Summary
Syndromic diarrhea/tricho-hepato-enteric syndrome (SD/THE) is a rare disease linked to the loss of function of either TTC37 or SKIV2L, two components of the SKI complex. It is characterized by a combination of 9 signs (intractable diarrhea, hair abnormalities, facial dysmorphism, immune abnormalities, IUGR/SGA, liver abnormalities, skin abnormalities, congenital heart defect and platelet abnormalities). We present a comprehensive review of the management of SD/THE and tested therapeutic regimens. A review of the literature was conducted in May 2017: 29 articles and 2 abstracts were included describing a total of 80 patients, of which 40 presented with mutations of TTC37, 14 of SKIV2L. Parenteral nutrition was used in the management of 83% of the patients and weaned in 44% (mean duration of 14.97 months). Immunoglobulins were used in 33 patients, but data on efficacy was reported for 6 patients with a diminution of infection (n = 3) or diarrhea reduction (n = 2). Antibiotics (n = 11) provided no efficacy. Steroids (n = 17) and immunosuppressant drugs (n = 13) were used with little efficacy and mostly in patients with IBD-like SD/THE. Hematopoietic stem cell transplantation (HSCT) was performed in 4 patients: 2 died, for one it corrected the immune defects but not the other features and for the last one, it provided only a partial improvement. Finally, no specific diet was effective except for some contradictory reports for elemental formula. In conclusion, the management of SD/THE mainly involves parenteral nutrition and immunoglobulin supplementation. Antibiotics, steroids, immunosuppressants, and HSCT are not recommended as principle treatments since there is no evidence of efficacy.
Keywords: TTC37, SKIV2L, very early onset IBD
1. Introduction
Syndromic diarrhea/tricho-hepato-enteric syndrome (SD/THE) is a rare disease linked to an alteration of the human SKI complex by recessive mutations of either TTC37 or SKI2VL. To date, it is characterized by the combination of 9 signs (1). As nearly constant features are found intractable diarrhea during infancy, hair abnormalities often found with presence of trichorrhexis nodosa, intra-uterine growth restriction or small size at birth for gestational age, facial dysmorphism, immune abnormalities (mostly a lack of immunoglobulin or a lack of antibody response to vaccination). The other signs seen in half of the cases are liver abnormalities, and skin abnormalities but congenital heart defects and platelet abnormalities are not often reported (1–2). To date case management involves parenteral nutrition and in some cases immunoglobulin supplementation (1). However, a lot of empirical treatments have been tried over the past 30 years because of delayed diagnosis. The aim of this review is to assess these treatments and their potential efficacy.
2. Methods
A search was done on PubMed (www.pubmed.com) in May 2017 using “trichohepatoenteric”, “tricho-hepato-enteric”, “intractable diarrhea with phenotypic anomalies”, “intractable diarrhea and trichorrhexis nodosa”, “syndromic diarrhea”, “syndromic diarrhoea” and “phenotypic diarrhea”, “stankler syndrome”, “SKIV2L” and “TTC37”. All in all, we retrieved 73 articles of which 27 had individual clinical data (3–29). A second search on Google scholar (www.scholar.google.fr) in the “cited by” article from Girault et al. (4) and Verloes et al. (5), produced 2 more articles (30–31). A search performed on abstracts from the European Society for Paediatric Gastroenterology Hepatology and Nutrition (ESPGHAN) and the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN) meetings from 2012 to 2017, produced two abstracts with unpublished data (32,33). Finally, a medical thesis provided more complete clinical data from patients that were only briefly described in reference 11 (34). Consequently, 29 articles, 2 abstracts and 1 medical thesis were included. For each case the clinical data (regarding the 9 canonical signs), genetic status, disease evolution, treatments and their efficacy were retrieved. Statistical analyses were performed with biostatgv software.
3. Results
3.1. Clinical data
Between 1982 and May 2017, 80 patients (sex ratio 35/39 for patients with recorded sex) were described as having SD/THE with some clinical data. 14 presented disease with variants in SKIV2L, 40 in TTC37, 25 were of unknown status and 1 was negative for both TTC37 and SKIV2L. The patients presented classical SD/THE symptomatology with nearly all (> 97%) presenting with intractable diarrhea, facial dysmorphism and hair abnormalities. More than 2/3 were small for gestational age, presented an immune deficiency or liver disease. Skin abnormalities (60%) and cardiac abnormalities (35%) were the least recorded signs. One third of the patients died at a mean age of 23.5 months (3–96), mostly, from infection (7 patients) or hepatic failure (7 patients) for the 18 patients with recorded information. The probability of survival for the whole cohort at 96 months was 0.64 (± 0.06) and 0.76 (± 0.07) for patients mutated in SKIV2L or TTC37 respectively, or 0.41 (± 0.11) for patients of unknown status at 87 months (p = 0.019). Table 1 summarizes the clinical data according to molecular defect. Figure 1 shows the Kaplan-Meier survival curve for the whole group of patients and compares patients according to their molecular status.
Table 1. Summary of clinical signs according to molecular defect.
| Items | All (n = 80) | Patient with mutation of TTC37 (n = 40) | Patient with mutation of SKIV2L (n = 14) | Patient not tested (n = 25) | Patient without mutation of SKIV2L or TTC37 (n = 1) |
|---|---|---|---|---|---|
| Sex (F/M) | 39/35 | 20/18 | 8/5 | 11/11 | 0/1 |
| Intractable diarrhea | 76/77 | 38/39 | 14/14 | 23/23 | 1/1 |
| Facial dysmorphism | 66/67 | 31/32 | 10/10 | 24/24 | 1/1 |
| Hair abnormalities | 71/73 | 36/36 | 11/13 | 23/23 | 1/1 |
| Trichorrhexis nodosa | 46/59 | 30/32 | 5/13 | 11/14 | |
| Immune deficiency | 48/67 | 28/36 | 5/12 | 15/18 | 0/1 |
| IUGR/SGA | 48/63 | 24/32 | 9/9 | 15/21 | 0/1 |
| Liver disease | 41/61 | 18/31 | 8/10 | 14/19 | 1/1 |
| Skin abnormalities | 29/48 | 15/24 | 6/6 | 8/17 | 0/1 |
| Hypo/hyperpigmented | 17/29 | 12/15 | 4/6 | 1/8 | |
| Cardiac abnormalities | 15/43 | 10/26 | 4/4 | 1/13 | |
| Outcome (Alive/Dead) | 56/24 | 30/10 | 13/1 | 12/13 | 1/0 |
Figure 1.
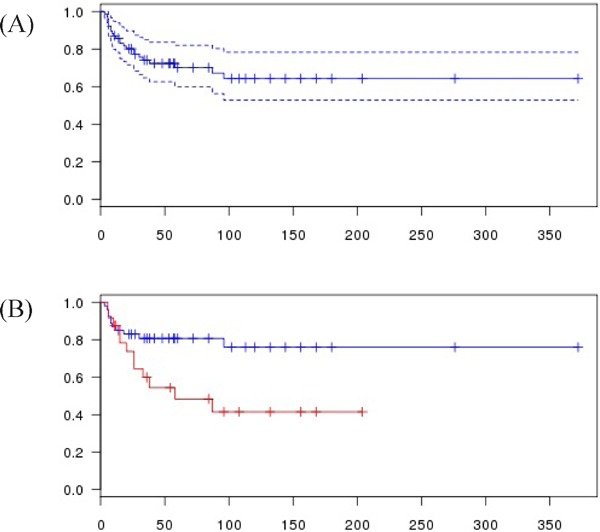
Kaplan-Meier survival curve. (A), whole cohort (dashed line 95% confidence Interval); (B), According to genetic status (mutated in SKIV2L or TTC37 in blue, Unknown in red); p = 0.019. Time in month
3.2. Therapeutics
Table 2 and 3 summarizes the therapeutic and dietetic management for the 80 patients according to molecular defect. A detailed account is given in the following paragraphs.
Table 2. Summary of therapeutic management according to molecular defect.
| Items | All (n = 80) | Patient with mutation of TTC37 (n = 40) | Patient with mutation of SKIV2L (n = 14) | Patient not tested (n = 25) | Patient without mutation of SKIV2L or TTC37 (n = 1) |
|---|---|---|---|---|---|
| Parenteral nutrition | 59/71 | 29/34 | 11/13 | 18/23 | 1/1 |
| Weaning of parenteral nutrition | 22/50 | 10/23 | 5/9 | 6/17 | 1/1 |
| Mean duration in month of parenteral nutrition for weaned patients | 14.97 (1–55) | 12.6 (1–29) | 10.62 (4–24) | 25 (1–55) | 6 |
| Mean duration in month of parenteral nutrition for ongoing patients | 57.09 (4–179) | 67.94 (13–55) | 105.33 (66–179) | 32.85 (4–155) | 6 |
| Immunoglobulin supplementation | 33/40 | 19/22 | 3/5 | 11/12 | 0/1 |
| Azathioprine | 5 | 2 | 2 | 1 | 0 |
| Methotrexate | 1 | 1 | 0 | 0 | 0 |
| Ciclosporine | 2 | 0 | 0 | 2 | 0 |
| Sirolimus | 2 | 1 | 1 | ||
| Tacrolimus | 3 | 2 | 1 | 0 | 0 |
| Steroids | 17 | 9 | 2 | 6 | 0 |
| TNF blockade | 7 | 5 | 2 | 0 | 0 |
| Antibiotics | 11 | 3 | 0 | 8 | 0 |
| 5 ASA | 4 | 3 | 1 | 0 | 0 |
| Hematopoietic stem cell transplantation | 4 | 3 | 0 | 1 | 0 |
Table 3. Summary of diet management according to molecular defect.
| Items | All (n = 80) | Patient with mutation of TTC37 (n = 40) | Patient with mutation of SKIV2L (n = 14) | Patient not tested (n = 25) | Patient without mutation of SKIV2L or TTC37 (n = 1) |
|---|---|---|---|---|---|
| Elemental formula | 7 | 2 | 2 | 2 | 1 |
| Lactose free diet | 3 | 2 | 1 | 0 | 0 |
| Glucose-Galactose free diet | 3 | 1 | 0 | 1 | 1 |
| Gluten free diet | 4 | 1 | 0 | 2 | 1 |
| Hydrolyzed formula | 11 | 4 | 1 | 5 | 1 |
3.2.1. Nutritional management
Parenteral nutrition was used in 83% of the patients. Nearly half had been weaned off parenteral nutrition with a mean duration of 14.97 months (1–55). However, non-weaned patients stayed on parenteral nutrition for a long period of time (Figure 2).
Figure 2.
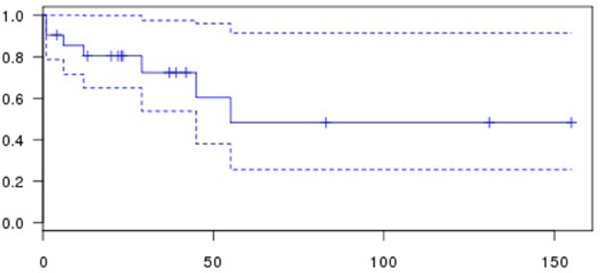
Kaplan-Meier survival curve of parenteral dependency according to the duration of parenteral nutrition (dashed line 95% confidence Interval). Time in month
3.2.2. Immunoglobulin supplementation
Thirty three patients were given immunoglobulin supplementation, but the effects were described in only 6 cases. Three reported a diminution of infection (4,19,21), 2 a reduction of diarrhea (4,23) and 1 described no effect either on diarrhea or infection (34).
3.2.3. Antibiotherapy
In 11 cases, antibiotics were used to treat SD/THE, mostly in Girault et al. (8 patients with Vancomycin, Colistimethate, Tobramycin, and Amphotericin B) but also in Busoni et al. (Vancomycin, Amoxiciline, Metronidazole, Quinolone) and in Lee et al. 2016 (Ceftriaxone, Amikacine and “aggressive antibiotics”) (4,23,27). In 10 cases (4,23) antibiotics had no effect and only in one case (27) lead to a temporary reduction in diarrhea.
3.2.4. Steroids
Steroids were administered to 17 patients (4,17,23,26,27,30,32–34). No effect was reported in 11 patients and in 5 patients only a partial amelioration was noted. In one patient (33) there were no details and it was before HSCT. It should be noted that the patients with partial effect presented with some aspect of IBD-like SD/THE (17,26,27,32). In some cases steroids were given in combination with immunosuppressant drugs.
3.2.5. Immunosuppressant drugs
Seven drugs were used for a combined total of 24 times in 13 patients (4,17,26,27,30,32,33). Thus, some patients were given multiple drugs, either sequentially or at the same time. Summing up: 5 ASA was used four times with no effect in three patients (17,27) and one case of partial amelioration in combination with steroids (27). Azathioprine was used 5 times, with no effect in 4 patients (4,17,26) and possibly a partial amelioration in one (26). Ciclosporine was used in two patients in combination with steroids: one patient died of infection (30) and the other showed only a mild improvement (4). Methotrexate was used in one patient (17) with no effect. Sirolimus was used in 2 patients without effect, Tacrolimus was used twice in 3 patients without any effect (17,26) and one before HSCT (33). Anti-TNF antibody was used in 7 patients; for one there was no description of outcome (33), for 2 (17) there was no improvement, for 3 there was a partial and inconsistant improvement (26,27,32).
Eight patients on immunosuppressive therapy were described as having an IBD-like SD/THE. Moreover, patients described in Kammermeier 2014 and 2017 (17,26) were given multiple immunosuppressant drugs (2 patients treated with 2 molecules, and 2 patients with 5). For these patients, reported in a synthetic table, it is rather hard to determine the efficacy of each therapy precisely.
3.2.6. Hematopoietic stem cell transplantation (HSCT)
HSCT was performed on 4 patients. The first one was in Girault et al., and the patient underwent two HSCT: the first was a failure and he died from severe interstitial pneumonia after the second attempt (4). Another case was reported in Kammermeier et al.: HSCT produced only a moderate improvement, however the case is very slightly reported (26). Two patients were reported in Cleminson et al.: one died, 46 days post HSCT, from adenovirus pneumonitis, the second reported successful engraftment and after nearly two years of follow-up, immunology normalized afterwards but diarrhea and failure to thrive persisted (33).
3.2.7. Diet management
For 22 patients, some information about diet was available (Table 3). 11 were given hydrolyzed formula, 7 an elemental formula, 4 a gluten free diet and 3 a lactose free diet and 3 a glucose-galactose free diet. Except for elemental formula which led to an amelioration of the diarrhea for 2 patients (21,24), all other types of diet did not improve the diarrhea. For one patient, both soy based formula and artisanal rice water with sugar cane were provided, but did not improve diarrhea (30).
Of the twelve patients who were not given parenteral nutrition, one was reported to have a normal diet (24) and one was given hydrolyzed formula (32). There is no data of the diet for the others. For the 22 patients weaned off parenteral nutrition, data are available about the diet for 11. Five patients were given elemental formula and/or gluten free and cow's-milk-free diets (18). All the others were given a different diet: no gluten or cow's milk (4), hydrolyzed formula (4), elemental formula (24), or a hydrolyzed formula, gluten free diversified diet (11,34), or normal diet with enteral supplement (24) or glucose galactose free formula (31).
4. Discussion
As far as we know, this is the first comprehensive review of the management of SD/THE. Up to now, no clinical trials have been organized, only single cases or small series are reported with only a low level of evidence. However, some elements can be highlighted. We confirm that parenteral nutrition is important in the management of SD/THE as already established in previous reviews (1,11). It also plays a vital role in the management of SD/THE, since 83% of the patients need it. However, there is some variability and 17% of the patients did not require parenteral nutrition. Except for some cases (19,24), it is not clear whether the absence of parenteral nutrition was due to non-availability or for some other reason. With parenteral nutrition, weaning can be achieved in nearly 50% of the patients as already reported in the literature (35). One of the limits with this approach is that it can also reflect different practices in different countries. Moreover, it often remains unclear if weaned patients have a good nutritional status or if some level of parenteral nutrition may still be useful. It has already been noted that SD/THE patients are of small stature despite adequate nutrition (11,35) and that in two patients growth hormone administration failed to improve growth (35).
Immunoglobulin supplementation was used in 33 patients, but the effects are rarely and poorly described. Nonetheless, an improvement of either the number of infections or of the diarrhea was noticed for 5/6 patients. Thus, immunoglobulin supplementation could probably be useful in some cases of SD/THE if an immune defect is present (notably low levels of immunoglobulin), but also in case of recurrent infection, as we know that immunoglobulin function is impaired (19). In all cases a discussion with immunologists appears mandatory.
Steroids, antibiotics or immunosuppressant drugs did not seem useful in the management of SD/THE and can even have adverse effects. The only exception is in IDB-Like SD/THE, where these drugs could be useful to some extent. However, as noted in Busoni et al., the effect seems transient or partial (27).
Hematopoietic stem cell transplantation presents only little data with no full reports. However according to the data, HSCT did not cure SD/THE, except possibly for the immune defects, but is associated with high mortality (2/4). Thus SD/THE is clearly different from defects in intestinal immune-related homeostasis like immunodysregulation polyendocrinopathy enteropathy, X-linked (IPEX) or IPEX-like disorders where either immunosuppressant drugs or HSCT could be useful (36).
For diet management, data are hard to come by and the only regimen that seems to have some effect is the elemental formula, and even then reports are contradictory. All the others did not seem to be effective. The diet of weaned patients is highly diverse thus it is hard to determine whether restrictive diets (like gluten, lactose, cow's milk free) are really useful. No suggestion can be made on the basis of the data and the choice should be made by the medical team in agreement with the patient and the family.
On a more general level, mortality is still high for SD/THE. Whereas, mortality is lower for patients with mutation of TTC37 or SKIV2L than for patients with unknown status. However, these cases could be a bias because most of the patients with unknown status are from older publications.
In conclusion, to date the management of SD/THE is mainly based on parenteral nutrition and immunoglobulin supplementation. Other drugs such as antibiotics, steroids and immunosuppressant drugs have, showed no evidence of efficacy, except in some cases of IBD-like SD/THE. HSCT could potentially treat the immune defects but does not improve the other signs and is associated with high mortality. Finally, diet management data are confusing and no clear conclusion can be made. SD/THE is a rare disease requiring management by an expert team, especially in relation to nutrition and immunity.
References
- 1. Fabre A, Martinez-Vinson C, Goulet O, Badens C. Syndromic diarrhea/Tricho-hepato-enteric syndrome. Orphanet J Rare Dis. 2013; 8:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Fabre A, Badens C. Human Mendelian diseases related to abnormalities of the RNA exosome or its cofactors. Intractable Rare Dis Res. 2014; 3:8-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Stankler L, Lloyd D, Pollitt RJ, Gray ES, Thom H, Russell G. Unexplained diarrhoea and failure to thrive in 2 siblings with unusual facies and abnormal scalp hair shafts: A new syndrome. Arch Dis Child. 1982; 57:212-216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Girault D1, Goulet O, Le Deist F, Brousse N, Colomb V, Césarini JP, de Potter S, Canioni D, Griscelli C, Fischer A, et al. Intractable infant diarrhea associated with phenotypic abnormalities and immunodeficiency. J Pediatr. 1994; 125:36-42. [DOI] [PubMed] [Google Scholar]
- 5. Verloes A, Lombet J, Lambert Y, Hubert AF, Deprez M, Fridman V, Gosseye S, Rigo J, Sokal E. Tricho-hepato-enteric syndrome: Further delineation of a distinct syndrome with neonatal hemochromatosis phenotype, intractable diarrhea, and hair anomalies. Am J Med Genet. 1997; 68:391-395. [DOI] [PubMed] [Google Scholar]
- 6. de Vries E, Visser DM, van Dongen JJ, Jacobs CJ, Hoekstra JH, van Tol MJ. Oligoclonal gammopathy in phenotypic diarrhea. J Pediatr Gastroenterol Nutr. 2000; 30:349-350. [DOI] [PubMed] [Google Scholar]
- 7. Landers MC, Schroeder TL. Intractable diarrhea of infancy with facial dysmorphism, trichorrhexis nodosa, and cirrhosis. Pediatr Dermatol. 2003; 20:432-435. [DOI] [PubMed] [Google Scholar]
- 8. Barabino AV, Torrente F, Castellano E, Erba D, Calvi A, Gandullia P. “Syndromic diarrhea” may have better outcome than previously reported. J Pediatr. 2004; 144:553-554. [DOI] [PubMed] [Google Scholar]
- 9. Dweikat I, Sultan M, Maraqa N, Hindi T, Abu-Rmeileh S, Abu-Libdeh B. Tricho-hepato-enteric syndrome: A case of hemochromatosis with intractable diarrhea, dysmorphic features, and hair abnormality. Am J Med Genet A. 2007; 143A:581-583. [DOI] [PubMed] [Google Scholar]
- 10. Fabre A, André N, Breton A, Broué P, Badens C, Roquelaure B. Intractable diarrhea with “phenotypic anomalies” and tricho-hepato-enteric syndrome: Two names for the same disorder. Am J Med Genet A. 2007; 143A:584-588. [DOI] [PubMed] [Google Scholar]
- 11. Goulet O, Vinson C, Roquelaure B, Brousse N, Bodemer C, Cézard JP. Syndromic (phenotypic) diarrhea in early infancy. Orphanet J Rare Dis. 2008; 3:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Egritas O, Dalgic B, Onder M. Tricho-hepato-enteric syndrome presenting with mild colitis. Eur J Pediatr. 2009; 168:933-935. [DOI] [PubMed] [Google Scholar]
- 13. Hartley JL, Zachos NC, Dawood B, et al. Mutations in TTC37 cause trichohepatoenteric syndrome (phenotypic diarrhea of infancy). Gastroenterology. 2010; 138:2388-2398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kotecha UH, Movva S, Puri RD, Verma IC. Trichohepatoenteric syndrome: Founder mutation in asian indians. Mol Syndromol. 2012; 3:89-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Morgan NV, Hartley JL, Setchell KD, Simpson MA, Brown R, Tee L, Kirkham S, Pasha S, Trembath RC, Maher ER, Gissen P, Kelly DA. A combination of mutations in AKR1D1 and SKIV2L in a family with severe infantile liver disease. Orphanet J Rare Dis. 2013; 8:74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bozzetti V, Bovo G, Vanzati A, Roggero P, Tagliabue PE. A new genetic mutation in a patient with syndromic diarrhea and hepatoblastoma. J Pediatr Gastroenterol Nutr. 2013; 57:e15. [DOI] [PubMed] [Google Scholar]
- 17. Kammermeier J, Drury S, James CT, Dziubak R, Ocaka L, Elawad M, Beales P, Lench N, Uhlig HH, Bacchelli C, Shah N. Targeted gene panel sequencing in children with very early onset inflammatory bowel disease--evaluation and prospective analysis. J Med Genet. 2014; 51:748-755. [DOI] [PubMed] [Google Scholar]
- 18. Monies DM, Rahbeeni Z, Abouelhoda M, Naim EA, Al-Younes B, Meyer BF, Al-Mehaidib A. Expanding phenotypic and allelic heterogeneity of tricho-hepato-enteric syndrome. J Pediatr Gastroenterol Nutr. 2015; 60:352-356. [DOI] [PubMed] [Google Scholar]
- 19. Rider NL, Boisson B, Jyonouchi S, Hanson EP, Rosenzweig SD, Casanova JL, Orange JS. Novel TTC37 mutations in a patient with immunodeficiency without diarrhea: Extending the phenotype of trichohepatoenteric syndrome. Front Pediatr. 2015; 3:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Oz-Levi D, Weiss B, Lahad A, Greenberger S, Pode-Shakked B, Somech R, Olender T, Tatarsky P, Marek-Yagel D, Pras E, Anikster Y, Lancet D. Exome sequencing as a differential diagnosis tool: Resolving mild trichohepatoenteric syndrome. Clin Genet. 2015; 87:602-603. [DOI] [PubMed] [Google Scholar]
- 21. Chong JH, Jamuar SS, Ong C, Thoon KC, Tan ES, Lai A, Aan MK, Tan WL, Foo R, Tan EC, Lau YL, Liew WK. Tricho-hepato-enteric syndrome (THE-S): Two cases and review of the literature. Eur J Pediatr. 2015; 174:1405-1411. [DOI] [PubMed] [Google Scholar]
- 22. Mahjoub FE, Imanzadeh F, Mahdavi Izadi S, Nahali Moghaddam A. Trichohepatoenteric syndrome or syndromic diarrhea-report of three members in a family, first report from Iran. Case Rep Pathol. 2016; 2016:9684910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lee WI, Huang JL, Chen CC, Lin JL, Wu RC, Jaing TH, Ou LS. Identifying mutations of the tetratricopeptide repeat domain 37 (TTC37) gene in infants with intractable diarrhea and a comparison of Asian and non-Asian phenotype and genotype: A global case-report study of a well-defined syndrome with immunodeficiency. Medicine (Baltimore). 2016; 95:e2918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lee WS, Teo KM, Ng RT, Chong SY, Kee BP, Chua KH. Novel mutations in SKIV2L and TTC37 genes in Malaysian children with trichohepatoenteric syndrome. Gene. 2016; 586:1-6. [DOI] [PubMed] [Google Scholar]
- 25. Zheng B, Pan J, Jin Y, Wang C, Liu Z. Targeted next-generation sequencing identification of a novel missense mutation of the SKIV2L gene in a patient with trichohepatoenteric syndrome. Mol Med Rep. 2016; 14:2107-2110. [DOI] [PubMed] [Google Scholar]
- 26. Kammermeier J, Dziubak R, Pescarin M, et al. Phenotypic and genotypic characterisation of inflammatory bowel disease presenting before the age of 2 years. J Crohns Colitis. 2017; 11:60-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Busoni VB, Lemale J, Dubern B, Frangi F, Bourgeois P, Orsi M, Badens C, Fabre A. IBD-like features in syndromic diarrhea/trichohepatoenteric syndrome. J Pediatr Gastroenterol Nutr. 2017; 64:37-41. [DOI] [PubMed] [Google Scholar]
- 28. Kinnear C, Glanzmann B, Banda E, Schlechter N, Durrheim G, Neethling A, Nel E, Schoeman M, Johnson G, van Helden PD, Hoal EG, Esser M, Urban M, Möller M. Exome sequencing identifies a novel TTC37 mutation in the first reported case of Trichohepatoenteric syndrome (THE-S) in South Africa. BMC Med Genet. 2017; 18:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bick D, Fraser PC, Gutzeit MF, et al. Successful application of whole genome sequencing in a medical genetics clinic. J Pediatr Genet. 2017; 6:61-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Cadena-León JF, José Francisco R, Rodríguez-Jurado Rodolfo. Diarrea crónica intratable asociada con diarrea fenotípica de la infancia (síndrome tricohepatoentérico). Acta Pediátrica de México. 2014; 35:483-489. [Google Scholar]
- 31. Salman MY, Mneimneh S, Rajab M. An infant with trichohepato-enteric syndrome: Case report. Int J Contemp Pediat. 2016; 3:1453-1455. [Google Scholar]
- 32. Roslavtseva E, Anushenko A, Tsimbalova E, et al. Two cases of trichohepato-enteric syndrome (syndromic diarrhea) complicated with Crohns-like disease. J Pediatr Gastroenterol Nutr. 2014; 58(S1):247. [Google Scholar]
- 33. Cleminson J, Andrew Cant A, Hambleton S, Flood F, Mary Slatter M, Gennery A, Emonts M, Haller W, Lawson M, Renji E, Bunn S. Similar presentation but heterogenous clinical course, gastrointestinal (GI) pathology, immunological defects in 5 children presenting with subsequently confirmed tricho-hepaticenteric syndrome (THE). J Pediatr Gastroenterol Nutr. 2017; 64(S1): 124. [Google Scholar]
- 34. Martinez-Vinson MC. Les diarrhées graves syndromiques [Medical thesis]. Université Paris Diderot-Paris, 7:2004. [Google Scholar]
- 35. Fabre A, Breton A, Coste ME, et al. Syndromic (phenotypic) diarrhoea of infancy/tricho-hepato-enteric syndrome. Arch Dis Child. 2014; 99:35-38. [DOI] [PubMed] [Google Scholar]
- 36. Pezzella V, Grimaldi G, Russo M, Mazza S, Mariniello DF, Paparo L, Elce A, Castaldo G, Canani RB. New insights and perspectives in congenital diarrheal disorders. Curr Pediatr Rep. 2017:5:156-166. [Google Scholar]


