physically active, yet spent most time being sedentary. Geographical differences were detected, and inpatients were more active than outpatients and those living in the community. Given the established health benefits of physical activity and its low levels in people with severe mental illness, future interventions specifically targeting the prevention of physical inactivity and sedentary behavior are warranted in this population.
Keywords: Physical activity, sedentary behavior, severe mental illness, schizophrenia, bipolar disorder, major depressive disorder, physical activity guidelines, cardiovascular disease, premature mortality
People with severe mental illness (schizophrenia, bipolar disorder or major depressive disorder) have higher levels of somatic comorbidities and premature mortality than the general population1, 2, 3. A recent meta‐analysis4 documented that mortality rates are approximately two to three times increased in these people. The higher premature mortality rates are largely attributable to cardiovascular disease5.
In the general population, there is evidence that physical activity and its structured form, exercise, are broadly as effective as pharmacological interventions in preventing cardiovascular disease and reducing mortality6. However, people with severe mental illness experience a range of barriers to engaging in physical activity and exercise, such as high levels of perceived stress, somatic comorbidities, low mood, and a lack of self‐confidence and of social support7, 8, 9, 10, 11.
More recently, the impact of prolonged periods of sedentary behavior on risk of cardiovascular disease and mortality has also been noted. A large meta‐analysis of general population studies12 reported that sedentary behavior (e.g., sitting or lying down during waking hours) is independently associated with increased risk of developing cardiovascular disease, type 2 diabetes, and all‐cause mortality.
Given that reduction in sedentary behavior and an active lifestyle are related to lower cardiovascular disease risk, understanding sedentary behavior, physical activity levels and their correlates among people with severe mental illness may aid in tailoring efforts to improve their long‐term physical health outcomes13. Next to this, there is a substantial body of evidence that physical activity may have important mental health benefits in people with severe mental illness, reducing depression and improving social and cognitive functioning14, 15, 16, 17, 18, 19.
Despite growing recognition of the importance of reducing sedentary behavior and increasing physical activity levels to improve the health and wellbeing of people with severe mental illness, several important questions remain unanswered20. For instance, although people with major depressive disorder, bipolar disorder and schizophrenia have been found to be more sedentary and less physically active than controls21, 22, 23, 24, it is unclear whether differences between diagnostic subgroups exist. Identifying whether there are differences in sedentary behavior and physical activity levels between these clinical groups may assist in developing rehabilitation priorities to prevent or reduce the risk for somatic comorbidities and premature mortality.
Pooling data across major diagnostic categories also allows for a large‐scale investigation of the role of demographic and clinical variables (gender, age, illness duration, employment status, educational level, marital status), physical health measures (body mass index, cardiorespiratory fitness levels), other lifestyle (smoking, alcohol use) and treatment‐related factors (psychotropic medication use), geographical differences, differences between treatment settings (e.g., outpatients versus inpatients) and differences in physical activity and sedentary behavior assessment (e.g., subjective versus objective assessments). Outcomes of these analyses will assist identification of specific vulnerable subgroups, environmental factors (e.g., differences in health‐related policies or available facilities) and assessment methods.
The aims of the present global systematic review and meta‐analysis were to: a) establish the mean time people with severe mental illness spend being sedentary or physically active (at light, moderate and high intensity) per day, b) investigate differences between clinical subgroups, c) investigate predictors of physical activity and sedentary behavior using meta‐regression analyses and d) explore differences in physical activity and sedentary behavior between people with severe mental illness and age‐ and gender‐matched healthy comparison subjects.
METHODS
This systematic review was conducted in accordance with the MOOSE guidelines25 and in line with the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) standard26.
Eligibility criteria
We included studies: a) with observational (cross‐sectional, retrospective or prospective) and clinical or randomized controlled trial designs having baseline data; b) in adults with a diagnosis – established through standard procedures (e.g., structured or semi‐structured diagnostic interviews) – of schizophrenia or related psychotic disorders, bipolar disorder or major depressive disorder according to DSM or ICD, irrespective of clinical setting (inpatient, outpatient, community or mixed); c) measuring physical activity and sedentary behavior using either self‐report questionnaires (e.g., the International Physical Activity Questionnaire, IPAQ27) or objective measures (e.g., accelerometer).
Physical activity was defined as any activity that involved bodily movement produced by skeletal muscles and that required energy expenditure28, while sedentary behavior was defined as an energy expenditure ≤1.5 metabolic equivalents of task (METs), while in a sitting or reclining posture during waking hours29.
We excluded studies restricted to patients with or without cardiovascular diseases, or with no adequate measure of physical activity or sedentary behavior (i.e., no mean time per day engaged in light, moderate or high intensity physical activity, or sedentary behavior).
Search criteria, study selection and critical appraisal
Two independent authors (DV, BS) searched PubMed, PsycARTICLES, Embase and Cumulative Index to Nursing and Allied Health Literature (CINAHL) from database inception to April 1, 2017, without language restrictions.
Key words used were “physical activity” OR “exercise” OR “sedent*” OR “sitting” OR “lying” OR “screen time” AND “severe mental illness” OR “serious mental illness” OR “schizophrenia” OR “psychosis” OR “bipolar disorder” OR “depression” OR “depressive disorder” in the title, abstract or index term fields.
Manual searches were also conducted using the reference lists from recovered articles and recent systematic reviews21, 22, 23, 24. Clinicaltrials.gov, www.crd.york.ac.uk/prospero and www.who.int/trialsearch were searched to identify any unpublished trials.
After removal of duplicates, the reviewers screened titles and abstracts of all potentially eligible articles. Both authors applied the eligibility criteria, and a list of full text articles was developed through consensus. Next, the two reviewers considered the full texts of these articles and the final list of included articles was reached through consensus. A third reviewer (FS) was available for mediation throughout this process. Methodological appraisal included evaluation of bias (confounding, overlapping data, publication bias).
Outcomes
The co‐primary outcomes were the mean time (min) per day that people with severe mental illness and healthy controls (in case‐control studies) engaged in physical activity, or were sedentary. We collected separate data for light, moderate and vigorous physical activity, in addition to total physical activity, as defined by the original authors, if these data were reported.
We also collected data on those not meeting the physical activity guidelines of 150 min of at least moderate intensity physical activity per week30, and physical activity behavior among healthy controls where this was reported.
Data extraction
One author (DV) extracted data using a pre‐determined data extraction form, which was independently validated by two authors (BS and FS). The data extracted included first author, country, geographical region (Europe, North America, South America, Asia, Africa, Oceania), income status of the country (low or middle versus high according to the World Bank classification), setting (inpatient, outpatient, community, mixed), diagnostic group (schizophrenia spectrum, bipolar disorder, major depressive disorder), type of study (cross‐sectional, prospective, retrospective, clinical or randomized controlled trial), age (years), gender (% males), employment status (% employed), educational level (% with low education: elementary school or none), marital status (% single), psychotropic medication use (% taking antipsychotics, antidepressants, mood stabilizers), smoking (% current smokers), alcohol use (units of alcohol per day), body mass index (kg/m2), cardiorespiratory fitness status (maximal oxygen uptake, ml/kg/min), physical activity and sedentary behavior assessment method (objective or self‐report), and the primary outcomes.
Statistical analyses
Due to anticipated heterogeneity, a random effects meta‐analysis was employed. Heterogeneity was measured by the I2 statistic, with values above 75 considered as a high level of heterogeneity31.
The meta‐analysis was undertaken in the following steps. First, we pooled data on each physical activity category and sedentary behavior for people with severe mental illness. Next, we compared physical activity and sedentary behavior levels between people with schizophrenia, bipolar disorder or major depressive disorder and general population control groups that were matched on age and gender, using data from studies in which they were directly compared. In both analyses, only comparisons of specific severe mental illness groups or a severe mental illness group with a matched general population group were included that had been performed within the same study, in order to minimize variability due to different sampling and assessment procedures. We also conducted subgroup analyses to investigate differences between the three main diagnostic subgroups, between settings and geographical regions, and between physical activity assessment methods (i.e., self‐reported vs. objective measures).
Further, we conducted meta‐regression analyses (if the number of studies was at least 4) to investigate potential moderators: age (years), % males, % unemployed, % single, % with low education, illness duration (years), % antipsychotic medication use, % antidepressant medication use, smoking prevalence, number of alcohol drinks per day, body mass index (kg/m2), and cardiorespiratory fitness levels (ml/kg/min), using the Comprehensive Meta‐Analysis software (version 3).
Publication bias was tested using the Egger's regression method32 and Begg‐Mazumdar test33, with a p value <0.05 suggesting the presence of bias. When we encountered publication bias, we conducted a trim and fill‐adjusted analysis to remove the most extreme small studies from the positive side of the funnel plot, and recalculated the effect size iteratively, until the funnel plot was symmetrical around the (new) effect size.
RESULTS
Study selection and included participants
The electronic database searches identified 526 articles (excluding irrelevant papers and duplicates) which were considered at the title and abstract level. Four‐hundred seventy full texts were reviewed and 401 were excluded (see Figure 1), with 69 unique studies (including 83 study estimates) meeting the eligibility criteria.
Figure 1.
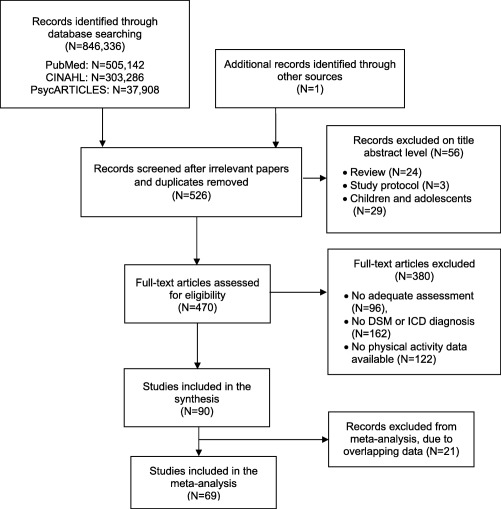
Flow diagram for the search results
The final sample comprised 35,682 unique persons with severe mental illness (mean age 43.0 years; 39.5% male) and 2,933 controls. The median sample size was 46. At study level, the mean illness duration of people with severe mental illness was 16.6 years (range 1.9‐31.6), the mean body mass index was 29.1 kg/m2 (range 23.5‐38.0) and the mean maximum oxygen uptake (measure of cardiorespiratory fitness) was 21.4 ml/kg/min (range 14.8‐31.6). Twenty‐four studies reported the percentage of current smokers, with a mean prevalence of 42.2% (95% CI: 35.9‐48.5%).
In data available from 20 studies, 57.6% (95% CI: 45.9‐69.2%) of the participants were single. In data reported in 16 studies, 62.3% (95% CI: 51.6‐72.9%) were unemployed. Nine studies reported on the educational level, with a percentage of 31.5% (95% CI: 11.8‐51.3%) having a level equal to or lower than elementary school.
In studies reporting on psychotropic medication use, 91.8% (95% CI: 85.4‐98.1%) were prescribed antipsychotics, 46.7% (95% CI: 33.7‐59.8%) antidepressants, and 17.9% (95% CI: 0.0‐36.9%) mood stabilizers. Overall, 23 study estimates of physical activity were based on objective measures, three utilized objective and subjective measures and 57 were based on self‐report questionnaires.
Daily amount of sedentary behavior
Across 21 study estimates, people with severe mental illness were sedentary for 476.0 min (95% CI: 407.3‐545.4) per day during waking hours. While the Begg‐Mazumdar (Kendall's tau b = 0.0, p=0.97) indicated no publication bias, the Egger test (bias = 7.1; 95% CI: 0.4‐13.7, p=0.04) did. The trim and fill analysis found, however, the same amount of sedentary behavior per day (476.0 min).
People with severe mental illness were more sedentary than healthy controls (standard mean difference, SMD = 0.1; 95% CI: 0.0‐0.2, p=0.003, I2=37.1), equating to a mean difference of 10.1 minutes per day (95% CI: 1.9‐22.2).
There were geographical differences in sedentary behavior (p<0.001, I2=99.2). People in Europe were significantly less sedentary (413 min per day, 95% CI: 335‐491) than those in North America (586 min per day, 95% CI: 461‐712), South America (555 min per day, 95% CI: 266‐844) or Asia (579 min per day, 95% CI: 369‐789).
People with bipolar disorder (615 min per day, 95% CI: 456‐774) were significantly more sedentary (p<0.001, I2=99.2) than those with schizophrenia (493 min per day, 95% CI: 400‐586) or major depressive disorder (414 min per day, 95% CI: 323‐505). There were no significant differences according to the setting in which patients were living.
Greater amounts of sedentary behavior were found when assessed using objective (574 min per day, 95% CI: 479‐668) versus self‐reported measures (403 min per day, 95% CI: 322‐485) (p<0.001).
None of the variables examined significantly moderated levels of sedentary behavior (see Table 1).
Table 1.
Meta‐regressions of moderators for physical activity behavior in people with severe mental illness
| N studies | β | 95% CI | p | R2 | |
|---|---|---|---|---|---|
| Sedentary behavior | |||||
| Age (years) | 22 | 1.7 | −4.6 to 8.1 | 0.58 | 0.00 |
| Illness duration (years) | 9 | 10.5 | −1.2 to 22.4 | 0.08 | 0.36 |
| % male | 20 | −0.2 | −3.4 to 3.0 | 0.90 | 0.00 |
| Body mass index (kg/m2) | 15 | 14.3 | −1.8 to 30.5 | 0.08 | 0.05 |
| % smoking | 6 | −9.0 | −18.8 to 0.7 | 0.07 | 0.62 |
| % antipsychotics | 5 | 14.4 | −11.4 to 40.3 | 0.27 | 0.04 |
| Moderate or vigorous PA | |||||
| Age (years) | 34 | 0.7 | −0.0 to 1.5 | 0.05 | 0.00 |
| Illness duration (years) | 12 | −0.3 | −2.0 to 1.4 | 0.72 | 0.11 |
| % male | 34 | 0.3 | 0.1 to 0.6 | 0.03 | 0.05 |
| % single | 4 | −1.3 | −2.2 to −0.4 | 0.003 | 0.60 |
| % unemployed | 6 | −0.3 | −0.4 to −0.2 | <0.001 | 1.00 |
| Body mass index (kg/m2) | 28 | −3.2 | −4.9 to −1.4 | <0.001 | 0.07 |
| % smoking | 9 | 0.6 | 0.3 to 0.9 | <0.001 | 0.67 |
| % antipsychotics | 14 | 0.5 | −6.1 to 7.1 | 0.88 | 0.00 |
| % antidepressants | 10 | −0.6 | −1.2 to −0.1 | 0.02 | 0.00 |
| Maximum oxygen uptake (ml/kg/min) | 8 | 9.9 | −6.7 to 13.0 | <0.001 | 0.01 |
| Not meeting PA guidelines | |||||
| Age (years) | 27 | 0.0 | −0.0 to 0.0 | 0.17 | 0.00 |
| Illness duration (years) | 9 | 0.0 | −0.0 to 0.1 | 0.04 | 0.71 |
| % male | 27 | −0.0 | −0.0 to −0.0 | 0.11 | 0.00 |
| % single | 9 | −0.0 | −0.0 to 0.0 | 0.80 | 0.00 |
| % low educational level | 5 | 0.0 | 0.0 to 0.1 | 0.005 | 0.82 |
| Body mass index (kg/m2) | 18 | −0.0 | −0.2 to 0.1 | 0.59 | 0.00 |
| % antipsychotics | 11 | −0.0 | −0.0 to −0.0 | 0.01 | 0.61 |
PA – physical activity
Daily amount of moderate or vigorous physical activity
The mean amount of moderate or vigorous physical activity in people with severe mental illness was 38.4 min per day (95% CI: 32.0‐44.8). The Begg‐Mazumdar (Kendall's tau b = 0.5, p<0.001) and the Egger test (bias = 7.2; 95% CI: 4.0‐10.4, p<0.001) indicated there was publication bias. The trim and fill analysis confirmed, however, the same mean amount of moderate or vigorous physical activity per day (38.4 min).
People with severe mental illness engaged in less moderate physical activity (mean difference = 10.2 min, 95% CI: 17.2‐3.2; SMD=0.35; 95% CI: 0.6‐0.1, p=0.002, I2=76.8) and vigorous physical activity (mean difference = 3.2 min, 95% CI: 6.4‐1.1, SMD=0.2, 95% CI: 0.3‐0.1, p<0.001, I2=53.0) than healthy controls.
Significantly higher levels of moderate or vigorous physical activity were reported in Europe (47.6 min per day, 95% CI: 39.3‐55.9), compared to North America (26.0 min per day, 95% CI: 17.9‐34.0) and Oceania (13.1 min per day, 95% CI: 0.0‐34.2) (p<0.001, I2=97.9).
People with bipolar disorder (84.2 min per day, 95% CI: 60.3‐108.1) engaged in significantly more (p<0.001, I2=97.9) moderate or vigorous physical activity than those with schizophrenia (37.5 min per day, 95% CI: 29.1‐46.0) and major depressive disorder (28.8 min per day, 95% CI: 17.8‐41.8).
Significant differences in moderate or vigorous physical activity levels were observed according to the treatment setting where patients were assessed (p=0.001, I2=97.9). Inpatients (90.1 min per day, 95% CI: 72.7‐107.5) were more physically active than outpatients (32.5 min per day, 95% CI: 25.6‐39.5), whilst community patients were the least active (16.0 min per day, 95% CI: 9.5‐22.5).
There were no significant differences between objective and subjective measures of moderate or vigorous physical activity, but significantly lower levels of vigorous physical activity (p=0.04, I2=95.8) were reported with objective measures (2.4 min per day, 95% CI: 0.0‐4.8) vs. subjective reports (7.2 min per day, 95% CI: 5.7‐8.7).
Meta‐regression analysis (Table 1) illustrated that a higher percentage of people taking antidepressants, a lower percentage of male and single participants, a higher percentage of unemployment, a lower percentage of smokers, a higher body mass index and a lower cardiorespiratory fitness were associated with lower moderate or vigorous physical activity levels.
Across 28 study estimates and 29,523 people with severe mental illness, 54.7% (95% CI: 48.8‐60.6%; p<0.001, I2=95.8) did not meet the recommended 150 min of moderate physical activity per week. While the Begg‐Mazumdar (Kendall's tau b = 0.1, p=0.58) indicated there was no publication bias, the Egger test (bias = 3.1; 95% CI: 1.3‐4.9; p=0.002) did. The trim and fill analysis found a lower rate (N adjustments = 7): 44.9% (95% CI: 38.2‐49.7%).
People with severe mental illness were more likely not to meet the physical activity guidelines than healthy controls (odds ratio = 1.5; 95% CI: 1.1‐2.0, p<0.001, I2=95.8).
People with bipolar disorder (31.4%, 95% CI: 12.8‐58.9) were less likely not to meet the guidelines than those with schizophrenia (54.8%, 95% CI: 43.4‐65.6%) and major depressive disorder (60.2%, 95% CI: 49.5‐69.9%). There were no significant differences between settings. The proportion meeting the target was similar when assessed via objective measures (57.0%, 95% CI: 37.7‐74.4%) or subjective questionnaires (54.5%, 95% CI: 48.2‐60.6%). Meta‐regression analysis demonstrated that longer illness duration, lower educational level, and antipsychotic medication prescription were associated with a greater likelihood of not meeting the physical activity target (see Table 1).
DISCUSSION
The present meta‐analysis is the first to examine sedentary behavior and physical activity levels and relevant predictors in people with severe mental illness using all of the data available around the world. Data indicated that these people are more sedentary than age‐ and gender‐matched controls from the general population, spending a mean of 476 min per day (or almost 8 hours) during waking hours in sedentary behavior. In addition, people with severe mental illness are significantly less physically active and spend only an average of 38.4 min per day in moderate or vigorous physical activity. Meta‐regression analysis revealed that a higher body mass index is associated with lower moderate or vigorous physical activity. Antidepressant prescription, male gender, unemployment, non‐tobacco use, and being single are associated with lower moderate or vigorous physical activity levels.
In addition, our analyses revealed that approximately half of people with severe mental illness do not meet the recommendation of at least 150 min of moderate physical activity per week, and that these people are 50% more likely not to meet this physical activity target compared to matched healthy controls. Not meeting physical activity guidelines is associated with longer illness duration, less years of education and antipsychotic medication prescription. Overall, not meeting physical activity guidelines is estimated to occur in around 30% of the world population34. Moreover, in the general population, it is estimated that a decrease of 10% in the number of people not meeting these guidelines could result in averting 533,000 premature deaths each year35. Reducing sedentary behavior and increasing physical activity levels of people with severe mental illness should therefore be a global public health priority. Our findings support recent calls to expand individual‐focused and community‐level interventions at a global level in order to reduce excess mortality in people with severe mental illness36, 37.
We found significant geographical differences. People with severe mental illness in Europe tend to have the highest moderate or vigorous physical activity levels. One possible explanation is that in many European mental health care settings, in contrast with elsewhere in the world38, 39, 40, physical activity is an integral part of the multidisciplinary treatment of people with severe mental illness41. These findings indicate that, although interest in physical activity in the treatment of these people is increasing, the potential utility of physical activity interventions as an integrated component of standard care is yet to be fully embraced in most parts of the world.
The higher levels of moderate or vigorous physical activity in inpatients suggest that there is increasing interest in aerobic exercise as a valuable treatment modality in psychiatric centres42, especially when delivered by specialized health care professionals43, 44. In regions with limited resources, where such specialists are not readily available, the existing workforce should be trained in assisting patients to reduce sedentary habits and adopt a more active lifestyle45, 46, 47, 48. In these low‐resource contexts, in particular in outpatient and community settings, a stepped‐care approach, where patients start with self‐management, may be a feasible strategy. Then, if patients do not achieve guideline‐specific levels of physical activity, they could continue with a manualized approach under the supervision of a non‐specialist (e.g., a nurse). Patients would only be referred to a specialist clinician (e.g., an exercise physiologist or physiotherapist) if no significant increase in physical activity levels occurs.
Our data documented that higher body mass index, lower cardiorespiratory fitness, and antidepressant or antipsychotic prescription might constitute barriers for engaging in physical activity. The association between antidepressant or antipsychotic prescription and less physical activity may be due to fatigue as a medication side effect. On the other hand, a psychotropic medication prescription might as well be a measure‐of‐proxy for illness severity. Due to the limited data available, we were not able to assess the role of individual psychiatric symptoms and illness severity in sedentary behavior and physical activity levels.
Our analyses also demonstrated that socio‐demographic factors should be considered. Those who are single or unemployed, those with a low educational level and men are less physically active. Novel strategies targeting outpatient and community programs are warranted, as we consistently found that inpatients engaged in higher levels of physical activity.
In our study, people with schizophrenia were the least physically active. While people with bipolar disorder were the most physically active, they were also the most sedentary diagnostic subgroup, indicating that both physical activity and sedentary behavior should be considered. In people with severe mental illness, sedentary behavior should be considered independent from physical activity and has been associated with poorer cognition49 and a worse metabolic profile50. Therefore, interventions to reduce sedentary behavior should be a major treatment focus. Pragmatic and feasible interventions to reduce sedentary behavior may include encouraging patients to rise from a chair and move around during television commercial breaks, or adding brief (e.g., less than or equal to 5 min) walks throughout the day, for example walking short distances rather than using motorized transport51.
Although many people with severe mental illness are unemployed, those who continue working in more sedentary environments, such as office workers, should be supported in the use of sit‐to‐stand desks as an effective way to reduce sedentary time52. In addition, there is provisional evidence that, as in the general population53, higher levels of physical activity may ameliorate the relationship between sedentary behavior and metabolic risk54, which adds to the pressing need to promote physical activity in this population.
Another interesting finding in our subgroup analyses was that objective measurement of physical activity resulted in higher estimates of sedentary behavior and lower estimates of vigorous physical activity compared to self‐report questionnaires. In contrast with general population studies, this result suggests that people with severe mental illness may underestimate the amount of sedentary behavior they engage in and overestimate their vigorous physical activity levels. There have been concerns that reliance on self‐report may lead to inaccurate estimates of physical activity in people with severe mental illness55, which may be exacerbated by cognitive impairment which is frequently present among people with schizophrenia and bipolar disorder56 as well as major depression57. Clearly, this calls for the development of more accurate and clinically useful measures for clinical practice, if we are to monitor and record physical activity in routine care58.
Finally, a somewhat counter‐intuitive finding was the association between higher moderate or vigorous physical activity levels and higher prevalence of tobacco smoking. It may be that individuals with severe mental illness who smoke at low levels have an increased affinity for physical activity, perhaps because of its reward‐related reinforcing effects. However, more research is needed to understand this relationship.
Whilst the results of this meta‐analysis are novel, several limitations should be noted. First, the vast majority of the studies included relied on data drawn from self‐report questionnaires. Second, we encountered high heterogeneity in the meta‐analyses we undertook, which is expected when pooling observational data25. However, our subgroup and meta‐regression analyses explained a large part of the between‐study heterogeneity. Third, there was inadequate information regarding specific medications prescribed, which precluded meta‐analytical or meta‐regression analyses. Fourth, the data were cross‐sectional and to date there is a paucity of longitudinal physical activity research in people with severe mental illness. Future research is required to understand the impact of specific antipsychotics, antidepressants and mood stabilizers on sedentary and physical activity behavior. Nevertheless, allowing for these caveats, the current meta‐analysis provides important information for clinicians and researchers.
In conclusion, our data document that people with severe mental illness engage in significantly more sedentary behavior and significantly less physical activity compared to healthy controls, and are less likely to meet physical activity targets as embodied in international guidelines. Addressing these modifiable risk factors for premature mortality through the implementation of evidence‐based sedentary behavior reduction and physical activity promotion interventions is an international imperative. We identified a number of potentially modifiable correlates of sedentary behavior and physical activity in this vulnerable population. Translation of evidence‐based interventions into routine care specifically aimed to reducing sedentary behavior and increasing physical activity is urgently required.
ACKNOWLEDGEMENTS
B. Stubbs and F. Gaughran receive support from the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care South London at King's College Hospital National Health Service (NHS) Foundation Trust and the Stanley Medical Research Institute. F. Gaughran is also supported by the NIHR Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King's College London. This paper represents independent research and the views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
REFERENCES
- 1. De Hert M, Correll CU, Bobes J et al. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry 2011;10:52‐77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Vancampfort D, Stubbs B, Mitchell AJ et al. Risk of metabolic syndrome and its components in people with schizophrenia and related psychotic disorders, bipolar disorder and major depressive disorder: a systematic review and meta‐analysis. World Psychiatry 2015;14:339‐47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Vancampfort D, Correll CU, Galling B et al. Diabetes mellitus in people with schizophrenia, bipolar disorder and major depressive disorder: a systematic review and large scale meta‐analysis. World Psychiatry 2016;15:166‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta‐analysis. JAMA Psychiatry 2015;72:334‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Correll CU, Solmi M, Veronese N et al. Prevalence, incidence and mortality from cardiovascular disease in patients with pooled and specific severe mental illness: a large‐scale meta‐analysis of 3,211,768 patients and 113,383,368 controls. World Psychiatry 2017;16:163‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Naci H, Ioannidis JP. Comparative effectiveness of exercise and drug interventions on mortality outcomes: metaepidemiological study. BMJ 2013;347:f5577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Firth J, Rosenbaum S, Stubbs B et al. Motivating factors and barriers towards exercise in severe mental illness: a systematic review and meta‐analysis. Psychol Med 2016;46:2869‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Vancampfort D, Correll CU, Probst M et al. A review of physical activity correlates in patients with bipolar disorder. J Affect Disord 2013;145:285‐91. [DOI] [PubMed] [Google Scholar]
- 9. Vancampfort D, Knapen J, Probst M et al. A systematic review of correlates of physical activity in patients with schizophrenia. Acta Psychiatr Scand 2012;125:352‐62. [DOI] [PubMed] [Google Scholar]
- 10. Vancampfort D, Stubbs B, Sienaert P et al. What are the factors that influence physical activity participation in individuals with depression? A review of physical activity correlates from 59 studies. Psychiatr Danub; 2015;27:210. [PubMed] [Google Scholar]
- 11. Speyer H, Nørgaard HCB, Birk M et al. The CHANGE trial: no superiority of lifestyle coaching plus care coordination plus treatment as usual compared to treatment as usual alone in reducing risk of cardiovascular disease in adults with schizophrenia spectrum disorders and abdominal obesity. World Psychiatry 2016;15:155‐65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Biswas A, Oh PI, Faulkner GE et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta‐analysis. Ann Intern Med 2015;162:123‐32. [DOI] [PubMed] [Google Scholar]
- 13. Ward MC, White DT, Druss BG. A meta‐review of lifestyle interventions for cardiovascular risk factors in the general medical population: lessons for individuals with serious mental illness. J Clin Psychiatry 2015;76:e477‐86. [DOI] [PubMed] [Google Scholar]
- 14. Rosenbaum S, Tiedemann A, Sherrington C et al. Physical activity interventions for people with mental illness: a systematic review and meta‐analysis. J Clin Psychiatry 2014;75:964‐74. [DOI] [PubMed] [Google Scholar]
- 15. Schuch FB, Vancampfort D, Richards J et al. Exercise as a treatment for depression: a meta‐analysis adjusting for publication bias. J Psychiatr Res 2016;77:42‐51. [DOI] [PubMed] [Google Scholar]
- 16. Firth J, Cotter J, Elliott R et al. A systematic review and meta‐analysis of exercise interventions in schizophrenia patients. Psychol Med 2015;45:1343‐61. [DOI] [PubMed] [Google Scholar]
- 17. Firth J, Stubbs B, Rosenbaum S et al. Aerobic exercise improves cognitive functioning in people with schizophrenia: a systematic review and meta‐analysis. Schizophr Bull 2017;43:546‐56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Melo MCA, Daher EDF, Albuquerque SGC et al. Exercise in bipolar patients: a systematic review. J Affect Disord 2016;198:32‐8. [DOI] [PubMed] [Google Scholar]
- 19. Biddle S. Physical activity and mental health: evidence is growing. World Psychiatry 2016;15:176‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Vancampfort D, Rosenbaum S, Probst M et al. Top 10 research questions to promote physical activity in bipolar disorders: a consensus statement from the International Organization of Physical Therapists in Mental Health. J Affect Disord 2016;195:82‐7. [DOI] [PubMed] [Google Scholar]
- 21. Stubbs B, Williams J, Gaughran F et al. How sedentary are people with psychosis? A systematic review and meta‐analysis. Schizophr Res 2016;171:103‐9. [DOI] [PubMed] [Google Scholar]
- 22. Vancampfort D, Firth J, Schuch F et al. Physical activity and sedentary behavior in people with bipolar disorder: a systematic review and meta‐analysis. J Affect Disord 2016;201:145‐52. [DOI] [PubMed] [Google Scholar]
- 23. Schuch F, Vancampfort D, Firth J et al. Physical activity and sedentary behavior in people with major depressive disorder: a systematic review and meta‐analysis. J Affect Disord 2017;210:139‐50. [DOI] [PubMed] [Google Scholar]
- 24. Stubbs B, Firth J, Berry A et al. How much physical activity do people with schizophrenia engage in? A systematic review, comparative meta‐analysis and meta‐regression. Schizophr Res 2016;176:431‐40. [DOI] [PubMed] [Google Scholar]
- 25. Stroup DF, Berlin JA, Morton SC et al. Meta‐analysis of observational studies in epidemiology: a proposal for reporting. Meta‐analysis of observational studies in epidemiology (MOOSE) group. JAMA 2000;283:2008‐12. [DOI] [PubMed] [Google Scholar]
- 26. Moher D, Liberati A, Tetzlaff J et al. Preferred Reporting Items for Systematic Reviews and Meta‐Analyses: the PRISMA Statement. PLoS Med 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Craig C, Marshall A, Sjostrom M et al. International physical activity questionnaire:12‐country reliability and validity. Med Sci Sports Exerc 2003;35:1381‐95. [DOI] [PubMed] [Google Scholar]
- 28. Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health‐related research. Publ Health Rep 1985;100:126. [PMC free article] [PubMed] [Google Scholar]
- 29. Cart LRSM . Letter to the editor: standardized use of the terms “sedentary” and “sedentary behaviours”. Appl Physiol Nutr Metab 2012;37:540. [DOI] [PubMed] [Google Scholar]
- 30. Vancampfort D, De Hert M, Skjerven LH et al. International Organization of Physical Therapy in Mental Health consensus on physical activity within multidisciplinary rehabilitation programmes for minimising cardio‐metabolic risk in patients with schizophrenia. Disabil Rehabil 2012;34:1‐12. [DOI] [PubMed] [Google Scholar]
- 31. Higgins J. Cochrane handbook for systematic reviews of interventions. Version 5.1.0. The Cochrane Collaboration, 2011. [Google Scholar]
- 32. Egger M, Davey SG, Schneider M et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50:1088‐101. [PubMed] [Google Scholar]
- 34. Hallal PC, Andersen LB, Bull FC et al. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet 2012;380:247‐57. [DOI] [PubMed] [Google Scholar]
- 35. Lee I‐M, Shiroma EJ, Lobelo F et al. Effect of physical inactivity on major non‐communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet 2012;380:219‐29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Liu NH, Daumit GL, Dua T et al. Excess mortality in persons with severe mental disorders: a multilevel intervention framework and priorities for clinical practice, policy and research agendas. World Psychiatry 2017;16:30‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Saxena S, Maj M. Physical health of people with severe mental disorders: leave no one behind. World Psychiatry 2017;16:1‐2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Pratt SI, Jerome GJ, Schneider KL et al. Increasing US health plan coverage for exercise programming in community mental health settings for people with serious mental illness: a position statement from the Society of Behavior Medicine and the American College of Sports Medicine. Transl Behav Med 2016;6:478‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Lederman O, Grainger K, Stanton R et al. Consensus statement on the role of accredited exercise physiologists within the treatment of mental disorders: a guide for mental health professionals. Australasian Psychiatry 2016;24:347‐51. [DOI] [PubMed] [Google Scholar]
- 40. Vancampfort D, Stubbs B, De Hert M et al. A systematic review of physical activity policy recommendations and interventions for people with mental health problems in Sub‐Saharan African countries. Pan African Med J 2017;26:104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Probst M. The International Organization of Physical Therapists working in Mental Health (IOPTMH). Ment Health Phys Act 2012;5:20‐1. [Google Scholar]
- 42. Soundy A, Roskell C, Stubbs B et al. Investigating the benefits of sport participation for individuals with schizophrenia: a systematic review. Psychiatr Danub 2015;27:2‐13. [PubMed] [Google Scholar]
- 43. Vancampfort D, Rosenbaum S, Schuch FB et al. Prevalence and predictors of treatment dropout from physical activity interventions in schizophrenia: a meta‐analysis. Gen Hosp Psychiatry 2016;39:15‐23. [DOI] [PubMed] [Google Scholar]
- 44. Stubbs B, Vancampfort D, Rosenbaum S et al. Dropout from exercise randomized controlled trials among people with depression: a meta‐analysis and meta regression. J Affect Disord 2016;190:457‐66. [DOI] [PubMed] [Google Scholar]
- 45. Stubbs B, Koyanagi A, Schuch F et al. Physical activity levels and psychosis: a mediation analysis of factors influencing physical activity target achievement among 204 186 people across 46 low‐and middle‐income countries. Schizophr Bull 2016;433:536‐45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Stubbs B, Koyanagi A, Schuch F et al. Physical activity and depression: a large cross‐sectional, population‐based study across 36 low‐ and middle‐income countries. Acta Psychiatr Scand 2016;134:546‐56. [DOI] [PubMed] [Google Scholar]
- 47. Stubbs B, Koyanagi A, Veronese N et al. Physical multimorbidity and psychosis: comprehensive cross sectional analysis including 242,952 people across 48 low‐ and middle‐income countries. BMC Med 2016;14:189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Vancampfort D, Koyanagi A, Ward PB et al. Chronic physical conditions, multimorbidity and physical activity across 46 low‐ and middle‐income countries. Int J Behav Nutr Phys Act 2017;14:6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Stubbs B, Ku P‐W, Chung M‐S et al. Relationship between objectively measured sedentary behavior and cognitive performance in patients with schizophrenia vs controls. Schizophr Bull 2017:43:566‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Vancampfort D, Sienaert P, Wyckaert S et al. Sitting time, physical fitness impairments and metabolic abnormalities in people with bipolar disorder: an exploratory study. Psychiatry Res 2016;242:7‐12. [DOI] [PubMed] [Google Scholar]
- 51. Vancampfort D, Stubbs B, Ward P et al. Integrating physical activity as medicine in the care of people with severe mental illness. Aust N Z J Psychiatry 2015;49:681‐2. [DOI] [PubMed] [Google Scholar]
- 52. Alkhajah TA, Reeves MM, Eakin EG et al. Sit‐stand workstations: a pilot intervention to reduce office sitting time. Am J Prev Med 2012;43:298‐303. [DOI] [PubMed] [Google Scholar]
- 53. Ekelund U, Steene‐Johannessen J, Brown WJ et al. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta‐analysis of data from more than 1 million men and women. Lancet 2016;388:1302‐10. [DOI] [PubMed] [Google Scholar]
- 54. Stubbs B, Chen L‐J, Chung M‐S et al. Physical activity ameliorates the association between sedentary behavior and cardiometabolic risk among inpatients with schizophrenia: a comparison versus controls using accelerometry. Compr Psychiatry 2017;74:144‐50. [DOI] [PubMed] [Google Scholar]
- 55. Soundy A, Roskell C, Stubbs B et al. Selection, use and psychometric properties of physical activity measures to assess individuals with severe mental illness: a narrative synthesis. Arch Psychiatr Nurs 2014;28:135‐51. [DOI] [PubMed] [Google Scholar]
- 56. Green MF. Cognitive impairment and functional outcome in schizophrenia and bipolar disorder. J Clin Psychiatry 2006;67(Suppl. 9):3‐8. [PubMed] [Google Scholar]
- 57. Lam RW, Kennedy SH, McIntyre RS et al. Cognitive dysfunction in major depressive disorder: effects on psychosocial functioning and implications for treatment. Can J Psychiatry 2014;59:649‐54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Rosenbaum S, Ward PB. The Simple Physical Activity Questionnaire. Lancet Psychiatry 2016;3:e1. [DOI] [PubMed] [Google Scholar]


