Abstract
Background and Objectives:
Robot-assisted hernia repair, combined with endoscopic component separation, has reduced recurrence and complication rates and allowed immediate intervention in obese patients. We sought to study surgical outcomes in this high-risk group of patients in a community hospital.
Methods:
We conducted a retrospective chart review of ventral, incisional, and umbilical hernia repairs performed at a small community hospital by a single surgeon from March 2014 through November 2016, with statistical analysis of the surgical outcomes. Patients included were those who underwent hernia repair during the study period and had a body mass index (BMI) >30. Patients were followed up for a minimum of 6 months (range, 6–37).
Results:
Forty-seven hernia repairs were performed, including 33 combined and 14 control cases. The demographics of each group were comparable when comparing sex, age, BMI, and ASA classification. Mean follow-up was 19.39 months in the study group and 28.64 months in the control group. There were no significant differences in total operative time, estimated blood loss, conversion rates, or hospital length of stay. Two complications occurred in each of the study and control groups, with no recurrences in the study group and 3 in the control group and no mortalities.
Conclusion:
Robotic laparoscopic repair of abdominal wall defects offers significant advantages, including easier primary defect closure. Our analyses showed that combining robot-assisted hernia repair with mesh and endoscopic component separation is an effective intervention in obese patients.
Keywords: da Vinci S, Incisional hernia, Obesity, Robotic general surgery, Ventral hernia
INTRODUCTION
Abdominal wall hernia repair is the most common major surgical procedure performed by general surgeons today, with ventral hernias accounting for ∼30% of that group.1 In this study, we focused on ventral, umbilical, and incisional hernias. The repair of anterior abdominal wall defects is well documented in the literature. Regardless of the use of open or laparoscopic repair, hernia repair is fraught with high recurrence rates when performed in obese patients. Many techniques have been described to successfully close these defects, ranging from open to laparoscopic, and more recently, robot-assisted laparoscopic approaches.1–3 All of these techniques provide reasonable outcomes, and advantages have been identified among the techniques. The differences between these groups have been debated for more than a decade, with the more recent literature suggesting some advantages of laparoscopy over open repair, particularly in reduction of wound complications.4 Both robotics and laparoscopy have been shown to be as good, if not better, in rates of recurrence when compared to open repair. The robotic platform potentially offers some advantage over laparoscopy, with the ability to perform intracorporeal sutures very quickly and effectively.5 One aspect of ventral, umbilical, and incisional hernia repair that is not debated is the significantly increased rate of recurrence in obese patients.6,7 This is a population that has several-fold higher recurrence rates versus nonobese patients,8 and in addition, there are higher rates of complications after hernia repair.9,10 The obese population is growing rapidly in the United States, with the overall incidence of obesity on the rise, as well as the number of procedures performed in this population, with the advent of bariatric surgeries.9 With this growing population, there is a need for further study to improve outcomes in hernia repair, an extremely common procedure in this high-risk group.
METHODS
With the approval of the Institutional Review Board of Florida State University College of Medicine, all ventral, incisional, and umbilical hernia repairs performed by a single surgeon at our institution were reviewed. In this study we focus on robot-assisted hernia repairs in obese patients. We conducted a retrospective chart review of ventral, incisional, and umbilical hernia repairs performed from March 2014 through November 2016, with statistical analysis of the following surgical endpoints: recurrence, operative time (broken down into: total operative time, docking time, and console time), estimated blood loss (EBL), conversion rates (to open surgery), 30 d morbidity and mortality, hospital readmission and emergency department visits, surgical site infection (SSI), and surgical site occurrences (SSO). Control cases are represented by patients operated on before the surgeon incorporated component separation into his practice. After implementation, the surgeon decided his standard of care would be to offer component separation to all patients with BMI >30. Thus, cases chosen for the study group were those in which patients had a BMI >30 and underwent surgery during this period (Figure 1). As stated earlier, The control group comprised patients who underwent hernia repair before the incorporation of component separation in addition to those who did not qualify for the study group (BMI <30). Patients were followed up after surgery for a minimum of 6 months (range, 6–37). The analysis compared the above listed outcomes in the study group with those of the control group.
Figure 1.
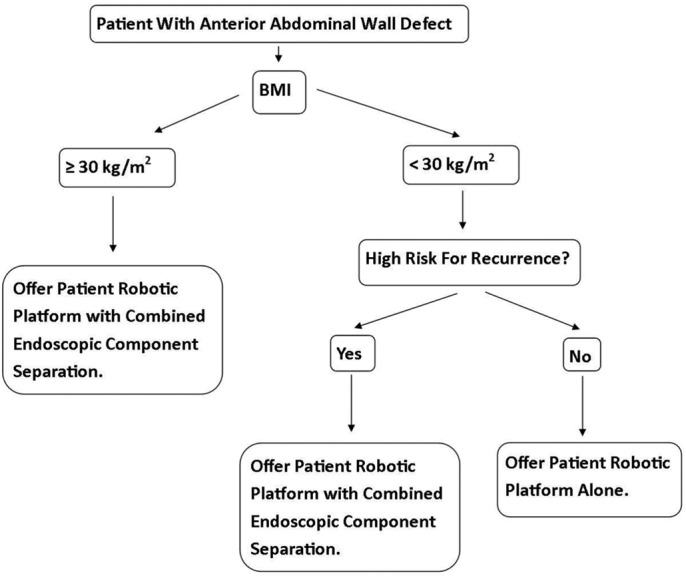
Algorithm depicting clinical decision making.
Surgical Technique
Individuals in the study group underwent ventral, incisional, and umbilical hernia repairs with the robot-assisted technology of the da Vinci S and, in later cases, the da Vinci Si surgical system. Before port placement, all patients in the study group underwent bilateral endoscopic component separation (with the exception of 1 patient who had unilateral component separation because of previous surgery), with an anterior approach. Bilateral 1.5-cm incisions were made at approximately the level of the umbilicus (Figure 2). A space was created between the planes of the external and internal oblique muscles that was continued superiorly. The space was entered with the laparoscopic hook cautery device, and the external oblique aponeurosis was released lateral to the linea semilunaris (Figure 3). Upon completion of the component separation, the robotic ports were placed. The hernia contents were reduced, with primary closure of the defect. An appropriate-size composite mesh was then placed and sutured with the robotic instruments (Figure 4). Control group individuals underwent an identical robotic procedure, without component separation.
Figure 2.
Image showing the size of the defect and planned sites for anterior component separation.
Figure 3.
Release of external oblique fascia lateral to the linea semilunaris.
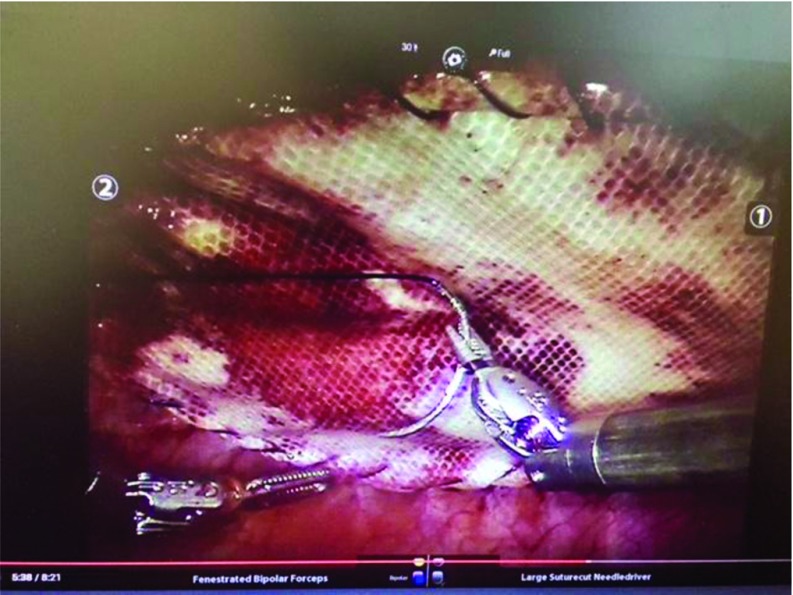
Figure 4.
Suturing of mesh after primary closure of the defect.
Data Analysis
Descriptive statistics are presented for both the study and control groups, with means, standard deviations, and ranges for numerical variables and proportions for categorical variables. The groups were compared on categorical variables by using chi square statistics. For numerical variables, the groups were compared by using t tests (with or without Satterthwaite correction for unequal variances). For all the analyses, P < .05 was considered significant. All analyses were performed with SAS (Statistical Analysis System) software. A post hoc power analysis for 2 independent-samples t test demonstrated 74.1% power.
RESULTS
A total of 47 ventral, incisional, and umbilical hernia repairs were performed. Our study included 33 combined-approach and 14 control cases. The defect size in both groups ranged from 3 to 12 cm. Size estimates were based on clinical examination and intraoperative estimates. The study group consisted of 19 women (57.6%) and 14 men (42.4%), and the control group consisted of 11 women (78.6%) and 3 men (21.4%). The mean BMI for the study group was 36.2 (range, 30–44.6), and average age was 52.2 (range, 29–77). The mean BMI for the control group was 33.1 (range, 22.5–80.1), and the average age was 50.3 (range, 34–81). Table 1 presents the descriptive statistics for the demographic characteristics of both groups. The demographics of each group were comparable for sex, age, BMI, and ASA class. Groups were created based on the methods described above. Groups consisted of ventral and incisional hernias and one large >- cm umbilical hernia (Table 2). Incisional hernias consisted of post-site hernias, previous exploratory laparotomy incisions, and recurrent umbilical hernias. The groups were observed after surgery in a retrospective manner. The study group was followed for a mean of 19.39 ± 7.06 months after surgery (range, 6–29). The control group was followed up for a mean of 28.64 ± 7.07 months after surgery (range, 18–37). Table 3 presents the descriptive statistics for the outcome variables in the study and control groups. The outcomes comparison can be found in Table 4. There were no significant differences in total operative time, EBL, conversion rate, or hospital length of stay (LOS). Two complications (6.06%) occurred in the study group: superficial cellulitis at the component separation incision and minor skin dehiscence at a port site. Two complications (14.29%) occurred in the control group; an intra-abdominal abscess caused by perforation of an enterorrhaphy for a small serosal tear and prolonged postoperative pain. There were no recurrences reported in the study group, during a median follow-up of 19.4 months (range, 6–29). Three recurrences were recorded in the control group, with a median follow-up of 28.6 months (range, 18–37). No mortalities occurred in either group, and all complications were resolved with good outcomes. A postoperative global health assessment was performed via phone interviews with the PROMIS v 1.1 Global Health Scale,11 and no significant differences in postoperative quality of life were found.
Table 1.
Group Demographics
| Characteristic | Study | Control | P |
|---|---|---|---|
| Age (mean ± SD) | 52.18 ± 14.12 | 50.29 ± 15.15 | .69 |
| Sex (female) | 19 (57.58%) | 11 (78.57%) | .63 |
| BMI (mean ± SD) | 36.24 ± 4.72 | 33.09 ± 15.52 | .46 |
| ASA | 2.61 | 2.07 | .23 |
N = 47.
Table 2.
Individual Procedure Breakdown
| Procedure | Male (n) | Female (n) | Total, n (%) |
|---|---|---|---|
| Study group (n = 33) | n = 14 | n = 19 | n = 33 |
| Ventral hernia repair | 8 | 9 | 17 (51.5) |
| Incisional hernia repair | 6 | 10 | 16 (48.5) |
| Umbilical hernia repair | 0 | 0 | 0 (0.0) |
| Control group (n = 14) | n = 3 | n = 11 | n = 14 |
| Ventral hernia repair | 1 | 3 | 4 (28.6) |
| Incisional hernia repair | 2 | 7 | 9 (64.3) |
| Umbilical hernia repair | 0 | 1 | 1 (7.1) |
Table 3.
Outcomes
| Outcome Measure | Mean ± SD or Incidence, n (%) |
|---|---|
| Study group (n = 33) | |
| Operative time (minutes) | 154.0 ± 44.18 |
| Console time (minutes) | 74.18 ± 30.01 |
| EBL (mean mL) | 18.9 |
| LOS (mean days) | 1.00 |
| Complications | 2 (6.1) |
| 30-Day morbidity | 0 (0.0) |
| Recurrences | 0 (0.0) |
| Follow-up achieved | 28 (84.8) |
| Control group (n = 14) | |
| Operative time (minutes) | 180.4 ± 59.81 |
| Console time (minutes) | 123.00 ± 65.04 |
| EBL (mean mL) | 17.9 |
| LOS (mean days) | 1.00 |
| Complications | 2 (15.4) |
| 30 Day morbidity | 1 (7.7) |
| Recurrences | 3 (23.1) |
| Follow-up Achieved | 11 (84.6) |
Table 4.
Outcome Comparison
| Study (n = 33) | Control (n = 14) | Statistical Test | P | |
|---|---|---|---|---|
| Operative Time (mean minutes ± SD) | 154.0 ± 44.18 | 180.4 ± 59.81 | Satterthwaite | .15 |
| Console time (mean minutes ± SD) | 74.18 ± 30.01 | 123.00 ± 65.04 | Satterthwaite | .02* |
| EBL (mean mL) | 18.9 | 17.9 | Satterthwaite | .69 |
| LOS (mean days) | 1.00 | 1.00 | Satterthwaite | – |
| Complications | 2 (6.1) | 2 (15.4) | Fisher's exact | .27 |
| 30 day morbidity | 0 (0.0) | 1 (7.7) | Fisher's exact | .30 |
| Recurrences | 0 (0.0) | 3 (23.1) | Fisher's exact | .02* |
| Follow-up Achieved | 28 (84.8) | 11 (84.6) | Fisher's exact | .73 |
Data are expressed as number of incidences (% of total cases), unless otherwise specified.
*Statistically significant outcome.
DISCUSSION
Treatment of ventral hernias in obese patients is known for high perioperative morbidity and recurrence. The advent of laparoscopy reduced the rates of complications, and the technique has been validated as a safe and effective option for treating these defects; however, the complication rates are still unacceptably high.2 Repair with the robotic platform combined with endoscopic component separation at the time of the primary repair may offer significant improvement in perioperative complications and recurrences. Overall, the incidence of complications in our study group was 6.06% compared to 14.29% in the control group, but because of the small sample, these data are not statistically significant. We also found that the data favored the study group rates of recurrence during the follow-up period. Three recurrences were observed in the control group, compared to none in the study group—a statistically significant result, although we recognize that this finding is somewhat limited by the follow-up period and small sample size. The combined technique enabling primary closure of the defect in a tension-free manner,12 assisted by the addition of the endoscopic component separation,13 was the key factor in improving outcomes in our patients. This improvement is in addition to any possible advantage offered by the robotic platform itself. Despite a small sample, particularly in our control group, our data showed that there was potential benefit gained from the addition of component separation. This technique may give surgeons more confidence in performing surgeries in this patient population. Some hold the opinion that elective operations on these patients should be deferred until significant weight loss is achieved. Our data suggest that such a delay is not necessary and that these patients can be operated on while still obese, with good outcomes.
The growing use of component separation in complex abdominal wall reconstruction has led to a significant increase in the techniques and options for performing component separation. We will not discuss the various new techniques that have arisen since the start of our study period, the most notable of which is the TAR (transversus abdominis release). It is important to note, however, that there is evidence to suggest a benefit to endoscopic component separation. It has been shown in the literature that the technique is a good option for reducing wound complications when compared to open component separation.14–16 This finding is supported by our study outcomes, with only 1 complication (3.03%) associated with the component separation.
Using this study, in addition to other studies cited in this article, we devised an algorithm (Figure 1), which the surgeon used for clinical decision-making when performing operative planning for these patients. As depicted in the algorithm, all patients with BMI >30 were offered component separation because of the inherent risk in that population. Other comorbidities, such as chronic steroid use were discussed, and we had 1 chronic steroid user who fit the study group cutoff of BMI >30 and thus was already included in the study group. We created another group, which was not represented in our study sample, that would include nonobese patients with other comorbidities such as diabetes, chronic steroid or other tissue-compromising drug use, or conditions that would predispose them to an increased risk of recurrence and complications. It is our hope that, with further study and an increasing number of cases, we can generate data to report on this cohort as well.
These procedures were performed safely in a small community hospital setting. As discussed in a previous publication, the robotic platform can be safely instituted in a small community hospital with excellent outcome for patients.17
Limitations
One of the major limitations of the study is the relatively short follow-up period for patients. The rate of recurrence would probably be slightly higher if a 5- to 10-year follow-up had been included.
CONCLUSION
In this retrospective case series, it appears that anterior abdominal wall defects can be successfully managed in obese patients by using this combined technique. These early data show that this technique can reduce complications and 30-day morbidity in these patients and suggest that there is potential for significant reduction in recurrence rates in this highly vulnerable population. A more extended follow-up and larger study sample are needed to confirm our findings, but early data are encouraging.
Contributor Information
Rodolfo J. Oviedo, Department of Surgery, Florida State University College of Medicine, Tallahassee, Florida, USA..
Jarrod C. Robertson, Department of Surgery, Florida State University College of Medicine, Tallahassee, Florida, USA..
Apurva Sunder Desai, University Department of Statistics, Florida State University, Tallahassee, Florida, USA..
References:
- 1. Gonzalez AM, Romero RJ, Seetharamaiah R, Gallas M, Lamoureux J, Rabaza JR. Laparoscopic ventral hernia repair with primary closure versus no primary closure of the defect: potential benefits of the robotic technology. Int J Med Robot. 2015;11:120–125. [DOI] [PubMed] [Google Scholar]
- 2. Heniford BT, Park A, Ramshaw BJ, Voeller G. Laparoscopic ventral and incisional hernia repair in 407 patients. J Am Coll Surg. 2000;190:645–650. [DOI] [PubMed] [Google Scholar]
- 3. Allison N, Tieu K, Snyder B, Pigazzi A, Wilson E. Technical feasibility of robot-assisted ventral hernia repair. World J Surg. 2012;36:447–452. [DOI] [PubMed] [Google Scholar]
- 4. Mann CD, Luther A, Hart C, Finch JG. Laparoscopic incisional and ventral hernia repair in a district general hospital. Ann R Coll Surg Engl. 2015;97:22–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tayar C, Karoui M, Cherqui D, Fagniez PL. Robot-assisted laparoscopic mesh repair of incisional hernias with exclusive intracorporeal suturing: a pilot study. Surg Endosc. 2007;21:1786–1789. [DOI] [PubMed] [Google Scholar]
- 6. Wassenberg D, Zarmpis N, Seip N, Ambe PC. Closure of small and medium size umbilical hernias with the Proceed Ventral Patch in obese patients: a single center experience. Springerplus. 2014;3:686–690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Froylich D, Segal M, Weinstein A, Hatib K, Shiloni E, Hazzan D. Laparoscopic versus open ventral hernia repair in obese patients: a long-term follow-up. Surg Endosc. 2016;30:670–675. [DOI] [PubMed] [Google Scholar]
- 8. Sauerland S, Korenkov M, Kleinen T, Arndt M, Paul A. Obesity is a risk factor for recurrence after incisional hernia repair. Hernia. 2004;8:42–46. [DOI] [PubMed] [Google Scholar]
- 9. Raftopoulos I, Courcoulas AP. Outcome of laparoscopic ventral hernia repair in morbidly obese patients with a body mass index exceeding 35 kg/m2. Surg Endosc. 2007;21:2293–2297. [DOI] [PubMed] [Google Scholar]
- 10. Marx L, Raharimanantsoa M, Mandala S, D'Urso A, Vix M, Mutter D. Laparoscopic treatment of incisional and primary ventral hernia in morbidly obese patients with a BMI over 35. Surg Endosc. 2014;28:3310–3314. [DOI] [PubMed] [Google Scholar]
- 11. Introduction to the PROMIS Global Health Scale. Bethesda, MD: National Institutes of Health; Available at http://www.healthmeasures.net/explore-measurement-systems/promis Accessed August 14 2017. [Google Scholar]
- 12. Strey CW. Triple-step laparoscopic incisional hernia repair: midline suture closure supported by dorsal component separation and intraperitoneal onlay mesh reinforcement. World J Surg. 2014;38:3276–3279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gonzalez R, Rehnke RD, Ramaswamy A, Smith CD, Clarke JM, Ramshaw BJ. Components separation technique and laparoscopic approach: a review of two evolving strategies for ventral hernia repair. Am Surg. 2005;71:598–605. [PubMed] [Google Scholar]
- 14. Jensen KK, Henriksen NA, Jorgensen LN. Endoscopic component separation for ventral hernia causes fewer wound complications compared to open components separation: a systematic review and meta-analysis. Surg Endosc. 2014;28:3046–3052. [DOI] [PubMed] [Google Scholar]
- 15. Ghali S, Turza KC, Baumann DP, Butler CE. Minimally invasive component separation results in fewer wound-healing complications than open component separation for large ventral hernia repairs. J Am Coll Surg. 2012;214:981–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Fox M, Cannon RM, Egger M, Spate K, Kehdy FJ. Laparoscopic component separation reduces postoperative wound complications but does not alter recurrence rates in complex hernia repairs. Am J Surg. 2013;206:869–874; discussion 874–865. [DOI] [PubMed] [Google Scholar]
- 17. Oviedo RJ, Robertson JC, Alrajhi S. First 101 robotic general surgery cases in a community hospital. JSLS. 2016. Jul-Sep;20(3):e2016.00056 DOI: 10.4293/JSLS.2016.00056. [DOI] [PMC free article] [PubMed] [Google Scholar]