Summary
A young adult man with 4-years history of lepromatous leprosy (received irregularly multidrug therapy) presented with two and half years history of symptoms suggestive of chronic erythema nodosum leprosum (ENL), initially responded to steroids and thalidomide, but later on failed. During the last 2-months, he developed fever, vomiting, and subsequently altered sensorium. On evaluation, he had hepatosplenomegaly, hyponatremia, hyperferritinemia, hemophagocytosis in bone marrow aspiration, lobular panniculitis in skin biopsy, and multiple parenchymal nodules in chest imaging. Hence diagnosis of ENL with hemophagocytic lymphohistiocytic (HLH) syndrome was established and treatment with dexamethasone (10 mg/m2) started. During hospitalization, he developed sinus bradycardia, QT prolongations, recurrent ventricular tachycardia, and moderate systolic dysfunction. The cardiac complications recovered using a temporary pacemaker and were presumed to be due to micronodular cardiac deposition of ENL. This case iterates that ENL can present with varied presentations like asymptomatic lung nodules and storming cardiac complications. More importantly leprosy, ENL, and HLH are a continuum of manifestations of the same agent-host interactions.
Keywords: Cardiac arrhythmia, hemophagocytic lymphohistiocytic syndrome, lepromatous leprosy, pulmonary nodule, type 2 lepra reaction
1. Introduction
In the era of leprosy elimination, a greater concern is the lepra reaction [erythema nodosum leprosum (ENL, type 2 reaction), reversal reaction (type 1 reaction), or Lucio's phenomena. It represents an acute episode that interrupts slow, insidious, and chronic evolution of leprosy. The ENL, characterized by painful erythematous nodulations that grows in apparently normal skin, is seen mainly in the lepromatous type of leprosy patients (1). Although there is a consensus of decreasing cases of ENL after the inclusion of clofazimine containing multidrug therapy (MDT), however, the greatest concerns are associated with systemic manifestations, morbidity, and mortality (2).
Hereby, we report a typical case of chronic ENL presenting with hemophagocytic syndrome, cardiac dysfunction, and asymptomatic lung nodules.
2. Case Report
A 26-year-old man was diagnosed as a case of Hansen's disease (multibacillary type as per slit smear) in February 2013. After continuous 6-months of treatment (MDT - rifampicin, clofazimine, and dapsone), he discontinued the treatment of his own when symptoms resolved. In October 2014, he developed multiple skin nodules over the body, fever, and joint pain. He was diagnosed as ENL and treated with prednisolone and restarted with MDT. During the tapering of steroids, he again developed similar symptoms and thalidomide was added and later on prednisolone was stopped. Symptoms improved. He also received MDT again, continued for 12-months. In April 2016, during the tapering of thalidomide, he again developed ENL symptoms; the dose of thalidomide was increased but symptoms didn't improve; and prednisolone was restarted along with MDT. But symptoms didn't improve and further worsened.
In September 2016, he presented to our hospital with above ENL symptoms. Along with these symptoms he had upper abdominal pain, vomiting, decreased oral intake, and leg swelling for 2-months and altered sensorium for 3-days.
On examination, he was drowsy and pale, and had pedal edema. Hemodynamically he was stable. Spleen and liver were enlarged. There was swelling and tenderness over both ankles and knees with multiple red nodular skin lesions over both shins. Other systemic examinations were unremarkable except for drowsiness. On day of presentation, his sensorium worsened without any focal neurological deficits and he developed respiratory distress. Mechanical ventilation was started and emergency investigations showed hyponatremia (Na+ 125 meq/L). After correcting sodium imbalance, his sensorium improved and he was extubated early. The hyponatremia was considered due to either long standing vomiting after use of multiple drugs (steroids, thalidomide, and MDT) or a part of the disease process. All previous ongoing drugs were stopped temporarily except steroids.
Routine hemogram showed Hb, 5.7mg/dL; WBC, 16.5×109/L; platelet count, 136×109/L; and ESR, 72mm/hr. Test for malaria, dengue, chikungunya, hepatitis B and C, and HIV were negative. CSF examination was also unremarkable. Routine cultures were sterile. Autoimmune tests including RA factor and ANA were negative. CECT chest and abdomen was performed that showed hepatosplenomegaly with multiple hypodense lesions in the liver and spleen, and multiple lung nodules (Figure 1) suggesting a possible disseminated fungal infection or ENL. Furthermore, bronchoalveolar lavage was performed that was negative for bacterial and fungal infections including a galactomannan study. However, antibacterials (cefoperazone and levofloxacin) and antifungal treatment (voriconazole) were started for possible superadded bacterial/fungal infections because of his prolonged immunosuppressed state, but symptoms didn't improve. Serum ferritin was high (2,000 ng/dL). Hence, secondary hemophagocytic lymphohistiocytosis (HLH) syndrome was suspected considering fever and hepatosplenomegaly. Bone marrow (BM) examination confirmed hemophagocytosis (Figures 2A and 2B). His serum triglyceride level was 98 mg/dL. NK cell activity was not done. HScore, an online software to determine the probability of the syndrome, was calculated, and found to be 194 (probability of HLH, 84%). Since both ENL and HLH as inflammatory conditions require steroids, he was started on injection dexamethasone (10 mg/m2) and his symptoms dramatically responded in few days. To know the primary cause of HLH, USG guided fine needle aspiration cytology of the liver was performed, which showed inconclusive results (repetition could not be performed because of major cardiac issues as described below). Skin biopsy of the nodular lesions was performed suggesting a lobular panniculitis and features were compatible with ENL with negative Fite stained bacilli (Figures 2C and 2D). A slit smear also was negative. Thalidomide (100 mg OD) was continued. Considering viable lepra persisters as triggers for both inflammatory conditions, especially HLH, he was restarted with MDT intensively with dapsone (100 mg OD) and rifampicin (600 mg monthly).
Figure 1.
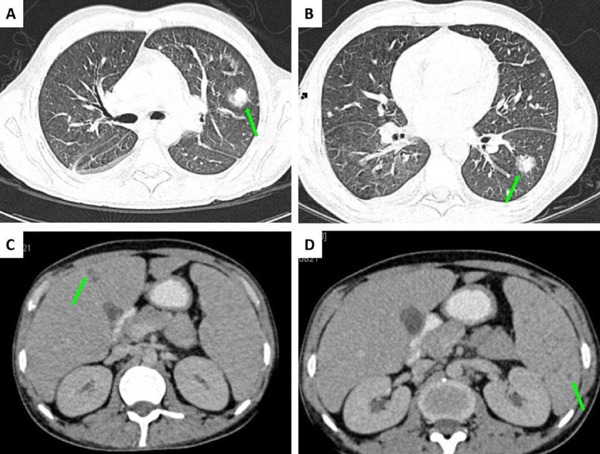
Contrast-enhanced computed tomography of chest and abdomen. Axial images of lung windows (A/B) revealing multiple parenchymal nodules (arrows) in both lungs without any cavitation and of abdomen (C/D) showing focal hepatic and splenic hypodense lesions (arrows).
Figure 2.
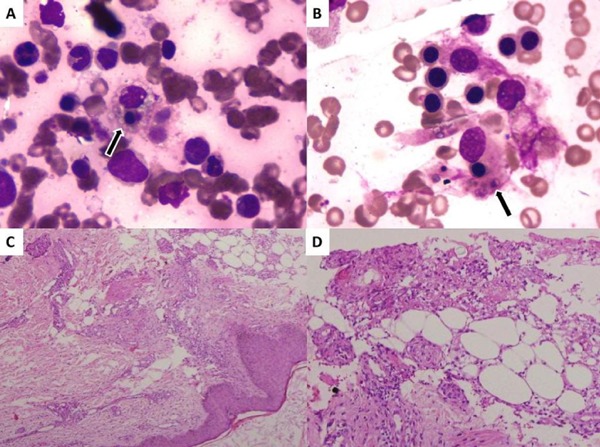
Photomicrographs of Bone marrow aspiration and Skin biopsy. Giemsa Stain of Bone marrow aspiration (A ×1,000, B ×1,000) showing multiple histiocytes with erythro-phagocytosis. Hematoxylin and Eosin stain of Subcutis (C ×100, D ×400) showing septal thickening, fibrosis, and inflammation comprised of lymphocytes, neutrophils, and histiocytes with spill over into the fat lobules, suggesting lobular panniculitis, possibly ENL. Modified Fite stain was negative.
However, during the hospital course, there were continuous brainstorming cardiac events that needed detailed description. Before biopsy results were obtained, one early morning, he developed retrosternal chest pain, typical of angina, with hypotension (BP, 80/60 mm/Hg). ECG showed anteroseptal deep T wave inversions with sinus bradycardia, inverted P waves, and QT prolongations (QTc, 516 ms), suggesting right ventricular myocardial infarction (Figure 3A), confirmed by screening 2D-Echo. He was given IV fluids and dual antiplatelets. Although symptoms improved except for persistent bradycardia and QT prolongation, in a few hours, he developed ventricular tachycardia (VT). He received defibrillation and VT resolved. Suspecting drug related arrhythmia, voriconazole and levofloxacin were stopped. However, again VT recurred and a temporary pacemaker was inserted and cardiac rhythm stabilized (Figure 3B). There were no electrolyte disturbances. Routine 2D-Echo showed moderate systolic dysfunction (EF-40%). After 3-weeks as the patient improved, the pacemaker was removed, however, sinus bradycardia was persistent with resolving T wave inversion (Figure 3C). To determine the local cause of these cardiac problems, cardiac-MRI was performed, which was normal, although it could not preclude small ENL granuloma causing these cardiac abnormalities, since the patient had already received high dose steroids for more than 3-weeks. Antiplatelets were stopped. The patient was discharged in hemodynamically stable condition with MDT, thalidomide, and a tapering steroid dose as per HLH protocol. Finally he was diagnosed as a case of chronic ENL with HLH syndrome and cardiopulmonary involvement.
Figure 3.
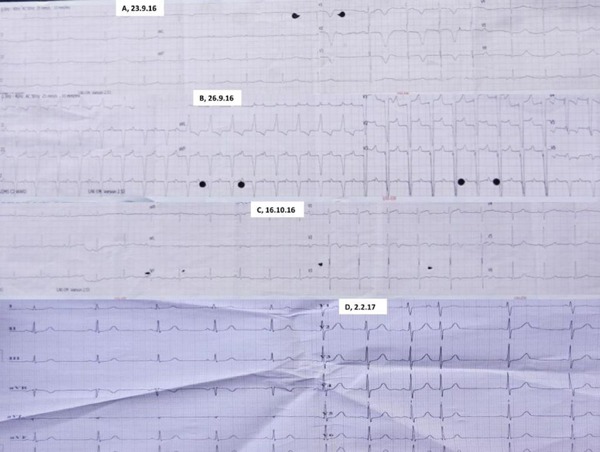
Electrocardiographs (ECG). On first day of cardiac problem, ECG (A) showing sinus bradycardia (HR, 55), inverted P waves (inferior leads), deep T wave inversions (anteroseptal leads), and prolonged QT intervals (QTc, 516 ms). Post-pacemaker ECG (B) showing persistence of prolongation of QT intervals. However, one month later after removal of pacemaker, ECG (C) showing normalization of QT interval but persistent sinus bradycardia. On recent follow up, ECG (D) showing persistent sinus bradycardia with variable block.
In a recent follow up, he was completely symptom free and ECG showed persistent sinus bradycardia with a variable block (Figure 3D). Repeat CT-chest and abdomen revealed disappearance of nodules in lungs, liver, and spleen. Treatment plan is to continue intensive MDT [rifampicin for 5-years, dapsone for life (to inhibit viable persisters)] and thalidomide for 6-months at least.
3. Discussion
Type 2 lepra reaction i.e. ENL is an immune-complex mediated disease. It is usually precipitated by lepromatous leprosy or borderline lepromatous disease with high bacterial load, pregnancy, lactation, puberty, intercurrent infection, vaccination, stress and use of interferon-gamma; however, sometimes it occurs spontaneously similar to our case (3).
ENL can affect any part of the body unpredictably during any time in the course of leprosy. Only active vigilance in society can help in detection of various manifestations of it. Hematological involvement in it are mainly chronic disease anemia, hemolytic anemia, leukocytosis, hyperfibrinogenemia, and sometimes a prothrombotic state (4). HLH is a very rare manifestation. There are only two reported cases of HLH in ENL with the simultaneous presence of multibacili leprosy (5–6). Furthermore, lepra bacilli is a known trigger for HLH even without ENL. Even isolated hemophagocytosis have been reported without HLH syndrome in leprosy (3). Our case represents the first described HLH case in association with ENL without evident lepra bacilli.
Triggers for HLH in our case are yet to be answered. As we know lepra bacilli can be dormant for lifelong as viable persisters. At any point in time under a favorable environment (e.g. stoppage of MDT treatment), the bacilli or their antigens can act as a trigger for an inflammatory state like ENL or HLH or both in a continuum like our case. In this regard, our case represents a possibility of leprosy, ENL, and HLH as progressive stages of manifestations based on host-antigen interactions. To make matters more intriguing, ENL presents with a similar clinical picture of dapsone hypersensitivity syndrome. In such a scenario, BM evaluation can be of great help to differentiate these entities. In our case, skin biopsy suggested ENL and BM revealed HLH. HSscore, often used for diagnosing HLH syndrome (http://saintantoine.aphp.fr/score), was higher suggesting an 84% chance of the possibility though we could not perform all diagnosed criteria (e.g. NK cell activity, soluble CD25) of the HLH-2004 protocol because of technical constraints.
Cardiac involvement has not been reported in ENL but is a known complication of leprosy, especially lepromatous type (8).
The cardiac conduction system is mainly affected in leprosy in the form of variable heart rate, ST and T wave changes, bundle branch block, extrasystoles, and prolongation of QT interval (9). Sudden cardiac death has also been reported. In our case, there is a possibility of granulomatous/nodular deposition in the cardiac tissue resulting in various rhythm disturbances and structural dysfunction. This possibility is considered after: ruling out HLH as a cause of cardiac problems since myocarditis is the usual manifestation and conduction abnormality has not been reported yet in this condition; and ruling out drug induced QT prolongation (voriconazole and levofloxacin) since after stopping the drugs it was not seen and structural dysfunction was not seen either.
Respiratory involvement has been described scarcely in ENL in contrast to frequent nasal and laryngeal involvement in leprosy patients. Only three cases of ENL in a radiological survey in 1976 have been reported to have lung parenchymal nodules that disappear subsequently with time (10). These are thought to be an allergic reaction to lepra antigen similar to a generalized immunological reaction. Our case describes a nodular lung involvement, possibly due to granuloma of ENL similar to their presence in the liver and spleen. This is another uniqueness to our case, however, a biopsy could not be done because of underlying cardiac issues. Interestingly, all nodules disappeared after treatment as was evident on a recent CT-scan.
In conclusion, the present case represents few rare manifestations of ENL including HLH, storming cardiac complication, and asymptomatic lung nodules. Furthermore, one should understand that leprosy, ENL, and HLH are a continuum of manifestation of the same agent-host interactions seen in the course of the illness. Hence, one should take precautions in withdrawing MDT and immunosuppressants in chronic/recurrent ENL patients.
References
- 1. Rea TH, Levan NE. Erythema nodosum leprosum in a general hospital. Arch Dermatol. 1975; 111:1575-1580. [PubMed] [Google Scholar]
- 2. Pocaterra L, Jain S, Reddy R, Muzaffarullah S, Torres O, Suneetha S, Lockwood DN. Clinical course of erythema leprosum: An 11-year cohort study in Hyderabad, India. Am J Trop Med Hyg. 2006; 74:868-879. [PubMed] [Google Scholar]
- 3. Kahawita IP, Walker SL, Lockwood DNJ. Leprosy type 1 reactions and erythema nodosum leprosum. An Bras Dermatol. 2008; 83:75-82. [Google Scholar]
- 4. Freitas TCD, Fleury RN. Hematologic profile of leprosy patients in reactional episode of erythema nodosum leprosum. Hansen Int. 1996; 21:58-66. [Google Scholar]
- 5. Desenfants A, Huguon E, Polfrit Y, Crouzat M, Rouleau V, Chassot V, Besson-Leaud L, Missotte I. Leprosy with an unusual course. Arch Pediatr. 2012; 19:1182-1186. (in French) [DOI] [PubMed] [Google Scholar]
- 6. Høyvoll LR, Fløisand Y, Orrem HL, Gunnarsson R, Landrø L, Brevig T, Gaustad P, Nordøy I. Hemophagocytic lymphohistiocytosis in leprosy. Lepr Rev. 2015; 86:403-406. [PubMed] [Google Scholar]
- 7. Zeng XZ, Wang YN, Wang JS, Wu L, Zhang J, Wei Q, Liu J, Wang Z. A case of lepromatous leprosy complicated by hemophagocytosis misdiagnosed as hemophagocytic lymphohistiocytosis. Int J Infect Dis. 2014; 23:28-30. [DOI] [PubMed] [Google Scholar]
- 8. Katoch K, Ramu G. Cardiovascular involvement in leprosy patients. Nihon Rai Gakkai Zasshi. 1983; 52:73-81. [DOI] [PubMed] [Google Scholar]
- 9. Goyal T, Varshney A, Bakshi SK, Sharma V. Lymph node abscess and cardiac involvement in a patient with nodular lepromatous leprosy (LL) with erythema nodosum leprosum (ENL): A rare occurrence. Lepr Rev. 2015; 86:112-116. [PubMed] [Google Scholar]
- 10. Kaur S, Malik SK, Kumar B, Singh MP, Chakravarty RN. Respiratory system involvement in leprosy. Int J Lepr Other Mycobact Dis. 1979; 47:18-25. [PubMed] [Google Scholar]


