Abstract
Subacromial impingement syndrome (SIS) is a very common cause of shoulder pain in the young adults. It can cause debilitating pain, dysfunction, and affects the activities of daily living. It represents a spectrum of pathology ranging from bursitis to rotator cuff tendinopathy which can ultimately lead to degenerative tear of the rotator cuff. Various theories and concepts have been described and it is still a matter of debate. However, most published studies suggest that both extrinsic and intrinsic factors have a role in the development of SIS. The management is controversial as both nonoperative and operative treatments have shown to provide good results. This article aims to provide a comprehensive current concepts review of the pathogenesis, etiologies, clinical diagnosis, appropriate use of investigations, and discussion on the management of SIS.
Keywords: Arthroscopy, coracoacromial, impingement, magnetic resonance imaging, shoulder
MeSH terms: Arthroscopy, rotator cuff, acromioclavicular joint, magnetic resonance imaging
Introduction
Subacromial impingement syndrome (SIS) is a clinical syndrome most often attributed to patients presenting with shoulder pain.1 SIS is a syndrome that encompasses a spectrum of subacromial pathologies ranging from bursitis, rotator cuff tendinosis, and partial tears leading up to full-thickness tear of the rotator cuff. Luime et al. estimated the prevalence of shoulder complaints to be in the region of 7%–34% and about 14.7 new cases/1000 patients/year seen in clinics.2 Of these, SIS is the most common reported diagnosis accounting for up to two-thirds of all shoulder pain.2
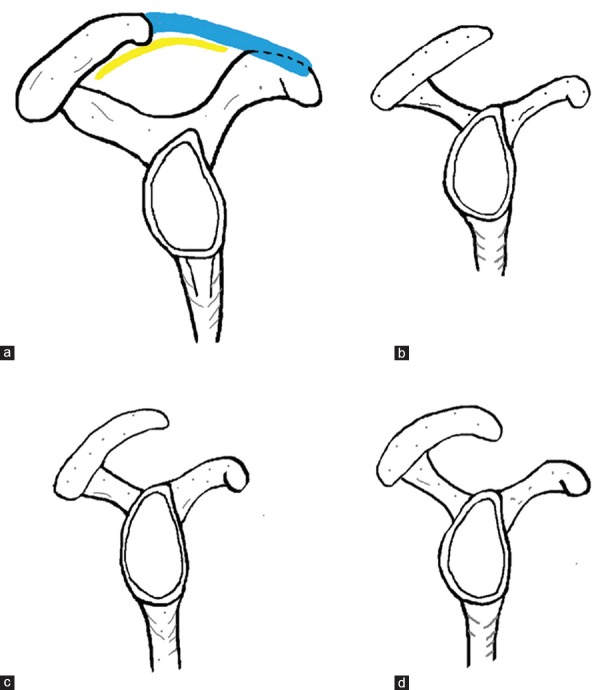
The subacromial space is boarded inferiorly by the humeral head and superiorly by the coracoacromial ligament (CAL), coracoid process, and undersurface of the anterior third of the acromion.3 These three structures form the coracoacromial arch [Figure 1a]. Radiologically, the average space between the acromion and the humeral head is between 10 and 15 mm.4 Structures in this space include the subacromial bursa, rotator cuff tendons, long head of biceps, and the CAL. Any changes due to trauma or degeneration of these structures can lead to an impingement syndrome.
Figure 1.
A line diagram of coracoacromial arch (CAL) showing coracoacromial ligament and arch (Normal) (b) Type 1 (Flat) acromion (c) Type 2 (curved) acromion (d) Type 3 (Hooked) acromion
Considering the prevalence of this syndrome, this article aims to discuss the historical aspects, theories behind the pathology of SIS, describe salient history and physical examination findings, analysis of the various investigations, and management of the pathologies encompassed by this syndrome.
Historical Aspects
When discussing about the current concepts, we feel that it is important to have the historical perspective of the condition to understand the evolution of management of the condition. The earliest available literature on shoulder pain is in French where Duplay talks about the “periarthrite” focusing on gleno-humeral disease.5 It is believed that he was probably talking about osteoarthritis or frozen shoulder. The first English literature comes from Codman's series in the early 20th century. He drew the attention to bursa and the rotator cuff tendons, although the condition was thought to be traumatic.6,7,8 Meyer, however, thought the condition to be due to “attrition” in which the rotator cuff tendon and biceps were caught between the acromion and humeral head.9,10
Theories: Extrinsic versus Intrinsic
According to Neer, the impingement process can be broken down into three distinct stages.11 Stage I of the process is defined as edema and hemorrhage of the subacromial bursa, often in patients under the age of 25 years. Stage II impingement is when irreversible changes have developed and are represented by tendinitis and fibrosis of the rotator cuff tendon, seen in patients between the age of 25 and 40 years. Stage III impingement is said to have occurred when there are chronic changes such as rotator cuff tears, common in patients over the age of 40 years.
Two major theories dominate the controversies surrounding the etiology of rotator cuff disease and its relationship with SIS.
Extrinsic compression
The extrinsic theory suggests an extratendinous cause for SIS. Several degenerative processes are thought to result in SIS. Tension of the CAL on its insertion point on the acromion has also been postulated to cause stress-induced spurs on the underside of the acromion, contributing to the syndrome.12 The CAL can also cause spur formation under the acromion according to Wolff's law of strain and can cause thickening and subsequently cause a potential reduction of the subacromial space. Variations in acromion morphology have also been associated with this theory. This was first reported in 1986 where three distinct shapes [Figure 1b-d] were identified; Type I was a flat acromion, Type II was curved, and Type III was hooked.13 Several early studies seemed to suggest a higher incidence of rotator cuff tears in patients with Type III acromion, but more recent studies have not been able to show a strong relationship between the two.14,15 Gill et al. went on to suggest that Type III acromion was more likely to be a degenerative phenomenon rather than a congenital variation.14 Osteophytes from osteoarthritis of the acromioclavicular joint can result in a reduction of the subacromial space.3
Neer and Marberry challenged early proponents of the extrinsic theory suggesting that the lateral acromion was the source of external impingement, and treatment with lateral or total acromionectomy was unnecessary and results in injury to the deltoid.16 His subsequent work on 100 cadavers then led to suggestions that spurs on the anterior aspect of the undersurface of the acromion was the source of external impingement.3
Once pain sets in, dysfunction of the rotator cuff musculature is thought to have occurred and this results in a vicious cycle of pain causing further dysfunction that in turn reduces the efficiency of the rotator cuff to depress the humeral head. The net effect of this is a reduced distance between the rotator cuff and the acromion.
Intrinsic degeneration
Several well-designed, prospective studies identified a pattern of increasing incidence of rotator cuff tear with advancing age while the incidence of acromial degeneration did not.17,18 Findings from these studies correlated well with the theory proposed by Lohr and Uhthoff's cadaveric study.19 In their study of 18 human cadavers, they identified an area of hypovascularity within the tendon of supraspinatus and in particular the articular surface of the tendon.
This area of hypovascularity degenerates with age and other comorbidities with associated vascular effects. Fibrotic changes to the underlying tendon reduce its tensile strength and the net effect is reduced ability of the tendon to prevent superior migration of the humerus.20 The net effect of this tendon degeneration is a thinning of tendon and reduction in subacromial space, and when chronic, may lead to acromial spurring secondary to abutment of the greater tuberosity on the acromion.
External versus Internal Impingement
The terms “external and internal impingement” are used to describe the underlying pathology leading to shoulder impingement syndrome. External (outlet) impingement refers to any variation in normal anatomy that results in the narrowing of the subacromial space. Internal or inlet impingement, as originally described by Walch et al. in 1992, refers to impingement secondary to repetitive minor trauma to the gleno-humeral joint, especially in the posteroinferior corner of the joint.21 Internal impingement occurs when the shoulder is abducted, externally rotated, and extended, such as the cocking phase of a throw. This results in the posteroinferior aspect of the labrum to impinge on the underside of the rotator cuff, and in isolation, is not a pathological process. However, when occurs chronically and repetitively, in throwing athletes and swimmers, it results in micro trauma and damage to both the articular surface of the rotator cuff and the labrum.22
Diagnosis
Accurate diagnosis of SIS is made by an accurate history, careful examination, and analysis of relevant investigations.
History
Patients with SIS can either present with acute pain, especially after a definite traumatic event, or an insidious history culminating in limitations of activities of daily living. Pain related to this syndrome is often described to be an anterolateral arm pain.23 Common exacerbating factors include lying on the affected shoulder, stretching, and reaching for overhead objects.
Clinical Examination
A routine examination of the shoulder joint as well as examination of the cervical spine should be carried out. The passive range of motion of the affected shoulder should be normal. Pain on abduction of the shoulder between 60° and 120° is referred to as the painful arc and may indicate the presence of SIS.
Index Tests
Numerous tests designed to elicit SIS have been described. However, not one particular test has been proven to be both specific and sensitive.
To identify which of these tests was most sensitive in diagnosing SIS, Park et al. looked at determining the diagnostic value of eight index tests. They reported that the combination of Hawkins–Kennedy test, painful arc sign, and weakness in external rotation was most likely to pick up the syndrome.24 In a systematic review by Watts et al., they identified 82% of the articles carried out by either Neer's or Hawkins–Kennedy test to diagnose SIS. In 70% of the studies, both of these tests were used in conjunction with each other.25
In their study, Watts et al. went on to comment on the value of clinical tests termed “excluding tests” to help reach the diagnosis of SIS.25 Eighty three percent of the studies reviewed in their article carried out at least one test to exclude other common shoulder pathologies and these tests ranged from the O’Brien's test for superior labral anteroposterior lesions, apprehension test for instability, and resisted tests.
Observations in this study mirrored a large review article by Hanchard et al. where they identified the combination of the Neer's and Hawkins–Kennedy test to be the most sensitive for SIS at the expense of a large number of false positives.26 The review went on to emphasize the importance of excluding other shoulder pathologies in the process of diagnosing SIS. In a study of ten individuals with normal shoulders (average age 32 years), Roberts found that the rotator cuff insertion was closest to the anteroinferior acromion at 90° of flexion (i.e., Hawkins sign position) but not at full elevation (i.e., Neer sign position).27 All shoulders in the Neer position demonstrated a contact between the soft tissues and the medial acromion. Shoulders in the Hawkins position had contact between soft tissues and the CAL. Although these studies were done in normal shoulders, which may influence the results, these tests for subacromial impingement seem to demonstrate contact consistent with mechanical impingement. Table 1 summarizes various key tests for the clinical examination of SIS.
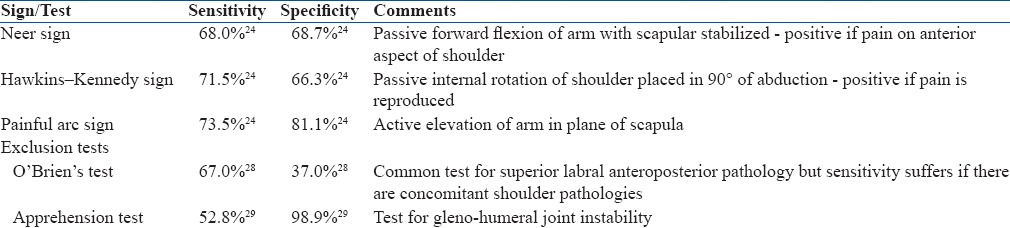
Table 1.
Summary of common tests done during evaluation for subacromial impingement syndrome
Imaging Studies
Plain radiographs of the affected shoulder should be obtained as a standard investigation and this plays a role mainly in excluding other shoulder pathologies. The minimum recommended projections should include an anteroposterior view, an axillary view, and a scapular outlet view. The senior author also routinely gets 30° caudal tilt and 15° cephalad tilt to look for any spurs.
The axillary view is helpful in visualizing, if there is a presence of an os acromiale and the scapular outlet view are excellent for assessing acromion morphology.20 Measurement of the acromial humeral distance can be done on plain radiograph and is reported to be an accurate reflection of patient's clinical picture.30
Any additional investigations of the shoulder should be used with caution and only if there is suspicion of a rotator cuff or other “repairable” shoulder pathologies such as tear of the labrum or instability.
Ultrasonography and magnetic resonance imaging (MRI) are both widely used investigations for SIS. Ultrasonography has several advantages over MRI scans as they tend to be more accessible, cheaper, and provide a dynamic assessment of the shoulder, but is highly operator dependent.31 Ideally, it should be performed by the clinician as the images are static for a dynamic study. A study by Middleton noted higher satisfaction in patients undergoing ultrasound scan (USS) for their shoulder pain compared to MRI scan.32 Despite this and evidence showing USS having a comparable accuracy in identifying rotator cuff pathologies as to MRI, this imaging modality is highly dependent on operator experience and habitus of the patient.33
MRI has of some time now been the noninvasive investigation of choice for patients with suspected SIS. It allows excellent static visualization of structures in the subacromial space. Signs suggestive of bursitis on MRI include bursal thickness of >3 mm and presence of fluid in the anterior aspect of the bursa.34 Studies consistently report sensitivity and specificity of around 90% in identifying rotator cuff tears on MRI which can be further improved by performing an arthrogram.35,36 A meta-analysis carried out by Roy et al. noted a higher sensitivity of detecting partial-thickness rotator cuff tears when compared to USS and noncontrast MRI scan of the shoulder.37 Their article went on to conclude that USS, MRI, and magnetic resonance arthrogram (MRA) had similar high level of diagnostic accuracy for full-thickness rotator cuff tears when performed in patients with shoulder pain. From this, we can conclude that an USS or MRI scan is sensitive enough in investigations for SIS without the invasiveness and associated risk of an MRA scan.
Caution should, however, be applied when interpreting results of these investigations as a significant number of patients in one study were found to have rotator cuff tears despite having a pain-free and asymptomatic shoulder.38 This finding was more common with increasing age and led to recommendations that these investigations should not be interpreted in isolation, and clinical correlation with patients’ history and physical examination findings is required before a diagnosis of SIS can be made.39
Management
The most beneficial and appropriate management of SIS is a topic of wide debate. Both nonoperative and operative treatment options have been described in literature with equally good outcomes. There is currently no evidence to suggest that surgical treatment provides superior outcomes compared to nonsurgical treatment and hence, surgery is usually only indicated in patients with failure of conservative management.40
Nonoperative Methods
Oral nonsteroidal anti-inflammatory drugs (NSAIDs) may be beneficial in the short term in people with acute tendonitis/subacromial bursitis.41 Petri et al. in a double-blind placebo-controlled trial showed improvement with oral naproxen in the management of SIS.42 However, a systematic review looking at the effectiveness of NSAIDs, steroid, or other injections found little evidence of oral NSAIDS being of much help.43 The authors do not recommend these in isolation, unless the pain is significant or in patients with sudden onset with or without trauma.
Steroid Injection in Subacromial Space
Corticosteroid injections into the subacromial space and physiotherapy, often in combination, form the mainstay of nonoperative management. Cummins et al. prospectively evaluated outcomes in 100 patients who had a subacromial steroid injection followed by physical therapy.44 They found that 79% of the patients did not require surgery after 2 years, and in these patients, the average American Shoulder and Elbow Surgeons (ASES) outcome score increased from 56 to 95, with an average decrease in the visual analog score (VAS) from 4.8 to 0.6. However, they also found that 30% of the patients who did not undergo surgery continued to have some shoulder pain. Kang et al. also reported an improvement in University California Los Angeles (UCLA) shoulder score and VAS up to 3 months postinjection.45 The use of ultrasound to perform the injection has not been shown to be any superior than doing it blindly using clinical landmarks.46 The improvement in VAS and ASES score was comparable.
Physical Therapy
Physiotherapy is considered a critical component of nonoperative and operative regimens for subacromial pain. Kuhn conducted a systematic review of 11 randomized controlled trials that had investigated the effect of exercise on subacromial impingement pain.47 They found that physical exercise improved pain but did not have an effect on function and strength. Ketola et al. conducted a randomized controlled trial comparing a supervised exercise program and acromioplasty followed by a similar exercise program.48 They did not find any difference in outcomes between the two groups after 2 years.
Dong et al. conducted a PRISMA systematic review and meta-analysis of various treatment options for SIS.49 They concluded that nonoperative treatments such as exercise therapy, acupuncture, ultrasound, pulsed electromagnetic field therapy, and corticosteroid injection all improved pain and the Constant–Murley score in patients with SIS. However, treatments in combination with exercise therapy showed better result.
Some studies have investigated the effect of injecting other therapeutic substances into the subacromial space. Karthikeyan et al. compared the effects of the NSAID tenoxicam with methylprednisolone and found that the steroid injections were more effective 6 weeks after the injection.50
Orthobiologics
Orthobiologics refers to the use of biological substances to help with the recovery of injured musculoskeletal tissues.51 Collectively, this includes the utilization of products such as platelet-rich plasma (PRP), stem cells, growth factors, and hyaluronic acid (HA). Several groups have hypothesized the benefit of PRP in the management of SIS, especially for tendinopathy. A recent meta-analysis of 18 studies showed good evidence to support the use of PRP for the treatment of tendinopathy, but studies included in this review were not specific to the treatment of SIS.52 Two randomized controlled trials have been carried out to specifically assess the benefit of PRP for rotator cuff tendinopathy. The first study compared PRP injection to a saline placebo and results from this study showed similar improvement in pain and function in both groups of patients.53 A second study compared dry needling to injection of PRP and the study reported improvement in pain and function in patients receiving the injection.54
HA, a component of synovial fluid, is another orthobiologic that has been put forward for the treatment of SIS. Early studies comparing HA injection with corticosteroids and placebo injection have not shown symptomatic or functional improvement in patients with subacromial impingment.55 However, a review of 11 studies concluded that intraarticular supplementation with HA did help improve symptoms of SIS patients with rotator cuff tears.56
Surgery
Failure of nonoperative management, in our opinion, is the only absolute indication for surgery in SIS without a full-thickness rotator cuff tear.
Historically, these patients have been treated by open acromioplasty as described by Neer.3 Neer described the goal of treatment to be pain relief in these patients and included open anterior acromioplasty and repair of the rotator cuff if necessary. This in his opinion would reduce the wear and degeneration of rotator cuff and biceps tendon.
Chin et al. reported that 88% of patients reported high satisfaction and 72% had no or minimal pain 25 years after undergoing open acromioplasty. Five patients required additional surgery, including distal clavicle excision (one patient), revision anterior acromioplasty (one patient), and repair of a new rotator cuff tear (three patients).57
With the evolution of arthroscopic techniques – this has become the gold standard for patients with persistent SIS. This allows the surgeon to inspect the gleno-humeral joint and look at intraarticular pathologies and the long head of biceps. Arthroscopy of the subacromial space allows the surgeon to assess the bursa and the undersurface of acromion. A typical lesion [Figure 2] shows scuffing of the undersurface of acromion and the bursal side of rotator cuff. The procedure can be carried out either in beach chair position or lateral position – based on individual preference. Each position has its advantages and disadvantages, details of which are beyond the scope of this article.
Figure 2.

Arthrosopic view showing Impingement Lesion
Ellman first described the technique of arthroscopic subacromial decompression (ASAD), and since then, this has now become the standard treatment for rotator cuff problems.46 He found that 88% of patients were satisfied and 12% were unsatisfied with the results.
Odenbring et al. reported good or excellent results in 77% of the patients 12–14 years after arthroscopic acromioplasty.58 Davis et al. conducted a meta-analysis of nine studies that compared open versus arthroscopic acromioplasty with a minimum of 1-year followup.59 They did not find any difference in clinical outcomes but suggested that open acromioplasty was associated with a longer hospital stay and greater time to return to work.
Taheriazam et al. attempted to predict factors that would lead to failure of nonoperative treatment and found that those with a high initial constant score, a long duration of symptoms, and Type II or III acromion morphology were more likely to require more invasive treatment options.60
Some authors have advocated performing a bursectomy in isolation without acromioplasty. Donigan and Wolf evaluated six studies and found that bursectomy alone provides similar outcomes to acromioplasty and bursectomy.61 However, only one of the six studies was a randomized controlled trial. Dong et al., on the other hand, concluded that a standard ASAD provides a better outcome than bursectomy alone.49
Although good results have been described in patients who have an ASAD, approximately 10% of patients continue to have pain postoperatively. Singh et al. evaluated 112 patients at 3 and 12 months following ASAD.62 They developed a preoperative scoring system consisting of six variables and found that 12 patients with a score of 2 or below continued to have pain even 1 year after surgery and 38 patients with a score of 3 or 4 had only a slight improvement in pain at 1 year postsurgery. After a multivariate analysis, they found that factors associated with a favorable outcome from surgery were the presence of radiological changes of impingement on both the acromion and the humerus followed by a positive response to a subacromial steroid injection. Patel et al. also found that a positive impingement test, i.e., pain relief after a subacromial steroid injection, was associated with a favorable subjective outcome as measured by patient satisfaction.63 It is, therefore, recommended that surgery should only be offered to those who have failed nonoperative management and where surgery is likely to lead to an improvement in pain and function.
The presence of partial or full-thickness cuff tears can also influence the outcome from surgery. Budoff et al. reported the long term results (mean 9.5 years) of 62 shoulders (sixty patients) with partial thickness tears treated with debridement without acromioplasty.64 The authors reported that 79% of shoulders had excellent or good results based on the UCLA shoulder scores and that, of the sixty patients, 77% had no or only minimal pain. Paulos and Franklin reported the results of eighty ASADs in 76 patients.65 At an average followup of 32 months, patients had decreased pain with activity and at night and showed decreased impingement signs at final followup. Poorer results were seen in patients with full-thickness cuff tears.
Summary
SIS is a common and painful condition seen in the active young adults. There is ongoing debate on the etiology of impingement and rotator cuff tears, but is likely to be multifactorial. If diagnosed and treated correctly, it has excellent outcomes. Operative intervention should only be advised once all means of nonoperative management have been exhausted. Caution must be advised in those above the age of 60 years and those with rotator cuff tears. There is still a need for high-quality research on the management of SIS.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Mitchell C, Adebajo A, Hay E, Carr A. Shoulder pain: Diagnosis and management in primary care. BMJ. 2005;331:1124–8. doi: 10.1136/bmj.331.7525.1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Luime JJ, Koes BW, Hendriksen IJ, Burdorf A, Verhagen AP, Miedema HS, et al. Prevalence and incidence of shoulder pain in the general population; a systematic review. Scand J Rheumatol. 2004;33:73–81. doi: 10.1080/03009740310004667. [DOI] [PubMed] [Google Scholar]
- 3.Neer CS., 2nd Anterior acromioplasty for the chronic impingement syndrome in the shoulder: A preliminary report. J Bone Joint Surg Am. 1972;54:41–50. [PubMed] [Google Scholar]
- 4.Umer M, Qadir I, Azam M. Subacromial impingement syndrome. Orthop Rev (Pavia) 2012;4:e18. doi: 10.4081/or.2012.e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Duplay S. Shoulder stiffness as a consequence of scapulo-humeral periarthritis. Arch Gén Méd. 1872;20:29. [Google Scholar]
- 6.Codman EA. On stiff and painful shoulders. Boston Med Surg J. 1906;154:613–20. [Google Scholar]
- 7.Codman EA. Rupture of the supraspinatus tendon 1911. Clin Orthop Relat Res. 1990;254:3–26. [PubMed] [Google Scholar]
- 8.Codman EA, Akerson IB. The pathology associated with rupture of the supraspinatus tendon. Ann Surg. 1931;93:348–59. doi: 10.1097/00000658-193101000-00043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Meyer AW. The minuter anatomy of attrition lesions. JBJS. 1931;13:341–60. [Google Scholar]
- 10.Meyer AW. Chronic functional lesions of the shoulder. Arch Surg. 1937;35:646–74. [Google Scholar]
- 11.Neer CS., 2nd Impingement lesions. Clin Orthop Relat Res. 1983;173:70–7. [PubMed] [Google Scholar]
- 12.Chambler AF, Bull AM, Reilly P, Amis AA, Emery RJ. Coracoacromial ligament tension in vivo. J Shoulder Elbow Surg. 2003;12:365–7. doi: 10.1016/s1058-2746(03)00031-4. [DOI] [PubMed] [Google Scholar]
- 13.Bigliani LU. The morphology of the acromion and its relationship to rotator cuff tears. Orthop Translat. 1986;10:228. [Google Scholar]
- 14.Gill TJ, McIrvin E, Kocher MS, Homa K, Mair SD, Hawkins RJ. The relative importance of acromial morphology and age with respect to rotator cuff pathology. J Shoulder Elbow Surg. 2002;11:327–30. doi: 10.1067/mse.2002.124425. [DOI] [PubMed] [Google Scholar]
- 15.Worland RL, Lee D, Orozco CG, SozaRex F, Keenan J. Correlation of age, acromial morphology, and rotator cuff tear pathology diagnosed by ultrasound in asymptomatic patients. J South Orthop Assoc. 2003;12:23–6. [PubMed] [Google Scholar]
- 16.Neer CS, 2nd, Marberry TA. On the disadvantages of radical acromionectomy. J Bone Joint Surg Am. 1981;63:416–9. [PubMed] [Google Scholar]
- 17.Tempelhof S, Rupp S, Seil R. Age-related prevalence of rotator cuff tears in asymptomatic shoulders. J Shoulder Elbow Surg. 1999;8:296–9. doi: 10.1016/s1058-2746(99)90148-9. [DOI] [PubMed] [Google Scholar]
- 18.Yamaguchi K, Ditsios K, Middleton WD, Hildebolt CF, Galatz LM, Teefey SA. The demographic and morphological features of rotator cuff disease. A comparison of asymptomatic and symptomatic shoulders. J Bone Joint Surg Am. 2006;88:1699–704. doi: 10.2106/JBJS.E.00835. [DOI] [PubMed] [Google Scholar]
- 19.Lohr JF, Uhthoff HK. The microvascular pattern of the supraspinatus tendon. Clin Orthop Relat Res. 1990 May;254:35–8. [PubMed] [Google Scholar]
- 20.Harrison AK, Flatow EL. Subacromial impingement syndrome. J Am Acad Orthop Surg. 2011;19:701–8. doi: 10.5435/00124635-201111000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Walch G, Boileau P, Noel E, Donell ST. Impingement of the deep surface of the supraspinatus tendon on the posterosuperior glenoid rim: An arthroscopic study. J Shoulder Elbow Surg. 1992;1:238–45. doi: 10.1016/S1058-2746(09)80065-7. [DOI] [PubMed] [Google Scholar]
- 22.McFarland EG, Hsu CY, Neira C, O’Neil O. Internal impingement of the shoulder: A clinical and arthroscopic analysis. J Shoulder Elbow Surg. 1999;8:458–60. doi: 10.1016/s1058-2746(99)90076-9. [DOI] [PubMed] [Google Scholar]
- 23.Gerber C, Galantay RV, Hersche O. The pattern of pain produced by irritation of the acromioclavicular joint and the subacromial space. J Shoulder Elbow Surg. 1998;7:352–5. doi: 10.1016/s1058-2746(98)90022-2. [DOI] [PubMed] [Google Scholar]
- 24.Park HB, Yokota A, Gill HS, El Rassi G, McFarland EG. Diagnostic accuracy of clinical tests for the different degrees of subacromial impingement syndrome. J Bone Joint Surg Am. 2005;87:1446–55. doi: 10.2106/JBJS.D.02335. [DOI] [PubMed] [Google Scholar]
- 25.Watts AR, Williams B, Kim SW, Bramwell DC, Krishnan J. Shoulder impingement syndrome: A systematic review of clinical trial participant selection criteria. Shoulder Elbow. 2017;9:31–41. doi: 10.1177/1758573216663201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hanchard NC, Lenza M, Handoll HH, Takwoingi Y. Physical tests for shoulder impingements and local lesions of bursa, tendon or labrum that may accompany impingement. Cochrane Database Syst Rev. 2013;4:CD007427. doi: 10.1002/14651858.CD007427.pub2. doi: 10.1002/14651858.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Roberts CS, Davila JN, Hushek SG, Tillett ED, Corrigan TM. Magnetic resonance imaging analysis of the subacromial space in the impingement sign positions. J Shoulder Elbow Surg. 2002;11:595–9. doi: 10.1067/mse.2002.127095. [DOI] [PubMed] [Google Scholar]
- 28.Hegedus EJ, Goode AP, Cook CE, Michener L, Myer CA, Myer DM, et al. Which physical examination tests provide clinicians with the most value when examining the shoulder? Update of a systematic review with meta-analysis of individual tests. Br J Sports Med. 2012;46:964–78. doi: 10.1136/bjsports-2012-091066. [DOI] [PubMed] [Google Scholar]
- 29.Lo IK, Nonweiler B, Woolfrey M, Litchfield R, Kirkley A. An evaluation of the apprehension, relocation, and surprise tests for anterior shoulder instability. Am J Sports Med. 2004;32:301–7. doi: 10.1177/0095399703258690. [DOI] [PubMed] [Google Scholar]
- 30.Mayerhöfer ME, Breitenseher MJ. Impingement syndrome of the shoulder. Radiologe. 2004;44:569–77. doi: 10.1007/s00117-004-1051-7. [DOI] [PubMed] [Google Scholar]
- 31.Harmon KG, O’Connor FG. Musculoskeletal ultrasound: Taking sports medicine to the next level. Br J Sports Med. 2010;44:1135–6. doi: 10.1136/bjsm.2010.080796. [DOI] [PubMed] [Google Scholar]
- 32.Middleton WD, Payne WT, Teefey SA, Hildebolt CF, Rubin DA, Yamaguchi K. Sonography and MRI of the shoulder: Comparison of patient satisfaction. AJR Am J Roentgenol. 2004;183:1449–52. doi: 10.2214/ajr.183.5.1831449. [DOI] [PubMed] [Google Scholar]
- 33.Teefey SA, Rubin DA, Middleton WD, Hildebolt CF, Leibold RA, Yamaguchi K. Detection and quantification of rotator cuff tears. Comparison of ultrasonographic, magnetic resonance imaging, and arthroscopic findings in seventy-one consecutive cases. J Bone Joint Surg Am. 2004;86-A:708–16. [PubMed] [Google Scholar]
- 34.White EA, Schweitzer ME, Haims AH. Range of normal and abnormal subacromial/subdeltoid bursa fluid. J Comput Assist Tomogr. 2006;30:316–20. doi: 10.1097/00004728-200603000-00030. [DOI] [PubMed] [Google Scholar]
- 35.Iannotti JP, Zlatkin MB, Esterhai JL, Kressel HY, Dalinka MK, Spindler KP. Magnetic resonance imaging of the shoulder. Sensitivity, specificity, and predictive value. J Bone Joint Surg Am. 1991;73:17–29. [PubMed] [Google Scholar]
- 36.Pavic R, Margetic P, Bensic M, Brnadic RL. Diagnostic value of US, MR and MR arthrography in shoulder instability. Injury. 2013;44(Suppl 3):S26–32. doi: 10.1016/S0020-1383(13)70194-3. [DOI] [PubMed] [Google Scholar]
- 37.Roy JS, Braën C, Leblond J, Desmeules F, Dionne CE, MacDermid JC, et al. Diagnostic accuracy of ultrasonography, MRI and MR arthrography in the characterisation of rotator cuff disorders: A systematic review and meta-analysis. Br J Sports Med. 2015;49:1316–28. doi: 10.1136/bjsports-2014-094148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sher JS, Uribe JW, Posada A, Murphy BJ, Zlatkin MB. Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Joint Surg Am. 1995;77:10–5. doi: 10.2106/00004623-199501000-00002. [DOI] [PubMed] [Google Scholar]
- 39.Lee JH, Lee SH, Song SH. Clinical effectiveness of botulinum toxin type B in the treatment of subacromial bursitis or shoulder impingement syndrome. Clin J Pain. 2011;27:523–8. doi: 10.1097/AJP.0b013e31820e1310. [DOI] [PubMed] [Google Scholar]
- 40.Dorrestijn O, Stevens M, Winters JC, van der Meer K, Diercks RL. Conservative or surgical treatment for subacromial impingement syndrome? A systematic review. J Shoulder Elbow Surg. 2009;18:652–60. doi: 10.1016/j.jse.2009.01.010. [DOI] [PubMed] [Google Scholar]
- 41.Kulkarni R, Gibson J, Brownson P, Thomas M, Rangan A, Carr AJ, et al. Subacromial shoulder pain. Shoulder Elbow. 2015;7:135–43. doi: 10.1177/1758573215576456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Petri M, Dobrow R, Neiman R, Whiting-O’Keefe Q, Seaman WE. Randomized, double-blind, placebo-controlled study of the treatment of the painful shoulder. Arthritis Rheum. 1987;30:1040–5. doi: 10.1002/art.1780300911. [DOI] [PubMed] [Google Scholar]
- 43.Cole BF, Peters KS, Hackett L, Murrell GA. Ultrasound-guided versus blind subacromial corticosteroid injections for subacromial impingement syndrome: A randomized, double-blind clinical trial. Am J Sports Med. 2016;44:702–7. doi: 10.1177/0363546515618653. [DOI] [PubMed] [Google Scholar]
- 44.Cummins CA, Sasso LM, Nicholson D. Impingement syndrome: Temporal outcomes of nonoperative treatment. J Shoulder Elbow Surg. 2009;18:172–7. doi: 10.1016/j.jse.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 45.Kang MN, Rizio L, Prybicien M, Middlemas DA, Blacksin MF. The accuracy of subacromial corticosteroid injections: A comparison of multiple methods. J Shoulder Elbow Surg. 2008;17(1 Suppl):61S–6S. doi: 10.1016/j.jse.2007.07.010. [DOI] [PubMed] [Google Scholar]
- 46.Ellman H. Arthroscopic subacromial decompression: Analysis of one- to three-year results. Arthroscopy. 1987;3:173–81. doi: 10.1016/s0749-8063(87)80061-0. [DOI] [PubMed] [Google Scholar]
- 47.Kuhn JE. Exercise in the treatment of rotator cuff impingement: A systematic review and a synthesized evidence-based rehabilitation protocol. J Shoulder Elbow Surg. 2009;18:138–60. doi: 10.1016/j.jse.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 48.Ketola S, Lehtinen J, Arnala I, Nissinen M, Westenius H, Sintonen H, et al. Does arthroscopic acromioplasty provide any additional value in the treatment of shoulder impingement syndrome?: A two-year randomised controlled trial. J Bone Joint Surg Br. 2009;91:1326–34. doi: 10.1302/0301-620X.91B10.22094. [DOI] [PubMed] [Google Scholar]
- 49.Dong W, Goost H, Lin XB, Burger C, Paul C, Wang ZL, et al. Treatments for shoulder impingement syndrome: A PRISMA systematic review and network meta-analysis. Medicine (Baltimore) 2015;94:e510. doi: 10.1097/MD.0000000000000510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Karthikeyan S, Kwong HT, Upadhyay PK, Parsons N, Drew SJ, Griffin D. A double-blind randomised controlled study comparing subacromial injection of tenoxicam or methylprednisolone in patients with subacromial impingement. J Bone Joint Surg Br. 2010;92:77–82. doi: 10.1302/0301-620X.92B1.22137. [DOI] [PubMed] [Google Scholar]
- 51.Dhillon MS, Behera P, Patel S, Shetty V. Orthobiologics and platelet rich plasma. Indian J Orthop. 2014;48:1–9. doi: 10.4103/0019-5413.125477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fitzpatrick J, Bulsara M, Zheng MH. The Effectiveness of platelet-rich plasma in the treatment of tendinopathy: A meta-analysis of randomized controlled clinical trials. Am J Sports Med. 2017;45:226–33. doi: 10.1177/0363546516643716. [DOI] [PubMed] [Google Scholar]
- 53.Kesikburun S, Tan AK, Yilmaz B, Yasar E, Yazicioglu K. Platelet-rich plasma injections in the treatment of chronic rotator cuff tendinopathy: A randomized controlled trial with 1-year followup. Am J Sports Med. 2013;41:2609–16. doi: 10.1177/0363546513496542. [DOI] [PubMed] [Google Scholar]
- 54.Rha DW, Park GY, Kim YK, Kim MT, Lee SC. Comparison of the therapeutic effects of ultrasound-guided platelet-rich plasma injection and dry needling in rotator cuff disease: A randomized controlled trial. Clin Rehabil. 2013;27:113–22. doi: 10.1177/0269215512448388. [DOI] [PubMed] [Google Scholar]
- 55.Penning LI, de Bie RA, Walenkamp GH. The effectiveness of injections of hyaluronic acid or corticosteroid in patients with subacromial impingement: A three-arm randomised controlled trial. J Bone Joint Surg Br. 2012;94:1246–52. doi: 10.1302/0301-620X.94B9.28750. [DOI] [PubMed] [Google Scholar]
- 56.Osti L, Buda M, Buono AD, Osti R, Massari L. Clinical evidence in the treatment of rotator cuff tears with hyaluronic acid. Muscles Ligaments Tendons J. 2016;5:270–5. doi: 10.11138/mltj/2015.5.4.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chin PY, Sperling JW, Cofield RH, Stuart MJ, Crownhart BS. Anterior acromioplasty for the shoulder impingement syndrome: Long term outcome. J Shoulder Elbow Surg. 2007;16:697–700. doi: 10.1016/j.jse.2007.02.116. [DOI] [PubMed] [Google Scholar]
- 58.Odenbring S, Wagner P, Atroshi I. Long term outcomes of arthroscopic acromioplasty for chronic shoulder impingement syndrome: A prospective cohort study with a minimum of 12 years’ followup. Arthroscopy. 2008;24:1092–8. doi: 10.1016/j.arthro.2008.04.073. [DOI] [PubMed] [Google Scholar]
- 59.Davis AD, Kakar S, Moros C, Kaye EK, Schepsis AA, Voloshin I. Arthroscopic versus open acromioplasty: A meta-analysis. Am J Sports Med. 2010;38:613–8. doi: 10.1177/0363546508328100. [DOI] [PubMed] [Google Scholar]
- 60.Taheriazam A, Sadatsafavi M, Moayyeri A. Outcome predictors in nonoperative management of newly diagnosed subacromial impingement syndrome: A longitudinal study. MedGenMed. 2005;7:63. [PMC free article] [PubMed] [Google Scholar]
- 61.Donigan JA, Wolf BR. Arthroscopic subacromial decompression: Acromioplasty versus bursectomy alone – does it really matter? A systematic review. Iowa Orthop J. 2011;31:121–6. [PMC free article] [PubMed] [Google Scholar]
- 62.Singh HP, Mehta SS, Pandey R. A preoperative scoring system to select patients for arthroscopic subacromial decompression. J Shoulder Elbow Surg. 2014;23:1251–6. doi: 10.1016/j.jse.2014.05.030. [DOI] [PubMed] [Google Scholar]
- 63.Patel VR, Singh D, Calvert PT, Bayley JI. Arthroscopic subacromial decompression: Results and factors affecting outcome. J Shoulder Elbow Surg. 1999;8:231–7. doi: 10.1016/s1058-2746(99)90134-9. [DOI] [PubMed] [Google Scholar]
- 64.Budoff JE, Rodin D, Ochiai D, Nirschl RP. Arthroscopic rotator cuff debridement without decompression for the treatment of tendinosis. Arthroscopy. 2005;21:1081–9. doi: 10.1016/j.arthro.2005.05.019. [DOI] [PubMed] [Google Scholar]
- 65.Paulos LE, Franklin JL. Arthroscopic shoulder decompression development and application. A five year experience. Am J Sports Med. 1990;18:235–44. doi: 10.1177/036354659001800303. [DOI] [PubMed] [Google Scholar]