Abstract
BACKGROUND/OBJECTIVES
The Emergency Department (ED) is an important venue for initial sepsis recognition and care. We sought to determine contemporary estimates of the epidemiology of United States (US) ED visits for sepsis.
DESIGN
Analysis of data from the National Hospital Ambulatory Medical Care Survey.
SETTING
US Emergency Departments visits, 2009–2011.
PARTICIPANTS
Adult (age≥18 years) ED sepsis patients. We defined serious infection as an ED diagnosis of a serious infection or a triage temperature >38 °C or <36 °C. We defined three ED sepsis classifications: 1) [Original ED Sepsis] serious infection + ED diagnosis of organ dysfunction, endotracheal intubation, or systolic blood pressure ≤90 mmHg, or explicit sepsis ED diagnoses; 2) [qSOFA ED Sepsis] serious infection + presence of ≥2 “quick” Sepsis-related Organ Failure Assessment (qSOFA) criteria (Glasgow Coma Scale ≤14, respiratory rate ≥22 breaths/min, or systolic blood pressure ≤100 mmHg); and 3) [Revised ED Sepsis] Original or qSOFA ED Sepsis.
INTERVENTIONS
None
MEASUREMENTS AND RESULTS
We used survey design and weighting variables to produce national estimates of annual adult ED visits using updated sepsis classifications. Over 2009–2011, there were 103,257,516 annual adult ED visits. The estimated number of ED sepsis visits were: 1) Original ED Sepsis 665,319 (0.64%; 95% CI 0.57–0.73); 2) qSOFA ED Sepsis 318,832 (0.31%; CI 0.26–0.37); and 3) Revised ED Sepsis 847,868 (0.82%; 95% CI 0.74–0.91).
CONCLUSIONS
Sepsis continues to present a major burden to US Emergency Departments, affecting up to nearly 850,000 ED visits annually. Updated sepsis classifications may impact national estimates of ED sepsis epidemiology.
Keywords: Sepsis, emergency department, epidemiology
INTRODUCTION
Sepsis, the syndrome of life-threatening organ dysfunction resulting from dysregulated host response to serious infection, is a major public health problem. International consensus recommendations highlight elements essential for optimizing sepsis outcomes, including prompt recognition and early aggressive intervention (1). The Emergency Department (ED) is often the initial setting for the treatment of acute care conditions such as acute myocardial infarction, stroke and major trauma. Likewise, the ED plays an extremely important role in the care of acute sepsis, providing the first opportunities in the hospital for early recognition and timely aggressive care (1–5).
In the effort to mitigate the societal burden of an acute illness such as sepsis, an important first step is to understand its epidemiology and presenting characteristics. While prior studies have described the characteristics of sepsis presenting to US EDs, several factors indicate the need for updated estimates (6). International sepsis care guidelines and new requirements from the Centers for Medicare and Medicaid Services have heightened ED clinician and institutional awareness of sepsis (1, 7). Medical record documentation and coding practices have similarly evolved, increasing the documentation and coding of sepsis (8–10). More recently, the European Society of Intensive Care Medicine and Society for Critical Care Medicine proposed the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3), providing new sepsis definitions that reduce emphasis on inflammation and increase emphasis on organ dysfunction (11–14). Furthermore, the total annual number of patients seeking ED care has escalated over the last 10 years, likely increasing the total number of ED sepsis cases (15).
In light of these many factors, the current national epidemiology of ED sepsis is unclear, and updated estimates are needed. In this study, we sought to determine the national characteristics of adult sepsis patients treated in US Emergency Departments.
METHODS
Study Design
We performed a cross-sectional analysis of data from the National Hospital Ambulatory Medical Care Survey (NHAMCS) (16). Because of the de-identified, publicly-available nature of the data set, this study was exempted from review requirements by the Institutional Review Board of the University of Alabama at Birmingham.
Data Source
NHAMCS is a national probability sample of ED and outpatient visits at hospitals across the US (16). Operated by the National Center for Health Statistics, the goal of the NHAMCS ED survey is to describe ED visits nationally. The survey’s four-stage probability design samples geographically defined areas, hospitals within these areas, emergency service areas within the emergency departments of the hospitals, and patient visits to the emergency services areas. For selected facilities, the survey examines all ED visits for a defined four-week period, identifying clinical data from all identified records. Collected clinical information varies by survey year but generally encompasses patient demographics, vital signs, ED tests and treatments, up to three ED diagnoses codified using the International Classification of Diseases Ninth Edition, and ED disposition and outcome. For this study, we used the 2009–2011 NHAMCS public-use data sets, encompassing a period with uniform reporting of systolic blood pressure, respiratory rate and Glasgow Coma Score needed for the planned analysis.
Study Population – Classifications of ED Sepsis
The Sepsis-3 criteria broadly defined sepsis as the combination of serious infection plus organ dysfunction. We modified the Sepsis-3 criteria to devise a novel “Revised ED Sepsis” classification system accommodating the data elements available in the NHAMCS data set. Our strategy drew upon the existing Angus, et al. severe sepsis criteria, our prior description of ED severe sepsis, as well as elements of the newer Sepsis-3 criteria (11, 12, 17). (Table 1) While Sepsis-3 eliminated the term “severe sepsis,” the guidelines retained the construct of [serious infection + organ dysfunction] as an indicator of sepsis (11, 12, 17). Therefore, we felt it was reasonable to apply the Angus, et al. criteria as a marker for sepsis in our Revised ED Sepsis system.
TABLE 1.
Emergency Department (ED) sepsis classifications.
| Elements | Original ED Sepsis | qSOFA ED Sepsis | Revised ED Sepsis |
|---|---|---|---|
| Serious Infection | [ED infection diagnosis] or [ED triage body temperature >38 °C or <36 °C] | ||
| Sepsis | Serious infection
|
Serious infection
|
Serious infection
|
SBP = systolic blood pressure. qSOFA = quick Sepsis Organ Failure Assessment. GCS = Glasgow Coma Scale.
We first defined “Original ED Sepsis” using our previously reported methods (6). (Table 1) Following the Angus, et al. criteria, we defined a serious infection as the presence of an ED diagnosis for a serious infection (Supplementary Appendix 1) or an ED triage body temperature >38 °C or <36 °C (6, 18). We defined “Original ED Sepsis” as the presence of a serious infection plus a) ED organ dysfunction diagnosis (Supplementary Appendix 2), b) ED triage systolic blood pressure ≤90 mmHg, or c) the performance of ED endotracheal intubation. While the Sepsis-3 criteria use a Sequential Organ Failure Assessment (SOFA) score ≥2 as an indicator of organ dysfunction, NHAMCS did not have data to calculate SOFA scores (11). Furthermore, we included the presence of explicitly coded severe sepsis (995.92) or septic shock (785.52) diagnoses in the definition of Original ED Sepsis.
The Sepsis-3 panel also proposed the use of the quick Sepsis-Related Organ Failure Assessment (qSOFA) to identify suspected infection patients at higher risk of poor outcomes outside of the intensive care unit (ICU). We thus defined “qSOFA ED Sepsis” as the presence of a serious infection plus ≥2 qSOFA criteria (Glasgow Coma Score ≤14, systolic blood pressure ≤100 mmHg, or respiratory rate ≥22 breaths per minute) (11). Finally, we defined “Revised ED Sepsis” as cases fulfilling either the Original or qSOFA ED Sepsis criteria.
Emergency Department Patient and Visit Characteristics
We characterized ED sepsis visits using variables available in the NHAMCS data set. Demographic characteristics included patient age, sex, race, ethnicity, hospital geographic region and population setting. Clinical characteristics included time and mode of arrival, triage vital signs, length of visit, and ED diagnoses. Outcomes for each ED visit included ED disposition (e.g., admission to the hospital), admission destination, and vital status. For the ED visit diagnoses, data abstractors identified the three most prominent documented diagnoses for each ED visit; the National Center for Health Statistics converts these diagnoses to International Classification of Disease, ninth edition (ICD-9) codes. Up to three ICD-9 ED diagnoses are recorded for each visit in NHAMCS. NHAMCS does not contain ICD-9 procedural codes.
Data Analysis
We analyzed the data using descriptive statistics, annualizing all frequency estimates, and incorporating sampling design and weight variables to calculate nationally-weighted estimates and their corresponding 95% confidence intervals (CI). We used ultimate cluster design (single stage sampling) in variance and 95% CI calculations, utilizing “masked” stratum and primary sampling unit identifiers provided with the NHAMCS public-use data set. Prior efforts have demonstrated that variance estimates using these methods are conservative (19). Because the NCHS considers estimates with greater than 30 percent relative standard error or based upon less than 30 raw observations to be unreliable, we noted table cells not fulfilling this threshold.
We calculated national estimates for annual adult ED sepsis visits using each sepsis classification and determined the overlap between classifications. We determined ED patient/visit characteristics and the proportions of serious infection and organ dysfunction subtypes among sepsis cases. We compared ED outcomes (admission rates, intensive care unit admission, and hospital vital status) between ED sepsis classifications. We conducted all analyses using Stata v.14.0 (Stata, Inc., College Station, Texas).
RESULTS
During 2009–2011 there were an estimated 309,772,539 total adult ED visits, translating to 103,257,516 (95% CI: 86,971,093–119,543,939) annual visits in the US. Approximately 21% of adult ED visits presented with a serious infection. Approximately 3% presented with organ dysfunction or ≥2 qSOFA criteria: organ dysfunction diagnosis 1.19%, triage SBP ≤90 mmHg 0.99%, ED endotracheal intubation 0.24%, and ≥2 qSOFA criteria 0.89%. The estimated number and proportion of annual adult ED sepsis cases were: 1) Original 665,319 (0.64%; 95% CI 0.57–0.73), 2) qSOFA 318,832 (0.31%; CI 0.26–0.37), and 3) Revised 847,868 (0.82%; CI 0.74–0.91). (Table 2). Of the 847,868 Revised ED Sepsis cases, 62.40% (CI 57.01–67.49) fulfilled the Original, 21.53% (CI 17.24–26.55) fulfilled the qSOFA, and 16.07% (CI 12.88–19.88) fulfilled both ED Sepsis classifications.
TABLE 2.
Estimated annual number of adult Emergency Department (ED) sepsis visits, 2009–2011.
| qSOFA ED Sepsis Classification |
|||
|---|---|---|---|
|
| |||
| Original ED Sepsis Classification |
Absent | Present | TOTAL |
|
| |||
| Absent | 102,409,648 | 182,549 | 102,592,197 |
| Present | 529,036 | 136,283 | 665,319 |
|
| |||
| TOTAL | 102,938,684 | 318,832 | 103,257,516 |
- = Original ED Sepsis + qSOFA ED sepsis
- = 529,036 + 182,549 + 136,283
- = 847,868 (95% CI: 692,616 – 1,003,121) ED visits [0.82% (95% CI: 0.74 – 0.91) of all adult ED visits]
Among Revised ED Sepsis cases, fever, respiratory and genitourinary serious infections were most common serious infections. (Table 3) The most common organ dysfunction diagnoses were pulmonary cardiovascular and renal. Approximately 38% exhibited SBP ≤90 mmHg, and 38% exhibited ≥2 qSOFA criteria. Explicit diagnoses for severe sepsis or septic shock were rare (3%). Most Revised ED Sepsis cases were older, with over one-third aged ≥75 years. (Table 4) Black patients comprised approximately one-sixth of adult ED sepsis visits. Over half of adult ED sepsis visits arrived by prehospital Emergency Medical Services. More than 38% of ED sepsis visits occurred in hospitals in the South Census Region. Approximately half of sepsis visits presented during the day shift (0700 AM-1459 PM). Less than 5% of sepsis visits were previously seen in the last 72 hours. Approximately one-sixth of adult ED sepsis patients had a history of congestive heart failure, and one-fifth had a history of diabetes. ED length of stay was prolonged for all sepsis visits, with over half spending more than 4 hours in ED. ED visit characteristics were similar across sepsis identification methods. (Appendices 3 and 4)
TABLE 3.
Characteristics of United States Emergency Department (ED) adult sepsis visits using Revised ED Sepsis classification, 2009–2011.
| Revised ED Sepsis | ||
|---|---|---|
|
| ||
| Characteristic | Annual N | % (95% CI) |
|
| ||
| Total Sepsis Events | 847,868 | --- |
| Infection | 839,720 | 99.0 (97.8–99.6) |
| Fever (triage body temperature >38 °C or <36 °C) | 385,827 | 45.5 (40.1–51.0) |
| Serious Infection Diagnosis | 585,110 | 69.0 (63.5–74.0) |
| Infectious/Parasitic Diseases | 12.9 (9.9–16.7) | |
| Respiratory System Infections | 33.9 (29.2–38.9) | |
| Digestive System Infections | 3.8 (2.4–5.9)* | |
| Genitourinary System Infections | 19.0 (15.3–23.4) | |
| Infectious Complications of Pregnancy, Childbirth, Puerperium | 1.2 (0.5–2.7)* | |
| Skin and Subcutaneous Tissue Infections | 3.3 (1.9–5.6)* | |
| Organ Dysfunction | 846,804 | 99.9 (99.5–100.0) |
| Organ Dysfunction Diagnosis Codes | 349,838 | 41.3 (35.9–46.8) |
| Cardiovascular | 10.6 (8.1–13.8) | |
| Hematologic | 4.0 (2.4–6.5)* | |
| Hepatic | 0.4 (0.1–1.1)* | |
| Neurologic | 2.8 (1.3–6.1)* | |
| Renal | 10.0 (6.9–14.2) | |
| Pulmonary | 14.2 (11.0–18.0) | |
| Endotracheal Intubation | 56,852 | 6.7 (4.7–9.4) |
| SBP ≤90 mmHg | 322,723 | 38.1 (32.9–43.5) |
| ≥2 qSOFA Criteria | 320,374 | 37.8 (32.7–43.2) |
| qSOFA Glasgow Coma Score (GCS ≤14) | 48.8 (40.0–57.8) | |
| qSOFA Respiratory (respiratory rate ≥22 breaths/min) | 43.4 (38.3–48.7) | |
| qSOFA Blood Pressure (systolic blood pressure ≤100 mmHg) | 53.2 (47.6–58.7) | |
| Diagnosis of Severe Sepsis or Septic Shock | 26,680 | 3.2 (1.9–5.1)* |
Estimate based upon <30 raw observations; the National Center for Health Statistics considers estimates based upon <30 raw observation to be unreliable.
TABLE 4.
Characteristics of adult Revised ED Sepsis visits, 2009–2011.
| Characteristic | Revised ED Sepsis Annual N= 847,868 % (95% CI) |
|---|---|
|
| |
| Age | |
| 18–24 years | 5.8 (3.9–8.5) |
| 25–44 | 10.3 (7.8–13.6) |
| 45–64 | 31.2 (26.5–36.4) |
| 65–74 | 17.8 (13.9–22.4) |
| ≥75 | 35.0 (30.0–40.2) |
| Sex | |
| Male | 44.7 (40.2–49.3) |
| Female | 55.3 (50.7–59.9) |
| Race | |
| White | 79.6 (74.5–84.0) |
| Black | 17.2 (13.2–22.0) |
| Other | 3.2 (1.8–5.7)* |
| Ethnicity | |
| Hispanic | 6.9 (4.9–9.7) |
| Non-Hispanic | 93.1 (90.3–95.1) |
| Arrival by EMS | |
| Yes | 57.0 (51.8–62.0) |
| No | 38.6 (33.7–43.8) |
| Unknown | 4.4 (2.3–8.3)* |
| Hospital Geographic Region | |
| Northeast | 18.4 (12.2–26.7) |
| Midwest | 23.7 (16.8–32.2) |
| South | 38.4 (29.9–47.7) |
| West | 19.6 (13.5–27.5) |
| Patient Residence Population Setting | |
| Metropolitan Statistical Area (MSA) | 81.6 (70.0–89.3) |
| Non-MSA | 18.4 (10.7–30.0) |
| Arrival Time | |
| Day (0700–1459) | 48.7 (43.8–53.6) |
| Evening (1500–2259) | 35.2 (30.4–40.3) |
| Night (2300–0659) | 16.1 (13.3–19.5) |
| Patient Seen in ED in Last 72 Hours | |
| Yes | 4.3 (2.6–6.9) |
| No | 80.9 (74.4–86.0) |
| Unknown | 14.9 (10.1–21.3) |
| Prior Medical History | |
| Stroke | 11.0 (7.8–15.2) |
| Congestive Heart Failure | 17.1 (13.5–21.3) |
| Dialysis | 6.2 (3.7–10.0) |
| HIV | 1.3 (0.5–3.4)* |
| Diabetes | 23.6 (19.4–28.4) |
| Triage Pulse | |
| 0–40 bpm | 0.2 (0.1–0.7)* |
| 41–80 | 31.2 (26.7–36.0) |
| 81–120 | 52.0 (47.0–57.0) |
| ≥120 | 13.9 (11.1–17.1) |
| Unknown | 2.8 (1.6–4.8)* |
| Triage Respiratory Rate | |
| 0–6 breaths/min | 0.4 (0.1–1.3)* |
| 7–12 | 3.4 (2.0–5.6)* |
| 13–20 | 48.7 (43.5–54.0) |
| 21–30 | 37.9 (32.9–43.1) |
| >30 | 5.9 (4.2–8.2) |
| Unknown | 3.8 (2.4–5.9)* |
| Triage Systolic Blood Pressure | |
| 0–80 mmHg | 10.3 (8.0–13.2) |
| 81–100 | 42.9 (37.6–48.3) |
| 101–120 | 15.0 (11.3–19.7) |
| ≥120 | 29.6 (25.0–34.6) |
| Unknown | 2.2 (1.1–4.3)* |
| Length of ED Stay | |
| 0–2 hours | 13.0 (10.2–16.5) |
| >2–4 | 31.8 (26.7–37.4) |
| >4–8 | 41.6 (36.5–46.9) |
| >8 | 10.6 (7.7–14.3) |
| Unknown | 3.1 (1.7–5.4)* |
Estimates based upon <30 raw observations.
ED = Emergency Department.
Among Revised ED Sepsis visits, 72.47% (CI 67.43–77.00) resulted in admission to the hospital. Admission destinations were: ICU 33.91%, non-ICU 50.96%, and unknown 15.13%. Admitted ED sepsis patients were older than non-admitted ED sepsis patients (mean 67.3 [CI 65.1–69.6] vs 54.4 [CI 50.3–58.6] years). Among non-admitted ED sepsis visits, 11.15% (CI 6.36–18.83 vs. 9.6%) met both Original and qSOFA criteria, while 17.94% (CI 14.21–22.39) of those admitted met both criteria.
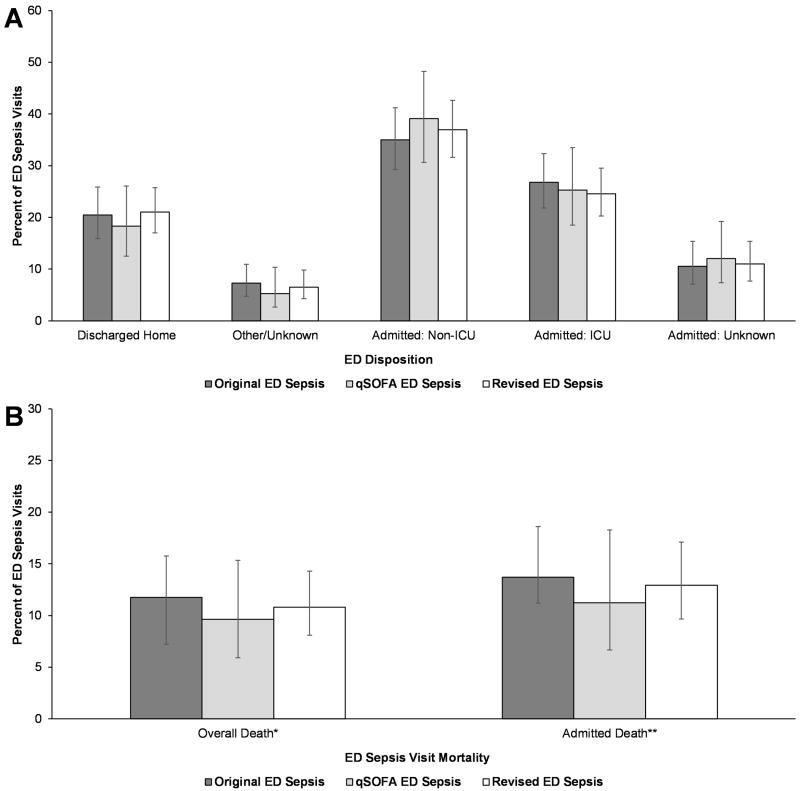
ED admission dispositions were similar between the Original, qSOFA and Revised ED Sepsis groups. (Figure 1A) Overall, 10.81% of Revised ED sepsis visits resulted in hospital death, with 12.94% of admitted sepsis cases dying in the hospital. Mortality was similar between ED Sepsis classifications. (Figure 1B) Compared to visits meeting only Original (19.9%) or qSOFA criteria (29.3%), sepsis visits meeting both Original and qSOFA sepsis criteria were more likely to be admitted to the ICU (45.4%). (Appendix 5)
FIGURE 1.
ED Disposition and Mortality by Sepsis Classification, 2009–2011. Other/Unknown disposition includes transfer, ED death, left ED, or unknown. *Includes death in ED or after hospital admission. **Includes death among those admitted. ED = Emergency Department; qSOFA = “quick” sepsis-related organ failure assessment; ICU = intensive care unit.
DISCUSSION
Epidemiologic information is essential to guide the care of acute care conditions, indicating the number and characteristics of the affected patients, the clinical settings and conditions, and associated complications and outcomes. Sepsis care is extremely complex, entailing early recognition and the management of intravenous fluids, antibiotics and vasopressors (20). As the venue for the initial arrival, assessment and care of critically ill patients, the ED is well positioned to play a pivotal role in sepsis care. The prior Rivers Early Goal Directed Therapy trial and the more recent ProCESS, ARISE and PROMISE trials underscore the importance of ED care in influencing downstream sepsis outcomes (3, 5, 21). Our study using the most contemporary available data and updated classification strategies affirms the huge persistent burden of sepsis upon US ED’s, comprising almost 850,000 adult ED visits annually or approximately 1 of every 120 adult ED visits. The acuity of these visits was high, with over 70% admitted to the hospital and nearly one fourth admitted to the ICU. These results underscore the importance of and great opportunities for leveraging the ED in organized strategies to reduce the societal burden of sepsis.
Using 2001–2004 NHAMCS data, we previously estimated the presence of 570,000 annual adult ED severe sepsis visits in the US (6). Our current estimate of 850,000 adult ED sepsis cases using 2009–2011 NHAMCS data is 50% higher than this prior report. There are numerous reasons for these distinctions. Sepsis-3 proposed qSOFA as a method for identifying patients with serious infection at high risk of poor outcomes. Extending upon this concept, we incorporated [serious infection + ≥2 qSOFA criteria] as an additional indicator of sepsis, resulting in the identification of an additional 182,549 sepsis cases. Numerous sepsis clinical initiatives, such as the international Surviving Sepsis Campaign, were promulgated during this intervening period and may have influenced sepsis detection, increasing the total number of identified sepsis cases (20). Medical record documentation and coding practices may have similarly evolved, increasing the documentation and coding of sepsis (8–10). The increased number of ED sepsis cases may also reflect the rise in the total number of annual adult ED visits from 83 to 103 million (15). Although our older study utilized the term “severe sepsis,” the definition closely follows the [infection + organ dysfunction] construct promoted by the current Sepsis-3 guidelines.
Intended to efficiently identify serious infection patients outside of the ICU at high risk of poor outcomes, the qSOFA criteria have been the subject of considerable controversy (11, 22) Our study provides important insights regarding the use of qSOFA criteria in characterizing ED sepsis epidemiology. Our study affirms that qSOFA is not suitable as a sole strategy for ED sepsis surveillance, as the use of qSOFA alone identified less than half of the potential ED sepsis cases. However, our application of the combination [serious infection + ≥2 qSOFA criteria] led to the detection of additional sepsis cases in the NHAMCS data set. The ED disposition and outcomes were similar between qSOFA and non-qSOFA sepsis cases, which contradicts the assumption that qSOFA would encompass higher acuity cases. However, in the context of this epidemiologic study, the similar outcomes between qSOFA and non-qSOFA sepsis cases may actually be a strength, supporting the use of qSOFA as an additional strategy for identifying sepsis cases. We have previously illustrated the utility of qSOFA in characterizing community-acquired sepsis susceptibility and mortality (23). We note that ED Sepsis cases fulfilling both Original and qSOFA criteria exhibited higher rates of ICU admission than those with either criteria alone, suggesting synergy between the two classification approaches.
Our observations affirm key observations about adult ED sepsis patients. Over half of ED sepsis patients were >65 years old. Older patients are challenging in sepsis resuscitation due to their frailty, multiple comorbidities, limited cardiovascular reserve, and atypical presentations (24, 25). Only one-sixth of ED sepsis patients were black, supporting current observations of higher sepsis risk among whites than blacks (26). Over half of ED sepsis patients arrived by EMS, highlighting the tremendous opportunity to leverage EMS as a resource for advance the prehospital recognition and treatment of sepsis (27). Almost 40% of ED sepsis cases occurred in the South census region, an observation consistent with our prior observations of increase sepsis incidence and mortality in the Southeastern US (28, 29). The most common infections diagnoses were pulmonary and genitourinary infections. Over one-third of cases presented with a triage SBP ≤90 mmHg, which is important given the newest recommendations for pressor use in sepsis treatment (20). Finally, over half of ED sepsis cases spent more than 4 hours in the ED, which is important given the growing challenges with ED overcrowding nationally (15, 30).
LIMITATIONS
One-fourth of the sepsis patients in this series were not admitted to the hospital. While it is conceivable for sepsis patients to have received effective resuscitation in the ED, this number is higher than expected. Furthermore, our observed sepsis mortality (13% of admitted patients) seems low compared with recent clinical trials (3, 5, 21). However, the latter studies enrolled only patients with septic shock. These observations reflect the heterogeneous nature of patients with sepsis receiving care across US EDs. Additional prospective study is needed to validate these observations.
NHAMCS is a probability sample data set and does not represent true surveillance of all US ED visits. The NHAMCS data set contained only three diagnoses; with a larger number of ED diagnoses, our detection of sepsis would have been higher. Results of definitive tests verifying the presence of an serious infection such as x-ray interpretations or blood cultures were not available. Laboratory values were not available, and hence we could not ascertain SOFA scores and acute kidney injury. Only triage vital signs were available – repeat physiologic measures were not available, so it is possible that we missed sepsis developing later during a hospital stay. While we were able to identify hospital survival, measures for risk adjustment were not available. Data on processes of ED care such as fluid resuscitation and the timeliness of antibiotic administration are not available. Our analysis focuses on the ED and cannot be extrapolated to other areas of hospital care.
CONCLUSION
Sepsis presents a continued major burden to US Emergency Departments, affecting up to nearly 850,000 ED visits annually. Updated sepsis classifications may impact estimates of national ED sepsis epidemiology.
Supplementary Material
Acknowledgments
FINANCIAL SUPPORT AND ACKNOWLEDGEMENTS
Dr. Wang received support from grant R01-NR012726 from the National Institute for Nursing Research.
Copyright form disclosure: Drs. Wang and Donnelly received support for article research from the National Institutes of Health.
Footnotes
Author Contributions:
HEW and JPD conceived the study. HEW and JPD conducted the analysis. All authors critically reviewed the results. HEW drafted the manuscript and all authors contributed to its critical review. HEW assumes overall responsibility for the paper.
CONFLICTS OF INTEREST
The authors do not report any related conflicts of interest.
Dr. Jones has disclosed that she does not have any potential conflicts of interest.
References
- 1.Dellinger RP, Levy MM, Rhodes A, et al. Surviving Sepsis Campaign: International Guidelines for Management of Severe Sepsis and Septic Shock: 2012. Critical care medicine. 2013;41(2):580–637. doi: 10.1097/CCM.0b013e31827e83af. [DOI] [PubMed] [Google Scholar]
- 2.Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. The New England journal of medicine. 2001;345(19):1368–1377. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- 3.Peake SL, Delaney A, Bailey M, et al. Arise Investigators. Anzics Clinical Trials Group. Goal-directed resuscitation for patients with early septic shock. The New England journal of medicine. 2014;371(16):1496–1506. doi: 10.1056/NEJMoa1404380. [DOI] [PubMed] [Google Scholar]
- 4.Mouncey PR, Osborn TM, Power GS, et al. Trial of early, goal-directed resuscitation for septic shock. The New England journal of medicine. 2015;372(14):1301–1311. doi: 10.1056/NEJMoa1500896. [DOI] [PubMed] [Google Scholar]
- 5.Yealy DM, Kellum JA, Huang DT, et al. ProCESS Investigators. A randomized trial of protocol-based care for early septic shock. The New England journal of medicine. 2014;370(18):1683–1693. doi: 10.1056/NEJMoa1401602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang HE, Shapiro NI, Angus DC, et al. National estimates of severe sepsis in United States emergency departments. Critical care medicine. 2007;35(8):1928–1936. doi: 10.1097/01.CCM.0000277043.85378.C1. [DOI] [PubMed] [Google Scholar]
- 7.Faust JS, Weingart SD. The Past, Present, and Future of the Centers for Medicare and Medicaid Services Quality Measure SEP-1: The Early Management Bundle for Severe Sepsis/Septic Shock. Emerg Med Clin North Am. 2017;35(1):219–231. doi: 10.1016/j.emc.2016.09.006. [DOI] [PubMed] [Google Scholar]
- 8.Gohil SK, Cao C, Phelan M, et al. Impact of Policies on the Rise in Sepsis Incidence, 2000–2010. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2016;62(6):695–703. doi: 10.1093/cid/civ1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lindenauer PK, Lagu T, Shieh MS, et al. Association of diagnostic coding with trends in hospitalizations and mortality of patients with pneumonia, 2003–2009. JAMA : the journal of the American Medical Association. 2012;307(13):1405–1413. doi: 10.1001/jama.2012.384. [DOI] [PubMed] [Google Scholar]
- 10.Thomas BS, Jafarzadeh SR, Warren DK, et al. Temporal trends in the systemic inflammatory response syndrome, sepsis, and medical coding of sepsis. BMC anesthesiology. 2015;15:169. doi: 10.1186/s12871-015-0148-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Seymour CW, Liu VX, Iwashyna TJ, et al. Assessment of Clinical Criteria for Sepsis: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA : the journal of the American Medical Association. 2016;315(8):762–774. doi: 10.1001/jama.2016.0288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA : the journal of the American Medical Association. 2016;315(8):801–810. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Angus DC, Seymour CW, Coopersmith CM, et al. A Framework for the Development and Interpretation of Different Sepsis Definitions and Clinical Criteria. Critical care medicine. 2016;44(3):e113–121. doi: 10.1097/CCM.0000000000001730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seymour CW, Coopersmith CM, Deutschman CS, et al. Application of a Framework to Assess the Usefulness of Alternative Sepsis Criteria. Critical care medicine. 2016;44(3):e122–130. doi: 10.1097/CCM.0000000000001724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention, National Center for Health Statistics. [cited 2017 March 27];Emergency Department Visits. 2017 Available from: https://www.cdc.gov/nchs/fastats/emergency-department.htm.
- 16.Walkey AJ, Wiener RS, Ghobrial JM, et al. Incident stroke and mortality associated with new-onset atrial fibrillation in patients hospitalized with severe sepsis. JAMA : the journal of the American Medical Association. 2011;306(20):2248–2254. doi: 10.1001/jama.2011.1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shankar-Hari M, Phillips GS, Levy ML, et al. Developing a New Definition and Assessing New Clinical Criteria for Septic Shock: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA : the journal of the American Medical Association. 2016;315(8):775–787. doi: 10.1001/jama.2016.0289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Angus DC, Linde-Zwirble WT, Lidicker J, et al. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Critical care medicine. 2001;29(7):1303–1310. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 19.Hing E, Gousen S, Shimizu I, et al. Guide to using masked design variables to estimate standard errors in public use files of the National Ambulatory Medical Care Survey and the National Hospital Ambulatory Medical Care Survey. Inquiry : a journal of medical care organization, provision and financing. 2003;40(4):401–415. doi: 10.5034/inquiryjrnl_40.4.401. [DOI] [PubMed] [Google Scholar]
- 20.Dellinger RP, Levy MM, Rhodes A, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Critical care medicine. 2013;41(2):580–637. doi: 10.1097/CCM.0b013e31827e83af. [DOI] [PubMed] [Google Scholar]
- 21.Mouncey PR, Power GS, Coats TJ. Early, Goal-Directed Resuscitation for Septic Shock. The New England journal of medicine. 2015;373(6):577–578. doi: 10.1056/NEJMc1506514. [DOI] [PubMed] [Google Scholar]
- 22.Vincent JL, Martin GS, Levy MM. qSOFA does not replace SIRS in the definition of sepsis. Crit Care. 2016;20(1):210. doi: 10.1186/s13054-016-1389-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Donnelly JP, Safford MM, Shapiro NI, et al. Application of the Third International Consensus Definitions for Sepsis (Sepsis-3) Classification: a retrospective population-based cohort study. The Lancet infectious diseases. 2017 doi: 10.1016/S1473-3099(17)30117-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carpenter CR, Shah MN, Hustey FM, et al. High yield research opportunities in geriatric emergency medicine: prehospital care, delirium, adverse drug events, and falls. The journals of gerontology Series A, Biological sciences and medical sciences. 2011;66(7):775–783. doi: 10.1093/gerona/glr040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Carpenter CR, Platts-Mills TF. Evolving prehospital, emergency department, and "inpatient" management models for geriatric emergencies. Clinics in geriatric medicine. 2013;29(1):31–47. doi: 10.1016/j.cger.2012.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moore JX, Donnelly JP, Griffin R, et al. Black-white racial disparities in sepsis: a prospective analysis of the REasons for Geographic And Racial Differences in Stroke (REGARDS) cohort. Crit Care. 2015;19:279. doi: 10.1186/s13054-015-0992-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang HE, Weaver MD, Shapiro NI, et al. Opportunities for Emergency Medical Services care of sepsis. Resuscitation. 2010;81(2):193–197. doi: 10.1016/j.resuscitation.2009.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang HE, Devereaux RS, Yealy DM, et al. National variation in United States sepsis mortality: a descriptive study. International journal of health geographics. 2010;9:9. doi: 10.1186/1476-072X-9-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moore JX, Donnelly JP, Griffin R, et al. Defining Sepsis Mortality Clusters in the United States. Critical care medicine. 2016;44(7):1380–1387. doi: 10.1097/CCM.0000000000001665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Weiss SJ, Derlet R, Arndahl J, et al. Estimating the degree of emergency department overcrowding in academic medical centers: results of the National ED Overcrowding Study (NEDOCS) Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2004;11(1):38–50. doi: 10.1197/j.aem.2003.07.017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.