Abstract
Current surgical treatment of acetabular fractures is open reduction and internal fixation and requires a large incision resulting in considerable blood loss and a potentially long duration of recovery. We report a case of an acetabular fracture that received laparoscopic internal fixation after three-dimensional (3D) modelling and printing of the acetabulum. A 43 year old male fell from a height of 3 m resulting in a right acetabulum anterior column fracture. Thin section computed tomography scanning with 0.6 mm increments and subsequent 3D reconstruction was performed, and a 3D model of the acetabulum and fracture was printed. The steel reconstruction plate was prebent in vivo and placed into the optimized position based on the 3D modelling and the optimized insert orientation and measured screw length were determined. The fracture was reduced and the plate placed laparoscopically without complications, and the patient had excellent functional recovery. Acetabular fractures are complex injuries, and while minimally invasive surgical techniques are used in many fields, they are not common for the treatment of acetabular fractures. 3D modelling is commonly used in medicine, and although 3D printing is used in some fields, it has not found widespread use in orthopedics.
Keywords: Acetabular fracture, endoscopic, internal fixation, laparoscopy, percutaneous, three-dimensional printing
MeSH terms: Acetabulum, fracture fixation, percutaneous, endoscopes
Introduction
Acetabular fracture accounts for 10–22% of all fractures and are associated with a variety of complications, with mortality ranging from 5% to 25%.1 Current surgical treatment of acetabular fractures is open reduction and internal fixation (ORIF) and requires a large incision resulting in considerable blood loss and a potentially long duration of recovery.2,3,4 Endoscopy has shown promise for the reduction and fixation of pelvic fractures.5,6 Three-dimensional (3D) computer reconstruction and modelling are used in many medical fields, and 3D printing, based on 3D computer graphics, is used in surgical planning, the production of personalized prostheses, and bone engineering.7,8,9
The purpose of this report is to describe the case of an acetabular fracture that was repaired by minimally invasive laparoscopic surgery after performing simulated surgery on a 3D-printed model of the pelvis and fracture, which allowed accurate preoperative fitting of the reconstruction plate and determination of screw size and placement.
Case Report
Informed consent was obtained from the patient for publication. A 43-year-old male fell from a height of 3 m resulting in a fracture of the right acetabulum and distal radius. The acetabular fracture was classified as a fracture of the anterior column based on the Letournel system.3 A complete preoperative examination was performed after hospital admission. Plain film pelvic radiography [Figure 1a and b] and thin-section computed tomography (CT) scanning with 0.6 mm increments [Figure 1c and d] were performed. The CT image showed a fracture displacement of >2 mm, which had surgical indications and could not be treated with percutaneous screw fixation method.
Figure 1.

(a) X-ray pelvis with hip joint showing anterior column fracture (b) Postoperative x-ray pelvis with hip joint of same patient showing plate in situ (c) Preoperative computed tomography showing fracture line (arrow) (d) Postoperative computed tmography showing reduction and plate in situ
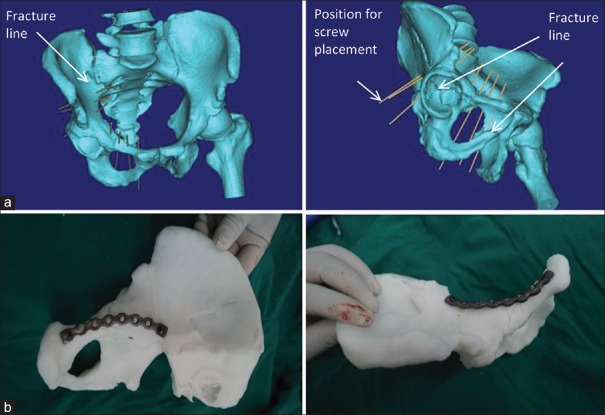
The CT images were imported into Mimics software (Materialise, Belgium) for 3D editing and virtual fracture reduction. Based on the multiplanar 3D reconstructions, the best location for the internal fixation plate was identified; the plate was designed and optimized, and the optimal screw length, position and orientation were determined [Figure 2a]. The fracture model was then printed with a 3D printer; the steel reconstruction plate was prebent ex vivo and placed into the optimized position based on the 3D modelling [Figure 2b]. Based on the optimized insert orientation and measured screw length obtained from the modelling, a simulated surgery was performed on the 3D-printed model and the details were recorded for use in the actual surgery.
Figure 2.
(a) Computed tomography three-dimensional reconstruction of the acetabulum and fracture. Arrows indicate the fracture line and the position for the screws placement. (b) Placement of a steel reconstruction plate on the three-dimensional printed model
Laparoscopic surgery was performed after induction of general anesthesia with the patient in the supine position with feet higher than the head by 15°, and buttocks of the affected side lifted by 20°. Trocars were placed 1.0 cm below the umbilicus, in the midline 1/3 the distance superior to the pelvis from the umbilicus, at McBurney's point and 1/3 of the distance from the pubic symphysis toward the anterior superior iliac spine of the affected side [Figure 3a]. Under laparoscopy, extraperitoneal incisions revealed the pubic tubercle, suprapubic region, and iliopubic tract, and the corona mortis was ligated. The arteriovenous vessels proximal to the ilium were protected using sterile gauze with appropriate traction. An ultrasonic scalpel was used for incision of the periosteum and the iliopectineal fascia. The exposed fracture was reduced using rod holders. The reconstruction plate was inserted through the abdominal puncture into the optimized position as determined by 3D modelling. Screws were placed as determined preoperatively [Figure 3b]. A drainage tube was placed prior to closure of the surgical incisions. The blood loss was 80 mL, and operation time was 180 min. Radiography confirmed the location of the plate and screws were identical to that determined with the 3D modelling [Figure 1a], and CT showed anatomical fracture reduction [Figure 1b]. The patient was able to roll over in bed the day of surgery, sit up the next day, and ambulate with crutches after 10 days.
Figure 3.
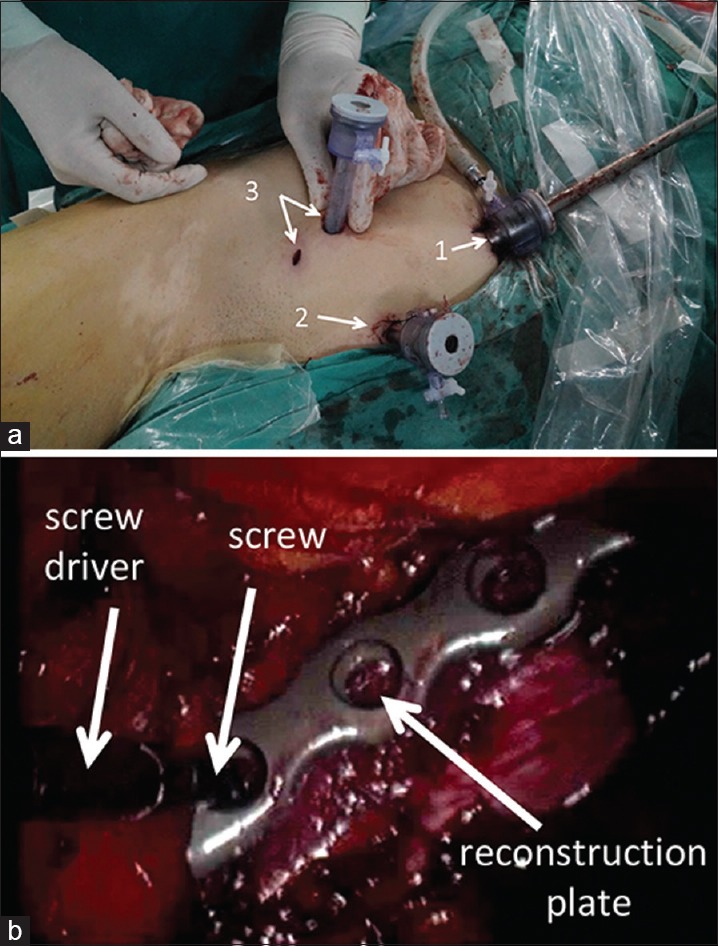
(a) An intraoperative view of the laparoscopic portals. Arrows indicate the light source (1), portal for rod holder (2), and portal for laparoscopy, reconstruction plate and screws (3). (b) Laparoscopic view of screws placement. Arrows indicate the screwdriver, screw, and reconstruction plate
Discussion
In this case, the 3D-printed model allowed precise prebending of the steel plate and determination of the exact length and position of the screws, thus simplifying the surgery and minimizing any chance of surgical errors.
Currently, pelvic fracture surgery includes the ilioinguinal approach,3 the improved Stoppa approach,2 and the lateral rectus approach.4 The method we described allowed for a clear anatomical view in the extraperitoneal pneumoperitoneum, accurate placement of a prebent plate and screws, minimal blood loss and a short recovery period and early restoration of function.
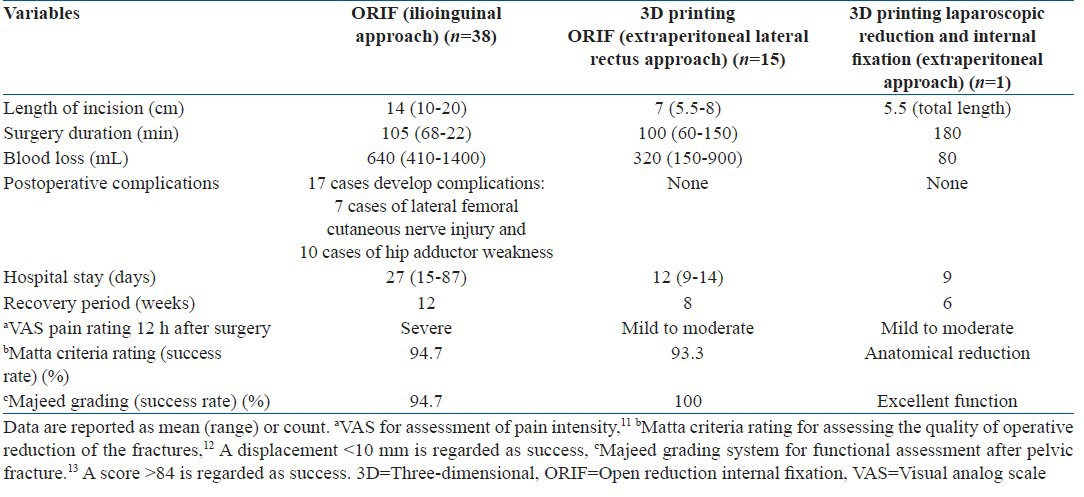
We have also used 3D printing ORIF via an extraperitoneal lateral rectus approach,10 which uses a 3D-printed model to determine the optimal surgical approach and design as in this report; however, the surgery is still performed open. After these experiences, we decided to perform this kind of surgery by a minimally invasive laparoscopic approach. A summary of the outcomes of the three methods is presented in Table 1. It can be seen that 3D printing and ORIF offers advantages over traditional ORIF via the ilioinguinal approach and the method described in this report offers further advantages over 3D printing and ORIF.
Table 1.
Outcomes of three types of acetabular fracture surgeries
There are still some limitations in our case. We took 3 h for surgery, which is about the same for open surgery. This is the first time that the author operated with the general surgeons to perform laparoscopic acetabular fracture fixation and is still not skilled in dissection the superior pubic ramus, iliopectineal eminence to sacroiliac joint. So far, there is still no specialized device for laparoscopic acetabular fracture fixation. We are going to develop new specialized devices, which could further reduce the overall operation time. Other limitations included that 3D printing laparoscopic technique is only applicable to mild cases of anteromedial acetabular fracture displacement and it involves a steep learning curve for surgeons.
To conclude, we have shown that 3D reconstruction and printing can allow for highly accurate preoperative planning for the treatment of acetabular fractures such that reduction and fixation can be performed with a minimally invasive laparoscopic approach. Further refinements of the method may allow a larger percentage of acetabular fractures to be treated in a minimally invasive manner.13
Financial support and sponsorship
This work was supported by grants from Science and Technology Projects in Guangdong Province (2014B090901055), Science and Technology Projects in Guangdong Province (2014A020212176), Science and Technology Projects of Tianhe district in Guangdong Province (201404KW025) and Science and Technology Project of Guangdong Province (2015B010125005).
Conflicts of interest
There are no conflicts of interest.
References
- 1.Gänsslen A, Frink M, Hildebrand F, Krettek C. Both column fractures of the acetabulum: Epidemiology, operative management and long term-results. Acta Chir Orthop Traumatol Cech. 2012;79:107–13. [PubMed] [Google Scholar]
- 2.Cole JD, Bolhofner BR. Acetabular fracture fixation via a modified Stoppa limited intrapelvic approach. Description of operative technique and preliminary treatment results. Clin Orthop Relat Res. 1994:112–23. [PubMed] [Google Scholar]
- 3.Letournel E. The treatment of acetabular fractures through the ilioinguinal approach. Clin Orthop Relat Res. 1993:62–76. [PubMed] [Google Scholar]
- 4.Keel MJ, Ecker TM, Cullmann JL, Bergmann M, Bonel HM, Büchler L, et al. The Pararectus approach for anterior intrapelvic management of acetabular fractures: An anatomical study and clinical evaluation. J Bone Joint Surg Br. 2012;94:405–11. doi: 10.1302/0301-620X.94B3.27801. [DOI] [PubMed] [Google Scholar]
- 5.Rubel IF, Seligson D, Mudd L, Willinghurst C. Endoscopy for anterior pelvis fixation. J Orthop Trauma. 2002;16:507–14. doi: 10.1097/00005131-200208000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Zobrist R, Messmer P, Levin LS, Regazzoni P. Endoscopic-assisted, minimally invasive anterior pelvic ring stabilization: A new technique and case report. J Orthop Trauma. 2002;16:515–9. doi: 10.1097/00005131-200208000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Kozakiewicz M, Elgalal M, Loba P, Komunski P, Arkuszewski P, Broniarczyk-Loba A, et al. Clinical application of 3D pre-bent titanium implants for orbital floor fractures. J Craniomaxillofac Surg. 2009;37:229–34. doi: 10.1016/j.jcms.2008.11.009. [DOI] [PubMed] [Google Scholar]
- 8.Luo Q, Lau TW, Fang X, Leung F. Application of three-dimensional printing technique in orthopaedics. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2014;28:268–71. [PubMed] [Google Scholar]
- 9.Petzold R, Zeilhofer HF, Kalender WA. Rapid protyping technology in medicine – Basics and applications. Comput Med Imaging Graph. 1999;23:277–84. doi: 10.1016/s0895-6111(99)00025-7. [DOI] [PubMed] [Google Scholar]
- 10.Briffa N, Pearce R, Hill AM, Bircher M. Outcomes of acetabular fracture fixation with ten years’ followup. J Bone Joint Surg Br. 2011;93:229–36. doi: 10.1302/0301-620X.93B2.24056. [DOI] [PubMed] [Google Scholar]
- 11.Breivik H, Borchgrevink PC, Allen SM, Rosseland LA, Romundstad L, Hals EK, et al. Assessment of pain. Br J Anaesth. 2008;101:17–24. doi: 10.1093/bja/aen103. [DOI] [PubMed] [Google Scholar]
- 12.Collinge C, Coons D, Tornetta P, Aschenbrenner J. Standard multi planar fluoroscopy versus a fluoroscopically based navigation system for the percutaneous insertion of iliosacral screws: A cadaver model. J Orthop Trauma. 2005;19:254–8. doi: 10.1097/01.bot.0000151821.79827.fb. [DOI] [PubMed] [Google Scholar]
- 13.Sagi HC, Ordway NR, DiPasquale T. Biomechanical analysis of fixation for vertically unstable sacroiliac dislocations with iliosacral screws and symphyseal plating. J Orthop Trauma. 2004;18:138–43. doi: 10.1097/00005131-200403000-00002. [DOI] [PubMed] [Google Scholar]