Abstract
Benign paroxysmal positional vertigo (BPPV) (otolith disease) is the most common neurological and position change related vertigo, accounting for 17–20% of peripheral vertigo. BPPV occur in the elderly. The high incidence age for BPPC was 50 to 70 years and mostly in female. According to the different parts of the lesions, it is divided into anterior canal BPPV (AC-BPPV), posterior canal BPPV (PC-BPPV), horizontal canal BPPV (HC-BPPV). Studies have shown that the incidence of PC-BPPV was 86.36%, the incidence of HC-BPPV was 11.37%, the incidence rate of AC-BPPV was 2.27%. Treatment for PC-BPPV includes manual reduction, drug treatment, psychological treatment, and surgical treatment. Repositioning is the preferred method for the treatment of PC-BPPV with high effective rate and low risk. The mechanism is through the different changes of head position to make the otolith back to utricle. Many manual reduction methods have been reported in clinical treatment of PC-BPPV. With the increasing emphasis on the BPPV, a variety of new methods are being developed and designed.
Keywords: benign paroxysmal positional vertigo, repositioning, utricle, peripheral vertigo, otolith disease
1. Introduction
Benign paroxysmal positional vertigo (BPPV) is a vertigo syndrome occurring due to postural changes and is characterized by nystagmus. BPPV was first described as vertigo caused by changes in the position of the head (1). Barany, the founder of Hungarian ear neurology, reported a female patient, aged 27 years, with vertigo which was associated with changes in the position of the head. Her vertigo tended to occur during the processes of getting up, lying down, and turning over, with transient symptoms lasting <1 min, and was repeatable. These symptoms were attributed to the otolithic membrane (2). Dix and Hallpike first proposed this diagnosis (3) after summarizing a large number of diseases with the same symptoms and finding a certain incubation period (mostly <1 min) prior to symptom onset. They also noted that the side with the ear facing downward was the affected side when vertigo occurred, that nystagmus was transient, rotary, geotropic, and apogeotropic, that nystagmus was induced again when the head rotated to its original position despite the movement being in the opposite direction (reversibility), and that nystagmus was attenuated (fatigue) after repeated position change stimulations. In 1985, McClure first reported seven BPPV patients with horizontal nystagmus induced by changing positions (4). Baloh et al (1993) (5) and Lempert (1994) (6) described the clinical characteristics of horizontal canal BPPV (HC-BPPV), and found that the inducing position and type of nystagmus for HC-BPPV were different than that of the previously reported posterior canal BPPV (PC-BPPV). Nystagmus was induced horizontally rather than via the previously reported rotary or apogeotropic motions, and corresponding reduction treatments were used (7). In 1994, Brandt first reported the clinical manifestation of PC-BPPV. Three years later, Herdman (8) found that some patients may experience vertigo and nystagmus when the position of head was changed, but the characteristics of nystagmus were different from previously reported cases: the nystagmus was induced by vertical, geotropic, and rotary movements, indicating that this was a new type of positional vertigo.
2. BPPV diagnosis
Otolith disease in the posterior semicircular canal typically occurs during the process of getting up or lying down (9). In 1952, Dix and Hallpike summarized the characteristics of vertigo and nystagmus in patients with PC-BPPV and developed the Dix-Hallpike test (3) (also named the Nylen-Barany test): i) the patient sits on the bed and rotates the head 45°, ii) the examiner asks the patient to change from sitting to supine position, with the head drooping to 30°, during which the presence of nystagmus was examined. If vertigo and nystagmus occurred after the transient incubation period, the patient was considered positive. iii) The patient is asked to return to sitting position, and vertigo and nystagmus occurred again during this process, with the nystagmus in the opposite direction and iv) the head is rotated to the other side and steps 1–3 are repeated. The degree of vertigo and the type and intensity of nystagmus was compared to determine whether the condition was PC-BPPV or anterior canal BPPV (AC-BPPV), and to identify the affected side. When significant vertigo and apogeotropic, rotary, and geotropic nystagmus occurred after a head 45° rotation to the right, the condition was considered right PC-BPPV, and when symptoms occurred after a 45° rotation to the left, the condition was considered left PC-BPPV. When significant vertigo and geotropic, rotary, and geotropic nystagmus occurred after the head rotated to both sides, the condition was considered bilateral PC-BPPV. Bo et al showed that when the patients with PC-BPPV underwent the Dix-Hallpike test, nystagmus was found in the direction of the affected side when the head was hanging in the supine position and in the direction of the healthy side when the patient was in sitting position; this phenomenon was noted as the interconvertibility of nystagmus (10). For patients with cervical spondylosis or cervical injury, the neck should not be stretched for too long, rendering the Dix-Hallpike test inappropriate. In such cases, the side-lying test, designed by Cohen (11), could be used. i) The patient sits on the bed with the head rotated to the non-testing side at a 45° angle. ii) While maintaining head position, the patient lies on the side to be tested, with the tested-side shoulder on the bed. Presence of vertigo and nystagmus were observed. iii) While maintaining head position, the patient then returns to a sitting position while indications of vertigo and nystagmus were observed in order to diagnose PC-BPPV and SC-BPPV. Xie also designed a test for limited cervical spine motion called the modified lateral decubitus position test (12). In this test, i) the subject wears cervical gear and sits in the middle of the bed with maintained head and neck position, ii) the body is then rotated to the left at a 45° angle while maintaining head position, and the patient is laid on the right side rapidly for right posterior semicircular canal examination and iii) after returing to a sitting position and resting for 1 min, the procedure is repeated for investigation of the left posterior semicircular canal.
Otolith disorders in the horizontal semicircular canal were usually induced by head rotation and turning over on the bed. The most commonly used diagnosis was the supine roll test (also called the Pagnini-McClure maneuver), which is the gold standard for the diagnosis of HC-BPPV (13). The procedure is as follows: i) the patient is placed in a sitting position, ii) the patient moves rapidly from a sitting to supine position, iii) the head is rotated 90° to one side and nystagmus in both eyes is examined and iv) the head is rotated 90° to the other side and the presence of vertigo and nystagmus are examined. This method could induce two forms of nystagmus representing different types of HC-BPPV (14): when the head was rotated 90° to the right and significant vertigo occurred/horizontal and geotropic nystagmus was induced, this was diagnosed as right horizontal canal otolith disorder. Otherwise, the condition was diagnosed as left horizontal canal otolith disorder. The etiology of both disorders is that the semicircular canal was affected. However, if the etiology was a lesion in the cupula cristae ampullaris, horizontal and apogeotropic nystagmus would be present, and the affected side was the side where no significant nystagmus occurred. This procedure should be prohibited for patients having short necks with poor mobility, morbid obesity, and severe kyphosis (15). Mei developed a modified supine roll test for these patients (16) with the following procedure: with the patient in supine position, the head was blocked up at an angle of 30°. All other steps were identical to the conventional supine roll test (16). Xie diagnosed patients with poor mobility using a modified supine positioning test (12): the patient wore a cervical and the head and neck positions were maintained. Both the head and the body were rotated 90° to one side, any occurrence of vertigo and nystagmus were determined, and the patient was returned to the sitting position. After 2 min, both the head and body were rotated 90° to the other side and any occurrence of vertigo and horizontal nystagmus were determined. The affected semicircular canal was determined based on the occurrence and type of nystagmus.
Apart from the commonly used supine roll test for HC-BPPV, Rahko and Kotti reported a walk-rotate-walk test (17), where the patient is rotated 180° with the heel serving as the axis during fast walking, then returned to the original position at the same speed. This cycle was repeated three times without any pause. Astasia, manual balance correction, and the need for pauses were observed during fast rotation. HC-BPPV could be diagnosed when these actions were observed repeatedly, and the side to which the patient rotated to was considered the affected side. Nuti et al used the head yaw test to diagnose HC-BPPV. The patient started in a supine position and rapidly rotated their head 90° to the side of the tested ear. As the rapid downward movement leads to nystagmus, called geotropic nystagmus, conversely, called apogeotropic nystagmus, Nuti et al developed the seated supine positioning test (18), where the patients head was held at 30° while the patient changed from sitting to supine position, potentially inducing seated supine positioning nystagmus. HC-BPPV patients with geotropic nystagmus rotated to the healthy side, while the HC-BPPV patients with apogeotropic nystagmus rotated to the affected side. Choung et al developed the bow and lean test to diagnose HC-BPPV (19): i) the HC-BPPV was bile duct stone HC-BPPV or crest stone HC-BPPV, ii) the patient is in a sitting position and bows their head greater than 45°, and the direction of nystagmus was observed (specific for bile duct stone HC-BPPV) and iii) the patient then throws their head back greater than 45° and the direction of nystagmus was observed (specific for crest stone HC-BPPV). When patients with bile duct stone HC-BPPV bowed their heads, nystagmus was induced in the direction of the affected semicircular canal. When patients with crest stone HC-BPPV threw their heads back, nystagmus was induced in the direction of the affected semicircular canal.
AC-BPPV was mainly induced during the process of getting up and lying down, and the diagnosis method was the same as with PC-BPPV. If vertigo and geotropic nystagmus occurred during the position-induced test, the diagnosis was AC-BPPV. If apogeotropic nystagmus occurred, it was contralateral AC-BPPV, and if geotropic nystagmus occurred, it was homolateral AC-BPPV. In addition, Rahko developed another diagnosis method for AC-BPPV (20): the patient, standing upright, closes their eyes and stoops down to a 60° angle, then rapidly stands upright again. If the patient toppled over to any side, they would be diagnosed with AC-BPPV. The shortcoming of these two methods was the presence of false positive diagnoses. Meng reported that the self-made SRM-IV system was sensitive to AC-BPPV, and speculated that the actual morbidity of AC-BPPV was much higher than presented in previous statistics due to missed diagnoses in conventional detection (21).
Recently, examination of vestibular function has been extensively applied for the diagnosis of BPPV. For example, the vestibular autorotation test can determine the function of both horizontal and vertical semicircular canals (22). Imaging has also been increasingly applied in the diagnosis of BPPV. Li reported that positive cranial MRI in BPPV patients showed affected semicircular canal and ear bones, as well as otolith detachment (23). Heavily T2-weighted magnetic resonance imaging of the inner ear can clearly demonstrate the internal acoustical meatus structure and allow full observation of the inner ear (24). Yan performed heavily T2-weighted magnetic resonance imaging of the ossa temporale in 48 BPPV patients and found that magnetic resonance imaging of the inner ear could provide imaging evidence for the diagnosis of BPPV (25).
3. Manual reduction of BPPV
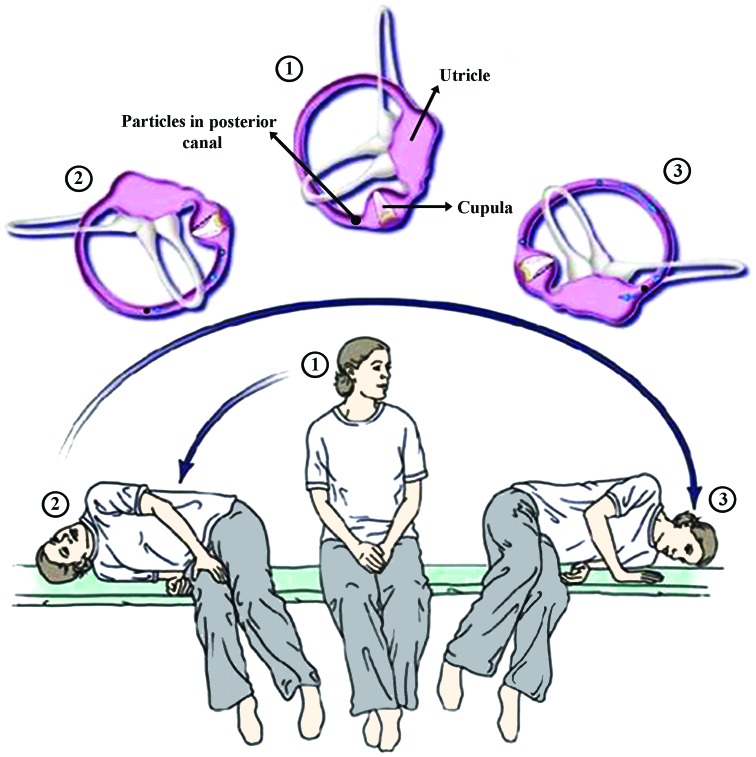
In 1980, Brandt and Daroff developed an exercise for the treatment of otolith disease (26): the patient starts in a sitting position, changes rapidly to a right supine position with the head rotated at a 45° angle to the left. Thirty seconds following the resolution of the resultant vertigo, the patient would sit rapidly and stare forward for another 30 sec, then change rapidly to a left supine position with the head rotated at a 45° angle to the right. This would be repeated 20 times, twice daily, 1–2 times per week, and could be gradually stopped after symptom remission. In 1988, Semont et al developed the modified liberatory maneuver based on the theory of crest otolith (27). The clinical significance of the modified liberatory maneuver was that only a single positioning exercise was required to achieve a cure. The procedure is as follows: i) the patient, in a sitting position, rotates their head to the healthy side at 45°, ii) the patient then switches rapidly to a lateral supine position while maintaining the position of their head, iii) the patient then switches from the affected side to the healthy side while again maintaining head direction (the apex nasi contacts the bed) and iv) the patient recovers to a sitting position with the head tilted forward at 20°. Nystagmus was evaluated after each procedure, and the subsequent procedure was performed 1 min after resolution of nystagmus (Fig. 1). van der Scheer-Horst et al performed a retrospective review of the effectiveness of Brandt-Daroff vestibular rehabilitation and manual reduction, and found that the onset of manual reduction was earlier than vestibular rehabilitation, yet the combination of vestibular rehabilitation and manual reduction was beneficial for the recovery of patients (28). Patients with limited cervical spine motion could use the modified Semont procedure (29): i) the patient wears a cervical gear while sitting on the front of the bed, then while maintaining head and neck position, rotates the body 45° to the left in order to treat the right posterior semicircular canal, ii) the patient changes rapidly to a right supine position (the same with the modified lateral supine position), the back of the head contacts the bed, and the apex nasi faces upward, iii) after resolution of vertigo and nystagmus, the patient changes from a right supine to a left supine position with the rear arm as the pivot point, the forehead and apex nasi contacting the bed, and the back of the head facing upward and iv) the patient sits up. The treatment for the left posterior semicircular canal was the same as that for the right posterior semicircular canal, except for reversed directions.
Figure 1.
Evaluation of nystagmus after each procedure. The subsequent procedure was performed 1 min after resolution of nystagmus.
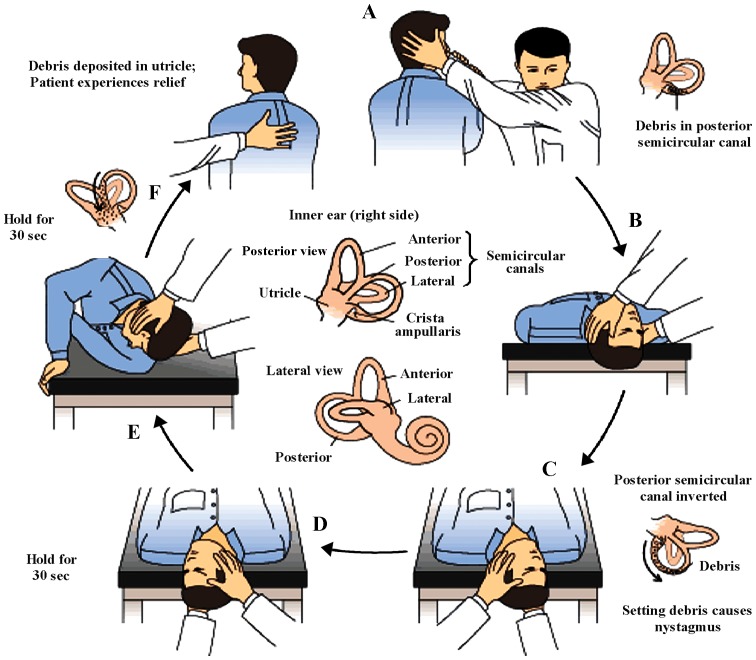
The most classical treatment for PC-BPPV is the Epley reduction, which was developed by Epley based on the hypothesis of otolith in the semicircular canal (30): i) the patient starts in a sitting position with their head tilted to the affected side at a 45° angle, ii) the patient changes from a sitting to a supine position with the head beneath the bed at an angle of 45°, iii) while maintaining the positioning of the body, the head was then rotated to the healthy side at a 45° angle, iv) both the body and the head then rotated to the healthy side at 90° angles, v) the body was then shifted to a supine position towards the healthy side, with an angle of 135° between the head and the bed and vi) the patient then sat and tilted their head forward at a 20° angle. Each position was maintained for 1 min. Rotation was stopped upon vertigo and continued 30 sec after resolution of nystagmus (Fig. 2). Epleys therapy was highly effective: success rates were found to be 90.7% after one conductance of an Epley reduction and 96.0% after two conductances. However, this therapy was not appropriate for patients with limited cervical spine motion, who could use the Semont procedure (31). Anagnostou et al treated 51 PC-BPPV patients each with the Epley procedure or the Semont procedure and found that the successful reduction rate was not significantly different between these two therapies: 7.8% of patients had HC-BPPV after treatment by the Epley procedure, while no patient had HC-BPPV after treatment by the Semon procedure (32). Yang demonstrated a modified 3-step procedure which was not limited to a specific treatment platform and could be performed on regular bed if a hard and 15-cm high pillow was put on the bed (33). This procedure was very convenient for clinical treatment. The reduction could be performed as three steps: i) the patient, in a sitting position and head rotated to the affected side at a 45° angle, lies down rapidly to create shoulder contact with the pillow while the head remains above the pillow facing downward at an angle of 30°, ii) the patient then rotates their head to the healthy side and rotates over into the prone position, then tilts their head back at an angle of 30° and iii) the patient reverts to sitting position with the head tilted forward at an angle of 30°.
Figure 2.
Procedures of Epley reduction for treatment of PC-BPPV. PC-BPPV, posterior canal benign paroxysmal positional vertigo.
In 1990, Baloh et al (34) and Lempert (6) reported that most commonly used treatment for HC-BPPV reduction was the barbecue roll maneuver, which aimed to remove the otolith from the horizontal semicircular canal (6). i) The patient starts in the supine position with the head rotated 90° to the healthy side, ii) the body then rotates 180°, moving the patient from the supine to the prone position without changing the position of the head, iii) the head maintains its 90° rotation while the apex nasi faces downward, iv) with the head still aligned at 90° towards the healthy side, the lateral face contacts the bed and v) the patient sits up again (35). The mean effective rate of BRM for HC-BPPV was 75%, with a reported range of 50–100% (36). BRM was more suitable for otolith disease or a crest otolith adhering to the cupula canal-side (CUP-C), and ineffective for a crest otolith adhering to the cupulautricle side (CUP-U) (37). Patients with obesity, cervical spondylosis, and muscle disease could not tolerate BRM due to limited positioning (38). In 1998, Gufoni et al developed a new treatment for HC-BPPV to complement BRM (39): i) the patient moves from a sitting to a lateral supine position (from CUP-C to the healthy side, from CUP-U to the affected side) while keeping the position of the head forward, ii) the head is rotated 45° to the healthy side without altering the position of the body and iii) the patient resumes a sitting position with the head position unchanged. Each position was maintained for 3 min.
The Gufoni procedure is convenient and highly effective, as well as suitable for all types of HC-BPPV (including otolith disease and crest otolith) (39). As vertigo symptoms were mild on the tilted side during reduction, the patient could tolerate the treatment). HC-BPPV patients with horizontal apogeotropic nystagmus could perform this step-by-step reduction (40–42), as Gufoni otolith detachment could transform horizontal apogeotropic nystagmus into horizontal geotropic nystagmus, at which point BRM could be performed to achieve good efficacy. Mei used a self-made otolith repositioning procedure to transform horizontal apogeotropic nystagmus into horizontal geotropic nystagmus, and also achieved good efficacy (43). Testa developed a modified Gufoni procedure to modify the turbulent flow in the ampulla during the motion of the semicircular canal so that the otolith materials were far away from crura commune. As a result, HC-BPPV was less likely to be transformed into PC-BPPV, thereby improving the efficacy from the classical Gufoni procedure (44). The Vannucchi-Asprella maneuver was another option for HC-BPPC and more convenient than BRM. However, it was limited by a requirement for successive multiple cycles to achieve good efficacy (38): i) the patient starts in supine position with the head rotated 90° to the healthy side, ii) the patient sits up slowly without changing head position, iii) the head slowly moves to face forward and iv) the patient moves from sitting to supine position. This procedure should be repeated several times. This procedure was considered a modified BRM, as it placed the otolith back into the alveus communis using gravity and angular acceleration (rotation of the head in supine position) through the changing between sitting and supine positions. Vannucchi-forced prolonged positioning is generally used as a complementary therapy for BRM rather than a single therapy. Vannucchi first developed this procedure in 1994 for patients with otolith disease. This procedure required the patient to maintain supine position on the healthy side for at least 12 h so as to ensure the opening of the alveus communis in the horizontal semicircular canal of the affected side was always facing downward, so that the otolith could returned to the alveus communis via gravity. Head rotation in a supine position could also be used to treat this BPPV: with the patient in supine position, the head is rapidly rotated 90° to the healthy side (for patients with otolith disease), then returned to the initial position slowly. The procedure was then repeated. Also, patients with crest otolith should rotate their heads to the affected side (45). The modified Epley procedure could also be used for AC-BPPV: the procedure was similar to the Epley procedure but with a slow frequency of reduction, a pause between each position longer than 1 min, and each maneuver was performed by the patients themselves (46). The Li maneuver was usually used for the treatment of AC-BPPV: i) the patient starts in supine position with head facing 20° downward and legs on both sides of the bed and ii) the patient then sits rapidly, changing from supine to prone position with the face contacting the bed. In 2009, the Yacovino procedure was first reported for the treatment of AC-BPPV (47): i) the patient starts in a sitting position with the head facing forward, ii) the patient rapidly changes to supine position with the head moving upward at a minimum of 20° for 2–3 min, iii) the head is elevated and bent forward for 2–3 min and iv) the patient returns to a sitting position and looks forward horizontally. The healthy or affected sides may not be considered. A previous study suggested that it was difficult to provide maximum stimulation to the affected side, given that it was left undetermined, possibly impacting efficacy (48). Xing suggested that the effective rate of this procedure was consistent with the modified Epley reduction, but the procedure itself was easier to perform (49).
Recently, whether position limitation was required is controversial. Some studies (50–52) and a recent meta-analysis by Mostafa et al (53) showed that the difference between limited motion and free motion after reduction was not significant. Zhang used manual reduction to treat PC-BPPV with good efficacy and no adverse reactions (54). Li used semi-supine positioning and a turning-over exercise to treat elderly BPPV patients; this procedure contained characteristic small motions and ease of operation, making it more acceptable in elderly patients than conventional reductions (55).
With the development of technology, more and more reduction machines have been implemented. The SRM-IV BPPV diagnosis and treatment system (developed in China) provided automatic, precise, quantitative, rapid diagnosis, and reduction for BPPV patients (56,57) with a total efficacy of 97.02% (58), which was superior to conventional manual reduction. This system could also reduce the incidence of vomiting, pale face, and cold sweats during artificial reduction (59). The TRV otolith instrument first appeared at the 111th Annual Meeting of French ENT (60); its efficacy was higher than most manual reductions (61). Xu reported a novel automatic 3D chair to assist manual reduction, but the clinical efficacy of this device requires further observation (62).
4. Other treatments for BPPV
Prior to the application of manual reduction, drugs that improve microcirculation and inhibit the vestibule have been used as first line drugs for BPPV, and have been shown to improve efficacy (63–65). For refractory BPPV patients, manual reduction alone could not achieve good efficacy, so two surgeries could be considered: i) single neurectomy could improve the clinical symptoms of BPPV patients. In fact, this surgery can achieve good efficacy, yet some patients may be subjected to high risk of hearing loss. ii) Semicircular canal occlusion can be used to occlude the space in the crest with special material to reduce the stimulation of the hair cell sensory receptors in the ampulla. This procedure has low risk. However, surgeries may cause severe hearing loss, and thus should be considered carefully and should only be used when the efficacy of manual reduction and medical treatment was unsatisfactory.
References
- 1.van der Plas JP, Tijssen CC. Benign paroxysmal positional vertigo. Ned Tijdschr Geneeskd. 1998;142:2669–2674. (In Dutch) [PubMed] [Google Scholar]
- 2.Bestuzheva NV, Parfenov VA, Zamergrad MV. Benign paroxysmal positional vertigo in a female with arterial hypertension and meningioma. Zh Nevrol Psikhiatr Im S S Korsakova. 2014;114:100–104. (In Russian) [PubMed] [Google Scholar]
- 3.Dix MR, Hallpike CS. The pathology symptomatology and diagnosis of certain common disorders of the vestibular system. Proc R Soc Med. 1952;45:341–354. doi: 10.1177/003591575204500604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McClure JA. Horizontal canal BPV. J Otolaryngol. 1985;14:30–35. [PubMed] [Google Scholar]
- 5.Baloh RW, Jacobson K, Honrubia V. Horizontal semicircular canal variant of benign positional vertigo. Neurology. 1993;43:2542–2549. doi: 10.1212/WNL.43.12.2542. [DOI] [PubMed] [Google Scholar]
- 6.Lempert T. Horizontal benign positional vertigo. Neurology. 1994;44:2213–2214. doi: 10.1212/WNL.44.11.2213-a. [DOI] [PubMed] [Google Scholar]
- 7.Brandt T, Steddin S, Daroff RB. Therapy for benign paroxysmal positioning vertigo, revisited. Neurology. 1994;44:796–800. doi: 10.1212/WNL.44.5.796. [DOI] [PubMed] [Google Scholar]
- 8.Herdman SJ. Advances in the treatment of vestibular disorders. Phys Ther. 1997;77:602–618. doi: 10.1093/ptj/77.6.602. [DOI] [PubMed] [Google Scholar]
- 9.Curthoys IS, Manzari L. Otolithic disease: clinical features and the role of vestibular evoked myogenic potentials. Semin Neurol. 2013;33:231–237. doi: 10.1055/s-0033-1354595. [DOI] [PubMed] [Google Scholar]
- 10.Bo Z, Sun J. The characteristic of nystagmus in naked eyes and electronystagmogram of BPPV patients and the location diagnosis analysis. J Audiol Speech Pathol. 2012;20:235–237. [Google Scholar]
- 11.Cohen HS. Side-lying as an alternative to the Dix-Hallpike test of the posterior canal. Otol Neurotol. 2004;25:130–134. doi: 10.1097/00129492-200403000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Xie X. The diagnosis and treatment of BPPV after cervical spine surgery. Chin J EENT. 2004;14:151–153. [Google Scholar]
- 13.Giannini S, Signorini L, Bonanome L, Severino M, Corpaci F, Cielo A. Benign paroxysmal positional vertigo (BPPV): it may occur after dentalimplantology. A mini topical review. Eur Rev Med Pharmacol Sci. 2015;19:3543–3547. [PubMed] [Google Scholar]
- 14.Luis L, Costa J, Vaz Garcia F, Valls-Solé J, Brandt T, Schneider E. Spontaneous plugging of the horizontal semicircular canal with reversible canal dysfunction and recovery of vestibular evoked myogenic potentials. Otol Neurotol. 2013;34:743–747. doi: 10.1097/MAO.0b013e318287f343. [DOI] [PubMed] [Google Scholar]
- 15.Psillas G, Vital I, Rachovitsas D, Vital V, Tsalighopoulos M. Conversion of canalolithiasis to cupulolithiasis in the course of a horizontal benign paroxysmal positional vertigo case. Am J Otolaryngol. 2011;32:174–176. doi: 10.1016/j.amjoto.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 16.Mei X. The diagnosis of horizontal canal BPPV by the modified roll test. Mod Diagn Treat. 2014;25:1959–1961. [Google Scholar]
- 17.Rahko T, Kotti V. Walk-rotate-walk test identifies patients responding to Lemperts maneuver, with benign paroxysmal positional vertigo of the horizontal canal. Eur Arch Otorhinolaryngol. 2001;258:112–115. doi: 10.1007/s004050100329. [DOI] [PubMed] [Google Scholar]
- 18.Nuti D, Vannucchi P, Pagnini P. Lateral canal BPPV: which is the affected side? Audiol Med. 2005;3:16–20. doi: 10.1080/16513860510028275. [DOI] [Google Scholar]
- 19.Choung YH, Shin YR, Kahng H, Park K, Choi SJ. ‘Bow and lean test’ to determine the affected ear of horizontal canal benign paroxysmal positional vertigo. Laryngoscope. 2006;116:1776–1781. doi: 10.1097/01.mlg.0000231291.44818.be. [DOI] [PubMed] [Google Scholar]
- 20.Rahko T. The test and treatment methods of benign paroxysmal positional vertigo and an addition to the management of vertigo due to the superior vestibular canal (BPPV-SC) Clin Otolaryngol Allied Sci. 2002;27:392–395. doi: 10.1046/j.1365-2273.2002.00602.x. [DOI] [PubMed] [Google Scholar]
- 21.Talaat HS, Kabel AM, Khaliel LH, Abuhadied G, El-Naga HA, Talaat AS. Reduction of recurrence rate of benign paroxysmal positional vertigo by treatment of severe vitamin D deficiency. Auris Nasus Larynx. 2016;43:237–241. doi: 10.1016/j.anl.2015.08.009. [DOI] [PubMed] [Google Scholar]
- 22.Jiang Z. The importance of vestibular examination in the diagnosis of vertigo. Chin Med J (Engl) 2011;91:32–41. [Google Scholar]
- 23.Li H. The importance of inner ear MRI in the diagnosis of BPPV (85 cases) Chin J Mod Med. 2012;22:84–86. [Google Scholar]
- 24.Zhang Y, Gao G, Xu O. MRI of posterior circulation ischemia vertigo. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2011;18:70–72. [Google Scholar]
- 25.Yan J. The importance of inner ear MRI in the diagnosis of BPPV. J Intern Intensive Med. 2013;19:93–94. [Google Scholar]
- 26.Brandt T, Daroff RB. Physical therapy for benign paroxysmal positional vertigo. Arch Otolaryngol. 1980;106:484–485. doi: 10.1001/archotol.1980.00790320036009. [DOI] [PubMed] [Google Scholar]
- 27.Semont A, Freyss G, Vitte E. Curing the BPPV with a liberatory maneuver. Adv Otorhinolaryngol. 1988;42:290–293. doi: 10.1159/000416126. [DOI] [PubMed] [Google Scholar]
- 28.van der Scheer-Horst ES, van Benthem PP, Bruintjes TD, van Leeuwen RB, van der Zaag-Loonen HJ. The efficacy of vestibular rehabilitation in patients with benign paroxysmal positional vertigo: a rapid review. Otolaryngol Head Neck Surg. 2014;151:740–745. doi: 10.1177/0194599814546479. [DOI] [PubMed] [Google Scholar]
- 29.Okubadejo GO, Hohl JB, Donaldson WF. Dysphonia, dysphagia, and esophageal injuries after anterior cervical spine surgery. Instr Course Lect. 2009;58:729–736. [PubMed] [Google Scholar]
- 30.Epley JM. The canalith repositioning procedure: for treatment of benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 1992;107:399–404. doi: 10.1177/019459989210700310. [DOI] [PubMed] [Google Scholar]
- 31.Babac S, Arsović N. Efficacy of Epley maneuver in treatment of benign paroxysmal positional vertigo of the posterior semicircular canal. Vojnosanit Pregl. 2012;69:669–674. doi: 10.2298/VSP1208669B. (In Serbian) [DOI] [PubMed] [Google Scholar]
- 32.Anagnostou E, Stamboulis E, Kararizou E. Canal conversion after repositioning procedures: comparison of Semont and Epley maneuver. J Neurol. 2014;261:866–869. doi: 10.1007/s00415-014-7290-2. [DOI] [PubMed] [Google Scholar]
- 33.Yang Q. The efficacy of modified 3-step manual reduction in the treatment of posterior canal HBBP. Clin J Otorhinolaryngol Head Neck. 2014;28:1796–1798. [PubMed] [Google Scholar]
- 34.Baloh RW, Honrubia V, Jacobson K. Benign positional vertigo: clinical and oculographic features in 240 cases. Neurology. 1987;37:371–378. doi: 10.1212/WNL.37.3.371. [DOI] [PubMed] [Google Scholar]
- 35.Kim JS, Oh SY, Lee SH, Kang JH, Kim DU, Jeong SH, Choi KD, Moon IS, Kim BK, Kim HJ. Randomized clinical trial for geotropic horizontal canal benign paroxysmal positional vertigo. Neurology. 2012;79:700–707. doi: 10.1212/WNL.0b013e3182648b8b. [DOI] [PubMed] [Google Scholar]
- 36.Mandalà M, Pepponi E, Santoro GP, Cambi J, Casani A, Faralli M, Giannoni B, Gufoni M, Marcelli V, Trabalzini F, et al. Double-blind randomized trial on the efficacy of the Gufoni maneuver for treatment of lateral canal BPPV. Laryngoscope. 2013;123:1782–1786. doi: 10.1002/lary.23918. [DOI] [PubMed] [Google Scholar]
- 37.Riga M, Korres S, Korres G, Danielides V. Apogeotropic variant of lateral semicircular canal benign paroxysmal positional vertigo: is there a correlation between clinical findings, underlying pathophysiologic mechanisms and the effectiveness of repositioning maneuvers? Otol Neurotol. 2013;34:1155–1164. doi: 10.1097/MAO.0b013e318280db3a. [DOI] [PubMed] [Google Scholar]
- 38.Korres S, Riga MG, Xenellis J, Korres GS, Danielides V. Treatment of the horizontal semicircular canal canalithiasis: pros and cons of the repositioning maneuvers in a clinical study and critical review of the literature. Otol Neurotol. 2011;32:1302–1308. doi: 10.1097/MAO.0b013e31822f0bc5. [DOI] [PubMed] [Google Scholar]
- 39.Gufoni M, Mastrosimone L, Di Nasso F. Repositioning maneuver in benign paroxysmal vertigo of horizontal semicircular canal. Acta Otorhinolaryngol Ital. 1998;18:363–367. (In Italian) [PubMed] [Google Scholar]
- 40.Qi Z, Zhao F, Zhuang J. The experience of treatment and treatment of horizontal canal BPPV with apogeotropie nystagmus. Chin J EENT. 2014;14:142–144. [Google Scholar]
- 41.Chen Y. The treatment of horizontal canal otolith disease and crest otolith in the ampulla by sequential method. Clin J Otorhinolaryngol Head Neck. 2014;28:10–12. [Google Scholar]
- 42.Ren Y. The efficacy of barbecue roll maneuver for horizontal BPPV. Clin J Otorhinolaryngol Head Neck. 2014;20:356–357. [Google Scholar]
- 43.Mei X. The diagnosis and manual reduction of horizontal apogeotropie BPPV. Clin J Otorhinolaryngol Head Neck. 2014;28:15–17. [Google Scholar]
- 44.Testa D, Castaldo G, De Santis C, Trusio A, Motta G. Treatment of horizontal canal benign paroxysmal positional vertigo: a new rehabilitation technique. Sci World J. 2012;2012:160475. doi: 10.1100/2012/160475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vannucchi P, Pecci R. Pathophysiology of lateral semicircular canal paroxysmal positional vertigo. J Vestib Res. 2010;20:433–438. doi: 10.3233/VES-2010-0387. [DOI] [PubMed] [Google Scholar]
- 46.Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV) CMAJ. 2003;169:681–693. [PMC free article] [PubMed] [Google Scholar]
- 47.Chen D, Xiong S, Cui Y. Treatment of anterior canal benignparoxysmal positional vertigo by Yacovino repositioning maneuver. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2015;29:17–19. [PubMed] [Google Scholar]
- 48.Das S, Rea PA. Bilateral posterior semi-circular canal obliteration surgery for refractory benign paroxysmal positional vertigo (BPPV) in three patients. Clin Otolaryngol. 2017;42:480–483. doi: 10.1111/coa.12636. [DOI] [PubMed] [Google Scholar]
- 49.Xing D. The efficacy of suspended head reduction for posterior canal BPPV. J Audiol Speech Pathol. 2014;22:524–526. [Google Scholar]
- 50.De Stefano A, Dispenza F, Citraro L, Petrucci AG, Di Giovanni P, Kulamarva G, Mathur N, Croce A. Are postural restrictions necessary for management of posterior canal benign paroxysmal positional vertigo? Ann Otol Rhinol Laryngol. 2011;120:460–464. doi: 10.1177/000348941112000707. [DOI] [PubMed] [Google Scholar]
- 51.Papacharalampous GX, Vlastarakos PV, Kotsis GP, Davilis D, Manolopoulos L. The role of postural restrictions after BPPV treatment: real effect on successful treatment and BPPVs recurrence rates. Int J Otolaryngol. 2012;2012:932847. doi: 10.1155/2012/932847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Balikci HH, Ozbay I. Effects of postural restriction after modified Epley maneuver on recurrence of benign paroxysmal positional vertigo. Auris Nasus Larynx. 2014;41:428–431. doi: 10.1016/j.anl.2014.05.007. [DOI] [PubMed] [Google Scholar]
- 53.Mostafa BE, Youssef TA, Hamad AS. The necessity of post-maneuver postural restriction in treating benign paroxysmal positional vertigo: a meta-analytic study. Eur Arch Otorhinolaryngol. 2013;270:849–852. doi: 10.1007/s00405-012-2046-z. [DOI] [PubMed] [Google Scholar]
- 54.Zhang F. The efficacy of a new modified manual reduction for pediatric BPPV. Chin Med. 2012;9:124–125. [Google Scholar]
- 55.Li Z. Sixty cases of semi-supine turning-over exercise in the treatment of elderly BPPV patients. Southwest J Med. 2012;24:751–753. [Google Scholar]
- 56.Shan X, Ma L, Peng X. Clinical study of the treatment and diagnosis of BPPV by BPPV system. Chin J Stroke. 2013;8:340–345. [Google Scholar]
- 57.Sun Q. The feasibility analysis of SRM-IV in speed ladder test. Chin J Otol. 2014;12:467–469. [Google Scholar]
- 58.Yuan H. The efficacy of SRM-IV vestibular function diagnosis and treatment system for BPPV. J Audiol Speech Pathol. 2014;22:308–310. [Google Scholar]
- 59.Wang J. Clinical efficacy of SRM-IV vestibular function diagnosis and treatment system, Air Force. J Med. 2012;28:138–140. [Google Scholar]
- 60.Richard-Vitton T, Viirre E. Unsteadiness and drunkenness sensations as a new sub-type of BPPV. Rev Laryngol Otol Rhinol (Bord) 2011;132:75–80. [PubMed] [Google Scholar]
- 61.Tian Y, Zhang T, Jiang X. Diagnosis and treatment of 318 benign paroxysmal positional vertigo cases. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2012;26:13–15. doi: 10.13201/j.issn.1001-1781.2012.01.009. (In Chinese) [DOI] [PubMed] [Google Scholar]
- 62.Xu F. The design and development of a chair for antumatic reduction of otolith. Chin J Med Instr. 2013;37:103–106. [Google Scholar]
- 63.Zhang H, Geng M, Yan B. Comparative analysis of simple manual reduction and concomitant medication in the treatment of HBBP. Clin J Otorhinolaryngol Head Neck. 2012;26:750–752. [PubMed] [Google Scholar]
- 64.Pan J. Clinical observation of combined manual reduction in the treatment of HBBP. Clin Ration Drug Use. 2014;7:108. [Google Scholar]
- 65.Guneri EA, Kustutan O. The effects of betahistine in addition to epley maneuver in posterior canal benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 2012;146:104–108. doi: 10.1177/0194599811419093. [DOI] [PubMed] [Google Scholar]