Abstract
Background:
Diagnosing and treatment of premenstrual syndrome (PMS) still pose a challenge in the routine medical practice which usually focuses on single pharmacological therapy. Recent research suggests that the combination of treatments including complementary alternative medicine (CAM) therapies may be more beneficial. The objective of this study was to assess the percentage of diagnosed and nondiagnosed PMS/premenstrual dysphoric disorder (PMDD) based on the presence of adequate symptoms and to compare population using hormonal or pharmaceutical agents versus CAM therapies.
Methods:
This is a cross-sectional study targeting sample population of 160 females of potentially reproductive age done in Ukraine between May 2014 and April 2015.
Results:
According to declared symptoms, 29% females versus 26% previously diagnosed by a medical professional qualify for “moderate/severe PMS,” P > 0.05. In 30% persons using pharmacological agents, major side effects, namely, nausea, insomnia, headache was caused by painkillers, contraceptives, and antidepressants. Only 37.5% of study population has been using CAM therapy methods to deal with the symptoms of PMS. Of these, 22% have achieved moderate degree in relief of the symptoms long term.
Conclusions:
We have concluded that when dealing with the burden of PMS/PMDD, the affected treatment-seeking women should have choice and access to the variety of therapies within integrative medicine (both conventional and nonconventional).
Keywords: Complementary alternative medicine, cross-sectional study, premenstrual dysphoric disorder, premenstrual syndrome
Introduction
The challenge of understanding and quantifying the burden of premenstrual syndrome (PMS) and premenstrual dysphoric disorder (PMDD) rests in the lack of uniformity of definitions and study methodology.[1,2] Across the literature concerning PMS, there is not a solid one number to describe the overall prevalence of PMS.[2,3,4] Conventional medical treatment[5,6,7] is symptom-based, usually prescribing a particular hormonal or pharmacological medication for one or two of the most troublesome symptoms that often results in serious side effects, but tending to ignore the whole picture.[8] Nonpharmacological interventions such as behavioral cognitive therapy, acupuncture, reflexology, unspecified physical exercise, yoga, massage, nutritional supplements, and other remedies result in effective PMS control.[9,10,11] Recent clinical research suggests that the combination of treatments (pharmacological and nonpharmacological) is more beneficial than single treatments.[12,13] Those suffering from these disorders deserve to have proper medical attention and to have choice of therapeutic treatment methods, including modalities of complementary alternative medicine (CAM).[14]
Recognizing, correctly diagnosing and applying ultimate treatment including CAM therapies in cases of PMS/PMDD condition is not a priority in the current routine medical practice in Ukraine, where medical system bears more reactive versus proactive character neglecting preventive care. Therefore, the primary objective of this study was to assess the percentage of diagnosed by a medical professional and nondiagnosed PMS/PMDD conditions based on the presence of adequate symptoms according to existent screening tools and to compare these assessments. To the best of our knowledge, there is no such study among Ukrainian population of any age groups. Secondary objective was to compare population using hormonal or pharmacological agents versus CAM therapies, assess consequential side effects in the users of pharmacological agents and the achieved degree of improvement of the condition in CAM therapies users and finally assess the overall level of awareness and acceptance of such therapies when dealing with PMS/PMDD.
Methods
Study design and setting
In the frame of educational curriculum of Master of Advanced Studies in Public Health at the University of Geneva, Switzerland, the observational cross-sectional study dedicated to the research of PMS/PMDD in general female population has been performed on the territory of Ukraine (Uzhgorod, Transcarpathia) in cooperation with the local diagnostics and treatment clinic in the period from May 2014 to April 2015. The current study is reported according to the STROBE Statement Checklist for Cross-Sectional Studies.[15]
A survey was launched through the Hemo-Medika[16] Center to collect suitable data related to PMS/PMDD in targeted female population of Uzhgorod (a town in Western Ukraine, bordering with Hungary and Slovakia). A questionnaire in Ukrainian language was designed with the help of DSM-IV definition of PMS and PMDD,[17] further inspired by and adapted from a nonvalidated questionnaire performed by PIHMA,[18] as well as adjusted from a validated premenstrual symptoms screening tool (PSST).[19,20] Our survey consisted of 20 questions, including sociodemographic information on age, profession, nature and nature of menstruation, health condition, and degree of physical activity. Further, it contained elements of the validated DSM-IV,[17] PMDD/PMS questionnaire related to presence/absence of related symptoms including 19 self-reported items assessing severity of PMS. Further, the questionnaire consisted of closed questions on determining whether the consultation with medical professional had taken place and if diagnosis of PMS/PMDD had been established; questions on the use of pharmacological agents and their possible side effects; questions on use of CAM methods and consequential degree of relieving the symptoms. Finally, there were three-Likert scale questions accessing openness and acceptance of the population toward CAM methods of treatment. The English version of the “Questionnaire” is provided in the Annex 1 of this article.
Description of the population/participants
The population under survey is a representative sample of a female population in the age range between 18 and 56 years visiting Clinic Hemo-Medika.[16] According to the data of epidemiological center in Uzhgorod, the total female population of reproductive age is approximately 32,000 persons. Clinic Hemo-Medika is one of the most established and frequented medical centers, providing a complete package of health services. Therefore, the selected population well represented the general population of the region.
Inclusion criteria
Females between 18 and 56 years of age, who are registered patients at the medical center Hemo-Medika, literate in Ukrainian language to be able to understand and read the proposed survey, potentially reproductive, and willing to participate were included in the study. The defined age limit being at 56 in potentially reproductive was inspired by the work of Minkin et al., 1997[21] where the limit age of menopause in modern Western world is defined at age 61 years and the average menopause age is at 56.
Exclusion criteria
Females in menopause and above 56 years of age, females younger than 18 years of age, with current major medical problems or with history of chronic illness, diabetes, high blood pressure, heart disease, or current depression, anxiety, and any other psychiatric disorder that have been previously diagnosed either at this medical center or at any other medical institution; those receiving hormonal therapy and experiencing a traumatic life event (marital separation or divorce, widowhood, death of a close person, imprisonment, dismissal from work) shortly before or during the study were excluded from the study.
Calculating the sample size
The sample size calculation can be based only on one outcome and in this study, it was assessing the percentage of PMS/PMDD. To calculate random sample size of the population, we have used the formula suggested by the Department of Obstetrics and Gynaecology of the Chinese University of Hong Kong (further DOBG CUHK).[22] According to the performed research of current studies, the prevalence is being estimated at 70%, and the acceptable error is defined at 0.07 with the margin of confidence interval (CI) at 95%, and the total population being 2400 persons (estimated number of visiting female residents aged 18 years and older of the medical center per year). The sample size, thus, was identified as 154 cases. We have verified the above calculations with the help of the suggested software by DOBG CUHK as well as the G*Power 3.1 (Heinrich Heine Universität Düsseldorf)[23] statistical power analysis software and we matched the results of manual and software calculations.
Statistical methods
For each question in the survey, we have identified and attributed a name of the corresponding variable (both qualitative and quantitative). The total number of collected and exploitable questionnaires with preliminary established masking was recreated within EpiData 3.1 statistical software programme (EpiData Association, Odense, Denmark, 2008)[24] and was entered for each submitted question for processing. Different sociodemographic, biological, reproductive, and psychosomatic variables were presented, compared, and analyzed. We exported the collected quantitative and qualitative variables to be further analyzed in a descriptive fashion and processed through STATA Statistical Software (StataCorp 11.0, 2009, Stata Statistical Software: Release 11. College Station, TX: StataCorp LP).[25] Kolmogorov–Smirnov test was used to analyze the distribution of the data, and one-way analysis of variance test was used to analyze the homogeneity of the data. Fisher's exact and Chi-square tests were used to compare the differences between groups. CI of 95% was calculated for percentage outcomes, and the results were considered statistically significant at P < 0.05 and nonsignificant at P > 0.05. The missing data (unanswered items on the questionnaire) were treated as N/A variables and included in the outcome analyses.
Ethical considerations
The managing board of the clinic as well as the Ethical Committee was approached in advance with a detailed protocol of the survey requesting the permission for the study. The followed procedures were also in accordance with the ethical standards of the Helsinki Declaration of 1975 and revised in 2000.[26] In the process of the study, the following ethical considerations were respected: protocol and study plan were approved beforehand by the Ethical Committee of Hemo-Medika; official written consent approved by the decree N110, as well as the primary registration form document N003-6/o, of February 14, 2012 have been signed by an eligible participant before proceeding to undertake the survey; each participant had the opportunity to learn more about this study from the principal investigator; all information about participants’ data has been kept confidential. Transmission of information related to participants’ answers to the questionnaire and their analysis in scientific publications have also remained anonymous.
Results
Study sample and participants profile
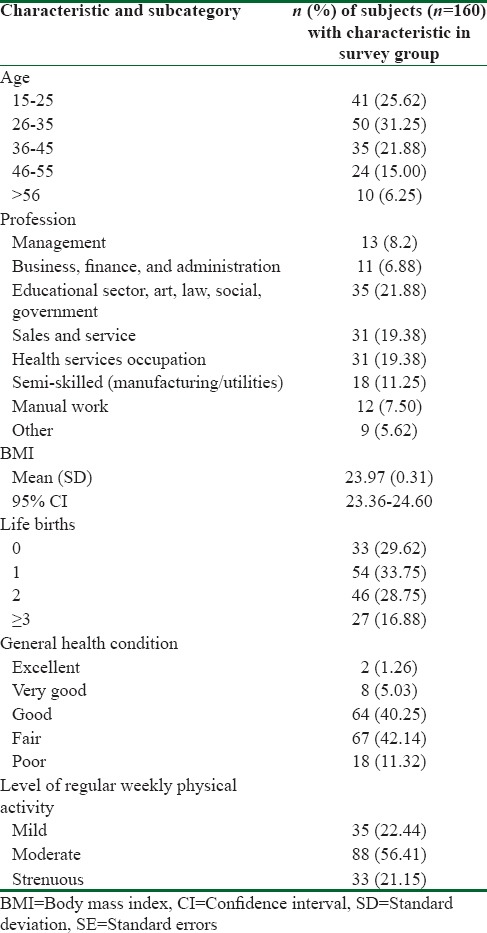
The total number of the participants in the study was 160 based on the calculated minimal sample size of 154. The majority of the surveyed population represented age group of 26–35 (31.25%). Largest group (21.88%) was represented by women from educational, art, law, social, or governmental segment. Average body mass index was 23.97 (standard deviation [SD] =0.31), CI 95% (23.36–24.60), having one live birth, with fair health condition and moderate physical activity per week. The overview of the population is presented in Table 1.
Table 1.
Sociodemographic characteristics of the surveyed population (n=160)
Outcome data
Affective and somatic symptoms in diagnosing of premenstrual syndrome, comparison of diagnosed and assessed premenstrual syndrome
As per our analysis, only 36% (CI 95%: 28.56–43.44) of sample population have solicited medical consultation in question of PMS complain symptoms, out of these only 26% (CI 95%: 19.43–33.07) were diagnosed with PMS/PMDD condition by a medical professional. According to a PSST validated tool[19] which gives more precise definition for diagnosis of PMS/PMDD (modified from existing DSM-IV criteria),[17] elements of which were partially used in our questionnaire as self-reported items, we can establish that in average women who have duly filled a 20-item symptomatic section can qualify for “no/mild PMS” (71% as per declared symptoms versus 74% as previously diagnosed by medical professional), or to “moderate/sever PMS” (29% vs. 26%, respectively), P > 0.05. In 30% of assessed population the PMS symptoms are present during three or more of consecutive months, and in 54% these symptoms are present during consecutive months for a period longer than a year. 48% of assessed population suffer the symptoms right before the onset of menstruation, and 37% - 1 week before their monthly period. The present symptoms qualify for PMS condition if the majority of affective and somatic symptoms occur during or longer than 3 consecutive months (29%), have an onset from 7 days before menstruation, and have been labeled as “moderate” or “severe.”
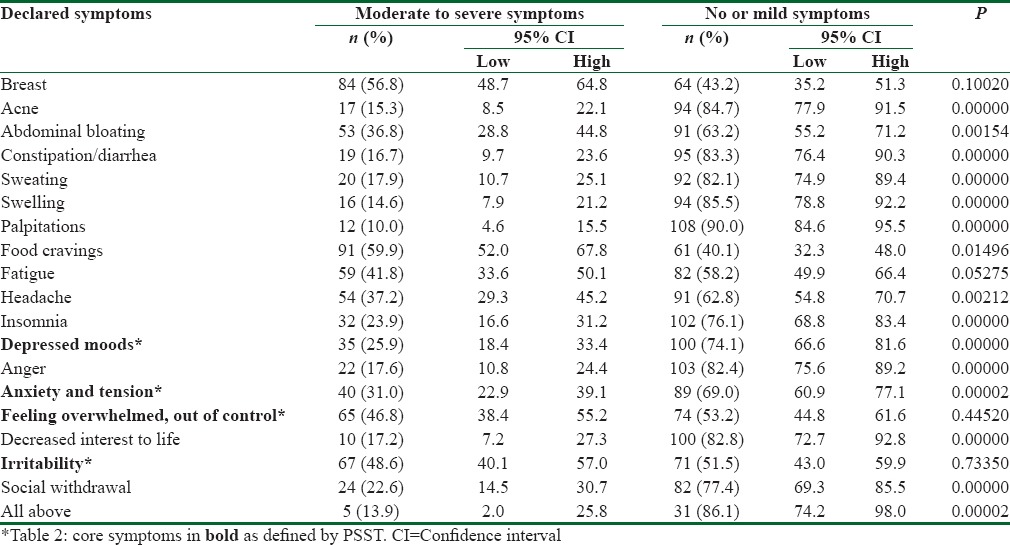
To qualify for PMDD, according to PSST criteria,[19] participants should have at least five to seven symptoms of affective and somatic character (with at least one being from the four core symptoms) that seriously interfere with social and economic performance, are not merely exacerbation of another disorder and have duration of ≥1 year. We have identified that in average 38% of the PMS group can be associated with PMDD syndrome. Results are presented in Table 2.
Table 2.
Affective and somatic symptoms in diagnosing of premenstrual syndrome
Using of hormonal and pharmacological agents and their side effects
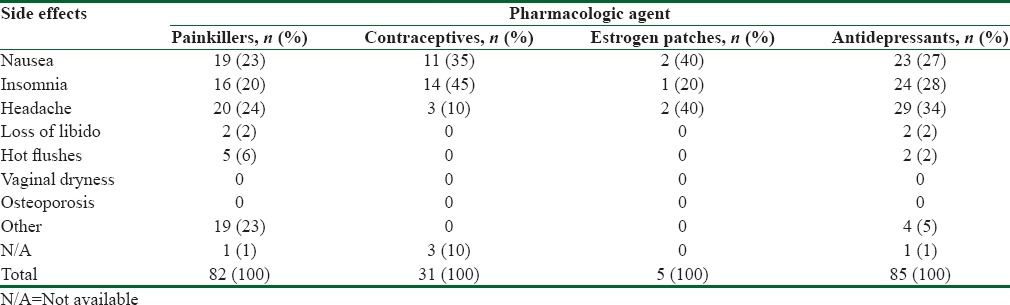
In 46/155 (30%, CI 95%: 22.79–37.21) of persons using pharmacological agents to suppress the symptoms of PMS/PMDD, major side effects, namely, nausea (23%–35%), insomnia (20%–45%), headache (10%–34%), or other were caused by either painkillers, contraceptives, or antidepressants. The most frequently used medications are antidepressants (55%, CI 95%: 47.17–62.83) – distributed between two subgroups “no/mild PMS” (21%) and “moderate/severe PMS” (34%), and painkillers (53%, CI 95%: 45.14–60.86), distributed between two subgroups “no/mild PMS” (22%) and “moderate/severe PMS,” (31%) respectively. Results of the analysis are presented in numbers in Table 3.
Table 3.
Hormonal and pharmacological agents and side effects
Complementary alternative medicine methods of treating premenstrual syndrome
We have assessed that only 60/160 (37.5%, CI 95%: 30–45) of study population have been turning to and using complementary alternative therapy methods (acupuncture, reflexology, massage, herbal medicine, vitamins, minerals and other supplements, nonspecified physical activity, yoga, etc.) to deal with the symptoms of PMS. These women were from both “no/mild PMS” (45%) and “moderate/severe PMS” (55%) subgroups. Of these, 22% (CI 95%: 11.52–32.48) has achieved moderate degree in relief of the symptoms long term, distributed between two subgroups “no/mild PMS” (49%) and “moderate/severe PMS” (51%), respectively. Unfortunately, in majority of surveys, despite our request to indicate the specific method of alternative medicine, the participants did not disclose the one most predominant modality they used.
Other analyzes
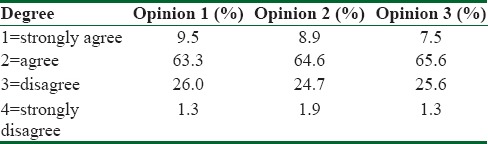
Finally, we have collected the opinion of the participants into three groups of questions: “I believe that CAM therapies are effective in treating PMS symptoms”; “I prefer to use the methods of treatment by CAM therapies in lieu of or in combination with the medicinal treatments;” “I will appreciate a concise and comprehensive printed information regarding possible therapies of CAM to treat PMS.” In each category of three questions, the most frequent answer in mean 102/160 (64%, CI 95%: 56.56–71.44) was “agree,” that is being receptive and open to the alternative medicine treatments and willing to accept the suggested proposition. The results are presented in Table 4.
Table 4.
Opinion survey
Discussion
Key results
Across the variety of criteria of assessment and interpretations of symptoms of premenstrual tension, the results for prevalence, in general, fluctuate between 5% and 97%.[27] Even though this subject has been researched for decades, the recognition and awareness of the condition are still in its embryonic stage. The clinician faced with these symptoms is called on to make a categorical judgment, presumably based on a clinical interview, as to whether a subject meets the diagnostic criteria for PMS/PMDD.[28,20] Existing studies differ in their interpretation of DSM-IV criteria, and definitions of clinically significant premenstrual symptoms are not comparable.[12,29,30] This study sheds new light on the phenomenology of PMS by estimating the prevalence based on assessing symptomatology of affective and somatic complaints, use of pharmacological agents and their impact on well-being, and identifying the perspectives for the noninvasive CAM therapies through increasing of awareness in the sample of Western Ukrainian female population.
Interpretation
The primary objective of the study has been achieved with statistically nonsignificant result (P > 0.05) in assessing the nondiagnosed PMS condition based on symptomatic assessment (in 128/160 of exploitable data) resulting in “moderate to severe PMS” group that has approximated the diagnosed condition (29.2%, SD = 2.05) versus 26.3%. Similar studies estimated the prevalence according to DSM-IV at 37.0%[31] and 35.6% of cases.[32] We have observed that the percentage of diagnosed PMS/PMDD condition by a medical professional has closely approached the percentage of assessed “moderate/severe PMS” condition. Thus, “mild PMS” symptomatic complaints might be neglected by medical professionals or by patients themselves and left out of potential relevant treatments to reestablish well-being at the initial stages of the problem. This is the area where CAM modalities would have a beneficial preventive application before letting the condition aggravate to more severe stage. Only 58/160 (36%) participants solicited medical consultation and treatment for their PMS, whereas in other similar study this was 48%.[31] Therefore, familiarity, recognizing, understanding of pathology and its stages, and the heightened level of awareness of possible treatment modalities is crucial in dealing with this condition in general, both in patients and in medical professionals.
The most common somatic complaints in the “moderate to severe” group were breast tenderness - 57%, food cravings - 60%, feeling overwhelmed and out of control – 47%, and being extremely irritable during the last week before the onset of their period – 49%. In the “No To Mild” symptomatic group, 90% of responders had been experiencing palpitations, swelling and edema of the limbs – 86%, acne - 85%, either constipation or diarrhea – 83%, anger – 82%, and finally experiencing insomnia – 76% and depressed moods - 74%. Grouping of various of these complaints represents precise patterns in Traditional Chinese Medicine (TCM) and involvement of different organs in somatic symptoms (i.e., heart or liver), which can be treated also in a more precise and accurate way. We have observed though that over one-quarter of the sample has turned toward hormonal and pharmacological agents and the most frequently used medications are painkillers and antidepressants to suppress the symptoms of PMS resulting in side effects (nausea, insomnia, and headache). Only 60/160 (37.5%) has turned to CAM therapies. In TCM, psychosomatic complaints are grouped into precise patterns and require different approach in treatment for each pattern. Therefore, antidepressants might not work for liver patterns but are better applied in heart patterns. The treatment modalities used in other similar study were painkillers – 63 (36.4%), hot drinks such as coffee and tea – 13 (7.5%), and massage therapy/exercise – 7 (4.0%).[30] In addition, as reported in the previous studies, more than half of PMS sufferers who used vitamins/dietary supplements,[33,34,35] acupuncture,[33,36] homeopathy,[33,37] yoga/mind body[35,37] and massage[34,35] have reported finding them satisfactory as a treatment.
There are numerous studies reporting positive effects of Chinese Herbal Medicine and acupuncture in the treatment of PMS. A systematic review and meta-analysis performed by Kim et al., 2011[11] have found a favorable effect of acupuncture over various controls (n = 429, pooled relative risk 1.55, 95% CI: 1.33–1.80, P < 0.00001). Nevertheless, as recent Australian study[38] on using CAM during premenstrual pain and discomfort shows, PMS sufferers are more likely to consult with an osteopath, massage therapist, naturopath/herbalist or alternative health practitioner and to have used all forms of CAM therapies except Chinese medicines than women who had infrequent PMS (all P < 0.05); however, there was an increasing trend to use herbal medicine with increasing frequency of PMS.[38] In spite of many years of sporadic use of yogic approaches that work on many areas simultaneously taking psychospiritual approach in perfecting and curing the body, it is in recent years when a long overdue effort is being carried on to establish these as a systematic cure method[39,40,41] and investigate the effectiveness of certain yogic practices in relieving negative symptoms of PMS.[42] As pointed out by Singh,[43] pharmacotherapy not only disturbs homeostatic rebalancing but also decreases motivation and self-insight where the regular practice of yoga develops a sensitivity of owns body and can sense and determine the ailments before they start developing into the physiological form. Even though Yoga/meditation has poor level of evidence while TCM has fairly strong level of evidence,[14,29] the above modalities of CAM are widely considered to be a catalyst for reversing the sub healthy state that PMS/PMDD present. Investigations of nutritional and multisupplements containing calcium (1200–1600 mg/day), magnesium, vitamin B6 (50–100 mg/day), essential micronutrients, and caffeine cessation show fair to good evidence.[14,29] Positive results for relieving somatic and psychologic symptoms of PMS were reported in a sham-controlled trial of reflexology.[44]
Even though a systemized CAM is still not established in Ukraine and many PMS sufferers may simply be unaware of existing CAM options, there are already many females (over half of our sample) turning to various methods for the treatment and are receptive to obtain more information. However, more extensive investigation is required to ascertain how effective and safe CAM use is in these circumstances, what is motivating their usage and how well informed all relevant health practitioners, as well as women with PMS/PMDD, are regarding the use of appropriate CAM.
Limitations and strengths of the study
The number of limitations of the current study includes impaired accuracy of the assessed data on actual symptoms and missing data on some questions; unfamiliarity of the studied population with the dysfunctional phenomenon of PMS/PMDD in general. Given that this topic is currently not on the priority list of health issues in Ukraine, this might explain the reluctant attitude toward the problematic by the female population. One of the major limitations of the study is that we used a nonvalidated questionnaire, but a combination of validated and nonvalidated questionnaires since the range of questions on the validated PSST tool was limited and did not reflect the objective of our study.[19] In addition, we did not differentiate between “no PMS” and “mild PMS”, and the assessment of PMDD differentiation was based on identified subgroup of “moderate/severe PMS”, which might bare the inaccuracy of estimation. Given that PMS/PMDD's symptoms strongly depend on somatic manifestations, further research is needed to incorporate the precise elements of the validated tools for screening to potentially combine it with the heritage of TCM which uses translation of both affective and somatic symptomatic manifestations into precise pattern differentiation that are used as a base for a treatment plan. Furthermore, our study pertains to one diagnosis within a specific region in Western Ukraine, and our results may not be applicable to other populations in Ukraine. As a result, this study should not be interpreted as endorsing method to assess of the prevalence of PMS. Nevertheless, this was one of the first studies dedicated to psychosomatic disorder conducted on the territory of Ukraine by the nonresident outside researchers.
Conclusions
This study has confirmed that PMS is a common health-care problem in general female population of reproductive age in Ukraine and is underrecognized by medical institutions in its management and treatment. To conclude, in seeking health-related information, affected women should be educated on and have access to the choice of therapies and remedies based on plausible established platform of evidence in dealing with the burden of PMS/PMDD. Further studies with larger sample size of population and using two comparative groups need to be conducted to confirm these results and to plan strategies for better detection, management, and preventive care of PMS.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
This work was supported and facilitated by the Clinic of Family Medicine - Hemo-Medika, in Uzhgorod, Ukraine. We wish to thank the staff and administration for their support and cooperation.
Questionnaire
This questionnaire is created to investigate and understand your condition of health and detect if you are prone to premenstrual syndrome (PMS). PMS refers to a number of physical and psychological symptoms that occur in certain women before the onset of their menses and interfere with their normal routines. The most usual symptoms are as described in point eight below. The condition may be severe enough to interfere with woman's social and occupational life, and long term may even lead to secondary infertility. Studies have shown that the burden of premenstrual symptoms is multidimensional, on health-related quality of life, health economic impact, and work productivity. Drug treatment which depends on a single-etiology/one-treatment mentality has not producing consistent success. A holistic noninvasive approach which combines diet and lifestyle changes as well as alternative therapies, has the ability to affect several systems in the body simultaneously treating the roots of a syndrome, and is the logical and most effective way to approach the treatment of PMS. Our aim is:
To find out how familiar are you with the condition and its possible ways of treatment
To increase your awareness of the condition and provide you with the self-effective tools of management of PMS
Please be so kind to answer the questions listed below:
-
Your age:
- 15–25
- 26–35
- 36–45
- 46–55
- >56.
-
Your occupation:
- Management
- Business, finance, and administration
- Occupation in education, art, law, social, government
- Sales and service
- Health services occupation
- Semi-skilled (manufacturing and utilities)
- Manual work
- Other activity (please describe) _______________________________________________
-
Your height and weight
- Height in centimeters
- Weight in kilograms.
-
How many life births did you have?
- 0
- 1
- 2
- ≥b.
-
In general, would you say your health is:
- Excellent
- Very good
- Good
- Fair
- Poor.
-
How active are you per week?
- Mild physical activity
- Moderate physical activity
- Strenuous physical activity.
-
Please tick out the box below that applies to you. Do you have:
- Regular menstruation, every 25–30 days
- Regular menstruation, shorter than every 25 days
- Regular menstruation, longer than every 30 days
- Menstruation with irregular intervals between bleeding
- Absence of menstruation
- Perimenopause.
-
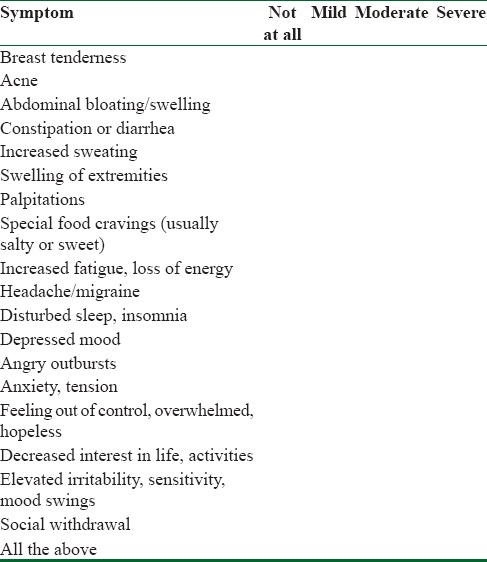
In case of having a menstruation, have you been or are you suffering from any of the below symptoms a few days or week/s before menstruation – please tick appropriate box as per the level of manifestation and fill out the last row below if you have any other symptom not listed below:
-
When do these symptoms occur?
- 7–14 days before menstruation
- 1–7 days before menstruation
- Right before and during menstruation
-
During how many consecutive symptomatic menstrual cycles have you experienced the above symptoms?
- ≤3 consecutive months
- ≥3 consecutive months
- Over a year or longer.
-
Have you seen a doctor or therapist with these complaints:
- Yes
- No.
-
Have you been diagnosed with PMS by your doctor/therapist?
- Yes
- No.
-
If you responded YES in the previous question, have you been using any of the below medications/aids to treat the above troubles:
- Painkillers (i.e. paracetamol)
- Contraceptive pills
- Estrogen only patches or implants
- Antidepressants, particularly selective serotonin reuptake inhibitors (i.e. fluoxetine, seraltine, prozac, zoloft, and paxil)
- Gonadotropin-releasing hormone analog in the form or injections.
-
Have you observed any of the following additional symptoms after taking any of the above medical aids:
- Nausea
- Insomnia
- Headache
- Loss of libido
- Hot flushes
- Vaginal dryness
- Osteoporosis (thinning of the bones)
- Any other that are not listed here.
-
Have you considered or tried any of the listed below alternative medical approach/es?
-
Yes
- Acupuncture
- Reflexology
- Massage
- Herbal Medicine
- Vitamins, minerals, and other supplements
- Diet change
- Physical activity (yoga, Pilates, gym, aerobics, walking/running) – please underline the relevant
- Homeopathy
- Any other not listed above
- No
-
-
Did you experience any relief from the symptoms described in point #5 through any of the alternative therapies, to what extend?
-
Yes
- Not at all
- Moderately
- Strongly
- No
-
-
If you responded yes, which alternative approach have you tried (please right it down)?
- ________________________
-
I believe that complimentary alternative medicine (therapies) are effective in treating symptoms indicated in point #5:
- Strongly agree
- Agree
- Disagree
- Strongly disagree
-
I prefer to use the methods of treatment by complimentary alternative medicine (therapies) in lieu of or in combination with the medicinal treatments:
- Strongly agree
- Agree
- Disagree
- Strongly disagree.
-
I will appreciate and will use for preventive self-treatment a concise and comprehensive printed information regarding possible methods of complimentary alternative medicine (therapies) to treat the condition of PMS:
- Strongly agree
- Agree
- Disagree
- Strongly disagree.
Thank You!
References
- 1.Johnson SR. The epidemiology and social impact of premenstrual symptoms. Clin Obstet Gynecol. 1987;30:367–76. doi: 10.1097/00003081-198706000-00017. [DOI] [PubMed] [Google Scholar]
- 2.Halbreich U, Borenstein J, Pearlstein T, Kahn LS. The prevalence, impairment, impact, and burden of premenstrual dysphoric disorder (PMS/PMDD) Psychoneuroendocrinology. 2003;28(Suppl 3):1–23. doi: 10.1016/s0306-4530(03)00098-2. [DOI] [PubMed] [Google Scholar]
- 3.Bakhshani NM, Mousavi MN, Khodabandeh G. Prevalence and severity of premenstrual symptoms among Iranian female university students. J Pak Med Assoc. 2009;59:205–8. [PubMed] [Google Scholar]
- 4.Khodjaeva N, Khaydarova F. Prevalence of pre-menstrual syndrome among women of child bearing age with regular menstrual cycle. Med Health Sci J. 2013;14:144–9. [Google Scholar]
- 5.De Monico SO, Brown CS, Ling FW. Premenstrual syndrome. Curr Opin Obstet Gynecol. 1994;6:499–502. [PubMed] [Google Scholar]
- 6.O’Brien PM, Abukhalil IE. Randomized controlled trial of the management of premenstrual syndrome and premenstrual mastalgia using luteal phase-only danazol. Am J Obstet Gynecol. 1999;180(1 Pt 1):18–23. doi: 10.1016/s0002-9378(99)70142-0. [DOI] [PubMed] [Google Scholar]
- 7.Freeman EW, Rickels K, Sondheimer SJ, Polansky M. A double-blind trial of oral progesterone, alprazolam, and placebo in treatment of severe premenstrual syndrome. JAMA. 1995;274:51–7. [PubMed] [Google Scholar]
- 8.Jang HS, Lee MS. Effects of qi therapy (external qigong) on premenstrual syndrome: A randomized placebo-controlled study. J Altern Complement Med. 2004;10:456–62. doi: 10.1089/1075553041323902. [DOI] [PubMed] [Google Scholar]
- 9.Marriam Z, Khawala TM. Pre-menstrual syndrome – A review. J Pharm Sci Res. 2012;4:1684–91. [Google Scholar]
- 10.Zhou J, Qu F. Treating gynaecological disorders with traditional Chinese medicine: A review. Afr J Tradit Complement Altern Med. 2009;6:494–517. doi: 10.4314/ajtcam.v6i4.57181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim SY, Park HJ, Lee H, Lee H. Acupuncture for premenstrual syndrome: A systematic review and meta-analysis of randomised controlled trials. BJOG. 2011;118:899–915. doi: 10.1111/j.1471-0528.2011.02994.x. [DOI] [PubMed] [Google Scholar]
- 12.Rapkin A. A review of treatment of premenstrual syndrome and premenstrual dysphoric disorder. Psychoneuroendocrinology. 2003;28(Suppl 3):39–53. doi: 10.1016/s0306-4530(03)00096-9. [DOI] [PubMed] [Google Scholar]
- 13.Rapkin AJ. New treatment approaches for premenstrual disorders. Am J Manag Care. 2005;11(16 Suppl):S480–91. [PubMed] [Google Scholar]
- 14.Stevinson C, Ernst E. Complementary/alternative therapies for premenstrual syndrome: A systematic review of randomized controlled trials. Am J Obstet Gynecol. 2001;185:227–35. doi: 10.1067/mob.2001.113643. [DOI] [PubMed] [Google Scholar]
- 15.Strobe-Statement.Org. ISPM; University of Bern. 2009. [Last cited on 2016 Jan 18]. Available from: http://www.strobestatement.org/fileadmin/Strobe/uploads/checklists/STROBE_checklist_v4_cross-sectional.pdf .
- 16. [Last accessed on 2017 Jun 02]. Available from: http://www.hemomedika-uzhgorod.eu/
- 17.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994. p. 715. [Google Scholar]
- 18.Pihma.edu. Phoenix: Complete a PMS Survey for the Foundation for PIHMA Research and Education, Phoenix Institute of Herbal Medicine and Acupuncture. [Last cited on 2016 Jan 18]. Available from: http://www.pihma.edu/complete-a-foundation-for-pihmaresearch-education-survey/
- 19.Steiner M, Macdougall M, Brown E. Original contribution: The premenstrual symptoms screening tool (PSST) for clinicians. Arch Womens Ment Health. 2003;6:203–9. doi: 10.1007/s00737-003-0018-4. [DOI] [PubMed] [Google Scholar]
- 20.O’Brien PM, Bäckström T, Brown C, Dennerstein L, Endicott J, Epperson CN, et al. Towards a consensus on diagnostic criteria, measurement and trial design of the premenstrual disorders: The ISPMD Montreal consensus. Arch Womens Ment Health. 2011;14:13–21. doi: 10.1007/s00737-010-0201-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Minkin MJ, et Carol V. Wright What Every Woman Needs to Know about Menopause. Yale University Press. US by R.R. Donnelley & Sons. 1997 ISBN 0-300-07261-9. [Google Scholar]
- 22.Department of Obstetrics and Gynecology. The Chinese University of Hong Kong: Sample Size Estimation. 2014. [Last cited on 2016 Jan 19]. Available from: http://www.department.obg.cuhk.edu.hk/researchsupport/Sample_size_EstPrev.asp .
- 23.Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–91. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- 24. [Last accessed on 2017 Jun 02]. Available from: http://www.epidata.dk/about.htm .
- 25. [Last accessed on 2017 Jun 02]. Available from: http://www.stata.com .
- 26. [Last accessed on 2017 Jun 02]. Available from: http://www.wma.net/en/30publications/10policies/b3/
- 27.Deadman P. Acupuncture in the treatment of premenstrual syndrome. J Chin Med. 1995;48:5–14. [Google Scholar]
- 28.Gehlert S, Hartlage S. A design for studying the DSM-IV research criteria of premenstrual dysphoric disorder. J Psychosom Obstet Gynaecol. 1997;18:36–44. doi: 10.3109/01674829709085567. [DOI] [PubMed] [Google Scholar]
- 29.Girman A, Lee R, Kligler B. An integrative medicine approach to premenstrual syndrome. Am J Obstet Gynecol. 2003;188(5 Suppl):S56–65. doi: 10.1067/mob.2003.403. [DOI] [PubMed] [Google Scholar]
- 30.Hylan TR, Sundell K, Judge R. The impact of premenstrual symptomatology on functioning and treatment-seeking behavior: Experience from the United States, United Kingdom, and France. J Womens Health Gend Based Med. 1999;8:1043–52. doi: 10.1089/jwh.1.1999.8.1043. [DOI] [PubMed] [Google Scholar]
- 31.Tolossa FW, Bekele ML. Prevalence, impacts and medical managements of premenstrual syndrome among female students: Cross-sectional study in college of health sciences, Mekelle University, Mekelle, Northern Ethiopia. BMC Womens Health. 2014;14:52. doi: 10.1186/1472-6874-14-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Balaha MH, Amr MA, Saleh Al Moghannum M, Saab Al Muhaidab N. The phenomenology of premenstrual syndrome in female medical students: A cross sectional study. Pan Afr Med J. 2010;5:4. doi: 10.4314/pamj.v5i1.56194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Domoney CL, Vashisht A, Studd JW. Use of complementary therapies by women attending a specialist premenstrual syndrome clinic. Gynecol Endocrinol. 2003;17:13–8. [PubMed] [Google Scholar]
- 34.Campbell EM, Peterkin D, O’Grady K, Sanson-Fisher R. Premenstrual symptoms in general practice patients. Prevalence and treatment. J Reprod Med. 1997;42:637–46. [PubMed] [Google Scholar]
- 35.Pullon SR, Reinken JA, Sparrow MJ. Treatment of premenstrual symptoms in Wellington women. N Z Med J. 1989;102:72–4. [PubMed] [Google Scholar]
- 36.Kuppermann M, Learman LA, Schembri M, Gregorich S, Jacoby A, Jackson RA, et al. Effect of noncancerous pelvic problems on health-related quality of life and sexual functioning. Obstet Gynecol. 2007;110:633–42. doi: 10.1097/01.AOG.0000279153.56275.b5. [DOI] [PubMed] [Google Scholar]
- 37.Singh BB, Berman BM, Simpson RL, Annechild A. Incidence of premenstrual syndrome and remedy usage: A national probability sample study. Altern Ther Health Med. 1998;4:75–9. [PubMed] [Google Scholar]
- 38.Fisher C, Adams J, Hickman L, Sibbritt D. The use of complementary and alternative medicine by 7427 Australian women with cyclic perimenstrual pain and discomfort: A cross-sectional study. BMC Complement Altern Med. 2016;16:129. doi: 10.1186/s12906-016-1119-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Garde KK. Principles and Practice of Yoga Therapy. Bombay: DB Taraporevala Sons; 1972. [Google Scholar]
- 40.Ikemi Y, Goyeche JR. Yoga as a potential psychosomatic therapy. Asian Med J. 1977;20:26–32. [Google Scholar]
- 41.Anand BK, China GS, Singh B. Some aspects of electroencephalographic studies of yogis. Electroencephalogr Clin Neurophysiol. 1961;13:452–6. [Google Scholar]
- 42.Sridevi K, Krishna Rao P. Yoga practice and menstrual distress. J Indian Acad Appl Psychol. 1996;22:47–54. [Google Scholar]
- 43.Singh AN. Role of yoga therapies in psychosomatic disorders. Int Congr Ser. 2006;1287:91–6. [Google Scholar]
- 44.Oleson T, Flocco W. Randomized controlled study of premenstrual symptoms treated with ear, hand and foot reflexology. Acta Obstet Gynec Scand. 1971;50:331–7. [PubMed] [Google Scholar]


