Summary
Recurrent bile duct stones is the most common complication after gallstone surgery and the incidence is about 4–24%. Sphincter of Oddi laxity will lead to duodenal content flow into the bile or pancreatic duct. Patients with recurrent bile duct stones and Oddis sphincter laxity were intractable. Here we sought to present the possible and helpful surgical treatments for such patients. Prospective randomized clinical trial are needed for evaluating the outcome of surgical treatments.
Keywords: Recurrent bile duct stones, Odds sphincter laxity, surgical treatments
1. Introduction
Recurrent bile duct stones usually refer to bile ducts stones that reappeared 2 years after bile duct exploration operation, and is the most common long-term complication after gallstone surgery (1,2). Because there are still no effective therapies for preventing this complication, some patients have experienced bile duct stone recurrence for many times. According to literatures, the incidence of recurrent bile duct stones is about 4–24% (3–5).
Gallstones are distinguished into the following two types: cholesterol gallstones that contain more than 50% of cholesterol (nearly 75–80% of gallstones) and pigment gallstones that contain less than 30% of cholesterol by weight, which can be subdivided into black pigment gallstones (10–15%) and brown pigment gallstones (5–10%) (6–9). Cholesterol gallstones are associated with risk factors such as dyslipidemia, total parenteral nutrition, gallbladder hypomotility, gender (female), and old age. Black pigment gallstones are associated with typical hyperbilirubinbilia factors such as hemolysis, liver cirrhosis, and pathologic enterohepatic cycling of unconjugated bilirubin. Brown pigment gallstones are associated with biliary infection (10–12). Recurrent bile duct stones mostly belong to pigment gallstones. Patients with recurrent bile duct stones with Oddis sphincter laxity were intractable; here we sought to present the possible and helpful surgical treatments for such patients.
2. Causes of pigment gallstone of bile duct
2.1. Bile infection
Pigment gallstones were often associated with severe bile duct inflammation and biliary tract infection. During the operation of bile duct lithotomy, surgical instruments can damage the bile duct wall, and the compression of the T tube can also damage the bile duct wall, these can destroy bile duct mucous membrane, further cause bile infection.
By electron microscopy, it was found that bacteria were present in the core of the gallstone, suggesting that bacteria plays a major role in the formation of bile pigment gallstones (13,14). Through the bacterial culture of bile, the highest positive rate is Escherichia coli (15). The mechanism of pigment gallstone to Escherichia coli, can be understood as the bile bacteria producing beta glucuronidase, it can be combined with bilirubin hydrolysis into unconjugated bilirubin and glucuronic acid, unconjugated bilirubin and calcium binding to bilirubin precipitated calcium, thereby promoting pigment gallstone formation (16–20).
2.2. The obstruction of biliary tract
Biliary tract exploration surgery can often lead to obstruction of the biliary tract, It was often occurred in the operation of exploratory rough, postoperative T tube compression, postoperative Oddi sphincter edema (21,22). These biliary lesions can cause biliary strictures during the healing process, and then cause a series of pathological changes. When bile duct obstruction occurs, the concentrated bile was strongly stimulated by the bile duct mucosa, which stimulates the exfoliated bile duct epithelial cells as well as the aggregated bacteria to precipitate more easily, resulting in bile pigment stones (23).
2.3. Duodenal diverticulum
Duodenal diverticulum (DD) was originally descripted by Chomel in 1710, and got more detailed appraisal by Morgagni in 1762 (24–26). It was difficult to evaluate the exact incidence of DD. According to published data, DD were seen in 15–22% of post mortem studies (27–30). Most diverticula are located in the second part of the duodenum, commonly within 2.5 cm of the ampulla.
It was reported that 88.9% of patients with DD were associated with bile duct stones. In Manometeric's study, duodenal diverticulum could lead to the formation of pigment stones. They reported that the pressure in the sphincter of Oddi may be decreased. The decreased pressure might allow reflux of intestinal microfloras for a stagnant diverticulum, and then β-glucuronidase derived from bacterial would deconjugate bile pigments. It would explain why patients with duodenal diverticula are more likely to suffer from pigment stones.
2.4. Sphincter of Oddi Laxity
The sphincter of oddi (SO), a smooth musle, was initially described by Ruggero Oddi in1887 (31). Regarding to the function of SO, there are three main functions: regulation the discharge of bile and pancreatic juice, resist reflux from duodenum juice to the bile and pancreatic duct, and make the gallbladder filling.
Normally, the diameter of the duodenum papilla orifice is no more than 2–3 mm, but in some patients, the sphincter of Oddis is completely relaxed, it was called sphincter of Oddi laxity (SOL) (32). Paimary or secondary SOL mainly depends on patients whether have a history of biliary tract surgery.
In SOL patients, the sphincter of Oddi lose the ability of reflux prevention, and will lead to duodenal content flow into the bile or pancreatic duct (33). It might result in bacterial infection and imbalance of biliary PH, and then β-glucuronidase generated by E.cilo lead to the formation of pigment stones in the biliary tract.
3. Causes of Sphincter of Oddi Laxity
Currently, it is not clear for the specific causes of SOL. These causes could disrupt the normal structure of SO, which results in altered function of SO, and eventually SO can not act as “gate” function. According to published data (32,33), SOL are classified as primary and secondary based on the causes. Primary sphincter of Oddi Laxity is mainly due to congenital abnormality, congenital malformation of smooth muscle and absence of some neurotransmitter receptors can result in SOL.
Secondary SOL (SSOL), the most common, was attributed to at least two major factors. The first cause of SSOL was mechanical injury by stones that repeatedly induced large amounts of inflammation mediators. Regular contraction and relaxation of SO response to neurotransmission is impaired, which may contribute to abnormal SO relaxation. The second cause of SSOL was iatrogenic injury, which include endoscopic retrograde cholanguopancreatography (ERCP), endoscopic sphincterotomy (EST), and Biliary tract exploration surgery using a Bake's dilator. Those above injuries would induce inflammation of SO over times, and then result in SSOL.
The discharge of bile into the duodenum involves both neural and hormonal pathways. The sphincter of Oddi relaxes while gallbladder contracts, the bile is discharged into the duodenum (34,35). Neural and hormonal regulation of Sphincter of Oddi loses work when there is Oddis sphincter laxity, the basal pressue of biliary tract decreases, then resulting in gallbladder excessive filling and possible decreased discharge of bile flow into duodenum, and subsequently biliary tract cholestasis develops.
4. Surgical treatments for patients with recurrent bile duct stones and Oddis sphincter laxity
Recurrent bile duct stone, as an intractable disease, is prevalent in China. The incidence was estimated as high as 24%. In some clinical practice, recurrent bile duct stone had a tendency of Oddis sphincter laxity and always needed reoperation. However, the current methods of reoperation have not been unified, and there are few clinical comparative studies showing which surgical procedure is better.
Many methods of surgical treatments can be considered for patients with recurrent bile duct stones. These are: a) postoperative fibrocholedochoscopic extraction of stones; b) endoscopic extraction of stones; c) choledocholithotomy and T tube drainage; d) choledochojejunostomy; e) percutaneous transhepatic cholangioscopy (Figure 1).
Figure 1.
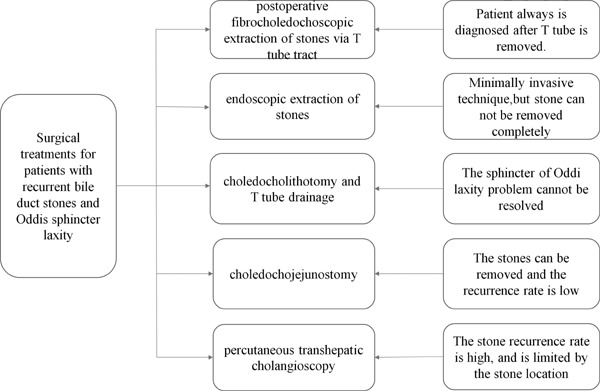
Surgical treatments for patients with recurrent bile duct stones and Oddis sphincter laxity.
Postoperatively, while T-tube is still in the common bile duct, a firm fibrous tract formed, and it is feasible to extract the recurrent stones through fibrocholedochoscopy (36,37). However, most of patients with recurrent bile duct stones were diagnosed after the removal of T-tube.
Since 1974, endoscopic sphincterotomy (EST) has been used for removal of recurrent common bile duct stones. After a successful EST, the stones can be extracted with Dormia basket (38,39). EST is generally considered both safe and effective, but the possibility of complications can not be ignored. Among the complications, post-procedural impaired Oddis sphincter is thought to be the major cause of Oddis sphincter laxity and recurrence of bile stones.
Percutaneous transhepatic cholangioscopy (PTCS), advocated in 1974, is a minimally invasive technique for removal of biliary stones. When patients with stones in more than two lobes of the liver, PTCS is a reasonable choice. Howerer, PTCS is ineffective in treatment of stenosis of bile duct and Oddis sphincter laxity (40,41). Hence, PTCS is only a temporary method of stone removal, and it can not be effective in preventing recurrence of bile duct stones.
If the stone is large and impacted in the bile duct, the above treatments may face failure. Under these circumstances, reoperation continues to be indicated for recurrent bile duct stones. Choledocholithotomy with T tube drainage and Choledochojejunostomy are the basic method in the treatment of recurrent bile duct stones. According to a retrospective study from China, when recurrent bile duct stones with Oddis sphincter laxity, the recurrence rate of bile duct stone after choledochojejunostomy was lower than that that of Choledocholithotomy with T tube drainage (42). The main reason is that choledochojejunostomy can make the bile duct drainage unobstructed. In addition, choledocholithotomy did not solve the problem of Oddis sphincter laxity, duodenal content can still flow into the bile or pancreatic duct.
5. Prospects for the future
It is generally known that recurrent bile duct stones are very common in Southeast Asian countries with high recurrence rate. Studies have shown that bile duct drainage was not unobstructed, however, there was still bile duct stones recurrence. The concurrent Oddis sphincter laxity maybe related to the recurrent bile duct stones.
By reviewing some clinical studies, we found that patients with Oddis sphincter laxity are more likely to suffer from bile duct stones and often need reoperation (43). However, there is no consensus on the surgical treatments of recurrent bile duct stones with concurrent Oddi sphincter laxity.
Oddi sphincter laxity will lead to intestinal juice reflux, biliary tract cholestasis, and further biliary tract infection, resulting in recurrence of bile duct stones. Therefore, we could conclude that Oddi sphincter laxity is one of the indirect cause of recurrent bile duct stones.
Choledochojejunostomy for the treatment obstruction of distal common bile duct have been better defined. And it was suggested that recurrent bile duct stones with Oddis sphincter laxity is also one indication of choledochojejunostomy (44). Roux-en-y Choledochojejunostomy can avoid stenosis of bile duct and make the bile drainage unobstructed. Then the high risk factor of recurrence of bile duct stones will be eliminated. Moreover, Oddi sphincter laxity often accompanied with intestinal reflux, Roux-en-y choledochojejunostomy is with ability of antireflux for some extent, which is another reason, that choledochojejunostomy can reduce or even eliminate the incidence of recurrent bile duct stones with Oddi sphincter laxity.
To our knowledge, there are no guidelines for when to perform Roux-en-y choledochojejunostomy for the treatment of patients with recurrent bile duct stones and Oddi sphincter laxity. Prospective randomized clinical trial is needed for evaluating the outcome of such surgical treatment.
Acknowledgement
This work was supported by National Natural Science Fund of China (81470860, Yuesi Zhong).
References
- 1. Oh CH, Dong SH. Recent Advances in the Management of Recurrent Bile Duct Stones. Korean J Gastroenterol. 2015; 66:251-254. (Article in Korean) [DOI] [PubMed] [Google Scholar]
- 2. Shapoval'Iants SG, Myl'Nikov AG, Pan'Kov AG, Nikonov AA, Ardasenov TB, Veselova VS. Recurrent choledocholithiasis. Diagnosis, prevention and treatment. Eksp Klin Gastroenterol. 2012; 4:32-38. (Article in Russian) [PubMed] [Google Scholar]
- 3. Tanaka M, Ikeda S, Yoshimoto H, Matsumoto S. The long-term fate of the gallbladder after endoscopic sphincterotomy. Complete follow-up study of 122 patients. Am J Surg. 1987; 154:505-509. [DOI] [PubMed] [Google Scholar]
- 4. Prat F, Malak NA, Pelletier G, Buffet C, Fritsch J, Choury AD, Altman C, Liguory C, Etienne JP. Biliary symptoms and complications more than 8 years after endoscopic sphincterotomy for choledocholithiasis. Gastroenterology. 1996; 110:894-899. [DOI] [PubMed] [Google Scholar]
- 5. Sugiyama M, Atomi Y. Risk factors predictive of late complications after endoscopic sphincterotomy for bile duct stones: Long-term (more than 10 years) follow-up study. Am J Gastroenterol. 2002; 97:2763-2767. [DOI] [PubMed] [Google Scholar]
- 6. Saharia PC, Zuidema GD, Cameron JL. Primary common duct stones. Ann Surg. 1977; 185:598-604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cariati A. Gallstone Classification in Western Countries. Indian J Surg. 2015; 77(Suppl 2):376-380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Jarrar BM, Al-Rowaili MA. Chemical composition of gallstones from Al-jouf province of saudi arabia. Malays J Med Sci. 2011; 18:47-52. [PMC free article] [PubMed] [Google Scholar]
- 9. Portincasa P, Moschetta A, Palasciano G. Cholesterol gallstone disease. Lancet. 2006; 368:230-239. [DOI] [PubMed] [Google Scholar]
- 10. Leuschner U, Guldutuna S, Hellstern A. Etiology, pathogenesis and therapy of pigment gallstones. Dig Dis. 1991; 9:282-293. [DOI] [PubMed] [Google Scholar]
- 11. Ostrow JD. The etiology of pigment gallstones. Hepatology. 1984; 4(5 Suppl):215S-222S. [DOI] [PubMed] [Google Scholar]
- 12. Soloway RD, Trotman BW, Ostrow JD. Pigment gallstones. Gastroenterology. 1977; 72:167-182. [PubMed] [Google Scholar]
- 13. Cetta FM. Bile infection documented as initial event in the pathogenesis of brown pigment biliary stones. Hepatology. 1986; 6:482-489. [DOI] [PubMed] [Google Scholar]
- 14. Wang L, Shen W, Wen J, An X, Cao L, Wang B. An animal model of black pigment gallstones caused by nanobacteria. Dig Dis Sci. 2006; 51:1126-1132. [DOI] [PubMed] [Google Scholar]
- 15. Cetta F. The role of bacteria in pigment gallstone disease. Ann Surg. 1991; 213:315-326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Stewart L, Oesterle AL, Erdan I, Griffiss JM, Way LW. Pathogenesis of pigment gallstones in Western societies: The central role of bacteria. J Gastrointest Surg. 2002; 6:891-903; discussion 903–904. [DOI] [PubMed] [Google Scholar]
- 17. Swidsinski A, Lee SP. The role of bacteria in gallstone pathogenesis. Front Biosci. 2001; 6:E93-103. [DOI] [PubMed] [Google Scholar]
- 18. Stewart L, Ponce R, Oesterle AL, Griffiss JM, Way LW. Pigment gallstone pathogenesis: Slime production by biliary bacteria is more important than beta-glucuronidase production. J Gastrointest Surg. 2000; 4:547-553. [DOI] [PubMed] [Google Scholar]
- 19. Cetta F. The role of bacteria in pigment gallstone disease. Ann Surg. 1991; 213:315-326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tabata M, Nakayama F. Bacteria and gallstones. Etiological significance. Dig Dis Sci. 1981; 26:218-224. [DOI] [PubMed] [Google Scholar]
- 21. Wernberg JA. Biliary tract surgery. Surg Clin North Am. 2014; 94:xv-xvi. [DOI] [PubMed] [Google Scholar]
- 22. Strasberg SM, Callery MP, Soper NJ. Laparoscopic hepatobiliary surgery. Prog Liver Dis. 1995; 13:349-380. [PubMed] [Google Scholar]
- 23. AYALA GA. Observations on the pathology and therapy in biliary tract surgery. Am J Gastroenterol. 1954; 22:363-381. [PubMed] [Google Scholar]
- 24. Christoforidis E, Goulimaris I, Kanellos I, Tsalis K, Dadoukis I. The role of juxtapapillary duodenal diverticula in biliary stone disease. Gastrointest Endosc. 2002; 55:543-547. [DOI] [PubMed] [Google Scholar]
- 25. Egawa N, Kamisawa T, Tu Y, Sakaki N, Tsuruta K, Okamoto A. The role of juxtapapillary duodenal diverticulum in the formation of gallbladder stones. Hepatogastroenterology. 1998; 45:917-920. [PubMed] [Google Scholar]
- 26. Kennedy RH, Thompson MH. Are duodenal diverticula associated with choledocholithiasis? Gut. 1988; 29:1003-1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kim CW, Chang JH, Kim JH, Kim TH, Lee IS, Han SW. Size and type of periampullary duodenal diverticula are associated with bile duct diameter and recurrence of bile duct stones. J Gastroenterol Hepatol. 2013; 28:893-898. [DOI] [PubMed] [Google Scholar]
- 28. Christoforidis E, Goulimaris I, Kanellos I, Tsalis K, Dadoukis I. The role of juxtapapillary duodenal diverticula in biliary stone disease. Gastrointest Endosc. 2002; 55:543-547. [DOI] [PubMed] [Google Scholar]
- 29. Egawa N, Kamisawa T, Tu Y, Sakaki N, Tsuruta K, Okamoto A. The role of juxtapapillary duodenal diverticulum in the formation of gallbladder stones. Hepatogastroenterology. 1998; 45:917-920. [PubMed] [Google Scholar]
- 30. Vaira D, Dowsett JF, Hatfield AR, Cairns SR, Polydorou AA, Cotton PB, Salmon PR, Russell RC. Is duodenal diverticulum a risk factor for sphincterotomy? Gut. 1989; 30:939-942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Toouli J. Evaluation of sphincter of Oddi function. Aust N Z J Surg. 1989; 59:445-448. [DOI] [PubMed] [Google Scholar]
- 32. Liang TB, Liu Y, Bai XL, Yu J, Chen W. Sphincter of Oddi laxity: An important factor in hepatolithiasis. World J Gastroenterol. 2010; 16:1014-1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Liang T, Su W, Zhang Q, Li G, Gao S, Lou J, Zhang Y, Ma T, Bai X. Roles of sphincter of Oddi Laxity in bile duct microenvironment in patients with Cholangiolithiasis: From the perspective of the microbiome and metabolome. J Am Coll Surg. 2016; 222:269-280.e10. [DOI] [PubMed] [Google Scholar]
- 34. Toouli J. Sphincter of Oddi: Function, dysfunction, and its management. J Gastroenterol Hepatol. 2009; 24 Suppl 3:S57-62. [DOI] [PubMed] [Google Scholar]
- 35. Afghani E, Lo SK, Covington PS, Cash BD, Pandol SJ. Sphincter of Oddi function and risk factors for dysfunction. Front Nutr. 2017; 4:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Sheen PC, Ker CG. Postoperative choledochofiberscopy. Prog Clin Biol Res. 1984; 152:303-319. [PubMed] [Google Scholar]
- 37. Chen MF, Chou FF, Wang CS, Jang YI. Experience with and complications of postoperative choledochofiberscopy for retained biliary stones. Acta Chir Scand. 1982; 148:503-509. [PubMed] [Google Scholar]
- 38. Yoon HG, Moon JH, Choi HJ, Kim DC, Kang MS, Lee TH, Cha SW, Cho YD, Park SH, Kim SJ. Endoscopic papillary large balloon dilation for the management of recurrent difficult bile duct stones after previous endoscopic sphincterotomy. Dig Endosc. 2014; 26:259-263. [DOI] [PubMed] [Google Scholar]
- 39. Itoi T, Wang HP. Endoscopic management of bile duct stones. Dig Endosc. 2010; 22 Suppl 1:S69-75. [DOI] [PubMed] [Google Scholar]
- 40. Kothaj P, Okapec S, Kudelova A. Complications after percutaneous transhepatic drainage of the biliary tract. Rozhl Chir. 2014; 93:247-254. [PubMed] [Google Scholar]
- 41. Choi JH, Lee SK. Percutaneous transhepatic cholangioscopy: Does its role still exist? Clin Endosc. 2013; 46:529-536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Han W. Comparison of therapeutis effects of different surgical treatments for recurrent bile duct stones (Master): Jilin University; Jilin, China, 2014. [Google Scholar]
- 43. Lygidakis NJ. Surgical approaches to recurrent choledocholithiasis. Choledochoduodenostomy versus T-tube drainage after choledochotomy. Am J Surg. 1983; 145:636-639. [DOI] [PubMed] [Google Scholar]
- 44. Escudero-Fabre A, Escallon AJ, Sack J, Halpern NB, Aldrete JS. Choledochoduodenostomy. Analysis of 71 cases followed for 5 to 15 years. Ann Surg. 1991; 213:635-642; discussion 643–644. [DOI] [PMC free article] [PubMed] [Google Scholar]


