Abstract
Patellar instability is a common presenting clinical entity in the field of orthopedics. This not only can occur from baseline morphologic variability within the patellofemoral articulation and alignment, but also from traumatic injury. While conservative management is many times employed early in the treatment course, symptomatic patellar instability can persist. This article reviews the available indexed published literature regarding patellar instability. Given the debilitating nature of this condition and the long term sequelae that can evolve from its lack of adequate recognition and treatment, this article details the most current methods in the evaluation of this entity as well as reviews the most up-to-date surgical treatment regimens that are available to address this condition.
Keywords: Medial patellofemoral ligament, patella alta, patellar instability, tibial tubercle osteotomy, tibial tubercle-trochlear groove, trochlear dysplasia, trochleoplasty
MeSH terms: Patella, osteotomy, patellar dislocation, patella femoral pain syndrome
Introduction
It is estimated that 2%–3% of orthopedic presentations involving the knee joint will involve patellar dislocations, with a 29/100,000 per capita risk of a first-time patellar dislocation, among adolescents.1,2,3 Fifty to sixty percentage of initial first-time lateral patellar dislocations will occur secondary to a sports related injury and will involve a compromised medial patellofemoral ligament (MPFL) and medial retinaculum at least 80% of the time.1,4,5,6 Age and race (15–19-year-old and African-Americans and Caucasians), were found to be risk factors for patellar dislocation; however, gender was not a factor.6 Whether patellar instability is caused by a traumatic event or from morphologic variants of baseline anatomy, it is crucial to understand the anatomic restraints to excessive patellar mobility and the clinical and radiographic assessments that will help guide the treatment regimens best suited for that patient. The multifactorial nature of the presenting problem, whether it be MPFL incompetence, trochlear dysplasia, excessive tibial tubercle (TT) lateralization with elevated tibial tubercle-trochlear groove (TTTG) distance, or patella alta, can be addressed with surgical interventions to address each one of the underlying pathologies.
Anatomy
Prior anatomic studies have nicely detailed the medial-sided knee structures. The MPFL is located 1.9 mm anterior and 3.8 mm distal to the adductor tubercle and 10.6 mm proximal and 8.8 mm posterior to the medial epicondyle.7 It has a broad insertion onto the medial superior half of the patella, and the most distal aspect of the vastus medialis obliquus (VMO) insertion.7 The role of the MPFL as the most important patellar stabilizer during the first 30° of knee flexion has been well-defined.8,9 During the first 30° of flexion, the MPFL provides 50%–60% of medial restraint to lateral subluxation, with the trochlear groove providing further patellar stability with deeper knee flexion.8,10 Variants in trochlear morphology can predispose the patella to maltracking or even gross subluxation/dislocation and can influence recurrent patellar instability.11,12,13 A large supratrochlear spur can be an impediment to normal patellar tracking into the trochlear groove, causing the patella to “kick” laterally as the knee goes from extension to flexion. Furthermore, patella alta can be a contributing factor for patellar instability, requiring a greater travel distance as the knee flexes to adequately center into the groove. Should a deficient trochlear groove or supratrochlear spur be present as well, this can also heavily influence symptomatic instability.14
The TT arises from the lateral aspect of the proximal tibia. Excessive lateralization of this tubercle increased tibial external rotation, severe genu valgum, or even increased femoral anteversion with a relative increase in femoral internal rotation, can all affect patellar tracking and cause a dramatic change in the Q-angle with resultant lateralized vector with quadriceps activation.14 This directly affects the patellofemoral articulation and should an MPFL be incompetent, this can have immediate effects in early flexion with patellar subluxation and recurrent dislocations.
Different surgical techniques have been developed over time to adequately address each one of the morphologic variants predisposing the knee to recurrent patellar instability. For the at risk knee, a tibial tubercle osteotomy (TTO) with varying degrees of obliquity can adequately address a lateralized TT and increased TTTG distance. While MPFL repairs have generally fallen out of favor given their lack of long term success, the development of the MPFL reconstruction with varying techniques has resulted in a more reproducible means of re-establishing the most important soft tissue restraint during early flexion. A sulcus deepening trochleoplasty can be a powerful correction to reshape the trochlear groove. This improves not only the osteochondral restraint to maintain satisfactory patellofemoral articulation in mid and deep flexion, but most importantly removes the supratrochlear spur that “kicks” the patella laterally in early flexion. Addressing these morphologic variants will allow the patella to adequately glide in normalized soft tissue and bony restraints during patellofemoral articulation.
Evaluation and Assessment
Physical examination
It is always important to define whether it is pain or instability as it pertains to the patellofemoral joint. Acute patellar dislocations occur in at-risk knees during slight knee flexion with a rotatory tibial external rotation moment or occasionally with a direct impact to the medial patella. This corresponds to when the patella is most vulnerable biomechanically, in early flexion given the lack of bony congruency as the patella has not engaged the bony constraint of the trochlea yet. With increased tibial external rotation, there is a relative increase in the Q-angle during quadriceps activation. Severe genu valgum can also increase the risk of patellar instability given the increased Q-angle with quadriceps activation and lateral directed vector on the patella. As the knee flexes further, the patella is trapped on the lateral knee to complete the dislocation. Pain related buckling, often confused by patients as patella instability, is an acute quadriceps inhibition from a painful stimulus, such as loading the patella during stair climbing or descent. A history of the event occurring while the knee is already flexed, such as on the stairs, is a clue to the pain-related buckling etiology rather than instability. Further gross clinical examination of “squinting patellae” can also clue the physician into the presence of excessive femoral anteversion, potentially requiring further advanced imaging.
Usually, an acute dislocation will present with a marked hemarthrosis, tenderness to palpation at the medial border of the patella or at the ligament's femoral origin, and possibly a block to the motion should a displaced osteochondral fragment be present. In the acute setting, assessments for apprehension can be difficult to obtain given effusion and patient willingness to comply with the examination secondary to pain. In the subacute to chronic conditions, marked apprehension with static and dynamic assessments can be seen. The sensitivity for the apprehension test has been reported to be only 39%, while the moving apprehension sign has been shown to be 100% sensitive and 88% specific for adequately and accurately determining patellar instability.15,16 The amount of knee flexion that still permits passive lateral patella translation can give an indication of just how unstable the patella is. For this test to be positive, both aspects need to be positive. The Sage sign, or patellar glide test to assess lateral patellar translation in extension, is normal if only one to two quadrants translation exists, corresponding to half the patellar width. Any further gross excursion would suggest prior injury or attenuation of the MPFL; however, baseline hypermobility should be assessed on the contralateral side and Beighton criteria should be assessed with a score of >5/9 suggesting baseline joint hypermobility.17,18 The “J” sign is a useful physical examination finding, which can provide insight to any gross malalignment, trochlear dysplasia, or patella alta that could be contributing to the patellar instability. With the knee at 90° of flexion, the patient actively extends their knee to full extension and the examiner closely watches for the patella to subluxate/dislocate laterally. This would either signify patella alta or a supratrochlear spur, or both and indicates the patella is fully out of any normal trochlear bony restraint. A positive patellar grind, or Clarke's test, would indicate patellofemoral chondromalacia and potentially correlate to a history of anterior knee pain. Overall limb alignment should not only be checked visually while the patient is standing, to review for excessive genu valgum which would increase the Q-angle vector during extensor mechanism activation but can also be checked with full length standing alignment films.
Diagnostic imaging
A standard 3-view radiographic series includes a standing flexion posteroanterior, lateral, and 45° flexed axial Merchant view of the knee. Axial views of the patella in deeper degrees of flexion are rarely helpful, and actually can be misleading since the patella is almost always well-centered in the trochlea. A true lateral radiograph of the knee can provide insight into the presence of trochlear dysplasia as well as patella alta. While there are numerous measurements available to quantify the patellar height, it is the Caton–Deschamps index (CDI) that is probably best to assess for patella alta, given it obviates the need to obtain a lateral radiograph in 30° of flexion [Figure 1]. This measurement is in contradistinction to the Blackburn–Peal ratio, which does require the lateral radiograph to be obtained in 30° of knee flexion, and furthermore the CDI does not include the nonarticulating patella nose in the calculation as does the Insall–Salvati ratio.19,20,21 We prefer to obtain an axial patellar view with the knee in 30° of flexion to determine the sulcus angle, patellar tilt angles, and congruence angles. An additional useful axial radiograph is the Laurin view, obtained at 20° of knee flexion and the beam directed from caudal to cephalad. Both of these axial radiographs are a reliable way to obtain information regarding patellar subluxation in early flexion that other axial patellar views miss secondary to the increased flexion angles with patellar re-engagement already. However, these radiographs cannot adequately view the proximal trochlea and will miss the presence of a supratrochlear spur, which is best appreciated on a lateral radiograph. Despite the information that can be gleamed from basic radiographs, further detailed assessments of trochlear dysplasia, patellar height, and TT lateralization are better assessed by advanced diagnostic imaging [Figure 2].
Figure 1.

A lateral radiograph of right knee joint showing the Caton–Deschamps index measured as the ratio of the blue line/yellow line (blue line distance measured from the tibial plateau to the inferior articular margin of the patella. Yellow line distance measured from the superior to inferior extent of patellar articular margin)
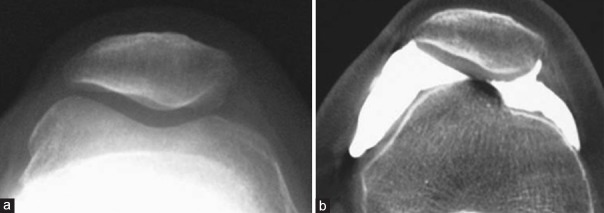
Figure 2.
(a) Standard axial patellar radiograph view of knee in 30° of flexion. (b) Computed tomography arthrogram axial image of the same knee in full extension revealing the presence of a supratrochlear spur
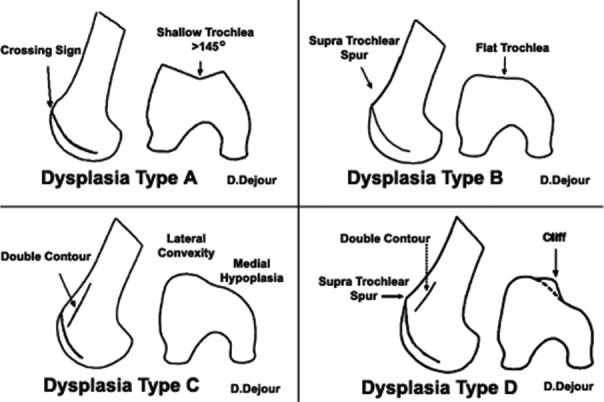
Advanced diagnostic imaging is recommended for evaluating osteochondral lesions in the acute setting, and to better define trochlear morphology, alignment, and patella height. Dejour and Le Coultre provided a standardized classification system after reviewing radiographs and computed tomography (CT) scans, defining trochlear dysplasia as morphologic variants containing combinations of the crossing sign, supratrochlear spur, and double contour sign [Figure 3].22 Type B and D trochleas contain a supratrochlear spur, which can be amenable to a sulcus deepening trochleoplasty to re-establish satisfactory osteochondral restraints during patellofemoral articulation. A CT and magnetic resonance imaging (MRI) scan can be of great benefit in defining the baseline anatomy in cases of patellar instability as well as providing guidance in planning for surgical procedures. A TTTG has largely supplanted the use of a Q-angle in assessing the overall lateralization of the TT. While proponents of a TT-posterior cruciate ligament (TT-PCL) distance >24 mm advocate for this measurement given it negates the rotational influence of the femur in the measurement as it is solely measured from tibial reference points, the TTTG is still more commonly utilized in assessing any gross axial malalignment given the measurements high specificity for predicting recurrent patellar instability.23,24,25 A CT scan can aid in classification of trochlear dysplasia with clear identification of a trochlear spur. Classically, a value of 20 mm has been set as a threshold for an excessive TTTG distance, where a surgical intervention is considered in the presence of patellar instability [Figure 4]. Several studies have confirmed the use of MRI in assessing trochlear dysplasia and in measuring the TTTG, however, they have reported that an MRI can underestimate the TTTG distance by up to 4 mm, challenging the aforementioned 20 mm threshold when measured on MRI.26,27 An MRI can be used to assess supratrochlear spur height, which is measured as a prominence extending anterior to a line drawn down the anterior femoral cortex, and the patellar trochlear index (PTI) [Figure 5].28 In the setting of chronically subluxated/dislocated patellae, it is impossible to use the PTI given the ratio cannot be defined on one sagittal image. Instead, the sagittal patellar engagement (SPE) measurement can be determined by taking a single sagittal image with the longest measured distance of the patellar cartilage and a second sagittal image with the most proximal extension of the trochlear cartilage.28,29 The PTI and SPE provide information on the presence of a dysplastic, short, proximal trochlea as well as decreased patellofemoral engagement. This can add additional information that can help determine and guide surgical treatments, especially when patella alta does not exist by classic patellar height radiographic measurements.30 Furthermore, on axial MRI, the trochlear depth can be determined to further assess the presence of a shallow trochlear floor as evidence of dysplasia. Previous published work reported that a trochlear depth <3 mm was 100% sensitive and 96% specific to this abnormal morphology.31 The mere flatness of the trochlea is not reason itself for a trochleoplasty, but rather the presence of a supratrochlear spur that can be removed as part of the deepening trochleoplasty.
Figure 3.
Trochlear dysplasia classification according to D. Dejour. In Type A, the crossing sign is present. Type B features include the crossing sign and trochlear spur. In Type C there is a crossing sign and the double-contour sign. Type D combines the crossing sign, supratrochlear spur and double-contour sign (with permission of Springer: Dejour D, Saggin P. The sulcus deepening trochleoplasty-the Lyon's procedure. Int Orthop 2010;34:313 Figure 2)
Figure 4.
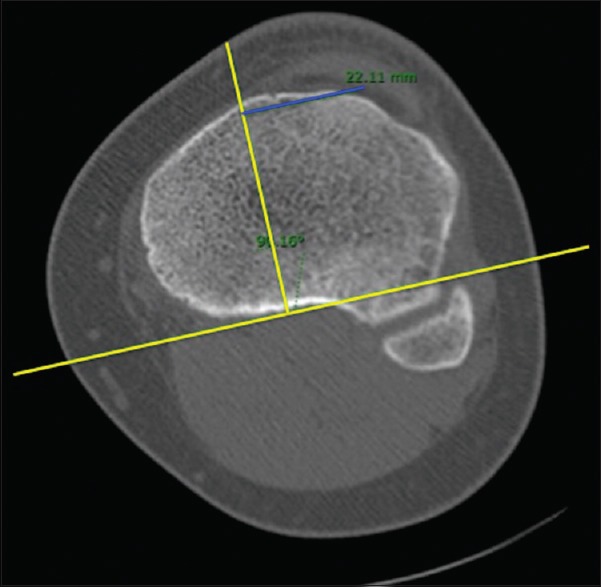
Axial computed tomography scan image left knee showing the tibial tubercle-trochlear groove has been measured at 22.11. This is measured by a perpendicular line drawn from the posterior femoral condylar axis through the bisecting point of the trochlear groove. This line is then superimposed onto the axial image of the midpoint of the tibial tubercle. The line drawn perpendicular to this trochlear groove line to the bisecting point of the tibial tubercle represents the tibial tubercle-trochlear groove distance
Figure 5.
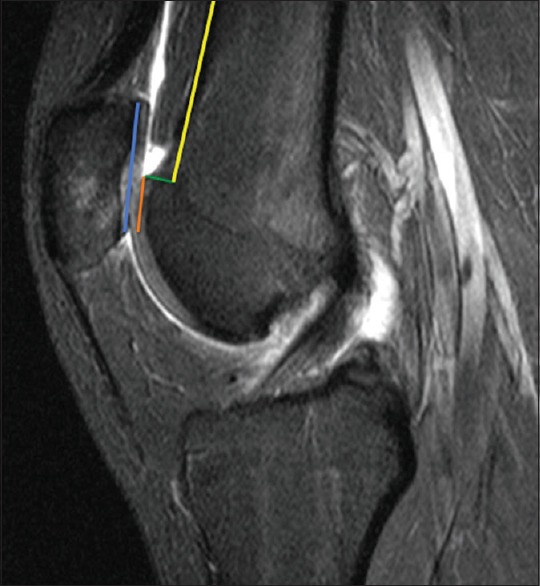
Sagittal magnetic resonance imaging T2W image measures the patellar trochlear index at 40%. The blue line corresponds to the superior to inferior most patellar articular cartilage. A right angle to that inferior most patellar cartilage is used to then measure a parallel line marking the length of corresponding trochlear cartilage to its superior-most extent. Patellar trochlear index = Orange/Blue ×100%. Furthermore, the yellow line marks the anterior femoral cortex and the supratrochlear spur is measured by the green line, which in this case is 6 mm in height
Nonoperative Management
In many instances, initial patellar dislocation events are managed conservatively; allowing for an effusion to resolve, reconditioning the VMO and allowing the adequate return of range of motion and function without recurrence.13,32 There are studies that report the positive role of VMO reconditioning.33 Furthermore, patellar taping and stabilization braces have been used to moderate effect to decrease the patients subjective feeling of patellar instability.34,35,36,37 For many, the nonoperative management will fail resulting in recurrent subjective patellar apprehension, which many times is indicative of residual micro-instability with subluxations without frank dislocations.4,33 In these instances of failed conservative management, the above listed further work up with diagnostic imaging is required as is a discussion regarding operative interventions.
Operative Management
Once an adequate history and physical examination, diagnostic imaging has been obtained, and an operative intervention is indicated, then there is a myriad of potential surgical procedures to aid in correcting the underlying pathology [Tables 1 and 2]. While an MPFL reconstruction, trochleoplasty and TTO are the more common procedures performed to address patellar instability, it is important to remember that in the setting of severe bony morphologic variances of genu valgum or femoral anteversion, distal femoral osteotomies, and derotational osteotomies can be indicated and effective procedures. Hemiepiphysiodesis has been successful at reducing patellar instability in the setting of severe genu valgum in the skeletally immature patient.38 Combined distal femoral opening wedge osteotomy procedures in skeletally mature individuals with genu valgum have been successful at improving not only the overall coronal limb alignment and objective outcomes measures but also limiting any further patellar dislocations.39 When indicated in patients with >25° of femoral anteversion and recurrent patellar dislocations, combined supracondylar distal femoral derotation osteotomies and an MPFL reconstruction have encouraging short-term results of statistically significant improvements in International Knee Documentation Committee (IKDC) outcomes and visual analog scale scores without further patellar dislocation.40
Table 1.
Acute patellar dislocation treatment algorithm
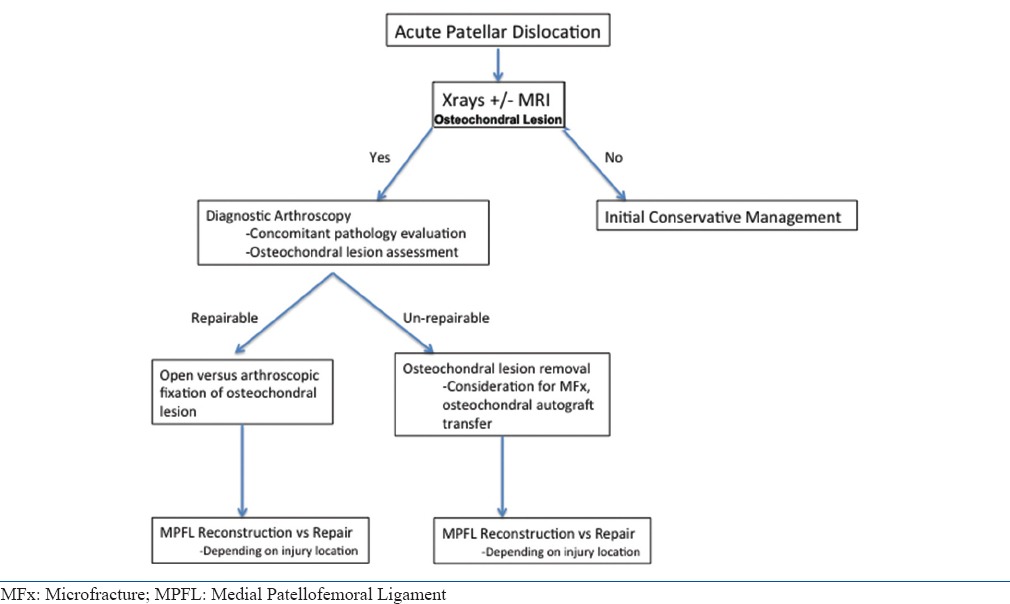
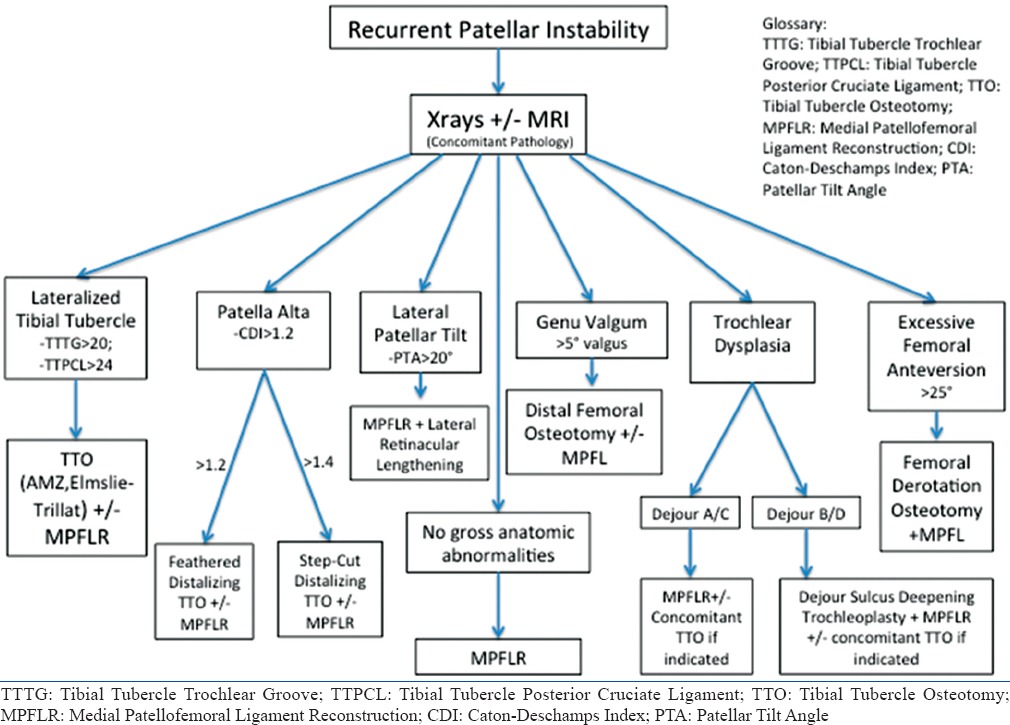
Table 2.
Recurrent patellar instability treatment algorithm
Medial patellofemoral ligament reconstruction
Today, the main stay of proximal soft tissue stabilization procedures is the MPFL reconstruction, it dramatically reduces subjective instability and frank dislocations.41,42,43,44,45,46 While this is a powerful surgical procedure at recreating the medial soft tissue check rein, it is vital to ensure that the remaining bony anatomy that contributes to patellar instability is identified and addressed in a satisfactory manner to maximize a good outcome. A very limited role exists for MPFL repair, namely in the setting of a sleeve avulsion off the medial patella in more adolescent patients, given the reported high rates of recurrent instability.33,47 Studies have revealed that the MPFL many times is damaged at multiple locations along its length and so it can be difficult to visualize exactly where the MPFL is torn, either by imaging or at surgery, which can lead to a failed repair.11,48,49 While stiffness is possible after MPFL repairs given the advancement of soft tissue during attempted repairs, the more likely complication from this procedure is recurrent patellar dislocations. This highlights not only the difficulty in determining where the native MPFL has been damaged but also the literature reporting that many times there is no difference in outcomes between primary repair and nonoperative treatment measures as it pertains to recurrent patellar instability.50,51
The indications for an isolated MPFL reconstruction are a normal TTTG (20 mm or less); a normal or Dejour Type A trochlea, a CDI measurement of <1.2 indicating no patella alta, and a patellar tilt measurement of <20°.28,52
There are many graft selection choices among autograft and allografts; without clear evidence supporting one over the other. Hamstring tendons, either gracilis or semitendinosus, are the most commonly used in a two-tailed configuration. In young patients with symptomatic patellar instability and wide-open physes, it might be worthwhile to consider a medial quadriceps turndown as local autograft fixed to suture anchors so as to limit the femoral bone tunnel routinely used in an adult MPFL reconstruction. In an adult MPFL reconstruction, there are many ways to fixate the graft to the patella, with studies reporting conflicting evidence as to the superiority of bone tunnels to suture anchors to interference screws; however, all of these means of fixation do approach or exceed the load to failure of the native MPFL.53,54,55
Critical to the success of the procedure is the proper positioning of the graft on the femur to restore the anatomy. While there are numerous radiographic measurements that can be used intraoperatively, like the distal femoral percentage measurements described by Stephen et al., it is Schöttle et al.'s point that is routinely referenced.8,56 Schöttle et al.'s point is a useful intraoperative radiographic location, which reproducibly places the femoral tunnel within a 5 mm isometric point for femoral fixation during MPFL reconstruction [Figure 6].56,57,58,59 There is no definitive guidance as to what knee flexion angle to fix the graft; however, there is evidence to support that fixation beyond 60° of flexion will exacerbate any malpositioned femoral tunnel placement.60 Furthermore, a malpositioned femoral tunnel will create a grossly anisometric graft, with placement too far proximal resulting in a graft that is tight in flexion and placement too far distal resulting in a graft that is loose as the knee is flexed.61 Finally, when tensioning the graft, it is not the same as tensioning an anterior cruciate ligament or other ligament reconstructions as over tensioning is a common technical mistake which can result in loss of flexion, over medialization of the patella, and potentially resultant painful chondrosis. Biomechanical studies show that only 2 N, or 0.5 lbs, of force is required to adequately stabilize the patella and restore normal contact pressures when the graft is fixed at a satisfactory femoral insertion site and with the knee in 30° of flexion.62,63 If not closely monitored during the procedure, all of these technical factors can jeopardize the graft and compromise the long term outcome.
Figure 6.
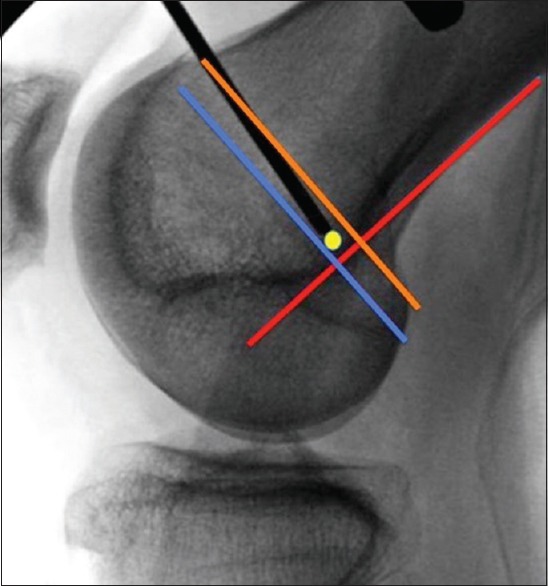
A perfect intraoperative C-arm lateral image of a left knee with complete posterior femoral condyle overlap. Schöttle's point is detailed as a yellow dot, noted as 1 mm anterior to the posterior cortex extension line (red line), 2.5 mm distal to the posterior origin of the medial femoral condyle (orange line), and proximal to the level of the posterior point of Blumensaat's line (blue line)
Outcomes and complications
When following the above indications, an isolated MPFL reconstruction is a powerful surgical technique, which can dramatically reduce recurrent dislocations. Kita et al. reported only a 4.5% re-dislocation rate, whereas Hinterwimmer et al. showed 95% excellent functional outcome scores in patients treated with MPFL reconstruction.64,65 As the surgical technique has evolved, so too has the surgical results, which suggest that MPFL reconstruction is far superior to an isolated medial imbrication or MPFL repair.
In the single largest retrospective case series to date on isolated MPFL reconstructions, Schiphouwer et al. have examined 192 knees and reported on the complication rate. In their study, using two 4.5 mm patellar tunnels drilled from the medial patellar border exiting on the anterior patellar cortex, an overall complication rate of 20.3% was reported, of which 14.1% were considered major.66 Seven patella fractures were reported with this technique at a rate of 3.6%. To avoid this complication for patellar fixation, it is recommended to drill tunnels <4.5 mm in size, to not drill the tunnels transversely across the patella, or to use suture anchors or interference screws. Continued patellar instability can persist with objective findings for continued instability reported at 3%–5% and subjective feelings of apprehension between 8% and 24%.67
Trochleoplasty
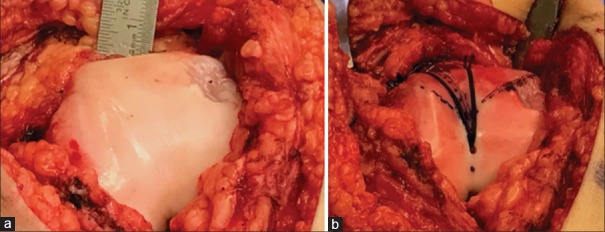
A descriptive classification scheme has been developed for the trochlea's morphologic variants [Figure 3]. For patients with Type A and C trochlea variants, there is no gross supratrochlear spur, and so a deepening trochleoplasty is problematic and generally not indicated. Type B and D variants routinely can be considered indications for this sulcus deepening trochleoplasty given the presence of a spur projecting from the anterior femoral cortex. For patients with this trochlear variant, it can be one of many reasons, as described above, for their initial and recurrent patellar instability. This supratrochlear spur can be a significant impediment that “kicks” the patella laterally and prevents the patella from engaging the more distal trochlear groove. For a normal knee without dysplasia, the deepest part of the trochlear groove merges with the anterior femoral cortex at the same level. By adequately removing this spur, creating a flush transition from trochlea to anterior femoral cortex, lateralizing and deepening the trochlear groove; this can not only reshape the trochlea to satisfactorily accept the patella throughout its arc of motion, but also subtly influence the alignment vector by creating the sulcus slightly more lateral than where it was natively placed. This effectively decreases the TTTG. In order for this procedure to be successful, the supratrochlear spur needs to be at least 5–6 mm in height.31,68 During the creation of the new trochlear sulcus, great care should be taken when developing the osteochondral trochlear shingles to preserve a 2–3 mm shell of subchondral bone for chondral viability. Suture anchors with absorbable suture pulled tightly across are used to provide reduction and stable fixation of the shingles in the new shape [Figure 7]. Open physes or patellofemoral arthrosis are contraindications to performing the procedure, with the latter potentially resulting in cracking the shell in random directions secondary to the more sclerotic bone.
Figure 7.
Intraoperative photos of left knee. (a) Pretrochleoplasty: Dejour B trochlea with nonexistent sulcus angle and supratrochlear spur. (b) Posttrochleoplasty: Note the medial/lateral shingle creation, with the reduction maintained by suture anchors loaded with #2 absorbable suture, and the restored sulcus with slight lateralization of the trochlear groove
Outcomes and complications
Biomechanical studies have clearly shown how trochlear dysplasia negatively affects patellar stability as well as how the use of a trochleoplasty procedure can adequately reduce patellar instability and normalize the patellofemoral kinematics.69,70 This gives hope to surgeons that by limiting further patellofemoral instability, this could delay or even limit the development of patellofemoral arthritis. When reviewing the available literature on trochleoplasty, the outcomes and results are varied given the heterogeneity of the designed studies, with differing etiologies of the patellar instability as well as differing surgical techniques and ancillary procedures performed at the time of the trochleoplasty.71,72,73,74 Ntagiopoulos et al. reviewed the midterm results at a mean of 7 years for this operation and have reported on the satisfactory stabilization of the patella with statistically significant improvements in functional IKDC and Kujala scores.74
The most frequently reported complication associated with trochleoplasty procedures is arthrofibrosis and resultant stiffness, many times that results in an additional surgery for lysis of adhesions (LOA) and manipulation under anesthesia (MUA).72,75 While this had been reported to be as high as 46%, more recent literature states a 0%–20% prevalence in association with trochleoplasty procedures, which is in keeping with our unpublished results.68,74,76 Return of function with satisfactory results has been achieved with LOA/MUA.68,75,77 Additional complications specific to trochleoplasties include trochlear shingle fracture line propagation, most commonly in the setting of dense/brittle subchondral bone associated with existing patellofemoral arthritis. The transition of the shingle to the intact bone more distally can settle over time, leading to a slight step off from subchondral collapse. This can be mitigated by placing small pieces of bone graft into the subchondral space laterally and medially at the edges of the corticocancellous region, helping to provide a tapered transition with adequate shingle reduction and maintenance with suture anchors and absorbable suture, which provides satisfactory healing.74,78,79
Tibial tubercle osteotomy
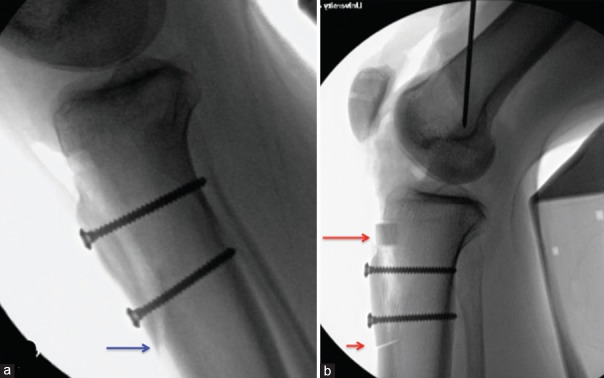
In addition to using an anteromedialization (AMZ) TTO for distal and lateral patellar facet chondrosis, as it was originally described for, it is routinely performed in the setting of patellar instability when there are findings of an elevated TTTG >20 mm, elevated TT-PCL, and patella alta with CDI >1.2. While direct medial, Elmslie–Trillat, and direct anteriorization, Maquet, osteotomies can be utilized, a more common TTO is the AMZ TTO, or Fulkerson osteotomy. Routinely this is determined by the TTTG present, with the goal of normalizing the TTTG to roughly 10 mm. When concomitant procedures of a sulcus deepening trochleoplasty are to be performed with an AMZ, significantly elevated TTTG distances of 25 or greater can be adequately addressed by not only anteromedializing the TT but also by slightly lateralizing the newly created trochlear sulcus. Classically, a CDI of >1.2 has been defined as patella alta. More recent criteria, which also can be helpful in determining whether to distalize the tubercle shingle, are the PTI and SPE, should they be <0.32 and 0.45, respectively.28,29 These measurements provide guidance to the patella's articulation in full extension/early flexion, which could be contributing to the lack of early engagement. We routinely use a CDI >1.2 and a J sign on examination to determine the necessity of a distalization TTO; however, this is routinely done by a feathered shingle to slide it up to 7 mm distally. When the CDI >1.4 and the need to distalize the shingle >1 cm exists, then a step-cut TTO is performed, but this does carry the risk of delayed healing [Figure 8]. By adequately distalizing the shingle, not only does this correct the patella alta but also can allow for earlier engagement with articulation. This could help address any subtle trochlear dysplasia present, Type C, where lateral trochlear ridge hyper-convexity could be causing a very slight “kick” and influencing its tracking, but not be fully indicated for a sulcus deepening trochleoplasty given the lack of a definitive spur measuring 6 mm.
Figure 8.
Intraoperative lateral C-arm images of a left knee: (a) Note the distalized feathered shingle (blue arrow) used to address mild patella alta. (b) The step-cut is performed to address severe patella alta (short red arrow reveals the distalization of the osteotomy shingle and the long red arrow shows the bone segment that was cut distally and transferred proximally as autogenous bone grafting)
Outcomes and complications
The outcomes for TTO procedures are generally quite good, with decreases in patellar dislocations and good to excellent Lysholm scores reported in 73% of patients when performed for patellar instability.80,81 We are in agreement with Krych et al. in their reporting that the addition of a TTO to a MPFL reconstruction can not only delay a patient's return to high-level competitive athletics but also the overall return to sport (RTS) rate.82 It is, however, our experience that an isolated MPFL reconstruction and a combined procedure with TTO roughly takes 3 and 6 months, respectively, for a RTS and this is ultimately determined once satisfactory strength and function have returned. Although, Feller et al. revealed that only 57% of patients RTS after a combined procedure.43 While a TTO is a reliable procedure and should be considered when indicated for reducing patellar instability, this literature provides further guidance to education and set expectations for all patient types.
A recent systematic review assessing the complications associated with TTOs, including concomitant soft tissue stabilization procedures, performed for patellar instability reported a 4.6% overall complication rate, with painful hardware resulting in hardware removal in 36.7% of cases.83 In addition, increased overall complication rates were seen when osteotomy shingles were completely detached distally instead of being “hinged.” Furthermore, nonunion rates and associated tibial fractures were reported at 0.8% and 1.0%, respectively, and are most at risk to occur with advancing weight bearing beyond 50% before the bone has adequately healed, or 6 weeks.83 Many times using either flat headed low profile screws, either 3.5 mm or 4.5 mm, and feathering the distal osteotomy cut can potentially help limit the above listed painful hardware, nonunion, and tibial shaft fracture complication rates.
Conclusion
It is imperative to provide an individualized treatment regimen based on critical evaluations of the patients plain radiographs and advanced imaging. In most instances, a MPFL reconstruction is performed with careful attention to a patient's TTTG, CDI and PTI/SPE, to help determine if and what type of TTO to provide, as well as the distances required to translate to normalize the values. Finally, increasing attention to trochlear dysplasia and its multiple variants can help guide a surgeon for when to consider the addition of a sulcus deepening trochleoplasty and restore more normal patellofemoral articulation by satisfactorily removing the supratrochlear spur, and to also help address an elevated TTTG.
Financial support and sponsorship
Nil.
Conflicts of interest
Dr. Diduch is a consultant for Depuy Synthes and receives royalties from Smith and Nephew; however, for the purposes of this review article, there are no gross conflicts of interest.
References
- 1.Fithian DC, Paxton EW, Stone ML, Silva P, Davis DK, Elias DA, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32:1114–21. doi: 10.1177/0363546503260788. [DOI] [PubMed] [Google Scholar]
- 2.Arendt EA, Fithian DC, Cohen E. Current concepts of lateral patella dislocation. Clin Sports Med. 2002;21:499–519. doi: 10.1016/s0278-5919(02)00031-5. [DOI] [PubMed] [Google Scholar]
- 3.Atkin DM, Fithian DC, Marangi KS, Stone ML, Dobson BE, Mendelsohn C, et al. Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. Am J Sports Med. 2000;28:472–9. doi: 10.1177/03635465000280040601. [DOI] [PubMed] [Google Scholar]
- 4.Nietosvaara Y, Aalto K, Kallio PE. Acute patellar dislocation in children: Incidence and associated osteochondral fractures. J Pediatr Orthop. 1994;14:513–5. doi: 10.1097/01241398-199407000-00018. [DOI] [PubMed] [Google Scholar]
- 5.Elias DA, White LM, Fithian DC. Acute lateral patellar dislocation at MR imaging: Injury patterns of medial patellar soft-tissue restraints and osteochondral injuries of the inferomedial patella. Radiology. 2002;225:736–43. doi: 10.1148/radiol.2253011578. [DOI] [PubMed] [Google Scholar]
- 6.Waterman BR, Belmont PJ, Jr, Owens BD. Patellar dislocation in the United States: Role of sex, age, race, and athletic participation. J Knee Surg. 2012;25:51–7. doi: 10.1055/s-0031-1286199. [DOI] [PubMed] [Google Scholar]
- 7.LaPrade RF, Engebretsen AH, Ly TV, Johansen S, Wentorf FA, Engebretsen L, et al. The anatomy of the medial part of the knee. J Bone Joint Surg Am. 2007;89:2000–10. doi: 10.2106/JBJS.F.01176. [DOI] [PubMed] [Google Scholar]
- 8.Stephen JM, Lumpaopong P, Deehan DJ, Kader D, Amis AA. The medial patellofemoral ligament: Location of femoral attachment and length change patterns resulting from anatomic and nonanatomic attachments. Am J Sports Med. 2012;40:1871–9. doi: 10.1177/0363546512449998. [DOI] [PubMed] [Google Scholar]
- 9.Amis AA, Firer P, Mountney J, Senavongse W, Thomas NP. Anatomy and biomechanics of the medial patellofemoral ligament. Knee. 2003;10:215–20. doi: 10.1016/s0968-0160(03)00006-1. [DOI] [PubMed] [Google Scholar]
- 10.Philippot R, Boyer B, Testa R, Farizon F, Moyen B. The role of the medial ligamentous structures on patellar tracking during knee flexion. Knee Surg Sports Traumatol Arthrosc. 2012;20:331–6. doi: 10.1007/s00167-011-1598-6. [DOI] [PubMed] [Google Scholar]
- 11.Weber-Spickschen TS, Spang J, Kohn L, Imhoff AB, Schottle PB. The relationship between trochlear dysplasia and medial patellofemoral ligament rupture location after patellar dislocation: An MRI evaluation. Knee. 2011;18:185–8. doi: 10.1016/j.knee.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 12.Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: An anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2:19–26. doi: 10.1007/BF01552649. [DOI] [PubMed] [Google Scholar]
- 13.Lewallen L, McIntosh A, Dahm D. First-time patellofemoral dislocation: Risk factors for recurrent instability. J Knee Surg. 2015;28:303–9. doi: 10.1055/s-0034-1398373. [DOI] [PubMed] [Google Scholar]
- 14.Steensen RN, Bentley JC, Trinh TQ, Backes JR, Wiltfong RE. The prevalence and combined prevalences of anatomic factors associated with recurrent patellar dislocation: A magnetic resonance imaging study. Am J Sports Med. 2015;43:921–7. doi: 10.1177/0363546514563904. [DOI] [PubMed] [Google Scholar]
- 15.Ahmad CS, McCarthy M, Gomez JA, Shubin Stein BE. The moving patellar apprehension test for lateral patellar instability. Am J Sports Med. 2009;37:791–6. doi: 10.1177/0363546508328113. [DOI] [PubMed] [Google Scholar]
- 16.Sallay PI, Poggi J, Speer KP, Garrett WE. Acute dislocation of the patella. A correlative pathoanatomic study. Am J Sports Med. 1996;24:52–60. doi: 10.1177/036354659602400110. [DOI] [PubMed] [Google Scholar]
- 17.Beighton P, De Paepe A, Steinmann B, Tsipouras P, Wenstrup RJ. Ehlers-danlos syndromes: Revised nosology, villefranche, 1997. Ehlers-danlos national foundation (USA) and Ehlers-Danlos Support Group (UK) Am J Med Genet. 1998;77:31–7. doi: 10.1002/(sici)1096-8628(19980428)77:1<31::aid-ajmg8>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 18.Grahame R, Bird HA, Child A. The revised (Brighton 1998) criteria for the diagnosis of benign joint hypermobility syndrome (BJHS) J Rheumatol. 2000;27:1777–9. [PubMed] [Google Scholar]
- 19.Caton J, Deschamps G, Chambat P, Lerat JL, Dejour H. Patella infera-apropos of 128 cases. Rev Chir Orthop Reparatrice Appar Mot. 1982;68:317–25. [PubMed] [Google Scholar]
- 20.Insall J, Salvati E. Patella position in the normal knee joint. Radiology. 1971;101:101–4. doi: 10.1148/101.1.101. [DOI] [PubMed] [Google Scholar]
- 21.Barnett AJ, Prentice M, Mandalia V, Wakeley CJ, Eldridge JD. Patellar height measurement in trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc. 2009;17:1412–5. doi: 10.1007/s00167-009-0801-5. [DOI] [PubMed] [Google Scholar]
- 22.Dejour D, Le Coultre B. Osteotomies in patello-femoral instabilities. Sports Med Arthrosc. 2007;15:39–46. doi: 10.1097/JSA.0b013e31803035ae. [DOI] [PubMed] [Google Scholar]
- 23.Seitlinger G, Scheurecker G, Högler R, Labey L, Innocenti B, Hofmann S, et al. Tibial tubercle-posterior cruciate ligament distance: A new measurement to define the position of the tibial tubercle in patients with patellar dislocation. Am J Sports Med. 2012;40:1119–25. doi: 10.1177/0363546512438762. [DOI] [PubMed] [Google Scholar]
- 24.Heidenreich MJ, Camp CL, Dahm DL, Stuart MJ, Levy BA, Krych AJ, et al. The contribution of the tibial tubercle to patellar instability: Analysis of tibial tubercle-trochlear groove (TT-TG) and tibial tubercle-posterior cruciate ligament (TT-PCL) distances. Knee Surg Sports Traumatol Arthrosc. 2015 doi: 10.1007/s00167-015-3715-4. [Epub ahead of print] DOI: 10.1007/s00167-015-3715-4. [DOI] [PubMed] [Google Scholar]
- 25.Camp CL, Heidenreich MJ, Dahm DL, Stuart MJ, Levy BA, Krych AJ, et al. Individualizing the tibial tubercle-trochlear groove distance: Patellar instability ratios that predict recurrent instability. Am J Sports Med. 2016;44:393–9. doi: 10.1177/0363546515602483. [DOI] [PubMed] [Google Scholar]
- 26.Camp CL, Stuart MJ, Krych AJ, Levy BA, Bond JR, Collins MS, et al. CT and MRI measurements of tibial tubercle-trochlear groove distances are not equivalent in patients with patellar instability. Am J Sports Med. 2013;41:1835–40. doi: 10.1177/0363546513484895. [DOI] [PubMed] [Google Scholar]
- 27.Anley CM, Morris GV, Saithna A, James SL, Snow M. Defining the role of the tibial tubercle-trochlear groove and tibial tubercle-posterior cruciate ligament distances in the work-up of patients with patellofemoral disorders. Am J Sports Med. 2015;43:1348–53. doi: 10.1177/0363546515576128. [DOI] [PubMed] [Google Scholar]
- 28.Biedert RM, Albrecht S. The patellotrochlear index: A new index for assessing patellar height. Knee Surg Sports Traumatol Arthrosc. 2006;14:707–12. doi: 10.1007/s00167-005-0015-4. [DOI] [PubMed] [Google Scholar]
- 29.Dejour D, Ferrua P, Ntagiopoulos PG, Radier C, Hulet C, Rémy F, et al. The introduction of a new MRI index to evaluate sagittal patellofemoral engagement. Orthop Traumatol Surg Res. 2013;99:S391–8. doi: 10.1016/j.otsr.2013.10.008. [DOI] [PubMed] [Google Scholar]
- 30.Ali SA, Helmer R, Terk MR. Patella alta: Lack of correlation between patellotrochlear cartilage congruence and commonly used patellar height ratios. AJR Am J Roentgenol. 2009;193:1361–6. doi: 10.2214/AJR.09.2729. [DOI] [PubMed] [Google Scholar]
- 31.Pfirrmann CW, Zanetti M, Romero J, Hodler J. Femoral trochlear dysplasia: MR findings. Radiology. 2000;216:858–64. doi: 10.1148/radiology.216.3.r00se38858. [DOI] [PubMed] [Google Scholar]
- 32.Lewallen LW, McIntosh AL, Dahm DL. Predictors of recurrent instability after acute patellofemoral dislocation in pediatric and adolescent patients. Am J Sports Med. 2013;41:575–81. doi: 10.1177/0363546512472873. [DOI] [PubMed] [Google Scholar]
- 33.Palmu S, Kallio PE, Donell ST, Helenius I, Nietosvaara Y. Acute patellar dislocation in children and adolescents: A randomized clinical trial. J Bone Joint Surg Am. 2008;90:463–70. doi: 10.2106/JBJS.G.00072. [DOI] [PubMed] [Google Scholar]
- 34.McConnell J. Rehabilitation and nonoperative treatment of patellar instability. Sports Med Arthrosc. 2007;15:95–104. doi: 10.1097/JSA.0b013e318054e35c. [DOI] [PubMed] [Google Scholar]
- 35.Lee SE, Cho SH. The effect of McConnell taping on vastus medialis and lateralis activity during squatting in adults with patellofemoral pain syndrome. J Exerc Rehabil. 2013;9:326–30. doi: 10.12965/jer.130018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Colvin AC, West RV. Patellar instability. J Bone Joint Surg Am. 2008;90:2751–62. doi: 10.2106/JBJS.H.00211. [DOI] [PubMed] [Google Scholar]
- 37.Khormaee S, Kramer DE, Yen YM, Heyworth BE. Evaluation and management of patellar instability in pediatric and adolescent athletes. Sports Health. 2015;7:115–23. doi: 10.1177/1941738114543073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kearney SP, Mosca VS. Selective hemiepiphyseodesis for patellar instability with associated genu valgum. J Orthop. 2015;12:17–22. doi: 10.1016/j.jor.2015.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Swarup I, Elattar O, Rozbruch SR. Patellar instability treated with distal femoral osteotomy. Knee. 2017;24:608–14. doi: 10.1016/j.knee.2017.02.004. [DOI] [PubMed] [Google Scholar]
- 40.Nelitz M, Dreyhaupt J, Williams SR, Dornacher D. Combined supracondylar femoral derotation osteotomy and patellofemoral ligament reconstruction for recurrent patellar dislocation and severe femoral anteversion syndrome: Surgical technique and clinical outcome. Int Orthop. 2015;39:2355–62. doi: 10.1007/s00264-015-2859-7. [DOI] [PubMed] [Google Scholar]
- 41.Astur DC, Gouveia GB, Borges JH, Astur N, Arliani GG, Kaleka CC, et al. Medial patellofemoral ligament reconstruction: A longitudinal study comparison of 2 techniques with 2 and 5-years followup. Open Orthop J. 2015;9:198–203. doi: 10.2174/1874325001509010198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Csintalan RP, Latt LD, Fornalski S, Raiszadeh K, Inacio MC, Fithian DC, et al. Medial patellofemoral ligament (MPFL) reconstruction for the treatment of patellofemoral instability. J Knee Surg. 2014;27:139–46. doi: 10.1055/s-0033-1360652. [DOI] [PubMed] [Google Scholar]
- 43.Feller JA, Richmond AK, Wasiak J. Medial patellofemoral ligament reconstruction as an isolated or combined procedure for recurrent patellar instability. Knee Surg Sports Traumatol Arthrosc. 2014;22:2470–6. doi: 10.1007/s00167-014-3132-0. [DOI] [PubMed] [Google Scholar]
- 44.Matthews JJ, Schranz P. Reconstruction of the medial patellofemoral ligament using a longitudinal patellar tunnel technique. Int Orthop. 2010;34:1321–5. doi: 10.1007/s00264-009-0918-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Panagopoulos A, van Niekerk L, Triantafillopoulos IK. MPFL reconstruction for recurrent patella dislocation: A new surgical technique and review of the literature. Int J Sports Med. 2008;29:359–65. doi: 10.1055/s-2007-965360. [DOI] [PubMed] [Google Scholar]
- 46.Panni AS, Alam M, Cerciello S, Vasso M, Maffulli N. Medial patellofemoral ligament reconstruction with a divergent patellar transverse 2-tunnel technique. Am J Sports Med. 2011;39:2647–55. doi: 10.1177/0363546511420079. [DOI] [PubMed] [Google Scholar]
- 47.Matic GT, Magnussen RA, Kolovich GP, Flanigan DC. Return to activity after medial patellofemoral ligament repair or reconstruction. Arthroscopy. 2014;30:1018–25. doi: 10.1016/j.arthro.2014.02.044. [DOI] [PubMed] [Google Scholar]
- 48.Sillanpää PJ, Peltola E, Mattila VM, Kiuru M, Visuri T, Pihlajamäki H, et al. Femoral avulsion of the medial patellofemoral ligament after primary traumatic patellar dislocation predicts subsequent instability in men: A mean 7-year nonoperative followup study. Am J Sports Med. 2009;37:1513–21. doi: 10.1177/0363546509333010. [DOI] [PubMed] [Google Scholar]
- 49.Nomura E. Classification of lesions of the medial patello-femoral ligament in patellar dislocation. Int Orthop. 1999;23:260–3. doi: 10.1007/s002640050366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Camp CL, Krych AJ, Dahm DL, Levy BA, Stuart MJ. Medial patellofemoral ligament repair for recurrent patellar dislocation. Am J Sports Med. 2010;38:2248–54. doi: 10.1177/0363546510376230. [DOI] [PubMed] [Google Scholar]
- 51.Christiansen SE, Jakobsen BW, Lund B, Lind M. Isolated repair of the medial patellofemoral ligament in primary dislocation of the patella: A prospective randomized study. Arthroscopy. 2008;24:881–7. doi: 10.1016/j.arthro.2008.03.012. [DOI] [PubMed] [Google Scholar]
- 52.Hopper GP, Leach WJ, Rooney BP, Walker CR, Blyth MJ. Does degree of trochlear dysplasia and position of femoral tunnel influence outcome after medial patellofemoral ligament reconstruction? Am J Sports Med. 2014;42:716–22. doi: 10.1177/0363546513518413. [DOI] [PubMed] [Google Scholar]
- 53.Mountney J, Senavongse W, Amis AA, Thomas NP. Tensile strength of the medial patellofemoral ligament before and after repair or reconstruction. J Bone Joint Surg Br. 2005;87:36–40. [PubMed] [Google Scholar]
- 54.Russo F, Doan J, Chase DC, Farnsworth CL, Pennock AT. Medial patellofemoral ligament reconstruction: Fixation technique biomechanics. J Knee Surg. 2016;29:303–9. doi: 10.1055/s-0035-1554922. [DOI] [PubMed] [Google Scholar]
- 55.Russ SD, Tompkins M, Nuckley D, Macalena J. Biomechanical comparison of patellar fixation techniques in medial patellofemoral ligament reconstruction. Am J Sports Med. 2015;43:195–9. doi: 10.1177/0363546514550992. [DOI] [PubMed] [Google Scholar]
- 56.Schöttle PB, Schmeling A, Rosenstiel N, Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35:801–4. doi: 10.1177/0363546506296415. [DOI] [PubMed] [Google Scholar]
- 57.Redfern J, Kamath G, Burks R. Anatomical confirmation of the use of radiographic landmarks in medial patellofemoral ligament reconstruction. Am J Sports Med. 2010;38:293–7. doi: 10.1177/0363546509347602. [DOI] [PubMed] [Google Scholar]
- 58.Jaecker V, Brozat B, Banerjee M, Otchwemah R, Bouillon B, Shafizadeh S, et al. Fluoroscopic control allows for precise tunnel positioning in MPFL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2015 doi: 10.1007/s00167-015-3613-9. [Epub ahead of print] DOI: 10.1007/s00167-015-3613-9. [DOI] [PubMed] [Google Scholar]
- 59.Smirk C, Morris H. The anatomy and reconstruction of the medial patellofemoral ligament. Knee. 2003;10:221–7. doi: 10.1016/s0968-0160(03)00038-3. [DOI] [PubMed] [Google Scholar]
- 60.Burrus MT, Werner BC, Cancienne JM, Gwathmey FW, Diduch DR. MPFL graft fixation in low degrees of knee flexion minimizes errors made in the femoral location. Knee Surg Sports Traumatol Arthrosc Apr. 2016 Apr 16; doi: 10.1007/s00167-016-4111-4. [Epub ahead of print] DOI: 10.1007/s00167-016-4111-4. [DOI] [PubMed] [Google Scholar]
- 61.Burrus MT, Werner BC, Conte EJ, Diduch DR. Troubleshooting the femoral attachment during medial patellofemoral ligament reconstruction: Location, location, location. Orthop J Sports Med. 2015;3:2325967115569198. doi: 10.1177/2325967115569198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Stephen JM, Kaider D, Lumpaopong P, Deehan DJ, Amis AA. The effect of femoral tunnel position and graft tension on patellar contact mechanics and kinematics after medial patellofemoral ligament reconstruction. Am J Sports Med. 2014;42:364–72. doi: 10.1177/0363546513509230. [DOI] [PubMed] [Google Scholar]
- 63.Stephen JM, Kittl C, Williams A, Zaffagnini S, Marcheggiani Muccioli GM, Fink C, et al. Effect of medial patellofemoral ligament reconstruction method on patellofemoral contact pressures and kinematics. Am J Sports Med. 2016;44:1186–94. doi: 10.1177/0363546516631736. [DOI] [PubMed] [Google Scholar]
- 64.Hinterwimmer S, Imhoff AB, Minzlaff P, Saier T, Rosenstiel N, Hawe W, et al. Anatomical two-bundle medial patellofemoral ligament reconstruction with hardware-free patellar graft fixation: Technical note and preliminary results. Knee Surg Sports Traumatol Arthrosc. 2013;21:2147–54. doi: 10.1007/s00167-013-2498-8. [DOI] [PubMed] [Google Scholar]
- 65.Kita K, Tanaka Y, Toritsuka Y, Amano H, Uchida R, Takao R, et al. Factors affecting the outcomes of double-bundle medial patellofemoral ligament reconstruction for recurrent patellar dislocations evaluated by multivariate analysis. Am J Sports Med. 2015;43:2988–96. doi: 10.1177/0363546515606102. [DOI] [PubMed] [Google Scholar]
- 66.Schiphouwer L, Rood A, Tigchelaar S, Koëter S. Complications of medial patellofemoral ligament reconstruction using two transverse patellar tunnels. Knee Surg Sports Traumatol Arthrosc. 2017;25:245–50. doi: 10.1007/s00167-016-4245-4. [DOI] [PubMed] [Google Scholar]
- 67.Shah JN, Howard JS, Flanigan DC, Brophy RH, Carey JL, Lattermann C, et al. A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2012;40:1916–23. doi: 10.1177/0363546512442330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Donell ST, Joseph G, Hing CB, Marshall TJ. Modified dejour trochleoplasty for severe dysplasia: Operative technique and early clinical results. Knee. 2006;13:266–73. doi: 10.1016/j.knee.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 69.Amis AA, Oguz C, Bull AM, Senavongse W, Dejour D. The effect of trochleoplasty on patellar stability and kinematics: A biomechanical study in vitro. J Bone Joint Surg Br. 2008;90:864–9. doi: 10.1302/0301-620X.90B7.20447. [DOI] [PubMed] [Google Scholar]
- 70.Van Haver A, De Roo K, De Beule M, Labey L, De Baets P, Dejour D, et al. The effect of trochlear dysplasia on patellofemoral biomechanics: A cadaveric study with simulated trochlear deformities. Am J Sports Med. 2015;43:1354–61. doi: 10.1177/0363546515572143. [DOI] [PubMed] [Google Scholar]
- 71.Song GY, Hong L, Zhang H, Zhang J, Li X, Li Y, et al. Trochleoplasty versus nontrochleoplasty procedures in treating patellar instability caused by severe trochlear dysplasia. Arthroscopy. 2014;30:523–32. doi: 10.1016/j.arthro.2014.01.011. [DOI] [PubMed] [Google Scholar]
- 72.McNamara I, Bua N, Smith TO, Ali K, Donell ST. Deepening trochleoplasty with a thick osteochondral flap for patellar instability: Clinical and functional outcomes at a mean 6-year followup. Am J Sports Med. 2015;43:2706–13. doi: 10.1177/0363546515597679. [DOI] [PubMed] [Google Scholar]
- 73.Testa EA, Camathias C, Amsler F, Henle P, Friederich NF, Hirschmann MT. Surgical treatment of patellofemoral instability using trochleoplasty or MPFL reconstruction: A systematic review. Knee Surg Sports Traumatol Arthrosc. 2015 doi: 10.1007/s00167-015-3698-1. [Epub ahead of print] DOI: 10.1007/s00167-015-3698-1. [DOI] [PubMed] [Google Scholar]
- 74.Ntagiopoulos PG, Byn P, Dejour D. Midterm results of comprehensive surgical reconstruction including sulcus-deepening trochleoplasty in recurrent patellar dislocations with high-grade trochlear dysplasia. Am J Sports Med. 2013;41:998–1004. doi: 10.1177/0363546513482302. [DOI] [PubMed] [Google Scholar]
- 75.Verdonk R, Jansegers E, Stuyts B. Trochleoplasty in dysplastic knee trochlea. Knee Surg Sports Traumatol Arthrosc. 2005;13:529–33. doi: 10.1007/s00167-004-0570-0. [DOI] [PubMed] [Google Scholar]
- 76.von Knoch F, Böhm T, Bürgi ML, von Knoch M, Bereiter H. Trochleaplasty for recurrent patellar dislocation in association with trochlear dysplasia. A 4- to 14-year followup study. J Bone Joint Surg Br. 2006;88:1331–5. doi: 10.1302/0301-620X.88B10.17834. [DOI] [PubMed] [Google Scholar]
- 77.Beaufils P, Thaunat M, Pujol N, Scheffler S, Rossi R, Carmont M, et al. Trochleoplasty in major trochlear dysplasia: Current concepts. Sports Med Arthrosc Rehabil Ther Technol. 2012;4:7. doi: 10.1186/1758-2555-4-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Burrus M, Carstensen S, Diduch DR. Trochleoplasty. In: Browne J, Owens B, editors. Operative Techniques: Knee Surgery. 2nd edition. Philadelphia, PA: Elsevier; 2017. pp. 315–21. [Google Scholar]
- 79.Burrus M, Tompkins M, Hinckel B, Diduch DR, Arendt EA. Repair and reconstruction of the medial patellofemoral ligament for treatment of lateral patellar dislocations: Surgical techniques and clinical results. In: Scott WN, editor. Insall and Scott: Surgery of the Knee. 6th ed. Philadelphia, PA: Elsevier; 2017. pp. 939–53. [Google Scholar]
- 80.Tjoumakaris FP, Forsythe B, Bradley JP. Patellofemoral instability in athletes: Treatment via modified fulkerson osteotomy and lateral release. Am J Sports Med. 2010;38:992–9. doi: 10.1177/0363546509357682. [DOI] [PubMed] [Google Scholar]
- 81.Pritsch T, Haim A, Arbel R, Snir N, Shasha N, Dekel S, et al. Tailored tibial tubercle transfer for patellofemoral malalignment: Analysis of clinical outcomes. Knee Surg Sports Traumatol Arthrosc. 2007;15:994–1002. doi: 10.1007/s00167-007-0325-9. [DOI] [PubMed] [Google Scholar]
- 82.Krych AJ, O’Malley MP, Johnson NR, Mohan R, Hewett TE, Stuart MJ, et al. Functional testing and return to sport following stabilization surgery for recurrent lateral patellar instability in competitive athletes. Knee Surg Sports Traumatol Arthrosc. 2016 doi: 10.1007/s00167-016-4409-2. [Epub ahead of print] doi: 10.1007/s00167-016-4409-2. [DOI] [PubMed] [Google Scholar]
- 83.Payne J, Rimmke N, Schmitt LC, Flanigan DC, Magnussen RA. The incidence of complications of tibial tubercle osteotomy: A systematic review. Arthroscopy. 2015;31:1819–25. doi: 10.1016/j.arthro.2015.03.028. [DOI] [PubMed] [Google Scholar]