Summary
Ameloblastoma is a rare low-grade odontogenic tumor of epithelial origin. The World Health Organization (WHO) has defined malignant ameloblastoma (MA) as a histologically benign-appearing ameloblastoma that has metastasized. Treatment of the primary ameloblastoma usually consists of radical excision of the tumor and adjuvant radiotherapy. Chemotherapy should be used to treat metastases due to its indolent clinical course. Presented here is the case of a 43-year-old woman who was admitted to a hospital in 2006 with a large mass involving the neck and left mandible. The mass had formed over years and had been neglected. The woman was diagnosed with a primary ameloblastoma of the mandible. Surgical resection was performed, followed by adjuvant radiotherapy. In September 2016, she was admitted again, and the findings were consistent with metastases of the previously identified ameloblastoma to the lungs. The patient was evaluated for further chemotherapy with 6 cycles of cisplatin at a dose of 100 mg/m2 on day 1, 5-FU at a dose of 1000 mg/m2/day on day 1–4 (3 wk), and pegylated filgrastim. The current case represents the classical course of a rare disease, which in this instance involved the common presentation of MA. This case is a valid incidence of MA based on the typical histology, findings from a lung biopsy, the immunohistochemical profile of the tumor, the typical clinical features, and a history of a previous primary disease.
Keywords: Ameloblastoma, ameloblastic carcinoma, metastases
1. Introduction
Ameloblastoma is a rare low-grade odontogenic tumor of epithelial origin. In most cases, it arises from the mandible (80%), but is also frequently found to affect the maxilla (20%). Despite being locally aggressive and highly recurrent after surgery, metastases from ameloblastoma are extremely rare and tend to appear years after treatment of the primary tumor (1). The World Health Organization has defined malignant ameloblastoma (MA) as a histologically benign-appearing ameloblastoma that has metastasized. Metastases are usually localized in the regional lymph nodes or distant organs – most commonly the lungs – and retain the benign characteristics of the primary neoplasm. Thus, whether metastasis will occur or not cannot be predicted based on histology. That said, an ameloblastoma displaying cellular atypia is considered to be an ameloblastic carcinoma (AC), which is a highly aggressive malignant tumor that should be treated as such. Treatment of the primary ameloblastoma usually consists of radical excision of the tumor and adjuvant radiotherapy, with the aim of minimizing the chances of recurrence and metastasis or its high-grade counterpart, i.e. ameloblastic carcinoma (2,3). However, there is considerable debate in the literature as to whether chemotherapy should be used to treat metastases due to its indolent clinical course.
2. Case Report
In 2006, a 43-year-old woman was admitted to a hospital with a large mass involving the neck and left mandible. The mass had formed over years and had been neglected. Diagnostic X-rays and a biopsy were performed. The woman was diagnosed with a primary ameloblastoma of the mandible. Surgical resection was then performed, consisting of left hemi disarticulation of the lower jaw, left parotidectomy, and neck lymph node dissection, followed by adjuvant radiotherapy. In September 2016, the woman was admitted again for dyspnea and hemoptysis without any significant weight loss. A chest X-ray revealed round, relatively homogenous opacities bilaterally, which suggested lung metastases. A CT scan of the chest with contrast was performed. The scan revealed lobulated lesions – 3 were located in the right lung (the largest had a diameter of 48 mm) and 1 was located in the left lung (with a diameter of 31 mm). All of lesions were contrast-enhanced. No significantly enlarged lymph nodes were detected. There were no signs of other metastases (Figure 1). To confirm the diagnosis, a fine-needle aspiration (FNA) biopsy was performed and it revealed malignant cytological material that suggested small-cell lung carcinoma (the cells were small, ovoid, and devoid of cytoplasm with large, oval, hyperchromatic nuclei). A subsequent Trucut biopsy revealed small nests of fusiform cells with oval hyperchromatic nuclei with a peripheral palisade. Squamous cell metaplasia was noted in the center of the nests – the findings were consistent with metastases of the previously identified ameloblastoma (Figure 2). Immunohistochemistry revealed the expression of CK5/6 and CK19 with no expression of TTF1. The patient was then evaluated for further chemotherapy with 6 cycles of cisplatin at a dose of 100 mg/m2 on day 1, 5-FU at a dose of 1000 mg/m2/day on day 1–4 (3 wk), and pegylated filgrastim. The patient underwent only two cycles of CT because she developed severe hematological toxicity (Figure 3).
Figure 1.
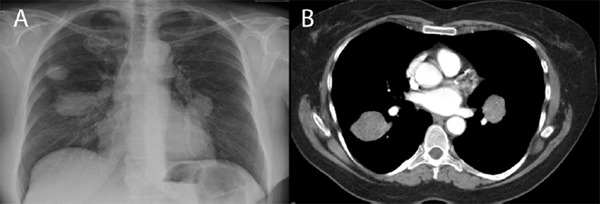
Lung metastases in the current case. (A), X-ray, (B), CT.
Figure 2.
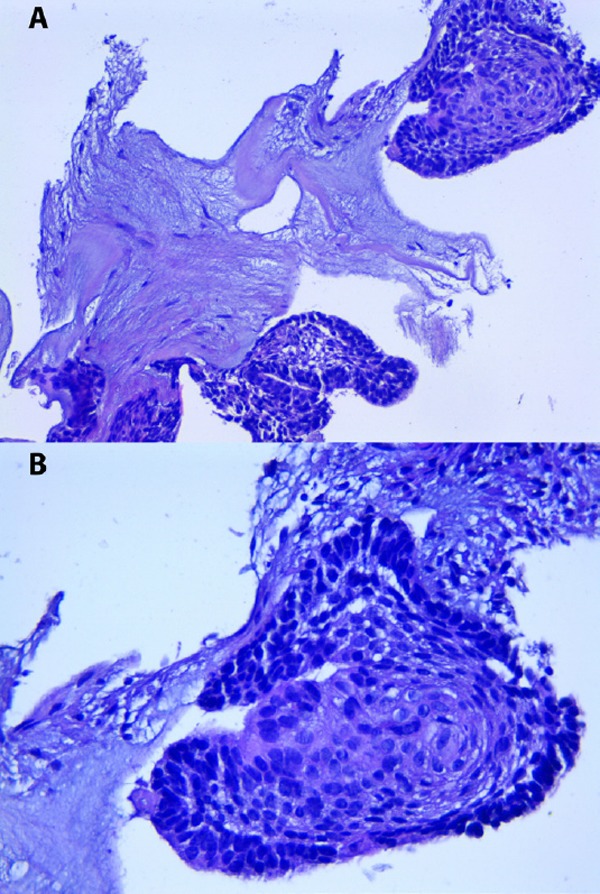
Histological slide confirming the metastasis of ameloblastoma. (A), Magnification 80×; (B), Magnification 160×.
Figure 3.
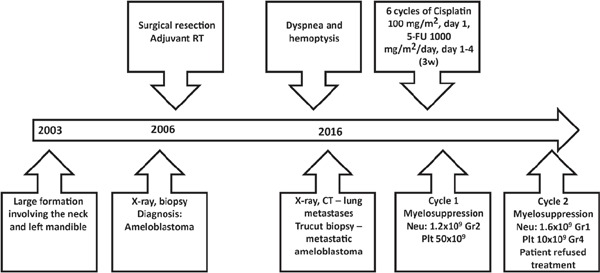
Timeline of the course of disease and the diagnostic and treatment strategy in the current case.
3. Discussion
In 2005, the WHO defined MA as a histologically benign-appearing ameloblastoma that has metastasized. The histological sample from the current case represents the classical form of ameloblastoma as has been described previously (4). Thus, whether metastasis will occur or not is impossible to predict based on histology. Consequently, MA was diagnosed retrospectively. Before ameloblastoma was defined as mentioned earlier, there were no clear diagnostic criteria for the condition. It was defined as a heterogeneous clinico-pathological entity that consists of ameloblastomas with different histological and clinical behaviors – from very aggressive to highly indolent. MA has also been previously reported under different names such as “metastatic ameloblastoma” and “ameloblastoma with metastasis.” Because cytological atypia is not excluded from the early diagnostic criteria for MA, many reported cases may be malignant entities other than MA (5). In contrast, AC is now an entirely different entity, which is characterized by the presence of cellular atypia. Ameloblastoma with cellular atypia is defined as carcinoma, even if metastases are absent. The distinction between these two terms is confusing and a distinction must be made.
Emmura was the first to report MA in 1923, and since then about 100 cases have been reported (6,7). MA represents 1.6–2.2% of all odontogenic tumors (8). There is one report, by Rizzitelli et al. in 2014, on the incidence of MA and its survival rate (9). Unfortunately, that study did not calculate the rate of MA and AC separately; instead, they were calculated as a single percentage. According to the authors, the overall incidence of MA, including both the benign-appearing metastatic form and the cancerous form, is 1.7 per 10 million people. The overall survival rate is 17.6 years – despite being metastatic, the disease has an indolent course. The peak incidence is between the third and fifth decade (9).
The most frequent site for metastases of MA is the lungs, which is where the first metastases manifested in the current patient. The frequency of metastases is estimated to be as high as 75–88% (7).
The disease-free interval in MA is usually quite long – ranging from 2 months to 45 years (mean: 14–18 years) (10) – and that interval was 10 years in the current case. Three mechanisms of tumor metastases are proposed: hematogenic, lymphatic, and via aspiration. Tumor development has been observed in the bronchi and bronchioli (11), which supports the aspiration mechanism. The literature contains no information regarding a predilection for one (right or left) or both lungs.
The immunohistochemical profile of ameloblastoma usually resembles that of normal odontogenic tissue. A number of cytokeratin (CK) subtypes are expressed, namely CK5, CK6, and CK19. In the current case, immunohistochemistry yielded similar results. CK13 and CK14 are found to be expressed in ameloblastoma (7,8,12). Thyroid transcription factor-1 (TTF-1) is a marker used to distinguish a primary lung adenocarcinoma from a lung metastasis. This is due to the fact that it is expressed only in lung adenocarcinoma and thyroid carcinoma. However, TTF-1 is not detected with adenocarcinomas arising from other sites (13). Thus, the tumor in the current patient was metastatic and of ameloblastic origin, a conjecture that was confirmed by additional immunohistochemistry.
The treatment for MA still remains controversial. For lung metastases, lung surgery with radical resection remains the main treatment option, and the role of chemotherapy and radiotherapy has yet to be specified. Based on data from case series and small-scale studies, chemotherapy is the treatment of choice when radical resection cannot be achieved. There is no standard chemotherapy regimen that can be recommended for patients with unresectable metastases.
About 50 cases of cytotoxic treatment of MA have been reported, though their outcomes varied (14). Therapy with cyclophosphamide, methotrexate, and 5-FU yielded passable results in a patient with lung metastases that recurred nine years after initial therapy. Gall et al. noted clinical improvement for long periods of time but no objective response (15). Another study noted partial response after 13 cycles of a combination of cisplatin and cyclophosphamide to treat lung metastases (11). Other drugs also had an effect (reducing the tumor size and alleviating symptoms), including vinblastine, bleomycin, paclitaxel, topotecan, and carboplatin (10,15–18). Based on the tumor spread in the current case and the desire for a more aggressive approach, a cisplatin-containing doublet as has been described in other studies (16,19) was chosen. Unfortunately, the current patient was unable to complete a regimen of 4 cycles with cisplatin and 5-FU due to severe myelosuppression, thus hampering adequate treatment and evaluation of its outcomes.
In conclusion, the current case represents the classical course of a rare disease, which in this instance involved the common presentation of MA. This case is a valid incidence of MA based on the typical histology, findings from a lung biopsy, the immunohistochemical profile of the tumor, the typical clinical features, and a history of a previous primary disease. This is important since most reports describing what was thought to be MA have in fact identified it as some other malignant entity instead.
References
- 1. Hariram, Mohammad S, Malkunje LR, Singh N, Das S, Mehta G. Ameloblastoma of the anterior mandible. Natl J Maxillofac Surg. 2014; 5:47-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Masthan KM, Anitha N, Krupaa J, Manikkam S. Ameloblastoma. J Pharm Bioallied Sci. 2015; 7:S167-S170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lee SK, Kim YS. Current concepts and occurrence of epithelial odontogenic tumors: I. Ameloblastoma and adenomatoid odontogenic tumor. Korean J Pathol. 2013; 47:191-202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. McClary AC, West RB, McClary AC, Pollack JR, Fischbein NJ, Holsinger CF, Sunwoo J, Colevas AD, Sirjani D. Ameloblastoma: A clinical review and trends in management. Eur Arch Otorhinolaryngol. 2016; 273:1649-1661. [DOI] [PubMed] [Google Scholar]
- 5. Ciment LM, Ciment AJ. Malignant ameloblastoma metastatic to the lungs 29 years after primary resection: A case report. Chest . 2002; 121:1359-1361. [DOI] [PubMed] [Google Scholar]
- 6. Laughlin EH. Metastasizing ameloblastoma. Cancer . 1989; 64:776-780. [DOI] [PubMed] [Google Scholar]
- 7. Bi R, Shen L, Zhu X, Xu X. Malignant ameloblastoma (metastatic ameloblastoma) in the lung: 3 cases of misdiagnosis as primary lung tumor with a unique growth pattern. Diagn Pathol. 2015; 10:123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Jing W, Xuan M, Lin Y, Wu L, Liu L, Zheng X, Tang W, Qiao J, Tian W. Odontogenic tumours: A retrospective study of 1642 cases in a Chinese population. Int J Oral Maxillofac Surg. 2007; 36:20-25. [DOI] [PubMed] [Google Scholar]
- 9. Rizzitelli A, Smoll NR, Chae MP, Rozen WM, Hunter-Smith DJ. Incidence and overall survival of malignant ameloblastoma. PLoS One. 2015; 10:e0117789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dissanayake RK, Jayasooriya PR, Siriwardena DJ, Tilakaratne WM. Review of metastasizing (malignant) ameloblastoma (METAM): Pattern of metastasis and treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011; 111:734-741. [DOI] [PubMed] [Google Scholar]
- 11. Henderson JM, Sonnet JR, Schlesinger C, Ord RA. Pulmonary metastasis of ameloblastoma: Case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999; 88:170-176. [DOI] [PubMed] [Google Scholar]
- 12. Hunter KD, Speight PM. The diagnostic usefulness of immunohistochemistry for odontogenic lesions. Head Neck Pathol. 2014; 8:392-399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Srodon M, Westra WH. Immunohistochemical staining for thyroid transcription factor-1: A helpful aid in discerning primary site of tumor origin in patients with brain metastases. Hum Pathol. 2002; 33:642-645. [DOI] [PubMed] [Google Scholar]
- 14. Amzerin M, Fadoukhair Z, Belbaraka R, Iraqui M, Boutayeb S, M'Rabti H, Kebdani T, Hassouni K, Benjaafar N, El Gueddari BK, Errihani H. Metastatic ameloblastoma responding to combination chemotherapy: Case report and review of the literature. J Med Case Rep. 2011; 5:491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gall JA, Sartiano GP, Shreiner DP. Ameloblastoma of the mandible with pulmonary metastasis. Oncology . 1975; 32:118-126. [DOI] [PubMed] [Google Scholar]
- 16. Van Dam SD, Unni KK, Keller EE. Metastasizing (malignant) ameloblastoma: Review of a unique histopathologic entity and report of Mayo Clinic experience. J Oral Maxillofac Surg. 2010; 68:2962-2974. [DOI] [PubMed] [Google Scholar]
- 17. Grunwald V, Le Blanc S, Karstens JH, Weihkopf T, Kuske M, Ganser A, Schoffski P. Metastatic malignant ameloblastoma responding to chemotherapy with paclitaxel and carboplatin. Ann Oncol. 2001; 12:1489-1491. [DOI] [PubMed] [Google Scholar]
- 18. Ramadas K, Jose CC, Subhashini J, Chandi SM, Viswanathan FR. Pulmonary metastases from ameloblastoma of the mandible treated with cisplatin, adriamycin, and cyclophosphamide. Cancer . 1990; 66:1475-1479. [DOI] [PubMed] [Google Scholar]
- 19. Amzerin M, Fadoukhair Z, Belbaraka R, Iraqui M, Boutayeb S, M'Rabti H, Kebdani T, Hassouni K, Benjaafar N, El Gueddari BK, Errihani H. Metastatic ameloblastoma responding to combination chemotherapy: Case report and review of the literature. J Med Case Rep. 2011; 5:491. [DOI] [PMC free article] [PubMed] [Google Scholar]


