Abstract
Background
Children take one medication each week on average at home. Better communication between parents and providers could support safer home medication use and prevent misuse of pediatric medications, such as intentional under or overdosing. Our primary objective was to assess the impact of an interactive voice response system on parent-provider communication about medications.
Methods
Parents of children 4 months - 11 years with upcoming well child visits were invited to call our interactive voice response system, called Personal Health Partner (PHP), which asked questions about the child's health and medication use. Responding parents were randomized to either PHP (interview and counseling) or control (injury prevention survey). Parent responses were embedded in the electronic health record. After the physical, research assistants performed a phone follow-up survey.
Results
Of 475 parents, including 293 PHP and 182 control, 93% were women. We found a high prevalence of misuse of medications: 14% reported under dosing (N=63) fever-reducer medications and 3% overdosing (N=13). 20% (N=37) of the 190 children under three had received cold medication. 33% (N=19) of 62 PHP parents of children on prescription medications reported non-adherence. Among children on prescription medications, PHP significantly increased discussion of medications at the physical, but not the number who brought medications to the visit; it had no impact on those not on prescription medications.
Conclusions
Pediatric medication misuse was common in this study. Use of a pre-visit IVR system increased medication-related communication during visits and supports the need for systems that better prepare patients for visits and improve medication-related patient-physician communication.
Keywords: medication errors, medication reconciliation, patient safety, health information technology
Background
The number of U.S. children taking daily medications has increased substantially in the past decade.1 The majority of children under twelve use one or more prescription or over-the-counter medication products in a given week. Recent studies have raised concerns regarding errors in over-the-counter and prescription medication use by children at home.2-4 The use of home medications in children is error prone, for many reasons, including the complexity of weight-based dosing, measurement of liquid medications, and confusion caused by dosing instruments.2,5-7
Communication between doctors and patients about home medication use is limited. Medication lists clinicians use to understand home medication use are commonly incorrect, due to problems with medication reconciliation.8,9 Dangerous medication errors occur when parents misunderstand physician instructions.4,10 When patients forget, skip, or alter doses of medication, they often do not tell their doctor.11,12 Parents may misuse pediatric medications by accidentally or intentionally over dosing or under dosing.2,13-15 Parental health literacy impacts the way medicines are measured at home.2 Patients may be uncomfortable telling doctors that they did not follow their instructions. Changes in guidelines regarding the use of over-the-counter medications may also contribute to parental confusion, including the 2008 restriction of cold medicine to children under 4 years old.16,17,18 To help parents prevent medication errors, AHRQ recommends several steps parents can take, including asking for a measurement instrument from the pharmacy.19 Electronic systems, often used to gather sensitive information from patients, may be effective at gathering information about medication use at home and supporting communication with clinicians, particularly when linked to a scheduled routine well child visit.
We have developed a pre-visit, parent-centered, interactive voice response system, the “Personal Health Partner” (PHP), integrated with an electronic health record. PHP targets routine health maintenance content and medication safety though automated interviews and tailored counseling. Results from the routine health maintenance content have been previously published.20 This report describes findings related to the medication safety portion of the study which included both information PHP captured during the randomized trial component of the study as well as post-visit surveys that were performed for all participants, including PHP and control patients. Our primary objective was to assess the impact of an interactive voice response system on medication-related parent-provider communication.
Methods
Study site
This study was conducted at an academic outpatient pediatric clinic in Boston with over 35,000 patient visits annually. The EHR used in the clinic has Centricity TM (GE Medical Systems). The study was approved by the Boston University Medical Campus Institutional Review Board.
Subject Recruitment
Parents of children ages 4 months to 11 years with upcoming routine health maintenance visits were recruited between May 2009 and February 2011. Potentially eligible patients were identified from electronic scheduling data. Parents were mailed an information brochure, telephone number, and unique login and were asked to call anytime during the 5 days prior to the child's clinic visit. Those not responding to the letter within 3 days of the visit were called and reminded by a research assistant.
Intervention
PHP calls have two primary components: 1) a pre-visit “conversation” with counseling; and 2) electronic health record data exchange for clinician review. Details of the routine health maintenance components of PHP have been published.20 The system uses synthetic speech and speech recognition to ask questions and capture spoken words over the telephone. During the call, the system explained the study, acquired consent, and then randomized the child to PHP or a control group. The study began with 1:1 randomization but quickly moved to 2:1 (intervention: control) randomization to increase the number of families using the intervention.
All calls started with introduction to medication safety section followed by a series of questions. Cold medication questions were limited to children under 3, prescription medication and adherence questions to those patients on at least one medication. Asthma–related questions were limited to patients with at least one ICD9 code for asthma on the problem list. Over-the-counter medication safety questions (including fever control) were asked of all patients; those who reported giving their child fever medicine in the last month were also asked what concentration and amount of medicine they gave. All parents were then asked about safe medication use behaviors recommended to parents by AHRQ- specifically asking for measurement instruments for liquid medicines and bringing medicine to the doctor.19 Finally, PHP performed a review of all the medications currently in the system (Medication Reconciliation).
Questions were conversational in nature. For example, parents were asked “Let's talk for a minute about fever medications. There are 2 different types of medications that people use for fever: Tylenol (also called acetaminophen) or Motrin (also called ibuprofen or Advil). Did you ever give less than the amount of fever medication that was prescribed by your doctor or less than the amount written on the box for your child's age?” Parents could answer “yes” or “no” to that question. The system is able to link parent responses to a menu of answers. For example, if the parent reported that they did give less than the recommended amount of fever medication, the system asked “Did you give less fever medication by accident, or, on purpose? Say accident, or, on purpose”. Parent reported data was used to build custom counseling messages. A parent focus group reviewed draft wording and made suggestions regarding style and vocabulary.
Questions regarding asthma medications were asked only of children with at least one ICD9 code for asthma on the problem list. For parents who reported using asthma controller medications to relieve exacerbations or who reported non-adherence to asthma medication, PHP counseled parents to bring medications to clinic to discuss with the clinician. PHP also counseled parents of children on prescription medications to bring the medications to the child's visit and counseled parents who reported incorrectly using over-the-counter cold medication or fever reducer to discuss with their clinician.
Medication reconciliation
Electronic health record data was used to develop a comprehensive list of all medications prescribed to patients in the eligible age range. Each unique prescription was linked to a generic drug name as well as a brand name if prescribed as a brand name medication. To ensure appropriate pronunciation of each medication name, medication names were recorded separately as discreet audio files by having the one of the investigators (WA) record the names. During calls, PHP asked the parent to get all the child's prescription medications before resuming the call. PHP then read each name from the active electronic health record medication list and asked the parents to state whether the patient was taking the medication. Parents were next asked if there were additional medications that the computer did not name. Errors in the medication list were categorized has having extra medications (medications listed which the child was not taking) or omissions (medications the child was taking which were not on the medication list).
Data on the patient's age, race, ethnicity, gender, and current and past medications were collected from the electronic health record. Parent gender, highest level of education, and employment status were collected by PHP.
Provider interface
An additional section was added to the EHR to hold PHP interview data, entitled “Patient entered data”. If a PHP interview occurred within 30 days of a health maintenance visit, a prompt stating that “Patient entered data are available” appeared. By clicking “Go” the clinician could view and edit the data. During the visit, the clinician could click “Accept all” and add the data to the clinic visit note. After 30 days, the PHP data were no longer available for viewing in the EHR.
Control
Patients randomized to the control group received an interactive voice response home safety survey, the Framingham Safety Survey.21 PHP gave this group tailored advice, based on their answers to the survey, related to unsafe behavior they reported. The timing of the survey was identical to the intervention group.
Final Interview
Two to three weeks after the patient's well child visit, research assistants contacted parents by phone and performed a 66-item follow up survey, which included 15 items related to medications. All follow up survey calls started with introduction to medication safety section followed by a series of questions. The research assistants asked all participants about fever reducer and cold medications using the same questions and wording as PHP. For children under 3, research assistants also asked the same questions about cold medications as PHP. For all patients, research staff assessed the accuracy of medication reconciliation during post-visit interviews using structured templates that were pre-filled with the patient's medication list as of the end of the visit. Parents were asked whether or not the patient was taking each medication in the template and then added medications that parents reported taking that were not on the list. Each patient's medication list was then reviewed to identify missing and inaccurate medications. Finally, research staff asked whether families discussed medications during the physical or brought medications to the physical. Patients who participated in the PHP interview but did not attend the physical or did not participate in the follow up survey were excluded from the study.
Measures and definitions
Our PHP interview and follow up survey assessed several items. Prescription medications were defined for parents as follows: “Doctors often write a prescription for a medication that can't be bought without a prescription- a medication other than cold or fever medication - these are called prescription medications, such as antibiotics, puffers for asthma, or ADHD medication”. Cough medications were defined as “medications that you can buy in the drug store that is used to help with cold, cough, or congestion”. Misuse of over-the-counter medication included parent report of accidental or intentional over- or under dosing of fever medications15 or use of cold medications in children under 3 years old.17 Misuse of prescription medication included parent report of nonadherence22 or self-reported accidental or intentional over- or under dosing of medications.4,15 (Table 3) Misuse of asthma medications included parent report of having a daily controller but not albuterol at home, report of using a daily controller to relieve an asthma exacerbation, or report of non-adherence to the daily controller.22 Parents also reported whether or not they ever asked for measurement instruments from a pharmacy, doctor or nurse for liquid medicines or whether they ever brought their medicine to the doctor, as recommended by AHRQ to reduce errors.19 To assess the impact of PHP counseling, we asked parents whether they discussed medications with the doctor, including prescription, asthma, fever, or cold medicines. We also asked parents whether they brought the child's medications to the clinic visit. Finally, we measured the accuracy of chart medication list by asking the parent to get all the child's prescription and over-the-counter medications.
Table 3.
Reports of use of prescription medications to the Personal Health Partner interactive voice response system.
| Questions about medication use | PHP IVR InterviewN (%) |
|---|---|
| Asthma medications1 | |
| Sometimes forget daily asthma medications | 6 (13.0%) |
| Sometimes alter dose of daily asthma medications | 8 (17.8%) |
| Albuterol at home | 35 (72.9%) |
| On a daily controller, Albuterol at home | 21 (84.0%) |
| Not on a daily controller, Albuterol at home | 14 (60.9%) |
| Use controller as needed for quick relief of asthma symptoms | 16 (64.0%) |
| Use controller to prevent future asthma symptoms | 16 (64.0%) |
| Any misuse of asthma medication | 23 (51.1%) |
| Prescription medications2 | |
| Any misuse of prescription medications | 6 (23.1%) |
| Sometimes forget to give prescription medications | 6 (23.1%) |
| Sometimes alter dose of prescription medications | 1 (4.0%) |
48 people on asthma medications, including 25 on a daily controller medication
26 children in the PHP group were on prescription medications
Analysis
Descriptive analyses were performed to quantify over-the-counter, asthma, and prescription medication usage behaviors. Generalized estimating equations with a compound symmetric covariance structure and robust standard errors were used to account for the intragroup correlation that resulted from measurements of multiple children per family, and robust standard errors were used to protect against the potential misspecification of the covariance structure. Generalized estimating equations were also used to evaluate the success of randomization and the impact of PHP on medication-related physical visit content and post-physical medication usage. All analyses were conducted in Stata version 12 (StataCorp, College Station, TX) using an intent-to-treat approach and a significance level of 0.05.
Results
The final sample had 475 patients, including 182 who were randomized to the control group and 293 who were randomized to the PHP group. (Figure 1) Brochures were mailed to 6910 parents; 425 were returned due to incorrect address. 593 parents called in and were randomized; 108 did not attend their physical visit and 10 did not complete the final interview and were lost to follow up. The control PHP calls were shorter in duration than the intervention calls. (29.3 minutes; SD = 5.9 vs 17.3 minutes, SD = 5; (P,0.001)) The median age of the study population was 4.7 years (range: 4 months – 11 years) and 48% were female. (Table 1) Health literacy, as measured using the Rapid Estimate of Adult Literacy in Medicine,23 showed 20% of parents having health literacy scores corresponding to less than a 9th grade reading level. There were significantly more female patients in the control group; otherwise there were no differences between groups.
Figure 1. Consort Diagram.
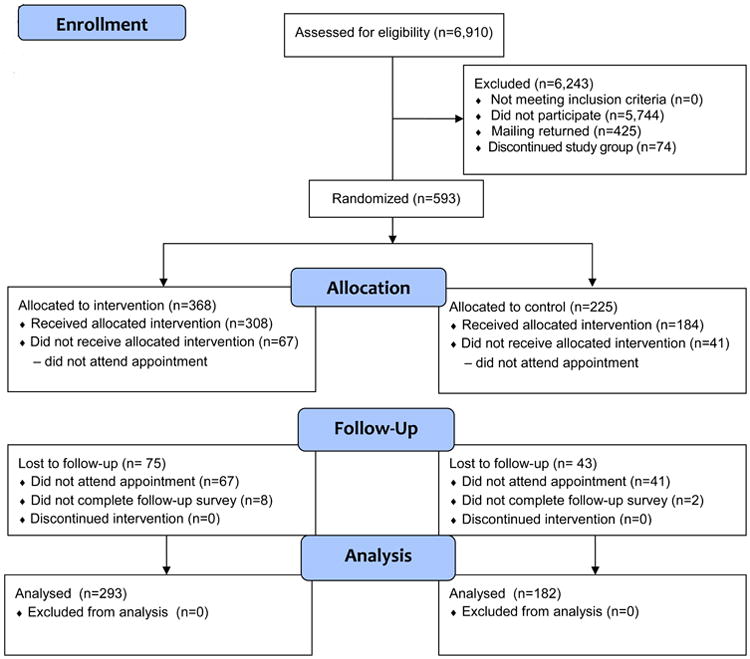
Table 1.
Demographics of parents and their children randomized to control or Personal Health Partner, intervention groups. P values assess statistical significance of differences between intervention and control groups.
| Entire Sample (N=475) N (%) or Mean (SD) | Intervention (N=293) | Control (N=182) | P-Value | |
|---|---|---|---|---|
|
| ||||
| Age of child (in years) | 4.7 (3.5) | 4.7 (3.5) | 4.8 (3.6) | 0.85 |
|
| ||||
| Child female gender | 229 (48.2%) | 128 (43.7%) | 101 (55.5%) | 0.01 |
|
| ||||
| Child race/ethnicity | 0.18 | |||
| African American | 319 (72.3%) | 201 (73.6%) | 118 (70.2%) | |
| Asian/PI | 0 | 0 | 0 | |
| Hispanic | 43 (9.8%) | 27 (9.9%) | 16 (9.5%) | |
| White | 59 (13.4%) | 35 (12.8%) | 24 (14.3%) | |
| Other | 20 (4.5%) | 10 (3.7%) | 10 (5.6%) | |
| No answer | 34 | 10 | 14 | |
|
| ||||
| Age of parent (in years) | 34.7 (8.4) | 34.4 (8.3) | 35.2 (8.4) | 0.46 |
|
| ||||
| Parent female gender | 438 (93.0%) | 271 (93.1%) | 167 (92.8%) | 0.83 |
|
| ||||
| Parent race/ethnicity | 0.66 | |||
| African American | 220 (47.0%) | 132 (45.8%) | 88 (48.9%) | |
| Alaskan native | 4 (0.9%) | 3 (1.0%) | 1 (0.6%) | |
| Asian/PI | 28 (6.0%) | 15 (5.2%) | 13 (7.2%) | |
| Hispanic | 28 (6.0%) | 16 (5.6%) | 12 (6.7%) | |
| White | 126 (26.9%) | 79 (27.4%) | 47 (26.1%) | |
| Other | 62 (13.2%) | 43 (14.9%) | 19 (10.6%) | |
| No answer | 7 | 5 | 2 | |
|
| ||||
| Parent educational level | 0.55 | |||
| Did not complete high school | 45 (10.7%) | 28 (10.8%) | 17 (10.7%) | |
| Completed high school | 95 (22.7%) | 57 (21.9%) | 38 (23.9%) | |
| Some college | 118 (28.2%) | 80 (30.8%) | 38 (23.9%) | |
| Completed college | 161 (38.4%) | 95 (35.5%) | 66 (41.5%) | |
| No answer | 56 | 33 | 23 | |
|
| ||||
| Parent employment | 0.11 | |||
| No | 205 (48.9%) | 130 (50.0%) | 75 (47.2%) | |
| Yes | 201(48.0%) | 118 (45.4%) | 83 (52.2%) | |
| Sometimes | 13 (3.1%) | 12 (4.6%) | 1 (0.6%) | |
| No answer | 56 | 33 | 23 | |
|
| ||||
| Parent Rapid Estimate of Adult Literacy in Medicine | ||||
| 0-18 3rd grade and below | 1 (0.4%) | 1 (0.7%) | 0 | |
| 19-44 4th -6th grade | 5 (2.2%) | 3 (2.1%) | 2 (2.4%) | 0.85 |
| 45-60 7th -8th grade | 40 (17.6%) | 23 (16.2%) | 17 (20.0%) | |
| 61-66 9th grade and above | 181 (79.7%) | 115 (81.0%) | 66 (77.7%) | |
| No answer | 248 | 151 | 97 | |
|
| ||||
| Median number prescription medications | 0 (range 0-17) | 0 (range 0-17) | 0 (range 0-8) | 0.13 |
|
| ||||
| Number children on prescription medication | 167 (35.2%) | 105 (36.0%) | 62 (34.1%) | 0.73 |
Misuse of over-the-counter medications
Our study identified a high rate of medication misuse: 18% (N=32) of control and 27% (N=40) PHP parents reported misuse of over-the-counter medications. (Table 2) Fourteen percent of parents (N=63) reported giving less than the indicated amount of fever medication. PHP asked parents why they under dosed fever medication: 84% reported doing this on purpose, 11% by accident, and 5% because the doctor told them to. A much smaller number of parents (3%; N=13) reported giving more than the correct amount of fever medication. Half told PHP this was by accident and half reported giving an overdose because they did not have the correct form of the medication at home. Parents were significantly more likely to tell PHP they under-dosed fever medication than to tell the research assistant at the post visit survey (25% vs 17%; p=0.01).
Table 2. Reports of over-the-counter medication use to the Personal Health Partner interactive voice response system and to research assistants during the post visit survey.
| Questions about medication use | PHP IVR Interview(N=293) | Post visit survey | Unadjusted p-value | Adjusted p-value4 | ||
|---|---|---|---|---|---|---|
| PHP (N=293) | Control (N=182) | TOTAL (N=475) | ||||
| Over-the-counter medications | ||||||
| Give less fever reducer than indicated | 21 (25%)1 | 46 (17%) | 17 (10%) | 63 (14%) | 0.01 | 0.01 |
| Give more fever reducer than indicated | 2 (2%)1 | 11 (4%) | 2 (1%) | 13 (3%) | 0.14 | 0.14 |
| Cough medication under 3 years old | 21 (20%)2 | 22 (19%) | 15 (21%) | 37 (20%) | 0.67 | 0.91 |
| Any misuse of over-the-counter medications | 40 (27%)3 | 69 (24%) | 32 (18%) | 101 (21%) | 0.17 | 0.17 |
90 parents who gave their children fever reducer in the past month answered this question during the PHP call
117 children in the PHP group and 73 children in the control group were under 3 years old
148 parents provided answers to the over-the-counter questions during the PHP interview
Adjusted for clustering of subjects within families using generalized estimating equations with a compound symmetric covariance structure
PHP asked each parent who gave their child fever medication in the past month what dose was administered. Of the 90 parents who gave their child fever medication in the past month, 6 could not recall the dose. Of the remaining parents, 73% gave the correct dose, based on the child's weight in the electronic health record. Twenty-five percent under dosed the medication and two parents overdosed (range 18-188% of correct dose).
We asked parents of children under 3 whether they ever gave their child cough medication during post-visit interviews. Of the 190 parents with children under three, 37 (20%) reported giving their child cough medications. At the time of this study, homeopathic cough medications for young children were not commercially available.
Misuse of prescription medication
Of the 26 parents of children on daily prescription medications in the PHP group, 6 (23%) reported non-adherence to prescription medications. (Table 3) This included six parents who reported forgetting to give the medication and one parent who reported both forgetting and sometimes altering the dose of the medication.
There were 48 children with asthma in the PHP group, including 25 children taking a daily controller medication. More parents of children on a daily controller medication reported that they had albuterol at home (84%; N=21) than parents of children who were not on a daily controller medication (61%; N=14). Of those on a daily controller medication, 16 (64%) reported using it for quick relief of asthma symptoms, such as cough or wheeze, and 16 reported using the controller to prevent future asthma symptoms (some reported both). Half of asthmatic children reported either not having albuterol at home, sometimes missing or altering doses of medication, or using a daily controller for acute symptoms.
Measurement instrument and bring medicine to doctor
In order to prevent a medication error, the Agency for Healthcare Quality suggests that all parents ask for a measurement instrument to measure the child's medication and bring the medication to the physician appointments. When asked by PHP, only 36% of parents reported ever asking the pharmacy, doctor, or nurse for a measurement instrument and only 13% of parents reported ever bringing medication to a doctor visit.
Impact of PHP counseling
Of parents of children on prescription medication, 86% in the PHP group (90 of 105 on prescription medications) and 73% in the control group (45 of 62 on prescription medications) discussed medications during the visit (p=0.04). Most of these reported discussing how much or how often medications are used. Of parents of children who are not on prescription medication, there was no difference in the number who discussed medications during the visit (15% control [N=18] vs 14% [N=27] PHP; p=0.95). Of parents of children on prescription medication, 19% (N=20) brought their medication to the clinic visit, compared to 10% (N=6) of control parents (p=0.26).
Medication Reconciliation
The rate of accuracy in the medication list was low during the PHP interview before the visit and in the follow up survey by research assistants after the physical for both the PHP (21% accurate) and control (24% accurate) groups. (Table 4) Overall 74% of patients' medication lists had an extra medication and 20% were missing a medication. Performance of medication reconciliation by PHP did not improve the accuracy of the medication list compared to controls.
Table 4. Medication reconciliation in PHP intervention and follow up.
| Medication reconciliation results | PHP IVR Interview (N=293) | Post visit survey | ||||
|---|---|---|---|---|---|---|
| PHP (N=293) N (%) | Control (N=182) N (%) | Total (N=475) N (%) | Unadjusted P1 | Adjusted P1 | ||
| Patients with extra meds on medical record medication list (Range number extra meds) | 193 (86.2%) (1-14 extra) | 131 (72.0%) (1-26 extra) | 222 (75.8%) (1-45 extra) | 353 (74.3%) | 0.35 | 0.55 |
| Patients with missing meds on medical record medication list (Range number of missing meds) | 0 (0.0%) | 66 (22.5%) (1-8 missing) | 30 (16.5%) (1-3 missing) | 96 (20.2%) | 0.09 | 0.22 |
| Patients with correct med list on survey | 31 (13.8%) | 62 (21.2%) | 43 (23.6%) | 105 (22.2%) | 0.51 | 0.67 |
Adjusted for clustering of subjects within families using generalized estimating equations with a compound symmetric covariance structure
Discussion
This study identified important findings in three areas: 1) we detected high rates of misuse of over-the-counter fever reducer and cold medication; 2) non-adherence to prescription medications and misuse of asthma medications was common in our population; and 3) an automated interactive voice response system was able to detect many of these behaviors and alert the pediatrician within the electronic health record. Despite the prevalent of problems with medications, parent reported frequency of communication with the clinician about home medication use was low. Fewer than half reported talking with the clinician at the visit about medication. One in five parents of children in the intervention on prescription medications brought them to the visit; only 10% of control parents brought medication.
The high rate of parent-reported over-the-counter and prescription medication misuse has not been previously described. While several studies describe errors in parental dosing of fever reducer, parents in our study were often intentionally administering incorrect doses of fever reducer.7 Approximately one in five parents reported giving children under three years old cough medication. We were not able to identify how parents determine the dose of cough medication to give to their young children. Parents may be guessing about the proper dose for their young child, putting children at risk for overdoses.
Among parents of children on prescription medications, one in four reported sometimes altering doses or forgetting to give the medication. Parents misunderstand indications for the controller medication and half report using their controller medication during an asthma attack to relieve wheezing. Previous studies indicate that patients who do not understand the indication for medications have significantly poorer adherence.24
In contrast to previously reported successes in routine health maintenance areas, PHP had mixed results with regard to medication safety. We found significantly increased communication during the physical about medications when the child was on prescription medications and nearly twice as many PHP parents brought medications to the clinic than control parents. However, PHP was unable to improve upon medication reconciliation.
Most parents reported neither discussing medications nor bringing medications to the physical. This is consistent with several studies which demonstrate that patients do not discuss medication side effects, changes in dose, or failure to take medications or fill prescriptions with their doctors.11,12 Even in the PHP group, only 32% of parents brought medications to clinic to discuss with the clinician. In another research study, only 50% of pediatric cancer patients who were asked to bring medications actually brought them to clinic.10 Improved physician-parent communication about medication use is essential to improving the safety of home medication use.25 Given the high prevalence of misuse of medications we found in this study, and the AHRQ recommendation that parents bring medications to clinic, further work is needed to increase the number of parents who bring and discuss medications in clinic.
While this is a large prospective study, it does have some limitations. First, this was a single site study; future multisite studies are needed to improve generalizability of findings. Second, while this was a large study with 475 participants, the number of children in some subgroups, such as children with asthma taking daily controller medications, was relatively small. However, the overall finding of a significant population of parents misusing pediatric medications was consistent in larger and smaller subpopulations we analyzed. Medication misuse, and other measures, were gathered using self-report; while social desirability may bias the study toward the null, rates of misuse reported by parents were high.
Taken together, our study indicates that while most parents report taking medications properly, a significant portion of parents misuse over-the-counter and prescription medications, and this behavior is often intentional. In using prescription medications, parents sometimes alter the use of medications to fit their needs at home, resulting in medication errors and injuries.4 In this study, parents reported several practices which are likely to reduce the effectiveness of medications, including incorrect dosing of over-the-counter medications, missed doses of prescription medications, and using prescription asthma medications for the wrong indication. Parents also reported practices which can injure children, including intentionally over-dosing fever reducer, administering cough medication to young children, and altering prescription doses.
Conclusions
In this prospective study parents reported high rates of misuse of prescription and over-the-counter medication, often intentional. While use of the IVR system led to an increase in communication related to prescription medication, the low percent of parents who reported discussing their use of medications at the child's routine well child visits highlights the need for better systems and increased clinician focus on medication-related communication during visits if we are to continue to improve the safety of medication use in the home.
What's known on this subject.
Errors using pediatric over-the-counter and prescription medications are common. When patients skip or alter medication doses, they often do not tell their doctor. Electronic systems, frequently used to gather sensitive information, may be effective at collecting information about medication use.
What this study adds.
We developed a pre-visit interactive voice response system with tailored counseling. Of parent respondents, 17% reported incorrectly dosing fever-reducers, 33% non-adherence and 20% cough medication for children under three. Intervention parents reported significantly increased discussion of medications with the doctor.
Acknowledgments
Funding/Support: This work is also supported by the Agency for Healthcare Research and Quality (1 R18 HS17248-01)
Abbreviations
- PHP
Personal Health Partner
Footnotes
Financial Disclosure: The authors have indicated they have no financial relationships relevant to this article to disclose
Conflict of Interest: The authors have no conflicts of interest to disclose.
Clinical trials registration: This trial has been registered at www.clinicaltrials.gov (identifier NCT01188629).
Contributors Statement: Kathleen Walsh: Dr. Walsh conceptualized and designed the study, designed data collection instruments, oversaw analysis, drafted the initial manuscript, and approved the final manuscript as submitted.
Janine Bacic: Ms. Bacic coordinated data analysis, interpretation of results, critically reviewed the manuscript, and approved the final manuscript as submitted.
Barrett Phillips: Ms. Phillips designed data collection instruments, coordinated data collection, revised the initial manuscript, and approved the final manuscript as submitted.
William Adams: Dr. Adams conceptualized and designed the study, designed data collection instruments, led data collection, revised the initial manuscript, and approved the final manuscript as submitted.
References
- 1.Vernacchio L, Kelly JP, Kaufman DW, Mitchell AA. Medication Use Among Children <12 Years of Age in the United States: Results From the Slone Survey. Pediatrics. 2009;124:446. doi: 10.1542/peds.2008-2869. [DOI] [PubMed] [Google Scholar]
- 2.Yin HS, Dreyer BP, Foltin G, van Schaick L, Mendelsohn AL. Association of low caregiver health literacy with reported use of nonstandardized dosing instruments and lack of knowledge of weight-based dosing. Ambul Pediatr. 2007;7(4):292–298. doi: 10.1016/j.ambp.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 3.Walsh KE, Dodd KS, Seetharaman K, et al. Medication Errors among Adults and Children with Cancer in the Outpatient Setting. Journal of Clinical Oncology. 2009;6:891–896. doi: 10.1200/JCO.2008.18.6072. [DOI] [PubMed] [Google Scholar]
- 4.Walsh KE, Mazor KM, Stille CJ, et al. Medication errors in the homes of children with chronic conditions. Arch Dis Child. 2011;96:581–586. doi: 10.1136/adc.2010.204479. [DOI] [PubMed] [Google Scholar]
- 5.Frush KS, Luo X, Hutchinson P, Higgins JN. Evaluation of a method to reduce over-the-counter medication dosing error. Arch Pediatr Adolesc Med. 2004;158(7):620–624. doi: 10.1001/archpedi.158.7.620. [DOI] [PubMed] [Google Scholar]
- 6.McMahon SR, Rimsza ME, Bay RC. Parents can dose liquid medication accurately. Pediatrics. 1997;100(3 Pt 1):330–333. doi: 10.1542/peds.100.3.330. [DOI] [PubMed] [Google Scholar]
- 7.Yin M H Shonna, MS, Mendelsohn Alan L, MD, Wolf Michael S, PhD, MPH, Parker Ruth M, MAF, MD, van Schaick Linda, MSEd, Bazan Isabel S, BA, Kline Matthew D., MBPD, MD Parents' Medication Administration Errors: Role of Dosing Instruments and Health Literacy. Archives Pediatr Med Adolesc. 2010;164(2):181–186. doi: 10.1001/archpediatrics.2009.269. [DOI] [PubMed] [Google Scholar]
- 8.Bédard P, Tardif L, Ferland A, et al. A medication reconciliation form and its impact on the medical record in a paediatric hospital. Journal of Evaluation in Clinical Practice. 2011;17:222–227. doi: 10.1111/j.1365-2753.2010.01424.x. [DOI] [PubMed] [Google Scholar]
- 9.Kilcup M, Schultz D, Carlson J, Wilson B. Postdischarge pharmacist medication reconciliation: Impact on readmission rates and financial savings. J Am Pharm Assoc. 2013;53:78–84. doi: 10.1331/JAPhA.2013.11250. [DOI] [PubMed] [Google Scholar]
- 10.Taylor JA, Winter L, Geyer LJ, Hawkins DS. Oral outpatient chemotherapy medication errors in children with acute lymphoblastic leukemia. Cancer. 2006;107(6):1400–1406. doi: 10.1002/cncr.22131. [DOI] [PubMed] [Google Scholar]
- 11.Bedell SE, Jabbour S, Goldberg R, et al. Discrepancies in the use of medications: their extent and predictors in an outpatient practice. Arch Intern Med. 2000;160(14):2129–2134. doi: 10.1001/archinte.160.14.2129. [DOI] [PubMed] [Google Scholar]
- 12.Wilson IB, Schoen C, Neuman P, et al. Physician-Patient Communication about Prescription Medication Nonadherance: A 50-state Study of America's Seniors. Journal of General Internal Medicine. 2006;22(1):6–12. doi: 10.1007/s11606-006-0093-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Walsh KE, Stille CJ, Mazor KM, Gurwitz JH. Vol 4 Technology and Medication Safety. Agency for Healthcare Research and Qaulity; Aug, 2008. Using home visits to understand medication errors in children. [PubMed] [Google Scholar]
- 14.Li S, Lathcer B, Crain E. Acetaminophen and ibuprofen dosing by parents. Pediatric Emergency Care. 2000;16:394–397. doi: 10.1097/00006565-200012000-00003. [DOI] [PubMed] [Google Scholar]
- 15.Heubi JE, Barbacci MB, Zimmerman HJ. Therapeutic misadventures with acetaminophen: hepatoxicity after multiple doses in children. J Pediatr. 1998;132(1):22–27. doi: 10.1016/s0022-3476(98)70479-2. [DOI] [PubMed] [Google Scholar]
- 16.MD W. Kids' Cold Medicines: Guidelines. http://www.webmd.com/cold-and-flu/cold-guide/kids-cold-medicines-new-guidelines#1.
- 17.Cohen A. Infant deaths associated with cough and cold medications - Two states, 2005. MMWR. 2007;56(1):1–4. [PubMed] [Google Scholar]
- 18.Shehab N, Schaefer MK, Kegler SR, Daniel S, Budnitz M., MPH Adverse Events From Cough and Cold Medications After a Market Withdrawal of Products Labeled for Infants. Pediatrics. 2010;126(6):1100–1107. doi: 10.1542/peds.2010-1839. [DOI] [PubMed] [Google Scholar]
- 19.AHRQ, AAP. Patient fact sheet: 20 Tips to help prevent medical errors in chidlren. Rockville, MD: Agency for Healthcare Research and Quality; 2002. [Google Scholar]
- 20.Adams WG, Phillips BD, Bacic JD, Walsh KE, Shanahan CW, Paasche-Orlow MK. Automated Conversation System Before Pediatric Primary Care Visits: A Randomized Trial. Pediatrics. 2014;134(3):e1–9. doi: 10.1542/peds.2013-3759. [DOI] [PubMed] [Google Scholar]
- 21.Bass J. Framingham Safety Survey. J Pediatr. 1997;131(3):499–500. doi: 10.1016/s0022-3476(97)80092-3. [DOI] [PubMed] [Google Scholar]
- 22.Conn KM, Halterman JH, Fisher SG, Yoos HL, Chil NP, Szilagyi PG. Parental beliefs about medications and medication adherence among urban children with asthma. Ambul Pediatr. 2005;2005(5):306–310. doi: 10.1367/A05-004R1.1. [DOI] [PubMed] [Google Scholar]
- 23.Arozullah A, Yarnold P, Bennett C, et al. Development and validation of a short-form, rapid estimate of adult literacy in medicine. Medical Care. 2007;45(11):1026–1033. doi: 10.1097/MLR.0b013e3180616c1b. [DOI] [PubMed] [Google Scholar]
- 24.Fletcher S, Fletcher R, Pappius E, Rudd R. A teaching hospital medical clinic: secondary rather than primary care. J Med Educ. 1979;54(5):384–391. [PubMed] [Google Scholar]
- 25.Landrigan CP. New Questions on the Road to Safer Health Care. Pediatrics. 2013;131:e1621. doi: 10.1542/peds.2013-0647. [DOI] [PubMed] [Google Scholar]


