Abstract
The EQ-5D-5L is a generic quality of life (QOL) measure widely used throughout the world, which has the advantage that it allows health state preferences to be elicited.
Aims
To examine if:
-
a)
Variation in the standardised reference period for EQ-5D-5L from “today” to “the last month” had a minimal clinically meaningful difference.
-
b)
EQ-5D-5L had convergent validity with a multidimensional pain measure in quantifying the impacts of pain.
Methods
As part of a larger study into the effectiveness and efficiency of care pathways for persistent oral facial pain (POFP) (http://research.ncl.ac.uk/deepstudy) participants with POFP (n=100) completed two versions of the EQ-5D-5L at the same time with different reference periods (‘Today’ versus ‘Last month’). Participants also completed the first section of the West-Haven Yale Multidimensional Pain inventory (v3) to assess convergent validity.
Two-tailed non-parametric inferential statistics, intra-class correlation coefficients (ICC), and within subject change scores were used to compare the two EQ-5D-5L versions. Convergent validity was assessed using Spearman Rho correlation coefficients.
Results
Health state valuations were significantly different (p<0.01), and there was good similarity between the two versions ICC 0.86 (95%CI 0.79-0.91). The within-subject mean change was 0.03 (95%CI 0.01-0.06). For convergent validity all relationships were significant (p<0.05), and in the expected directions.
Conclusion
EQ-5D demonstrates sufficient convergent validity to be used with POFP and a change in the standard reference period may be unnecessary if a multidimensional pain measure is also used.
Keywords: Quality of Life, Persistent orofacial pain, EQ-5D, Facial pain, Pain, Outcome
Introduction
Persistent (chronic) pain affecting the orofacial region is defined as pain lasting greater or equal to three months (1). It can be caused by any one of a heterogeneous group of conditions, which are either neuropathic, musculoskeletal, or neurovascular in origin (2). Given the heterogeneity of these conditions it has been necessary to construct instruments that measure the multidimensional nature of the biopsychosocial effects that persistent (orofacial) pain can exert. One of the most frequently used multidimensional instruments in persistent orofacial pain (POFP) over the last three decades is the West Haven Yale Multidimensional Pain Inventory (3).
Perhaps unsurprisingly, given the need for multidimensional pain inventories, POFP is known to affect oral health related quality of life (OHRQOL) and exert psychosocial impacts on sufferers (4–11). Only limited data exist on using generic quality of life (QOL) measures with the group of conditions comprising POFP (5, 9, 12–22) with the majority of these studies using the 36-item short form health survey (SF-36 (23)) (5, 9, 12–15, 17, 19–21) and only four studies using the EQ-5D to examine QOL in Trigeminal neuralgia amongst other conditions producing pain elsewhere in the body (11, 16, 18, 22).
The predominant use of condition, or disease-specific, OHRQOL measures in POFP is understandable given the advantages these instruments possess in terms of sensitivity and specificity for the impacts of the particular condition or disease (24–26), but it also means that, despite some conversion formula being suggested (27), it is difficult to compare the impact of POFP conditions with other (pain) conditions presenting elsewhere in the body. There are also currently no population norms available for the most frequently used OHRQOL measure in POFP the Oral Health Impact Profile (28) and therefore valuations of particular (oral) health states are currently impossible.
Both the SF-36 and the EQ-5D (29) have the capacity to generate health-state valuations from population norms although the former does so through a recently devised estimation process. Whilst the estimation process developed is robust there are concerns over the reliability of the tool amongst more severe conditions (30). Given recent OHRQOL data this is the situation expected in POFP (6). In contrast the EQ-5D has been shown to perform well in differentiating between severe health states (31). The EQ-5D was specifically designed to estimate health state preferences as the basis of calculation of quality adjusted life years (QALYs) and has extensive population norm data available from across Europe (32). QALYs are especially important in chronic conditions as they take into account both the quality, and quantity, of life and thereby permit comparison of different health care interventions’ using a common and consistent numeraire.
The latest iteration of EQ-5D, the EQ-5D-5L, examines limitations in five dimensions: mobility, pain/discomfort, self-care, anxiety/depression, and usual activities, by asking respondents to indicate their level of disability on a five item ordinal scale, with lower scores equating to less disability in that dimension. The standard reference period for the response is the respondent’s “own health state today”. Despite widespread use across a vast variety of other conditions the EQ-5D has received scant attention in the POFP literature (11, 16, 18, 22) and has never been employed with a heterogeneous group of POFP. The heterogeneity of POFP conditions means they can impact differently both at the individual patient level but also at a condition-level and may do so in a fluctuating manner over short periods of time. This study, therefore, aimed to examine whether:
-
a)
Variation in the standardised reference period for EQ-5D-5L from “today” to “the last month” produced minimum clinically meaningful differences (also known as the minimally important difference) in responses.
-
b)
EQ-5D-5L had convergent validity with a multidimensional pain measure (West-Haven Yale Multidimensional Pain Inventory [MPI] (3)) in quantifying the impacts of POFP.
Methods
This study is part of the larger and ongoing DEEP study (Developing Effective and Efficient care pathways in chronic Pain http://research.ncl.ac.uk/deepstudy) and received ethical approval from the UK NHS National Research Ethics Service Committee Leeds West (Ref 12-YH-0338). The DEEP study protocol is available on open access and contains full details of the methods of the overall programme of research (33). Details relevant to this particular part of the DEEP study are included below.
Participants and procedures
A convenience sample of consecutive patients was drawn from the community (general medical and dental practice) and hospital (specialist dental or medical) practice using the centres recruiting for the DEEP study (33). Consecutive, consenting, patients presenting with POFP defined as pain affecting the orofacial region for greater than or equal to three months were screened for eligibility using two validated screening instruments (34, 35). Patients were eligible if the screening indicated that the origin to their persisting pain was either of a musculoskeletal, neurological, or combined musculoskeletal/neurological origin (35) (34). Exclusion criteria were that the patient: lacked sufficient comprehension of the English language to complete the questionnaires or give informed consent; was less than eighteen years old; screened as only having Dentoalveolar pain (35).
Eligible patients were invited to participate and all gave written informed consent. All patients enrolled in the study received a structured baseline interview where the instruments used in the study were explained to them in a standardised fashion to ensure their comprehension. Patients then completed the instruments in their own time and sent them back in prepaid envelopes to the study team. Missing data identified within either instrument were followed up by phone-call with the participant and entered as appropriate to the participant’s verbal response prior to calculating summary scores.
Measures and instruments
Patients were issued with several questionnaire booklets in a standardised numerical order. Two of these questionnaire booklets are relevant to this particular study: one booklet contained the EQ-5D-5L, and the other booklet contained section one (severity, interference, life control, affective distress, support) of the multidimensional pain inventory version 3 (MPI) (3). Section one of the MPI contained the constructs of interest to test the convergent validity of the two versions of EQ-5D.
The EQ-5D-5L booklet had the EQ-5D-5L presented twice in a standardised order: once using the standard reference period of “…health state today” (TODAYQ), and the other iteration with the new reference period “…health state over the last month” (MONTHQ). All the other aspects of EQ-5D-5L remained unaltered (a good summary of EQ-5D can be found at http://www.euroqol.org).
Section one of the MPI was unaltered from the standard version 3 of the instrument. Both instruments’ summary scores were calculated in the standardised fashion as described in the literature (29, 36). The MPI summary scores were calculated using the item-response theory method (Rasch model of Version 3 of the MPI software and instrument). The health state valuations for EQ-5D-5L were calculated by firstly concatenating the response codes to each item to produce a final health state summary score ranging from 11111 (least disability) to 55555 (worst disability). This health state summary score was then compared to normative data sets to generate a health state valuation: ranging from -0.59 (state worse than death) through 0 (equivalent to being dead) up to 1 (perfect health) using the crosswalk data set for the UK population norms (37).
Data analysis
An a priori power calculation determined that in order to detect a small to moderate effect size of 0.3 (38), with 80% confidence of detecting a type I error of 5%, using paired, two tailed, inferential statistics, ninety patients would be required to complete the two versions of the EQ-5D questionnaire. One hundred patients were therefore recruited to allow for a 10% drop-out rate which was based on the authors’ previous experiences with this type of research.
All data analyses were conducted with STATA, Release 12 (Stata Statistical Software, College Station, TX, USA). The main aim of the analysis was to examine differences between the two versions of the EQ-5D-5L and compare these to the clinically meaningful difference (CMD) as determined in the literature. The secondary aim of the analyses was to examine the two versions’ convergent validity with the outputs from section one of the MPIv3.
Simple descriptive statistics were used to help present and examine the data. Wilcoxon signed rank tests were used to test for significant differences between the health state valuations generated by the two different versions of EQ-5D-5L. An intraclass correlation coefficient (ICC 2,1) was calculated in order to examine the correlation between all possible orderings of pairs of responses between TODAYQ and MONTHQ health state values. The within-subject change was then examined using the method described by Sutinen and colleagues for a similar reference period study (39); that is subtracting the MONTHQ health state value from the TODAYQ value and comparing this value to a point estimate (0.07) for the CMD (40). The CMD was defined as the smallest amount of change that patients perceive as beneficial or that would suggest a change in management (40). The point estimate used in this study for the CMD was derived from Walters and Brazier’s research (40) which employed both distribution and anchor based methods in a secondary analysis of large data set from a range of different conditions in order to calculate EQ-5D’s CMD. This more generic CMD is similar to the CMDs identified in more recent, condition specific, studies on cancer, inflammatory bowel disease, and post traumatic stress disorder (41–43), but lower than those identified in spinal surgery (44–46). The correlation between the health state values and the subscales of the MPI were also examined using a Spearman’s Rho correlation coefficient.
Results
A total of 100 patients were recruited to the study. Of these 100 patients five failed to fully complete both questionnaires, all of whom were male. There was no significant difference between those who did or did not complete the study on the basis of age, gender, or diagnostic group (p>0.2). Of those failing to complete both questionnaires one individual did so through non-response to the original distribution and follow-up and the remainder did so through non-response to the telephone follow-up of missing data on the questionnaires. All had too much missing data to allow any form of imputation. There were no missing data amongst the remainder of the sample (n=95) who completed both questionnaires for this study.
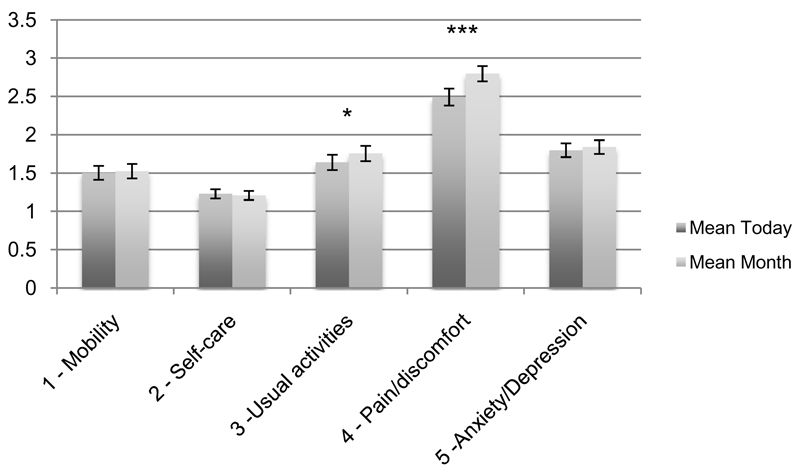
Table 1 demonstrates the sample’s demographics and origin of pain. The majority of the sample were female (n=77, 81%), and had pain of a combined origin (n=52, 55%). Figure 1 shows the respondents’ scores to the five dimensions (items) of the EQ-5D-5L by the reference period of the question. The mean difference between ‘Today’ and ‘Month’ health state valuation was 0.03 (95% CI 0.02-0.05) and the difference exceeded the CMD for 21 individuals in the sample. The difference between ‘Today’ and ‘Month’ valuations for those who exceeded the CMD was 0.07-0.74 (mean 0.18). There was a statistically, but not clinically, significant difference (P<0.001, effect size 0.14) between the ‘Today’ health state valuation (Mean 0.70, 95%CI 0.65-0.74) and the ‘Month’ health state valuation (Mean 0.66, 95%CI 0.62-0.71). The ICC showed good similarity between scores 0.86 (95%CI 0.79-0.91) between the two versions of EQ-5D-5L. When the within subject variance was examined the mean raw difference was 0.03 (95%CI 0.01-0.06).
Table 1. Sociodemographic of sample and origin of pain.
| Variable | Gender | Cohort | |
|---|---|---|---|
| Male (n=18) |
Female (n=77) |
||
| Mean age (SD) | 52 (17) | 52 (16) | 52 (16) |
| Origin of pain as determined by screening (Hapak et al 1994; Gonzalez et al 2011) | |||
| Musculoskeletal % (n) | 22 (4) | 13 (10) | 15 (14) |
| Neuropathic/Neurovascular % (n) | 28 (5) | 31 (24) | 30 (29) |
| Combined % (n) | 50 (9) | 56 (43) | 55 (52) |
Figure 1. Respondents’ mean scores by dimension and reference period of EQ-5D-5L.
*p<0.05
***p<0.001
Error bars give standard error of the estimate
The correlation coefficients for the Spearman’s Rho calculations between the subscales of the MPI and the health state valuations are shown in Table 2. All correlations were significant and in the expected direction. The majority of coefficients were of moderate or large size (38).
Table 2. Spearman Rho correlation between dimensions of MPI and summary score of EQ-5D-5L (Month reference period “MONTHQ” and standard Today reference period “TODAYQ”).
| EQ-5D-5L summary scores | MPI Dimension summary scores | |||||||
| MONTHQ | TODAYQ | Pain severity | Interference | Life control | Affective distress | Support | ||
| Coeff (95% CI) | Coeff (95% CI) | Coeff 95% CI | Coeff 95% CI | Coeff 95% CI | Coeff 95% CI | Coeff 95% CI | ||
| EQ-5D-5L summary scores | MONTHQ | 1 | 0.87*** (0.81, 0.91) | -0.68*** (-0.78,-0.56) | -0.48*** (-0.63,-0.31) | 0.42*** (0.23,0.57) | -0.46*** (-0.61,-0.28) | -0.26* (-0.44,-0.06) |
| TODAYQ | 1 | -0.67*** (-0.77,-0.54) | -0.49*** (-0.63,-0.32) | 0.43*** (0.25,0.58) | -0.50*** (-0.64,-0.33) | -0.29** (-0.47,-0.10) | ||
Coeff – Spearman’s rho correlation coefficient
95% CI – 95% Confidence interval of coeff.
p=0
p<0.01
p<0.05
Discussion
This was the first study, using POFP as a group of conditions, to assess the variation in the standardised reference period for the EQ-5D-5L and to examine whether this measure has convergent validity with a multidimensional pain measure, MPI, when quantifying the impacts of POFP.
The results indicate a statistically significant difference in the health state valuation between the reference points ‘Today’ and ‘Month’, illustrating the difficulties in capturing the impact of persistent pain using a standardised generic QOL measure. The magnitude (effect size) of the statistically significant difference between the two health state values was, however, small and therefore not likely to be clinically relevant. When the point estimate of the mean raw difference between the two reference points is examined it too is below clinically meaningful difference for EQ-5D in the literature (0.07 (40)). The difference in scores between the two reference periods was related to fluctuations in the dimensions of pain and activity levels with the month reference period capturing greater levels of impact than the today reference period. This is consistent with the known fluctuation of symptoms, and therefore impact, of several of the conditions comprising POFP (6, 47).
EQ-5D-5L demonstrated good convergent validity with the condition specific measure, the MPI, suggesting that EQ-5D-5L is an appropriate tool for use with POFP. If EQ-5D-5L is to be used with POFP using the standard “today” reference period there is a conscious trade-off to be considered. This trade-off is between generating generic cross-condition/disease QALYs that can be compared, versus losing detail on the level of impact of POFP thereby potentially slightly underestimating its impact. At present the authors would suggest to compensate for this loss of detail by utilising an instrument such as the MPI alongside the EQ-5D in order to help capture the impact over a longer period of time. The MPI clearly also captures some additional data beyond the scope of the EQ-5D given the lower correlation coefficients in its social support domain. Its concomitant use may, therefore, help further explain the reasons behind the impact of POFP, but would have to be weighed against the risk of attrition and or acquiescence bias with the use of more questions. Given the data presented in this paper the authors feel the advantages of using the standard reference period of “Today” outweigh the potential disadvantages as long as they are recognised as a limitation in any data produced using this method.
This study had some limitations. The study assessed a broad heterogeneous group of patients who had not received a specialist diagnosis. This limitation may also be viewed as a strength however, as the aim of the study was to apply EQ-5D-5L to POFP not a particular subset of the disorders. The study also did not assess whether the EQ-5D-5L measure was responsive to change. It is possible that with the ongoing prospective data collection in the DEEP study we will be in a position to provide an answer to this question and also a POFP specific CMD. We did, however, purposefully choose one of the more generic, CMDs in the literature to compare the performance of the two versions of the instrument against in order to carefully examine the difference made by the change in reference period. It is, however, conceivable that perhaps this is not a stern enough test, that is the CMD for POFP is actually lower than this, but we feel it is more likely that the CMD for POFP is higher than this. One further limitation of our method is the standardised order in which we presented the two versions of EQ-5D. We chose to do this so it was absolutely clear to the participants that the two questionnaires were not just duplicates of each other and had a subtle difference. We accept, however, that methodologically it might have been stronger to randomise the order.
Comparing the health state valuation of POFP in this study to other conditions is somewhat difficult, as data on other conditions’ health state valuation, at the time of writing, currently exists only through the use of EQ-5D-3L. This said the EQ-5D-5L values used in this study are those cross-walked from the EQ-5D-3L (37) so are somewhat equivalent. Our estimates (today reference period) of health state valuations for POFP are comparable to other persistent (chronic) health states such as arthritis, and depression, but less than conditions such as back, pain, stroke and Parkinson’s (37). Examining studies that have also used EQ-5D with singular entities (Trigeminal neuralgia (22), Inferior Alveolar and Lingual nerve damage (11)) comprising part of the group of POFP conditions it would appear that we are broadly comparable to the range they identified (0.56-0.68). Our confidence interval for the health state valuation of POFP is also less than that of the UK health population norm (0.75-0.94) for the age groups 25-75+.
Conclusion
The impact of POFP on an individual’s quality of life is captured using EQ-5D-5L’s standard “Today” reference period and the instrument possesses sufficient convergent validity to be used with POFP. Results from EQ-5D-5L using the standard reference period may tend towards a slight underestimate of the actual impact of POFP on individuals’ QOL and therefore it is advisable to use another multidimensional pain measure in conjunction that possesses longer reference period to compensate for this.
Acknowledgements
This study and JD are funded by a NIHR Clinician Scientist award (NIHR-CS-011-003). The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research, or the Department of Health in the United Kingdom.
We would also like to thank the patients and health professionals who participated in this study and made it possible.
Footnotes
The authors have no conflicts of interest to declare.
References
- 1.IASP. International Association for the Study of Pain - Pain Terminology. 2007.
- 2.De Leeuw R, Klasser GD. Orofacial pain: guidelines for assessment, diagnosis, and management. Hanover Park, IL: Quintessence; 2013. [Google Scholar]
- 3.Kerns RD, Turk DC, Rudy TE. The West Haven-Yale Multidimensional Pain Inventory (WHYMPI) Pain. 1985;23:345–356. doi: 10.1016/0304-3959(85)90004-1. [DOI] [PubMed] [Google Scholar]
- 4.Aggarwal VR, Lunt M, Zakrzewska JM, Macfarlane GJ, Macfarlane TV. Development and validation of the Manchester orofacial pain disability scale. Community Dent Oral Epidemiol. 2005;33:141–149. doi: 10.1111/j.1600-0528.2004.00193.x. [DOI] [PubMed] [Google Scholar]
- 5.Lopez-Jornet P, Camacho-Alonso F, Lucero-Berdugo M. Quality of life in patients with burning mouth syndrome. J Oral Pathol Med. 2008;37:389–394. doi: 10.1111/j.1600-0714.2008.00672.x. [DOI] [PubMed] [Google Scholar]
- 6.Moufti MA, Wassell RW, Meechan JG, Allen PF, John MT, Steele JG. The Oral Health Impact Profile: ranking of items for temporomandibular disorders. Eur J Oral Sci. 2011;119:169–174. doi: 10.1111/j.1600-0722.2011.00809.x. [DOI] [PubMed] [Google Scholar]
- 7.Reisine ST, Weber J. The effects of temporomandibular joint disorders on patients’ quality of life. Community Dent Health. 1989;6:257–270. [PubMed] [Google Scholar]
- 8.Reissmann DR, John MT, Schierz O, Wassell RW. Functional and psychosocial impact related to specific temporomandibular disorder diagnoses. J Dent. 2007;35:643–650. doi: 10.1016/j.jdent.2007.04.010. [DOI] [PubMed] [Google Scholar]
- 9.Souza FT, Santos TP, Bernardes VF, et al. The impact of burning mouth syndrome on health-related quality of life. Health Qual Life Outcomes. 2011;9:57. doi: 10.1186/1477-7525-9-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zheng J, Wong MC, Lam CL. Key factors associated with oral health-related quality of life (OHRQOL) in Hong Kong Chinese adults with orofacial pain. J Dent. 2011;39:564–571. doi: 10.1016/j.jdent.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 11.Smith JG, Elias LA, Yilmaz Z, et al. The psychosocial and affective burden of posttraumatic neuropathy following injuries to the trigeminal nerve. J Orofac Pain. 2013;27:293–303. doi: 10.11607/jop.1056. [DOI] [PubMed] [Google Scholar]
- 12.Azar M, Yahyavi ST, Bitaraf MA, et al. Gamma knife radiosurgery in patients with trigeminal neuralgia: quality of life, outcomes, and complications. Clin Neurol Neurosurg. 2009;111:174–178. doi: 10.1016/j.clineuro.2008.09.020. [DOI] [PubMed] [Google Scholar]
- 13.Liu LJ, Xiao W, He QB, Jiang WW. Generic and oral quality of life is affected by oral mucosal diseases. BMC Oral Health. 2012;12:2. doi: 10.1186/1472-6831-12-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lopez-Jornet P, Camacho-Alonso F, Lucero Berdugo M. Measuring the impact of oral mucosa disease on quality of life. Eur J Dermatol. 2009;19:603–606. doi: 10.1684/ejd.2009.0762. [DOI] [PubMed] [Google Scholar]
- 15.Lopez-Jornet P, Camacho-Alonso F, Andujar-Mateos P. A prospective, randomized study on the efficacy of tongue protector in patients with burning mouth syndrome. Oral Dis. 2011;17:277–282. doi: 10.1111/j.1601-0825.2010.01737.x. [DOI] [PubMed] [Google Scholar]
- 16.Navarro A, Saldana MT, Perez C, Torrades S, Rejas J. Patient-reported outcomes in subjects with neuropathic pain receiving pregabalin: evidence from medical practice in primary care settings. Pain Med. 2010;11:719–731. doi: 10.1111/j.1526-4637.2010.00824.x. [DOI] [PubMed] [Google Scholar]
- 17.Pan HC, Sheehan J, Huang CF, Sheu ML, Yang DY, Chiu WT. Quality-of-life outcomes after Gamma Knife surgery for trigeminal neuralgia. J Neurosurg. 2010;113(Suppl):191–198. doi: 10.3171/2010.8.GKS10879. [DOI] [PubMed] [Google Scholar]
- 18.Perez C, Navarro A, Saldana MT, Martinez S, Rejas J. Patient-reported outcomes in subjects with painful trigeminal neuralgia receiving pregabalin: evidence from medical practice in primary care settings. Cephalalgia. 2009;29:781–790. doi: 10.1111/j.1468-2982.2008.01792.x. [DOI] [PubMed] [Google Scholar]
- 19.Sardella A, Lodi G, Tarozzi M, Varoni E, Franchini R, Carrassi A. Acupuncture and Burning Mouth Syndrome: A Pilot Study. Pain Pract. 2013 doi: 10.1111/papr.12031. [DOI] [PubMed] [Google Scholar]
- 20.Ta LE, Dionne RA. Treatment of painful temporomandibular joints with a cyclooxygenase-2 inhibitor: a randomized placebo-controlled comparison of celecoxib to naproxen. Pain. 2004;111:13–21. doi: 10.1016/j.pain.2004.04.029. [DOI] [PubMed] [Google Scholar]
- 21.Tjakkes GH, Reinders JJ, Tenvergert EM, Stegenga B. TMD pain: the effect on health related quality of life and the influence of pain duration. Health Qual Life Outcomes. 2010;8:46. doi: 10.1186/1477-7525-8-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tolle T, Dukes E, Sadosky A. Patient burden of trigeminal neuralgia: results from a cross-sectional survey of health state impairment and treatment patterns in six European countries. Pain Pract. 2006;6:153–160. doi: 10.1111/j.1533-2500.2006.00079.x. [DOI] [PubMed] [Google Scholar]
- 23.Ware JEJ, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 24.Allen PF, McMillan AS, Walshaw D, Locker D. A comparison of the validity of generic- and disease-specific measures in the assessment of oral health-related quality of life. Community Dent Oral Epidemiol. 1999;27:344–352. doi: 10.1111/j.1600-0528.1999.tb02031.x. [DOI] [PubMed] [Google Scholar]
- 25.Guyatt GH, Bombardier C, Tugwell PX. Measuring disease-specific quality of life in clinical trials. CMAJ. 1986;134:889–895. [PMC free article] [PubMed] [Google Scholar]
- 26.Guyatt GH, Feeny DH, Patrick DL. Measuring health-related quality of life. Ann Intern Med. 1993;118:622–629. doi: 10.7326/0003-4819-118-8-199304150-00009. [DOI] [PubMed] [Google Scholar]
- 27.Brennan DS, Spencer AJ. Mapping oral health related quality of life to generic health state values. BMC Health Serv Res. 2006;6:96. doi: 10.1186/1472-6963-6-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dahlstrom L, Carlsson GE. Temporomandibular disorders and oral health-related quality of life. A systematic review. Acta Odontol Scand. 2010;68:80–85. doi: 10.3109/00016350903431118. [DOI] [PubMed] [Google Scholar]
- 29.Brooks R. EuroQol: the current state of play. Health Policy. 1996;37:53–72. doi: 10.1016/0168-8510(96)00822-6. [DOI] [PubMed] [Google Scholar]
- 30.Brazier J, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF-36. J Health Econ. 2002;21:271–292. doi: 10.1016/s0167-6296(01)00130-8. [DOI] [PubMed] [Google Scholar]
- 31.Obradovic M, Lal A, Liedgens H. Validity and responsiveness of EuroQol-5 dimension (EQ-5D) versus Short Form-6 dimension (SF-6D) questionnaire in chronic pain. Health Qual Life Outcomes. 2013;11:110. doi: 10.1186/1477-7525-11-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Szende A, Janssen B, Cabases J, editors. Self-reported population health: an international perspective based on EQ-5D. New York: SpringerOpen; 2014. [PubMed] [Google Scholar]
- 33.Durham J, Breckons M, Araujo-Soares V, Exley C, Steele J, Vale L. Developing Effective and Efficient care pathways in chronic Pain: DEEP study protocol. BMC Oral Health. 2014;14:6. doi: 10.1186/1472-6831-14-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gonzalez YM, Schiffman E, Gordon SM, et al. Development of a brief and effective temporomandibular disorder pain screening questionnaire: reliability and validity. J Am Dent Assoc. 2011;142:1183–1191. doi: 10.14219/jada.archive.2011.0088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hapak L, Gordon A, Locker D, Shandling M, Mock D, Tenenbaum HC. Differentiation between musculoligamentous, dentoalveolar, and neurologically based craniofacial pain with a diagnostic questionnaire. J Orofac Pain. 1994;8:357–368. [PubMed] [Google Scholar]
- 36.Rudy TE. Multidimensional Pain Inventory version 3 user’s guide. 2005 [Google Scholar]
- 37.van Hout B, Janssen MF, Feng YS, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health. 2012;15:708–715. doi: 10.1016/j.jval.2012.02.008. [DOI] [PubMed] [Google Scholar]
- 38.Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. New Jersey: Lawrence Erlbaum; 1988. [Google Scholar]
- 39.Sutinen S, Lahti S, Nuttall NM, et al. Effect of a 1-month vs. a 12-month reference period on responses to the 14-item Oral Health Impact Profile. Eur J Oral Sci. 2007;115:246–249. doi: 10.1111/j.1600-0722.2007.00442.x. [DOI] [PubMed] [Google Scholar]
- 40.Walters SJ, Brazier JE. Comparison of the minimally important difference for two health state utility measures: EQ-5D and SF-6D. Qual Life Res. 2005;14:1523–1532. doi: 10.1007/s11136-004-7713-0. [DOI] [PubMed] [Google Scholar]
- 41.Le QA, Doctor JN, Zoellner LA, Feeny NC. Minimal clinically important differences for the EQ-5D and QWB-SA in Post-traumatic Stress Disorder (PTSD): results from a Doubly Randomized Preference Trial (DRPT) Health Qual Life Outcomes. 2013;11:59. doi: 10.1186/1477-7525-11-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pickard AS, Neary MP, Cella D. Estimation of minimally important differences in EQ-5D utility and VAS scores in cancer. Health Qual Life Outcomes. 2007;5:70. doi: 10.1186/1477-7525-5-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stark RG, Reitmeir P, Leidl R, Konig HH. Validity, reliability, and responsiveness of the EQ-5D in inflammatory bowel disease in Germany. Inflamm Bowel Dis. 2010;16:42–51. doi: 10.1002/ibd.20989. [DOI] [PubMed] [Google Scholar]
- 44.Parker SL, Adogwa O, Paul AR, et al. Utility of minimum clinically important difference in assessing pain, disability, and health state after transforaminal lumbar interbody fusion for degenerative lumbar spondylolisthesis. J Neurosurg Spine. 2011;14:598–604. doi: 10.3171/2010.12.SPINE10472. [DOI] [PubMed] [Google Scholar]
- 45.Parker SL, Adogwa O, Mendenhall SK, et al. Determination of minimum clinically important difference (MCID) in pain, disability, and quality of life after revision fusion for symptomatic pseudoarthrosis. Spine J. 2012;12:1122–1128. doi: 10.1016/j.spinee.2012.10.006. [DOI] [PubMed] [Google Scholar]
- 46.Parker SL, Godil SS, Shau DN, Mendenhall SK, McGirt MJ. Assessment of the minimum clinically important difference in pain, disability, and quality of life after anterior cervical discectomy and fusion: clinical article. J Neurosurg Spine. 2013;18:154–160. doi: 10.3171/2012.10.SPINE12312. [DOI] [PubMed] [Google Scholar]
- 47.Zakrzewska JM, Palmer J, Ettlin DA, et al. Novel design for a phase IIa placebo-controlled, double-blind randomized withdrawal study to evaluate the safety and efficacy of CNV1014802 in patients with trigeminal neuralgia. Trials. 2013;14:402. doi: 10.1186/1745-6215-14-402. [DOI] [PMC free article] [PubMed] [Google Scholar]