Abstract
Introduction
One of the criticisms of rehabilitation techniques is their limited application to the patient’s daily life. In the past, cinema has been used as a psychiatric rehabilitation tool, with the primary objective of facilitating training in social abilities and communication. In this study, we consider the use of film not only as a clinical recovery tool but also as a novel cognitive recovery tool for additional rehabilitation not only for communication and social abilities but also for all of the basic cognitive and social cognition processes.
Methods
In this randomized clinical trial, 48 patients with schizophrenia were assigned to an experimental or control group. Both of the groups received treatment sessions that included viewing episodes of the television series The Sopranos. Next, the experimental group participated in a structured cognitive training session that featured questions and exercises based on the episodes. The control group participated in an idea-sharing session (of the same duration and frequency) about what the group members saw in the episode.
Results
At the end of the treatment, both the positive and negative clinical symptoms of the experimental group improved significantly compared with the control group. However, this improvement was not observed in basic or social cognitive functions.
Discussion
A brief intervention based on transforming the activities of daily life can be an effective tool for psychiatric rehabilitation. However, the study’s current characteristics and sample did not produce benefits in cognitive parameters.
Keywords: Schizophrenia, Cognition, Film, Psychiatric rehabilitation, Functionality
1. Introduction
Patients with schizophrenia are characterized by the presence of cognitive problems in their daily lives (Harvey and Bowie, 2005). Their functioning in standard activities such as employment, living independently, or maintaining normal social activity is very limited (Harvey et al., 2010), and pharmacological treatments have little effect on their cognitive and functional recovery. Consequently, common attempts at intervention focus on cognitive remediation and other psychiatric rehabilitation alternatives.
There is a line of investigation regarding cognition in schizophrenia based on the development and implementation of evaluation techniques designed to promote autonomic function in this group of patients. In the same fashion that neuropsychological testing progresses toward methods more concerned with daily life (Ruse et al., 2014), cognitive remediation increasingly tends to introduce methods relating to the patient’s real life. Traditionally, attempts to carry out cognitive remediation relevant to the patient’s daily life have adopted a top-down focus that has been criticized for its limitations (Jardri and Deneve, 2013). The primary difficulty of these approaches is that they neglect training in basic cognitive functions (such as attention, language, and memory), and as a result, the patient is not guaranteed sufficient recovery of those functions, which help in the successful execution of superior, more complex processes. However, although bottom-up approaches accomplish such training, they have a limited capacity to compensate for daily acquisitions in the patient’s real life. Far from being a dead end, this challenge has prompted authors to develop appropriate methodologies that include the best of each approach and target matters that the patients can develop in a normalized life.
More than a century ago, the appearance of film as a form of artistic expression evolved together with the globalization of society, which converted film into both a social phenomenon of the masses and a tool of cognitive, artistic, audiovisual, and social development (Bordwell et al., 1997, Cook, 1981). According to Dudai (2012), the historical success of cinema is due to its status as a unique art form that integrates, exploits, and promotes the cognitive faculties of the human brain: working memory (WM), the capacity to mentally travel through time (MTT), and the capacity to travel through the emotions. Based on this approach, the author proposes that film may be studied through neurocerebral and neurocognitive substrates. The ability to follow and understand a movie requires, inter alia, visuospatial capacity, phonological and multisensory competency, efforts in WM, language, episodic memory, mental management of time that sometimes flows in a non-linear fashion, management of concentrated attention, management of temporo-spatial coordinates, and management of social empathy with the characters (Dudai, 2012). All of these cognitive capacities together, whether simple or more complex, entail high cognitive demand and enable us to understand why patients with cerebral lesions or problems make functional complaints about difficulty following a movie.
In people’s lives, cinema represents an activity that incorporates fictional stories and contexts that are in some way close to an individual’s realities through the representation of behavior and the transmission of emotion (Bellour, 2009). Accordingly, a movie offers an intermediate context in the gap between real life and fiction. Movie showings have traditionally been used in psychiatric rehabilitation contexts because of movies’ ability to effectively reproduce both real situations and situations that are close to reality (Hasson et al., 2008a, Hasson et al., 2008b). The results of some studies that have used film in rehabilitation report benefits in clinical symptoms, state of mind, and patients’ social abilities (Gelkopf et al., 2006).
Encouraged by these reported benefits, a group from Madrid’s Puerta del Hierro Hospital developed a structured method of cognitive remediation based upon fictional cinema and the famous series The Sopranos. This method is based on both film analysis theory (Aumont and Marie, 1988, Goliot-Lété and Vanoye, 2012) and the principle of cognitive remediation (Penadés and Gastó, 2010, Roder and Medalia, 2010, Roberts and Penn, 2013).
Adopting this approach, our team designed a clinical trial using film to evaluate the effect of cognitive remediation in patients with schizophrenia. This trial also used The Sopranos, which contains structured, homogeneous episodes that enable an analysis of the impact of this technique on basic cognition, social cognition, clinical symptoms, and functionality. Our hypothesis is that the group that watches the series, in conjunction with the structured analytic techniques and cognitive training, will improve its general cognitive capacity and functional autonomy with respect to the control group.
2. Method
2.1. Participants
Forty-eight hospitalized patients with schizophrenia were recruited from both the Refractory Psychosis Unit of the Alava Psychiatric Hospital and the Puerta de Hierro University Hospital in Majadahonda, Madrid (both in Spain) in a collaborative study with the University of Deusto Psychology Department. The inclusion criteria were the following: between 18 and 75 years of age and fulfilling the diagnostic criteria of schizophrenia according to the American Psychiatric Association’s Diagnostic and Statistical Manual DSM-IV-TR. The exclusion criteria included an age of less than 18 years or more than 75 years, evidence of drug or alcohol abuse within the previous 30 days, a currently outstanding episode of seasonal affective disorder, previous history of significant loss of consciousness, mental retardation, history of a relevant neurological or medical episode, and participation in another clinical trial. Both groups received the standard treatment, which includes individual case management and medical reviews.
All of the patients were stable at the time of their participation in the study and received pharmacological treatment during their participation.
2.2. Approval of protocol, registration, and informed consent
All of the participants voluntarily agreed to participate and signed the informed consent of the study. The study’s protocol was approved by the University of Deusto’s Committee of Ethics and Research.
2.3. Measures of clinical, cognitive, and functional evaluation
Twelve days after entry, all of the patients were evaluated from a clinical, cognitive, and functional point of view. The clinical evaluation included the SCID-I semi-structured diagnostic interview for psychosis: Spanish version (First et al., 1997), the Positive and Negative Syndrome Scale (PANSS, Spanish version) (Peralta Martín and Cuesta Zorita, 1994), the Scale to Assess Unawareness in Mental Disorder (SUMD) (Amador et al., 1994), and the Clinical Global Impressions Scale (CGI) (Guy, 1970).
The neuropsychological evaluation included the Trail-Making Test Parts A and B (Reitan and Wolfson, 1985), BACS test (Keefe et al., 2004), the Hopkins Verbal Learning and Memory test (HVLT) (Brandt and Benedict, 2001), the Brief Visuospatial Memory Test-Revised (BVMT-R) (Benedict et al., 1996); the Letters and Numbers test, the WAIS-III mazes (Wechsler, 1997), and a verbal and phonological fluency test (Peña-Casanova, 1990). Each participant’s social cognition performance was objectively evaluated using the Mayer-Salovey-Caruso Emotional Intelligence Test -MSCEIT (Mayer et al., 2002), the Reading the Mind in the Eyes Test (Baron‐Cohen et al., 2001), the Faux-Pas Recognition Test, the Internal, Personal, and Situational Attributions Questionnaire (IPSAQ) (Kinderman and Bentall, 1996). In this fashion, we obtained measurements of the four principal factors that constitute social cognition: emotion perception, social perception, theory of mind, and attributional style. The total scores on the WAIS-III Vocabulary subtests were taken as an estimation of the participant’s premorbid intellectual performance.
Each patient’s functional level was evaluated according to the score obtained on the Personal and Social Performance Scale (PSP) (Garcia-Portilla et al., 2013).
2.4. Procedure
First, an analysis of statistical power was conducted to determine the size of the sample based on previous studies of cognitive remediation with the same group (Sánchez et al., 2013). A sample of 40 subjects, 20 in each group, was sufficient to obtain an effect size of 0.88, which detects a difference in cognitive remediation and clinical variables with 80% power and a 5% confidence level.
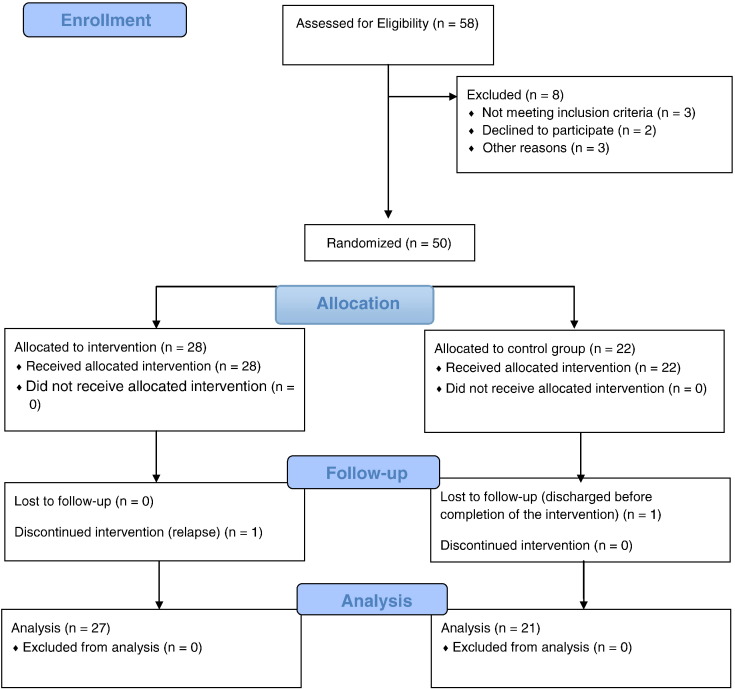
The design of the study was a randomized trial. Recruitment of the participants was carried out between September of 2011 and March of 2014. Following admission to the study, a simple random assignment (tossing a coin) was conducted to place each participant in either the experimental (n = 28) or control (n = 22) group (see Fig. 1). The post-treatment evaluation occurred at a maximum of one week after each patient completed his or her participation in the groups. All of the evaluators were blind to the experimental or control condition in which they encountered the participants. For ethical reasons, all of the participants in the control group were offered the opportunity to participate in a group that received the experimental intervention once the study was finished.
Fig. 1.
Flow diagram following CONSORT 2010 recommendations.
2.5. Intervention
By consensus, the first season of the television series The Sopranos was selected from a set of possible television series due to its quality, cognitive-affective content, display of interpersonal relationships, and widespread public acceptance. The program was implemented in a group format using pencil-and-paper tasks. All of the participants received 26 one-hour and 45-minute sessions over a period of 13 weeks. Two weekly sessions, each separated by 48 hours, were conducted. The structure of the sessions, as along with the design of the treatment program, was crafted by the Psychiatry Services team at the Puerta del Hierro Hospital in Madrid.
The experimental group (EG) received specific, guided training based on a systematic analysis of the series. After viewing each episode, a systematic discussion of the footage was held and the worked scenes were projected again, this time including the corrections viewed in the first showing. The basis of this method is inspired by film analysis theory. Film analysis is an intellectual exercise of fragmenting a movie into its most basic elements to establish and break down the relationships among them.
In the control group (CG), each patient spoke about his or her favorite scene. Afterwards, a group discussion occurred without any type of standardized guidance from the therapist. Both the experimental and control group sessions had the same duration and frequency.
2.6. Statistical analysis
The normality of the data was examined using the Kolmogorov-Smirnov test. The categorical data were analyzed using a chi-square test. The multivariate analysis of variance (MANOVA) repeated measures analysis included the neuropsychological, clinical, and functional test results obtained in the two evaluation times as an intra-group factor, and the group type (experimental vs. control) was included as an inter-group factor. The significance level was established at 0.05. All of the tests were bilateral. All of the statistical analyses were conducted using version 21 of the Statistical Package for the Social Sciences statistical program (SPSS).
3. Results
3.1. Sociodemographic characteristics of the groups
The sociodemographic characteristics of the experimental (EG) and control (CG) groups are shown in Table 1. The general sample was a group of patients with chronic schizophrenia who had severe symptomatology and a high number of hospitalizations. The differences between the groups were analyzed to ensure good randomization. We did not encounter significant differences between the groups in any of the sociodemographic variables analyzed. Both of the groups were equivalent in age, sex, and premorbid adjustment. There were also no significant differences between the groups in clinical characteristics such as age at the first diagnosis of schizophrenia, number of previous hospitalizations, or presence of diagnostic subtypes. The average dose of antipsychotics (mg/day of chlorpromazine equivalents) was similar at the baseline (F = 0.54 and p = 0.61) and the end of the intervention (F = 3.83 and p = 0.06).
Table 1.
Distinguishing sociodemographics and diagnostics of the participants by group. Average (standard deviation).
| Experimental group | Control group | Group differences | p | |
|---|---|---|---|---|
| Age (years) | 35.93 (8.1) | 32.52 (9.8) | F = 1.735 | 0.194 |
| Education (years) | 9.23 (2.7) | 10.24 (2.8) | F = 2.17 | 0.146 |
| Sex: n (%) | ||||
| Men | 20 (57.0%) | 15 (71.4%) | χ2 = 0.838 | 0.546 |
| Women | 7 (43%) | 6 (28.6%) | ||
| Time of disease progression (days) | 145,8 (92,3) | 125,1 (91,) | F = 0.598 | 0.,443 |
| Number of previous hospitalizations | 3.2 (2.3) | 3.33 (3.2) | F = 0.035 | 0.853 |
| WAIS-III vocabulary | 38,93 (6.01) | 36,71 (8.6) | F = 1.12 | 0.301 |
| Premorbid adjustment (Cannon-Spoor) | 49.64 (25.5) | 46.75 (22.2) | F = 0.30 | 0.582 |
| Doses of psychiatric medication (converted to mg/day of chlorpromazine) | 695.09 (362.6) | 911.88 (922.9) | F = 1.77 | 0.186 |
| DSM-IV-TR: n (%) | ||||
| Paranoid | 29 (80.6%) | 40 (77.9%) | χ2 = 0.73 | 0.866 |
| Disorganized | 4 (11.1%) | 3 (6.3%) | ||
| Residual | 2 (5.6%) | 3 (6.3%) | ||
| Unspecified | 1 (2.8) | 2 (4.2%) | ||
| Occupation: n (%) | ||||
| Employed | 3 (8.3%) | 2 (4.2%) | χ2 = 2.35 | 0.308 |
| Unemployed | 9 (25.0%) | 7 (14.6%) | ||
| Disabled | 24 (66.7%) | 39 (81.3%) | ||
| Marital Status: n (%) | ||||
| Single | 33 (91.7%) | 45 (93.8%) | χ2 = 0.13 | 0.935 |
| Married | 1 (2.1%) | 1 (2.8%) | ||
| Separated or divorced | 2 (5.6%) | 2 (4.2%) |
Note. DSM-IV-TR = Diagnostic and Statistical Manual of Mental Disorders 4th edition, Revised Text.
3.2. Changes between EG and CG after the intervention
Except for letters and numbers, no statistically significant differences were found between the two groups in the pre-treatment evaluation in any of the analyzed variables (see Table 2, Table 3). The pattern of cognitive deterioration observed at baseline in both groups did not change significantly in either group after the intervention (see Table 2). This absence of change was reflected in the results obtained from both basic and social cognition. The functional performance analyzed through results obtained in the personal and social performance (PSP) scale did not show significant variations before or after the intervention in either of the two groups (see Table 2 for more details).
Table 2.
Changes in basic cognition, social cognition, and functionality between baseline and post-treatment in the experimental and control groups.
| Average (SD) |
Differences Pre-treatment |
Primary effect Group |
Primary effect Time |
Interaction group × time |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Experimental group | Control group | F | p | F | p | F | P | F | p | ||
| PSPtotal | Pre | 52.67 (2.7) | 55.00 (3.0) | 0.49 | 0.484 | 0.15 | 0.71 | 8.74 | 0.005 | 0.39 | 0.538 |
| Post | 57.42 (2.9) | 58.10 (3.2) | |||||||||
| TMT-A T° | Pre | 50.08 (4.7) | 43.67 (4.3) | 0.95 | 0.334 | 0.11 | 0.75 | 3.79 | 0.059 | 0.17 | 0.686 |
| Post | 47.00 (5.1) | 42.80 (4.7) | |||||||||
| Bacs T° | Pre | 38.50 (1.9) | 39.50 (2.1) | 0.29 | 0.590 | 0.00 | 0.97 | 4.56 | 0.039 | 0.68 | 0.413 |
| Post | 42.46 (2.6) | 41.25 (2.8) | |||||||||
| HVLT total | Pre | 20.42 (1.1) | 21.25 (1.1) | 0.27 | 0.601 | 0.14 | 0.71 | 6.18 | 0.017 | 1.71 | 0.198 |
| Post | 22.83 (1.1) | 22.00 (1.1) | |||||||||
| BVLT total | Pre | 17.42 (1.7) | 19.45 (1.7) | 0.97 | 0.328 | 0.39 | 0.54 | 0.11 | 0.744 | 0.04 | 0.841 |
| Post | 17.83 (1.7) | 19.50 (1.8) | |||||||||
| Letters and numbers | Pre | 11.63 (0.5) | 13.350 (0.6) | 4.85 | 0.033 | 3.61 | 0.06 | 1.47 | 0.232 | 0.07 | 0.792 |
| Post | 11.21 (0.7) | 12.70 (0.8) | |||||||||
| Mazes | Pre | 11.04 (1.3) | 12.15 (1.5) | 0.84 | 0.363 | 1.02 | 0.32 | 7.21 | 0.010 | 2.43 | 0.127 |
| Post | 11.67 (1.4) | 14.50 (1.5) | |||||||||
| Verbal fluency | Pre | 16.79 (0.7) | 18.20 (0.8) | 1.34 | 0.252 | 0.73 | 0.40 | 3.49 | 0.068 | 0.50 | 0.482 |
| Post | 18.46 (1.0) | 18.95 (1.0) | |||||||||
| MSCEIT | Pre | 86.91 (1.7) | 84.57 (1.9) | 0.46 | 0.497 | 0.60 | 0.44 | 1.45 | 0.235 | 0.01 | 0.914 |
| Post | 88.53 (2.5) | 86.52 (2.7) | |||||||||
| Mind reading | Pre | 21.29 (0.8) | 19.10 (0.9) | 3.85 | 0.056 | 0.89 | 0.35 | 0.72 | 0.400 | 3.60 | 0.015 |
| Post | 20.63 (0.9) | 20.85 (0.8) | |||||||||
| Faux-pas recognition | Pre | 29.50 (3.3) | 32.35 (3.6) | 0.14 | 0.703 | 0.58 | 0.45 | 4.64 | 0.037 | 0.18 | 0.004 |
| Post | 33.13 (3.9) | 37.75 (4.3) | |||||||||
Note. SD = Standard; PSPtotal = Overall score in the Personal and Social Performance test (PSP); TMT-AT° = Total time in seconds to complete part A of the Trail-Making test; BacsT° = Total time in seconds to complete BACS; HVLT total = Total number of words after three training period trials of the Hopkins Verbal Learning and Memory Test; BVLT total = Total number of drawings after three training period trials of the Brief Visual Learning and Memory test; Letters and Numbers = Total number of items in the Letters and Numbers subtest of WAIS-III; Mazes = Total time in seconds of the maze subtest of WAIS-III; Verbal fluency = Total number of words evoked in one minute; MSCEIT = Total score on the Mayer-Salovey-Caruso Emotional Intelligence Test; Mind reading = Total score on the Reading the Mind in the Eyes test; Faux pas recognition = Total score in the faux-pas recognition test.
Table 3.
Changes in clinical symptoms between baseline and post-treatment in the experimental and control groups.
| Average (SD) |
Differences Pre-treatment |
Primary effect Group |
Primary effect Time |
Interaction group × time |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Experimental group | Control group | F | p | F | p | F | P | F | p | ||
| Positive symptoms (PANSS) | Pre | 15.17 (1.2) | 12.85 (1.3) | 1.81 | 0.186 | 0.40 | 0.84 | 8.80 | 0.005 | 6.71 | 0.013 |
| Post | 10.75 (0.9) | 12.63 (0.9) | |||||||||
| Negative symptoms (PANSS) | Pre | 21.54 (1.6) | 17.91 (1.7) | 2.39 | 0.129 | 0.22 | 0.64 | 28.86 | 0.000 | 12.9 | 0.001 |
| Post | 15.00 (1.4) | 16.65 (1.5) | |||||||||
| General psychopathology (PANSS) | Pre | 37.63 (2.8) | 32.35 (3.1) | 1.56 | 0.217 | 0.32 | 0.56 | 15.74 | < 0.001 | 6.39 | 0.413 |
| Post | 28.83 (1.8) | 30.40 (2.0) | |||||||||
| CGI | Pre | 4.10 (0.83) | 3.87 (0.92) | 2.39 | 0.131 | 0.20 | 0.66 | 13.85 | 0.001 | 9.75 | 0.198 |
| Post | 3.33 (0.73) | 3.80 (1.01) | |||||||||
PANSS = Positive and Negative Syndrome Scale; CGI = Clinical General Impression Scale.
However, the experimental group showed a significant reduction of clinical symptoms measured by the PANSS in comparison with the control group. This change was objectively seen in positive (p < 0.005), negative (p < 0.000), and general symptoms (p < 0.000) (see Table 3).
4. Discussion
The design of the intervention program with cinema used in this sample of patients with schizophrenia is based both on principles of film analysis theory and on cognitive remediation, which intends to improve the clinical and cognitive situation of the population to which it is applied. Following its intensive use in our sample of participants, we did not observe any significant change in the realm of cognition, the participants’ more basic processes (attention, language, memory), or in their more complex processes of social cognition. Despite the fact that the structure, objective, and content of the sessions were mainly directed towards the search for remediation of the selected sample’s cognitive deficits, it seems that the mechanisms that would make such a recovery effective are not reflected in the employed method.
That notwithstanding, the practiced intervention with the experimental group did lead to an important change in the gravity of their clinical symptomatology. The reduction in clinical symptoms (positive and negative) was much higher than that observed in the control group, even though the rest of the interventions were ordinary. This fact is especially apparent in the negative symptoms, which are habitually more resistant to recovery through other therapeutic measures. Given that both groups shared the remainder of the variables during the clinical trial, we cannot attribute the symptom recovery in the experimental group to other factors such as the hours of attention received, the qualification of the therapists who intervened, or the type of pharmacological treatment used. In accordance with what other authors have identified in schizophrenia, it is more likely that the combination of pharmacological and psychological treatments together with the experimental intervention reinforced the symptomatological recovery (Fusar-Poli et al., 2014). In previous clinical trials, our group tested neuropsychological rehabilitation methods demonstrating combined efficacy in cognition and negative symptomatology (Sánchez et al., 2013). In the methodology with the Rehacop program, however, the reinforcement principles of bottom-up mechanisms were applied. In this clinical experiment, only top-down mechanisms were used. Further studies that directly compare the efficacy of these two methodologies in the processes of cognitive recovery in schizophrenia are necessary. Although some clinical groups claim the need for personalized treatment of the negative symptoms of patients with schizophrenia (Foussias et al., 2014), we have already used treatments applied in a group setting that seem efficient in reducing negative symptoms.
Despite this study’s presentation of promising data in terms of clinical changes exhibited by the patients, it also presents some limitations. The first is that this study lacks measurement scales for quality of life and other functional scales additional to the PSP. Future studies should measure the effect of this type of intervention on the aforementioned factors. The second limitation is that the measurement of negative symptoms was conducted with the traditional PANSS, whereas currently, and subsequent to the design of this study, there are more appropriate clinical scales available with less limitation for measurement of the same attributes.
The clinical profile of the patients requires mention. The severity of the profile has not been a factor in preventing improvement in clinical symptoms, but it is a factor in finding positive changes in cognition and functionality. Finally, a long-term, longitudinal follow-up would be convenient to analyze whether the observed clinical changes persist through time.
Conflict of Interest
The authors do not have any conflict of interest to declare in relation to this study.
Acknowledgements
The authors would like to thank Drs. Luis Caballero and Inés García and their entire team at the Puerta del Hierro Hospital in Madrid for sharing both their film analysis method applied to the series The Sopranos and the study’s experimental design.
References
- Amador X.F., Flaum M., Andreasen N.C., Strauss D.H. Awareness of illness in schizophrenia and schizoaffective and mood disorders. Arch. Gen. Psychiatry. 1994;51(10):826–836. doi: 10.1001/archpsyc.1994.03950100074007. [DOI] [PubMed] [Google Scholar]
- Aumont J., Marie M. Nathan; París: 1988. L'analyse des films. [Google Scholar]
- Baron‐Cohen S., Wheelwright S., Hill J., Raste Y., Plumb I. The “Reading the Mind in the Eyes” test revised version: A study with normal adults, and adults with Asperger syndrome or high‐functioning autism. J. Child Psychol. Psychiatry. 2001;42(2):241–251. [PubMed] [Google Scholar]
- Bellour R. POL; 2009. Le corps du cinéma: hypnoses, émotions, animalités. [Google Scholar]
- Benedict R.H., Schretlen D., Groninger L., Dobraski M., Shpritz B. Revision of the Brief Visuospatial Memory Test: studies of normal performance, reliability, and validity. Psychol. Assess. 1996;8(2):145. [Google Scholar]
- Bordwell D., Thompson K., Ashton J. McGraw-Hill; New York: 1997. Film art: an introduction. [Google Scholar]
- Brandt J., Benedict R.H.B. Psychological Assessment Resources; Lutz, FL: 2001. Hopkins Verbal Learning Test-Revised. [Google Scholar]
- Cook D.A. Norton; New York: 1981. A history of narrative film. [Google Scholar]
- Dudai Y. The cinema-cognition dialogue: a match made in brain. Front. Hum. Neurosci. 2012;6 doi: 10.3389/fnhum.2012.00248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First M.B., Spitzer R.L., Gibbon M., Williams J.B.W. American Psychiatric Press; Washington, DC: 1997. Structured Clinical Interview for DSM-IV Axis I Disorders-Clinical Version (SCID-CV) [Google Scholar]
- Foussias G., Siddiqui I., Fervaha G., Agid O., Remington G. Dissecting negative symptoms in schizophrenia: opportunities for translation into new treatments. J. Psychopharmacol. 2014 doi: 10.1177/0269881114562092. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P., Papanastasiou E., Stahl D., Rocchetti M., Carpenter W., Shergill S., McGuire P. Treatments of negative symptoms in schizophrenia: Meta-analysis of 168 randomized placebo-controlled trials. Schizophr. Bull. 2014 doi: 10.1093/schbul/sbu170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Portilla M.P., Gomar J.J., Bobes-Bascaran M.T., Menendez-Miranda I., Saiz P.A., Muniz J., Arango C., Patterson T.L., Harvey P.D., Bobes J., Goldberg T.E. Validation of a European Spanish-version of the University of California performance Skills Assessment (Sp-UPSA) in patients with schizophrenia and bipolar disorder. Schizophr. Res. 2013;150(2–3):421–426. doi: 10.1016/j.schres.2013.07.049. [DOI] [PubMed] [Google Scholar]
- Gelkopf M., Gonen B., Kurs R., Melamed Y., Bleich A. The effect of humorous movies on inpatients with chronic schizophrenia. J. Nerv. Ment. Dis. 2006;194(11):880–883. doi: 10.1097/01.nmd.0000243811.29997.f7. [DOI] [PubMed] [Google Scholar]
- Goliot-Lété A., Vanoye F. Armand Colin; 2012. Précis d'analyse filmique. [Google Scholar]
- Guy W. Manual for the ECDEU Assessment Battery. National Institute of Mental Health; Chevy Chase: 1970. CGI: Clinical global impressions. [Google Scholar]
- Harvey P.D., Bowie C.R. Late-life schizophrenia. What providers need to know. Director. 2005;13(2):90. (93-4) [PubMed] [Google Scholar]
- Harvey P.D., Wingo A.P., Burdick K.E., Baldessarini R.J. Cognition and disability in bipolar disorder: Lessons from schizophrenia research. Bipolar Disord. 2010;12(4):364–375. doi: 10.1111/j.1399-5618.2010.00831.x. [DOI] [PubMed] [Google Scholar]
- Hasson U., Furman O., Clark D., Dudai Y., Davachi L. Enhanced intersubject correlations during movie viewing correlate with successful episodic encoding. Neuron. 2008;57(3):452–462. doi: 10.1016/j.neuron.2007.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasson U., Landesman O., Knappmeyer B., Vallines I., Rubin N., Heeger D.J. Neurocinematics: The neuroscience of film. Projections. 2008;2(1):1–26. [Google Scholar]
- Jardri R., Deneve S. Circular inferences in schizophrenia. Brain. 2013;136(Pt 11):3227–3241. doi: 10.1093/brain/awt257. [DOI] [PubMed] [Google Scholar]
- Keefe R.S., Goldberg T.E., Harvey P.D., Gold J.M., Poe M.P., Coughenour L. The Brief Assessment of Cognition in Schizophrenia: reliability, sensitivity, and comparison with a standard neurocognitive battery. Schizophr. Res. 2004;68(2):283–297. doi: 10.1016/j.schres.2003.09.011. [DOI] [PubMed] [Google Scholar]
- Kinderman P., Bentall R.P. A new measure of causal locus: the internal, personal and situational attributions questionnaire. Personal. Individ. Differ. 1996;20(2):261–264. [Google Scholar]
- Mayer J.D., Salovey P., Caruso D.R. MHS; 2002. Mayer-Salovey-Caruso Emotional Intelligence Test: MSCEIT. Item booklet. [Google Scholar]
- Peña-Casanova J. Masson; Barcelona: 1990. Programa integrado de exploración neuropsicológica. Manual. [Google Scholar]
- Penadés R., Gastó C. Herder; 2010. El tratamiento de rehabilitación neurocognitiva en la esquizofrenia. [Google Scholar]
- Peralta Martín V., Cuesta Zorita M.J. Validación de la escala de los síndromes positivo y negativo (PANSS) en una muestra de esquizofrénicos españoles. Actas Luso Esp. Neurol. Psiquiatr. Cienc. Afines. 1994;22(4):171–177. [PubMed] [Google Scholar]
- Reitan R., Wolfson D. Neuropsychology Press; Tucson: 1985. The Haldstead-Reitan neuropsychological test battery. [Google Scholar]
- Roberts D.L., Penn D.L. Oxford University Press; 2013. Social cognition in schizophrenia: From evidence to treatment. [Google Scholar]
- Roder V., Medalia A. Karger Medical and Scientific Publishers; 2010. Neurocognition and social cognition in schizophrenia patients: basic concepts and treatment. [Google Scholar]
- Ruse S.A., Harvey P.D., Davis V.G., Atkins A.S., Fox K.H., Keefe R.S. Virtual reality functional capacity assessment in schizophrenia: Preliminary data regarding feasibility and correlations with cognitive and functional capacity performance. Schizophr. Res. Cogn. 2014;1(1):e21–e26. doi: 10.1016/j.scog.2014.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sánchez P., Peña J., Bengoetxea E., Ojeda N., Elizagárate E., Ezcurra J., Gutiérrez M. Improvements in negative symptoms and functional outcome after a New generation cognitive remediation program: A randomized controlled trial. Schizophr. Bull. 2013 doi: 10.1093/schbul/sbt057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D. Psychological Corporation; New York: 1997. WAIS-III manual: Wechsler adult intelligence scale-III. [Google Scholar]