Abstract
Smartphone fundus photography is a simple technique to obtain ocular fundus pictures using a smartphone camera and a conventional handheld indirect ophthalmoscopy lens. This technique is indispensable when picture documentation of optic nerve, retina, and retinal vessels is necessary but a fundus camera is not available. The main advantage of this technique is the widespread availability of smartphones that allows documentation of macula and optic nerve changes in many settings that was not previously possible. Following the well-defined steps detailed here, such as proper alignment of the phone camera, handheld lens, and the patient's pupil, is the key for obtaining a clear retina picture with no interfering light reflections and aberrations. In this paper, the optical principles of indirect ophthalmoscopy and fundus photography will be reviewed first. Then, the step-by-step method to record a good quality retinal image using a smartphone will be explained.
Keywords: Medicine, Issue 125, Smartphone, Fundus photography, Retina, Optic nerve, Ophthalmoscopy, Indirect Ophthalmoscopy, Fundus camera, Handheld plus lens
Introduction
Fundus photography is the standard method for documenting ocular fundus findings. Fundus photography is traditionally performed in a clinic setting using a fundus camera. However, fundus cameras are not available in many situations including in emergency rooms or on hospital floors where documentation of the retinal changes may be necessary. Indirect ophthalmoscope-mounted and handheld contact and non-contact fundus cameras are alternative ways to document retinal images, but availability and high cost limit their day-to-day use in most ophthalmology practices. Smartphones equipped with high-resolution cameras are increasingly being used for anterior segment and retinal imaging in ophthalmology.1,2
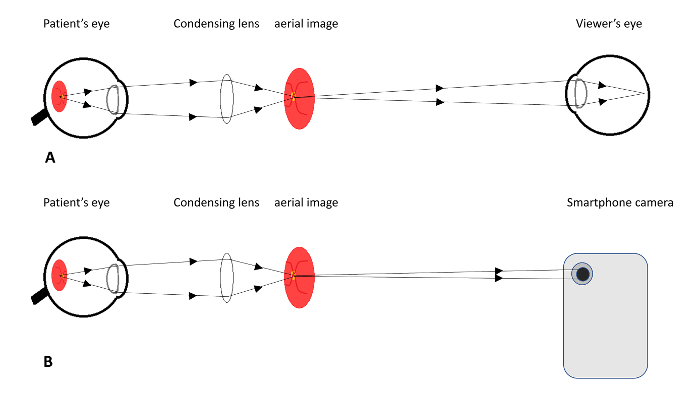
In smartphone retinal imaging, the smartphone camera's coaxial flashlight and a handheld high plus power lens create an indirect ophthalmoscopy-like optical system that is able to record high resolution digital retinal images (Figure 1).3,4,5,6,7 Smartphone adaptors for such retinal photography are commercially available from multiple companies3 and educational videos are publicly available to teach how to obtain retinal images using smartphones and these products. However, smartphone retinal photography does not necessarily need such adaptors. Here, we intend to teach how to record a good quality retinal image with a smartphone and tools readily available in an ophthalmology practice.
With increasing availability of smartphones and the expansion of telemedicine, this method can be adapted by ophthalmologists and optometrists to document retinal pathologies in emergency room settings and telemedicine consultations. In addition, health care providers may find this method useful in developing countries and in medical aid camps during a disaster rescue operation. Like any new technique, mastering smartphone retinal photography needs practice.8 The following protocol will explain detailed steps for smartphone photography. Optical basis of the technique will be discussed in the next section. Technical and operational constraints such as image resolution, field of view, and patient privacy and confidentiality will be discussed in the end.
Protocol
Ensure that fundus photography in the protocol follows the guidelines of your institutes human research ethics committee.
Note: Smartphone retinal imaging, like conventional indirect ophthalmoscopy, should be performed through a dilated pupil. A strong smartphone camera flash light is crucial to obtain a clear fundus picture, especially with mild to moderate media opacity. Make sure to practice the method on a model eye or on peers before attempting to examine the patient. Patient cooperation is a key for good smartphone fundus photography.
1. Smartphone Retinal Imaging
Explain the procedure to the patient and obtain permission. Explain that the process may take 1 - 2 min and involves shining a bright light into the eye.
Dilate the patient's pupil using a combination of mydriatic drops such as 2.5% Phenylephrine and 1% Tropicamide ophthalmic drops (one drop from each, 2 - 3 min apart, in the eye to be examined). Wait 15 - 20 min for pupils to dilate.
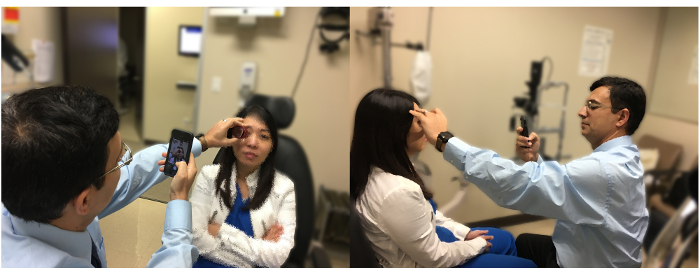
Sit in front of the patient on a comfortable chair and be positioned 30 - 60 cm from the patient and at about the same level (Figure 2).
Ask the patient to look at a far target with the other eye.
Set the smartphone camera on video mode.
Turn on the camera's flashlight.
After darkening the room, press the camera record button on the smartphone to record a continuous video.
Hold the +20 diopter (D) or any other indirect ophthalmoscopy lens in front of the patient’s eye with your thumb and index finger. Use the middle and ring fingers to stabilize the hand and lens and to help keep eyelids open.
Hold the camera 10 - 35 cm from the lens. Direct the camera along the patient's pupillary axis. Aim the light to the pupil and find the retina glow. Direct the light through the lens onto the retina and continue video recording.
While recording, move the camera and the lens to find a good focus and an image free of light reflections. Adjust the handheld lens to and from the patient’s eye to see a clear retina image filling the entire lens area. NOTE: In our experience, the lens should be held 3 - 5 cm from the eye (this is slightly further away from the cornea surface compared to what is appropriate for an indirect ophthalmoscopy exam).
Try to eliminate unnecessary light reflections by adjusting the camera and lens positions. Losing the image while searching the retina means that the camera and its flash light are not aligned with the handheld lens and pupil. It takes practice to keep the camera, handheld lens, and patient pupil aligned.
Continue to record video until a good view of the area of interest without significant light reflections and aberrations is captured.
Stop the recording and ask the patient to sit back and be comfortable.
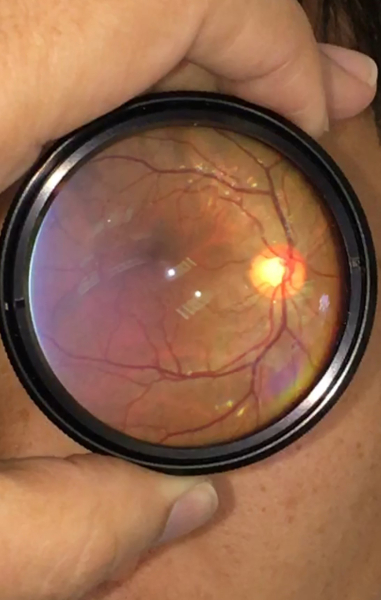
Re-play the recorded movie until there is a good retina view within the handheld lens area. Stop the movie and take a screen shot of the view (Figure 3).
Magnify the screen shot and take another screen shot for a larger retina image (Figure 3). Like an indirect ophthalmoscope view, this image is inverted.
Representative Results
The optics of fundus imaging using a smartphone camera is similar in principle to retina examination with indirect ophthalmoscope (Figure 1).9 In an indirect ophthalmoscope, a beam of light is directed toward the patient's retina and the reflected rays off the retina are condensed to a real aerial image using a handheld +15 - +30 D lens (Figure 1). The viewer sees the real, inverted aerial image that is located 2 - 4 cm from the handheld lens, depending on the power of the lens. With a smartphone, the camera's flashlight replaces the indirect ophthalmoscope light source and the smartphone camera recording the aerial image replaces the observer's eye. Conventional fundus cameras are also designed based on the same optical principles; the camera's film or digital sensor array is located where the aerial image is formed.
The portability of smartphones makes smartphone retinal imaging a promising technique for emergency rooms, telemedicine consulting, and retinal disease screening programs. Two representative images (Figure 4 and Figure 5) are recorded in emergency room and hospital floor consultation settings.
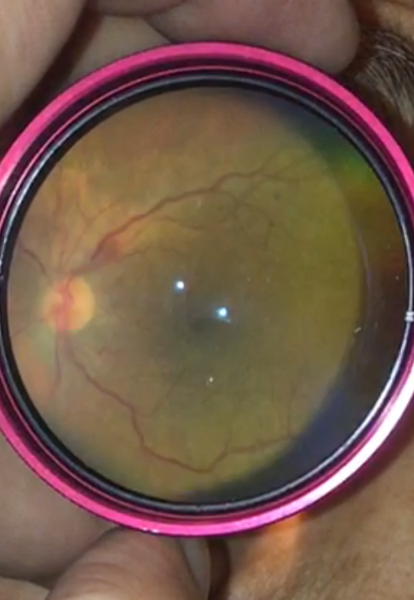

Figure 1: Optics of Indirect Ophthalmoscopy and Smartphone Fundus Photography. Schematic drawing shows the viewing system of an indirect ophthalmoscope (A) and fundus photography using a smartphone (B). Please click here to view a larger version of this figure.
Figure 2: Examiner and Patient Positioning for Smartphone Fundus Photography. The examiner sits in front and slightly to the side of the patient and holds the smartphone in one hand and the handheld lens in another hand about an arm length distance from the phone. Please click here to view a larger version of this figure.
Figure 3 : A Normal Macula and Optic Nerve Imaged Using a Smartphone. Please click here to view a larger version of this figure.
Figure 4: Nonproliferative Diabetic Retinopathy Imaged Using a Smartphone. Note flame-shaped and dot and blot retinal hemorrhages. Please click here to view a larger version of this figure.
Figure 5: Nonarteritic Anterior Ischemic Optic Neuropathy Imaged Using a Smartphone. Note the blurring of optic disc margins in this image. Please click here to view a larger version of this figure.
Discussion
The quality of fundus images taken by smartphone could be comparable to that of fundus cameras. In one comparison study of fundus images taken by smartphones and fundus cameras, masked reviewers did not find a significant difference.8,10 In the same study, the quality of fundus images was higher when images were captured by more experienced examiners compared to junior examiners.8
Smartphone fundus photography may appear a challenging technique in the beginning. However, like any other examination technique, mastering the technique needs practice and the process of smartphone imaging of the retina becomes routine with time. A particular challenge is related to the location of smartphone cameras and their screen. Most smartphone cameras are located at the corner of the phone while the screen to view and focus the image is at the center. A beginner should focus on mastering coordination between filming and lens hands and proper alignment of the phone, handheld lens, and the pupil axis.
Flashlight intensity cannot be adjusted within most smartphone camera settings. However, one may dim the light intensity by applying a semitransparent adhesive tape over the light source. Alternatively, filming interface apps may help adjusting the camera light intensity. Multiple smartphone apps are available that allow adjusting exposure, focus control, and flashlight intensity.4 While not an absolute requirement for smartphone fundus photography, examiners may find these filming/image taking interfaces helpful in improving the quality of their images.
The field of view varies with the diopter strength of the handheld indirect ophthalmoscopy lens. Lower power lenses (such as +15 D or +20 D lenses) provide a smaller field of view with higher magnification.
The confidentiality of personal data in accordance with Health Insurance Portability and Accountability Act 1996 (HIPAA), the Data Protection Act 1998, and Access to Health Records Act 1990 is a critical issue when using personal cameras to record health information. We take still retina pictures within our institute's electronic medical record (EMR) app that allows recording and transferring confidential patient images. Using dedicated cameras, encrypted phones, and HIPAA compatible email services are mandatory in many institutes for protecting patient privacy.
Smartphone fundus photography is a safe technique. Kim et al. showed that iPhone 4 camera flashlight is 10 times less luminous than a conventional indirect ophthalmoscope light.11 While this may offer more comfort for patients during imaging, it limits image clarity in the presence of moderate to significant media opacity. In the same study, the light levels of the smartphone light source were 150 times below the limit set by the International Organization for Standardization (ISO 15004-2.2) for ocular thermal hazard and 240 times below those limits for the photochemical hazard. Although light intensity and energy have not been measured for other smartphone models, it is suggested that they can be well below hazard limits.11
Although retinal images obtained with smartphone could be comparable to images taken by a fundus camera,8,10 recording a high-resolution smartphone retinal image requires an experienced examiner, a well-dilated pupil, clear ocular media, and a cooperative patient. Also, the field of view is usually limited in smartphone fundus images and creating widefield montage images may be time consuming. Nevertheless, smartphone fundus photography is a unique simple and affordable technique that allows picture documentation of retinal changes in many clinical settings where retinal imaging was not previously possible.
Disclosures
No proprietary interest to declare.
Acknowledgments
This work is supported in part by an educational found FRS 445960. We would like to thank Anh Tran, Juan Ortiz, and Ali Nazari for their help in preparing figure 2.
References
- Lord RK, et al. Novel uses of smartphones in ophthalmology. Ophthalmology. 2010;117(6):1274–1274. doi: 10.1016/j.ophtha.2010.01.001. [DOI] [PubMed] [Google Scholar]
- Chhablani J, Kaja S, Shah VA. Smartphones in ophthalmology. Indian J Ophthalmol. 2012;60(2):127–131. doi: 10.4103/0301-4738.94054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolster NM, Giardini ME, Bastawrous A. The Diabetic Retinopathy Screening Workflow: Potential for Smartphone Imaging. J Diabetes Sci Technol. 2015;10(2):318–324. doi: 10.1177/1932296815617969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haddock LJ, Kim DY, Mukai S. Simple, Inexpensive Technique for High-Quality Smartphone Fundus Photography in Human and Animal Eyes. J Ophthalmol. 2013. [DOI] [PMC free article] [PubMed]
- Maamari RN, et al. A mobile phone-based retinal camera for portable wide field imaging. Br J Ophthalmol. 2014;98(4):438–441. doi: 10.1136/bjophthalmol-2013-303797. [DOI] [PubMed] [Google Scholar]
- Raju B, Raju NS. Regarding fundus imaging with a mobile phone: a review of techniques. Indian J Ophthalmol. 2015;63(2):170–171. doi: 10.4103/0301-4738.154407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanmugam MP, et al. Fundus imaging with a mobile phone: a review of techniques. Indian J Ophthalmol. 2014;62(9):960–962. doi: 10.4103/0301-4738.143949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adam MK, et al. Quality and Diagnostic Utility of Mydriatic Smartphone Photography: The Smartphone Ophthalmoscopy Reliability Trial. Ophthalmic Surg Lasers Imaging Retina. 2015;46(6):631–637. doi: 10.3928/23258160-20150610-06. [DOI] [PubMed] [Google Scholar]
- Snead MP, Rubinstein MP, Jacobs PM. The optics of fundus examination. Surv Ophthalmol. 1992;36(6):439–445. doi: 10.1016/s0039-6257(05)80025-6. [DOI] [PubMed] [Google Scholar]
- Russo A, et al. Comparison of smartphone ophthalmoscopy with slit-lamp biomicroscopy for grading diabetic retinopathy. Am J Ophthalmol. 2015;159(2):360–364. doi: 10.1016/j.ajo.2014.11.008. [DOI] [PubMed] [Google Scholar]
- Kim DY, Delori F, Mukai S. Smartphone photography safety. Ophthalmology. 2012;119(10):2200–2201. doi: 10.1016/j.ophtha.2012.05.005. author reply 2201. [DOI] [PubMed] [Google Scholar]


