Abstract
Background and Objectives:
As the performance of minimally invasive hysterectomy has increased in the United States, the need to apply outcomes measures has also increased. This study was conducted to determine the impact of a fellowship-trained minimally invasive gynecologic surgery (MIGS) specialist on patient outcomes after laparoscopic hysterectomy (LH) in a gynecology department.
Methods:
This is a retrospective review of 218 patients who underwent a laparoscopic hysterectomy for benign indications at a suburban academic-affiliated tertiary care hospital with a broad patient base from 2010 to 2014.
Results:
A total of 218 women underwent conventional laparoscopic hysterectomy by 10 members of a gynecology department: 96 women (44%) by a MIGS specialist and 122 women (56%) by a group of general gynecologists. Operative time was less (119 vs 148 min; P < .001), and patients were more likely to be discharged on the same day (90.6% vs 66.4%; P < .001) for the MIGS specialist compared to other surgeons. More patients of the MIGS specialist had undergone prior laparotomies (42.7% vs 17.2%; P = < .001) and had a greater uterine weight (392 vs 224 g; P < .001). Although the difference was not statistically significant, conversion to laparotomy (0 vs 2 cases; P = .505) and postoperative infection (6 vs 16 cases; P = .095) were lower for the MIGS specialist. Total billing charges were also lower for the MIGS specialist ($9,920 vs $11,406; P < .001).
Conclusion:
A fellowship-trained MIGS specialist performed laparoscopic hysterectomy in less time on more difficult surgical patients, with a shorter length of stay and lower costs, and no difference in complications compared to other providers in a gynecology department.
Keywords: Hysterectomy, Minimally invasive gynecologic surgery, Outcomes
INTRODUCTION
Hysterectomy is the most common major gynecologic surgery, with millions performed annually worldwide.1 In the United States, 30.5% of hysterectomies are performed laparoscopically.2 This percentage continues to increase because of established reductions in perioperative morbidity and shorter recovery times compared with abdominal hysterectomy.3 Patient outcomes of laparoscopic hysterectomy are potentially further improved when the procedure is performed by a surgical subspecialist.
It is well established that high-volume surgeons have superior surgical outcomes for select procedures. The volume effect has been widely demonstrated for oncologic and cardiovascular procedures.4,5 Increasing evidence has also shown improved outcomes for high-volume gynecologists performing all types of hysterectomy.6–10 Similar data for high-volume gynecologic subspecialists in gynecologic oncology and urogynecology demonstrate reduced perioperative morbidity for hysterectomies performed for malignancy and pelvic reconstruction, respectively.11–15
Little is known about the specific influence of advanced training in minimally invasive gynecologic surgery (MIGS) on patient outcomes for laparoscopic hysterectomy. Advanced fellowship training in MIGS has been established to improve proficiency in gynecologic endoscopic procedures, including laparoscopic hysterectomy. MIGS fellowship programs not only operate with high volume but also perform laparoscopic hysterectomies with complex pelvic anatomy, adhesive disease, and large uteri. The objective of this study was to compare outcomes for laparoscopic hysterectomy performed by a fellowship-trained MIGS specialist and all other gynecologic surgeons in a gynecology department.
MATERIALS AND METHODS
Internal review board approval was obtained from Lahey Hospital and Medical Center. All patients who underwent a laparoscopic hysterectomy, either total or supracervical, at Lahey Hospital and Medical Center between October 2010 and September 2014 were identified from the operating room records. Ten gynecologists including a MIGS specialist and 9 general gynecologists, all of whom exclusively practice gynecology, performed the operations. To limit confounding variables, laparoscopic hysterectomies performed for malignant indications were excluded. Furthermore, laparoscopic hysterectomies with concomitant surgery other than adnexal surgery were excluded. In addition, robot-assisted laparoscopic hysterectomies were excluded because most cases in the department were performed via a conventional laparoscopic approach. The robot is used exclusively by the gynecologic oncologists in the department.
Information was collected from the medical record including patient characteristics, details of the procedure, perioperative outcomes, and costs. Patient demographics that were analyzed included age, body mass index (BMI), parity, and surgical history. Details of the procedure that were analyzed included the indications for hysterectomy, procedure type (total vs supracervical hysterectomy), findings, procedure duration, estimated blood loss, specimen pathology, uterine weight, and intraoperative complications. Intraoperative complications were defined as conversion to an open procedure, vessel or visceral organ injury, hemorrhage ≥1000 mL, and cardiopulmonary events. Postoperative outcomes that were analyzed included patient length of stay and postoperative complications. Postoperative complications were defined as readmissions, reoperations, bowel obstruction, ileus, pulmonary embolism, deep vein thrombosis, infection, hematoma, or seroma.
Cost data were collected from the hospital finance system. The analysis included total charges, total costs, and direct costs. Total charges included the set amount that the hospital charged a patient for all services provided. Total costs included direct plus indirect costs. Direct costs included patient-specific costs such as laboratory tests, medications, surgical supplies, operating room nursing time, and physician time. Indirect costs included hospital costs that cannot be identified with a particular patient or unit of the hospital such as information technology, financial services, and hospital facility maintenance. All cost data were adjusted for medical inflation using the Consumer Price Index and reported in 2010 U.S. dollars.16
Patient characteristics, details of the procedure, postoperative outcomes, and costs were compared for the MIGS specialist and other surgeons. Continuous variables were analyzed by using Student's t test or Mann-Whiney U-test, depending on the distribution of the data. Categorical variables were analyzed with Pearson's chi-square test or Fisher's exact test, as appropriate. Statistical significance was set at a value of P ≤ .05.
RESULTS
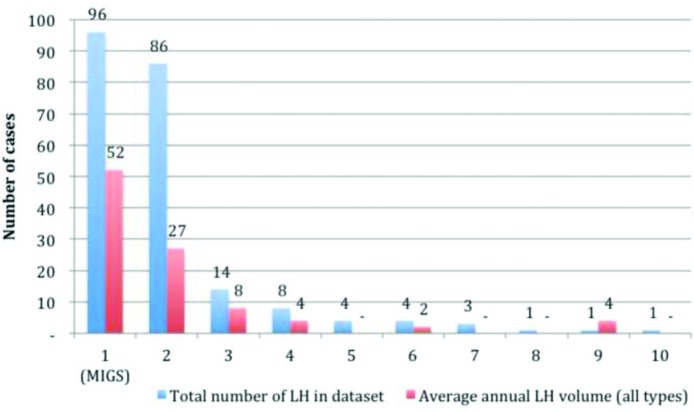
A total of 218 patients underwent conventional laparoscopic hysterectomy for benign disease, performed by 10 members of the gynecology department from 2010 through 2014. Ninety-six (44%) procedures were performed by a MIGS specialist and 122 (56%) were performed by a group of general gynecologists. The average annual laparoscopic hysterectomy volume was generated for each surgeon by reviewing total cases and the time the surgeon had been active at the institution (Figure 1). Total case volume was determined for all types of laparoscopic hysterectomy, including robot-assisted, and laparoscopic vaginal hysterectomy. The MIGS specialist and one other gynecologist met commonly used definitions of intermediate-to-high-volume surgeons with greater than 10 average annual cases.6
Figure 1.
Total number of laparoscopic hysterectomies (LH) over the 4-year period and average annual number of laparoscopic hysterectomies performed by 10 surgeons. The MIGS specialist is displayed on the left-most bars. Four surgeons do not have an average annual laparoscopic hysterectomy volume displayed, because they had been performing the procedure for less than a year.
The patients who underwent laparoscopic hysterectomy by the MIGS specialist and other gynecologists did not differ significantly in age, BMI, or parity (Table 1). Patients of the MIGS specialist had a greater number of prior laparotomies (42.7% vs 17.2%; P = < .001). The type of laparoscopic hysterectomy differed significantly, with more patients undergoing a total laparoscopic hysterectomy by the MIGS specialist (82.3% vs 26.2%; P < .001). Operative indications did not differ significantly with the exception of abnormal uterine bleeding, which was a less common indication for hysterectomy for patients of the MIGS specialist (52.1% vs 73.0%; P = .001). Operative findings did not differ with regard to the presence of leiomyoma (confirmed on pathology) or adhesions (seen at the time of procedure); however, the MIGS specialist had fewer patients with endometriosis at the time of the procedure (2.1% vs 9.8%; P = .020). Uterine weight was nearly twice as large for the MIGS specialist's patients (392.0 g vs 223.6 g; P < .001).
Table 1.
Patient and Procedure Characteristics by Surgeon
| MIGS (n = 96) | Other (n = 122) | P | |
|---|---|---|---|
| Age (y), median (95% CI) | 46.0 (44.0–49.0) | 46.5 (43.0–50.0) | .826 |
| BMI (kg/m2), median (95% CI) | 27.1 (23.8–31.5) | 26.3 (23.4–30.0) | .396 |
| Parous, n (%) | 80 (83.3) | 93 (76.9) | .239 |
| Prior laparotomy, n (%) | 41 (42.7) | 21 (17.2) | <.001 |
| Prior laparoscopy, n (%) | 39 (40.6) | 39 (32.0) | .215 |
| Hysterectomy type, n (%) | |||
| Total | 79 (82.3) | 32 (26.2) | <.001 |
| Supracervical | 17 (17.7) | 90 (73.8) | <.001 |
| Operative indications, n (%) | |||
| Abnormal uterine bleeding | 50 (52.1) | 89 (73.0) | .001 |
| Leiomyoma | 63 (65.6) | 70 (57.4) | .215 |
| Pelvic pain | 18 (18.8) | 30 (24.6) | .302 |
| Adenomyosis | 6 (6.3) | 11 (9.0) | .450 |
| Endometriosis | 4 (4.2) | 8 (6.6) | .442 |
| Endometrial hyperplasia | 4 (4.2) | 7 (5.7) | .759 |
| Cervical dysplasia | 1 (1.0) | 6 (4.9) | .138 |
| Pelvic organ prolapse | 3 (3.1) | 0 (0) | .084 |
| Operative findings, n (%) | |||
| Leiomyoma | 77 (80.2) | 99 (81.1) | .861 |
| Endometriosis | 2 (2.1) | 12 (9.8) | .020 |
| Adhesions | 37 (38.5) | 41 (33.6) | .450 |
| Uterine weight (g), mean (SD) | 392.0 (345.0) | 223.6 (191.6) | <.001 |
Perioperative outcomes including complications are listed in Table 2. Median operative time was less for the MIGS specialist (109.5 min, 95% CI 86.1–148.2, vs 136.2 min, 95% CI 117.0–163.2; P < .001). Patients were more likely to be discharged on the same day for the MIGS specialist (90.6% vs 66.4%, P < .001). Median estimated blood loss was the same for both groups (98.0 mL; P = <.001).
Table 2.
Perioperative Outcomes and Complications
| MIGS (n = 96) | Other (n = 122) | P | |
|---|---|---|---|
| Procedure duration (min), median (95% CI) | 109.5 (86.1–148.2) | 136.2 (117.0–163.2) | <.001 |
| Same-day discharge (days), n (%) | 87 (90.6) | 81 (66.4) | <.001 |
| Estimated blood loss (mL), median (95% CI) | 98.0 (98.0–100.0) | 98.0 (50.0–99.0) | <.001 |
| Intraoperative complications, n (%) | |||
| Conversions | 0 (0) | 2 (1.6) | .505 |
| Organ injury | 1 (1.0) | 0 (0) | .440 |
| Hemorrhage ≥1000 mL | 0 (0) | 0 (0) | – |
| Cardiopulmonary events | 0 (0) | 0 (0) | – |
| Postoperative complications, n (%) | |||
| Readmission | 1 (1.0) | 6 (4.9) | .138 |
| Reoperation | 0 (0) | 0 (0) | – |
| Bowel obstruction/ileus | 0 (0) | 1 (0.8) | 1.000 |
| PE/DVT | 0 (0) | 0 (0) | – |
| Infection | 6 (6.3) | 16 (13.1) | .095 |
| Hematoma/seroma | 1 (1.0) | 4 (3.3) | .387 |
| Urinary retention | 0 (0) | 1 (0.8) | 1.000 |
PE/DVT, pulmonary embolism/deep venous thrombosis.
Intraoperative and postoperative complications were rare overall, with no significant differences between the MIGS specialist and other surgeons. Although not statistically significant, no cases were converted to open procedures for the MIGS specialist, and 2 were converted for the other surgeons (P = .505). There was a single cystotomy for the MIGS specialist that occurred in a patient with 2 prior cesarean sections and adhesions and was repaired at the time of surgery by the MIGS specialist. There were no significant differences in readmission, reoperation, bowel obstruction, ileus, pulmonary embolism, deep vein thrombosis, infection, hematoma, seroma, or urinary retention. A single patient operated on by the MIGS specialist required readmission for management of bleeding from a vaginal laceration that occurred from uterine extraction. Six patients operated on by the other surgeons required readmission for various reasons including pelvic abscess, pelvic hematoma, pelvic seroma, small bowel obstruction, and pancreatitis. Postoperative infection was lower for the MIGS specialist (6 vs 16 cases; P = .095), but the difference was not statistically significant. Infections included pelvic abscess, vaginal cuff cellulitis, incisional cellulitis, and urinary tract infection. It is also worth noting that there were 9 total complications for the MIGS specialist and 30 total complications for the other surgeons.
Median costs are listed in Table 3. Total charges were lower for the MIGS specialist with a median total billing charge of $9,920 versus $11,406 (P < .001). Total and direct costs were not significantly different for the MIGS specialist and other surgeons.
Table 3.
Median Costs
| MIGS (n = 96) | Other (n = 143) | P | |
|---|---|---|---|
| Total charges | $9,920 (7,357–16,592) | $11406 (7,219–21,849) | <.001 |
| Total costs | $5,890 (4,243–9,743) | $6,252 (3,779–13,930) | .076 |
| Direct costs | $3,257 (2,389–5,498) | $3,069 (1,903–6,948) | .056 |
Data are expressed as median, minimum, and maximum in U.S. dollars.
DISCUSSION
Studies examining the relationship between surgeon volume and perioperative outcomes for laparoscopic hysterectomy have overall shown a positive correlation, although the data are conflicting. A large database analysis of 124,615 benign laparoscopic hysterectomies performed between 2000 and 2010 found significantly decreased morbidity, complications, length of stay, and resource utilization for high-volume surgeons.7 A prospective cohort of 1534 laparoscopic hysterectomies performed over 1 year showed no effect of surgical volume on estimated blood loss, operative time, or adverse events.10 A retrospective review of 877 benign laparoscopic hysterectomies showed decreased operating time, length of stay, and estimated blood loss with no difference in complications for high-volume surgeons.6
Although surgeon volume is an important indicator of surgical proficiency, it is not the sole determinant of patient outcomes. Fellowship training increases surgical volume, increases exposure to surgically challenging cases, and often teaches a reproducible method of tackling these challenges. Few studies have looked directly at the impact of fellowship training in gynecologic subspecialties. In the general surgery literature, a review of 23 studies demonstrated a positive impact of fellowship training on patient outcomes across several surgical subspecialties.17 This meta-analysis showed a lower conversion of laparoscopic to open procedures for fellowship-trained minimally invasive surgeons. Of the 11 studies comparing fellowship-trained surgeons to those without fellowship training, one study showed increased survival, another showed decreased length of stay, and the remainder showed no difference in patient outcomes.
Our study showed that a fellowship-trained MIGS specialist performs laparoscopic hysterectomy on larger uteri with decreased operative time and no significant difference in perioperative complications. Patients undergoing laparoscopic hysterectomy by the MIGS specialist had uteri nearly twice as large and more prior surgeries. Procedure time and length of stay were also significantly shorter, which may contribute to decreased total charges. The MIGS specialist had a lower conversion rate and fewer overall perioperative complications, though these outcomes were rare and did not reach statistical significance. Our results emphasize the positive impact of a MIGS specialist when compared to other gynecologists in a department.
Endometriosis was more commonly reported as an intraoperative finding by the other gynecologists than by the MIGS specialist. Endometriosis may have increased the difficulty of laparoscopic hysterectomy in these patients; however, visualization is subjective, and its presence alone does not indicate the extent of the disease or complexity of the procedure. The specific training of the MIGS specialist may also lead one to report endometriosis only if proven by biopsy.
Also, total and supracervical laparoscopic hysterectomies were not evenly distributed across the groups, with the MIGS specialist performing 82.3% total hysterectomies compared to 26.2% for the other surgeons (P < .001). The differences in chosen procedure may reflect a comfort level with each procedure or with laparoscopic suturing. This discrepancy may affect our results, given that a large Cochrane review comparing total with supracervical hysterectomy showed a clinically insignificant increase in blood loss (57 mL) and procedure duration (11 min) for total versus supracervical hysterectomy.18 Our study found a clinically insignificant increase in blood loss for the MIGS specialist, the procedure duration was shorter for the MIGS specialist, despite the greater proportion of total hysterectomies. The Cochrane review also showed a higher likelihood of postoperative fever and urinary retention for total compared to supracervical hysterectomy, neither of which was more likely for patients operated on by the MIGS specialist, despite the greater proportion of total hysterectomies.
A strength of this study is that all data were taken from a single gynecology department that exclusively performs gynecologic procedures at one hospital. This underscores the comparative value of MIGS training, even when compared to other gynecologists of all surgical volumes exclusively performing these procedures. The study takes place over 4 years, encompassing multiple surgeons and procedures. The study was performed at a single institution with the same operating room staff and trainee team, reducing external factors on perioperative outcomes.
Our study is limited by its retrospective nature and that only one MIGS specialist was examined. Surgical outcomes are a function of many factors and it is difficult to isolate the impact of surgeon training in a retrospective cohort with one MIGS specialist. Many gynecology departments across the country have only 1 or 2 MIGS specialists, at most. A multi-institutional study may make it difficult to account for institutional, patient, and regional differences. Although differences in patient characteristics, including prior surgeries and uterine weight, highlight the challenging laparoscopic cases selected by the MIGS specialist, other unmatched characteristics may affect the results.
Future studies should expand to include multiple MIGS-trained surgeons to encompass the breadth of the subspecialty and fellowship training. A larger sample size would also improve the ability to detect a difference in rare complications. Future studies should also include multiple minimally invasive procedures, including robot-assisted laparoscopic hysterectomy and other procedures emphasized during fellowship training.
CONCLUSION
A MIGS surgeon performed laparoscopic hysterectomy in less time on more difficult surgical patients, with a shorter length of stay and lower charges and no difference in complications compared to other providers in a gynecology department. Our findings demonstrate the benefits of advanced training in MIGS for patients undergoing laparoscopic hysterectomy. Advanced training in MIGS is a valuable means of providing safe surgical care and improving access to minimally invasive surgery for challenging surgical candidates. Further work is necessary to determine the relationship between MIGS subspecialization and patient perioperative morbidity.
Contributor Information
Nisse V. Clark, Department of Obstetrics and Gynecology, Brigham and Women's Hospital, Boston, Massachusetts..
Harneet S. Gujral, Department of Obstetrics and Gynecology, Brigham and Women's Hospital, Boston, Massachusetts..
Kelly N. Wright, Department of Obstetrics and Gynecology, Cedars-Sinai Medical Center, Los Angeles, California..
References:
- 1. Garry R. Health economics of hysterectomy. Best Pract Res Clin Obstet Gynaecol. 2005;19:451–465. [DOI] [PubMed] [Google Scholar]
- 2. Wright JD, Ananth CV, Lewin SN, et al. Robotically assisted vs laparoscopic hysterectomy among women with benign gynecologic disease. JAMA. 2013;309:689–698. [DOI] [PubMed] [Google Scholar]
- 3. Nieboer TE, Johnson N, Lethaby A, et al. Surgical approach to hysterectomy for benign gynaecological disease. The Cochrane Database of Systematic Reviews. 2009;12:CD003677. [DOI] [PubMed] [Google Scholar]
- 4. Birkmeyer JD, Stukel TA, Siewers AE, Goodney PP, Wennberg DE, Lucas FL. Surgeon volume and operative mortality in the United States. N Engl J Med. 2003;349:2117–2127. [DOI] [PubMed] [Google Scholar]
- 5. Chowdhury MM, Dagash H, Pierro A. A systematic review of the impact of volume of surgery and specialization on patient outcome. Br J Surg. 2007;94:145–161. [DOI] [PubMed] [Google Scholar]
- 6. Vree FE, Cohen SL, Chavan N, Einarsson JI. The impact of surgeon volume on perioperative outcomes in hysterectomy. JSLS. 2014;18:174–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wallenstein MR, Ananth CV, Kim JH, et al. Effect of surgical volume on outcomes for laparoscopic hysterectomy for benign indications. Obstet Gynecol. 2012;119:709–716. [DOI] [PubMed] [Google Scholar]
- 8. Boyd LR, Novetsky AP, Curtin JP. Effect of surgical volume on route of hysterectomy and short-term morbidity. Obstet Gynecol. 2010;116:909–915. [DOI] [PubMed] [Google Scholar]
- 9. Doll KM, Milad MP, Gossett DR. Surgeon volume and outcomes in benign hysterectomy. J Minim Invasive Gynecol. 2013;20:554–561. [DOI] [PubMed] [Google Scholar]
- 10. Twijnstra AR, Blikkendaal MD, van Zwet EW, et al. Predictors of successful surgical outcome in laparoscopic hysterectomy. Obstet Gynecol. 2012;119:700–708. [DOI] [PubMed] [Google Scholar]
- 11. Wright JD, Lewin SN, Deutsch I, Burke WM, Sun X, Herzog TJ. Effect of surgical volume on morbidity and mortality of abdominal hysterectomy for endometrial cancer. Obstet Gynecol. 2011;117:1051–1059. [DOI] [PubMed] [Google Scholar]
- 12. Yasunaga H, Nishii O, Hirai Y, Ochiai K, Matsuyama Y, Ohe K. Impact of surgeon and hospital volumes on short-term postoperative complications after radical hysterectomy for cervical cancer. J Obstet Gynaecol Res. 2009;35:699–704. [DOI] [PubMed] [Google Scholar]
- 13. Rogo-Gupta LJ, Lewin SN, Kim JH, et al. The effect of surgeon volume on outcomes and resource use for vaginal hysterectomy. Obstet Gynecol. 2010;116:1341–1347. [DOI] [PubMed] [Google Scholar]
- 14. Sung VW, Rogers ML, Myers DL, Clark MA. Impact of hospital and surgeon volumes on outcomes following pelvic reconstructive surgery in the United States. Am J Obstet Gynecol. 2006;195:1778–1783. [DOI] [PubMed] [Google Scholar]
- 15. Anger JT, Rodríguez LV, Wang Q, Pashos CL, Litwin MS. The role of provider volume on outcomes after sling surgery for stress urinary incontinence. J Urol. 2007;177:1457–1462. [DOI] [PubMed] [Google Scholar]
- 16. U. S. Department of Labor Bureau of Labor Statistics. Consumer Price Index, 2014. Available at: http://www.bls.gov/cpi/. Retrieved August 30, 2015.
- 17. Johnston MJ, Singh P, Pucher PH, et al. Systematic review with meta-analysis of the impact of surgical fellowship training on patient outcomes. Br J Surg. 2015;102:1155–1166. [DOI] [PubMed] [Google Scholar]
- 18. Lethaby A, Mukhopadhyay A, Naik R. Total versus subtotal hysterectomy for benign gynaecologic conditions. The Cochrane Database of Systematic Reviews. 2012; 10.1002/14651858.CD004993.pub3. [DOI] [PubMed] [Google Scholar]