Abstract
Background
Intra-abdominal fat is an important factor in determining the metabolic syndrome/insulin resistance, and thus the risk of diabetes and ischaemic heart disease. Computed Tomography (CT) fat segmentation represents a defined method of quantifying intra-abdominal fat, with attendant radiation risks. Bioimpedance spectroscopy may offer a method of assessment without any risks to the patients. A comparison is made of these two methods.
Methods
This was a preliminary study of the utility of multifrequency bioimpedance spectroscopy of the mid abdomen as a measure of intra-abdominal fat, by comparison with fat segmentation of an abdominal CT scan in the −30 to −190 HU range.
Results
There was a significant (P < 0.01) correlation between intra-abdominal fat and mid-upper arm circumference, as well as the bioimpedance parameter, the R/S ratio. Multivariate analysis showed that these were the only independant variables and allowed the derivation of a formula to estimate intra-abdominal fat: IAF = 0.02 × MAC − 0.757 × R/S + 0.036.
Conclusions
Circumabdominal bioimpedance spectroscopy may prove a useful method of assessing intra-abdominal fat, and may be suitable for use in studies to enhance other measures of body composition, such as mid-upper arm circumference.
Introduction
Obesity and rising BMI is a feature of life in the Western world with the average BMI in the United States being 28.8 kg/m2, second only in the world, rather surprisingly, to Kuwait (29.5 kg/m2). Malawi, by contrast, has an average BMI of 22.2 kg/m2, and the lowest average BMI in the world is found in Bangladesh (20.2). Expressed another way, 68% of the US population and 61% of the UK population were overweight (BMI > 25) in 2008 and 33.8% (US) and 22.7% (UK) were obese (BMI > 30).1 In Africa, although obesity is still found in resource-poor settings among the affluent elite, malnutrition is a more pressing issue for the common man.
In day to day clinical practice surrogates such as waist circumference, waist:hip ratio and body mass index (BMI) are used to assess body fat. However, individuals with the same BMI may have different body composition and BMI is particularly influenced by muscle bulk and skeletal frame size. Furthermore it is the intra-abdominal fat in particular rather than obesity in general that has a poor prognostic significance for the metabolic syndrome2 or insulin resistance, and hence of diabetes and ischaemic heart disease. Parameters such as the BMI, waist:hip ratio, and mid arm circumference are crude and a better measure of intra-abdominal fat is needed.
Accurate measurement of body composition and body fat requires Computerised Tomography (CT) scanning, dual-energy X-ray absorptiometry (DEXA) or isotope dilution methods, but such methods are not all widely available and are associated with radiation exposure. MRI offers an advantage for composition measurement of no radiation exposure but is more suited to static organs such as the brain and may be limited by gut movement artifact in the abdomen because of slower acquisition speeds, quite apart from the high cost and limited availability particularly in low resource settings. By contrast, bioimpedance measurement is totally harmless and painless and is a well established method of assessing body composition in common use by health screening clinics and health and fitness clubs. It also forms the basis of a method of obtaining images of the human body by electrical impedance tomography (EIT).3 Single frequency bioimpedance meters are commercially available (e.g. BodyStat, UK) and multi-frequency meters are becoming available (e.g. Xitron, US and BodyStat, UK). Bioimpedance spectroscopy has been proposed as a method of detecting cardiac rejection post transplant,4 and is used to estimate body fluid composition in critical care.5 By using a multifrequency measurement of bioimpedance and using a curve fitting routine to derive a Cole-Cole equation model, a more accurate assessment of intracellular and extracellular bioimpedance (and hence fat content) can be made, by contrast with the single frequency meters which give a single impedance measurement and hence do not allow differentiation of the various components of the impedance (capacitance, resistance etc).
The aim of this study was to derive a measure of intra-abdominal fat (IAF) content using bioimpedance measurements validated against CT scan estimations of IAF.
Methods
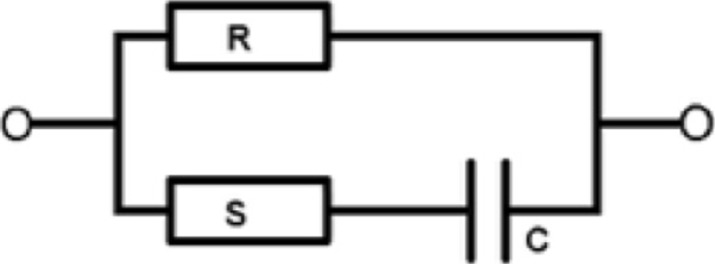
Biological tissue has an impedance to an applied electrical current which depends upon the frequency of the alternating current and on the nature and substance of the tissue under study. The electrical conductivity of living tissue can be modeled by the circuit diagram shown in Figure 1.
Figure 1.
Equivalent circuit modeling biological tissue
The values for the elements can be derived by fitting observed impedance at various frequencies to a mathematical model described by the following Cole-Cole equation6:
The value of the resistances R (R0) and S (derived from R0 and R∞) represent the contributions offered by the extracellular (R) and intracellular (S) fluid component respectively, whilst the capacitance C represents the cell membrane. The factor α in the Cole-Cole equation represents a dispersion coefficient which also characterises the tissue. Fatty tissue, which is non-conductive, displaces conductive electrolyte fluid and hence increases the impedance offered by fatty tissue to an applied current.
Subjects were patients undergoing CT scan of the abdomen for various indications, but with no abnormality on CT scan found. Specifically patients found to have intra-abdominal malignancy, acute abdominal disease, or ascites were excluded. Anthropometric data recorded included age and gender, height, weight, body mass index (BMI) and circumference at waist and hip, mid-upper arm circumference (MUAC - averaged from left and right) and skin fold thickness (SFT - averaged from left and right at mid arm).
Eligible patients were offered bioimpedance spectroscopy (i.e. multifrequency bioimpedance measurement) using an instrument commissioned from the University of Sheffield Medical Physics department (Clinical Instrumentation and Specialist Patient Services approved, job number 2208) accurate in the low impedance ranges involved in transabdominal measurement (4 to 10 ohms). Bioimpedance was measured at frequencies of 4.8, 9.6, 19.2, 38.4, 76.8, 153.6, 307.2 and 614.4 kHz.
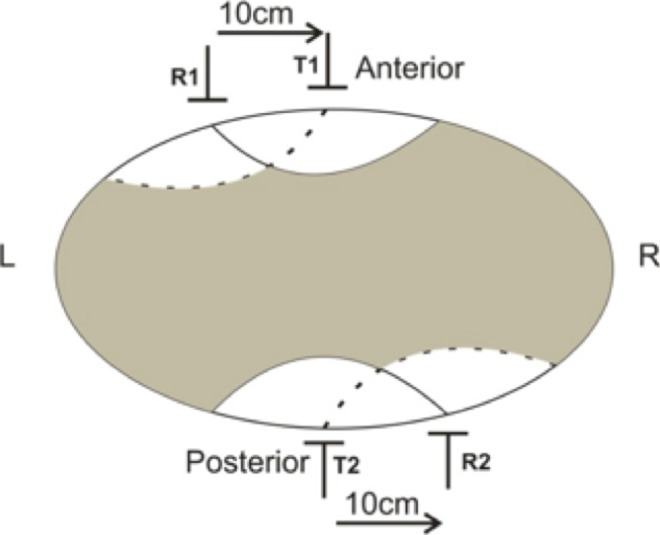
Bioimpedance spectroscopy was performed by attaching adhesive ECG electrodes around the abdomen at the level of the umbilicus. The electrode positions were designed to maximize the sensitivity for the intra-abdominal area — the area of maximum sensitivity is that within the area enclosed by the isopotentials derived from the transmit electrodes which end on the receive electrodes and by reciprocity, vice versa as indicated in Figure 2.
Figure 2.
Area of maximum sensitivity for bioimpedance measurement determined by electrode placement
T = transmit; R = receive electrodes.
The results were then fitted to the Cole-Cole equation using a Levenberg-Marquardt minimization algorithm repeated iteratively by adjusting R, S, frequency and dispersion coefficient α each by 0.2% until the residual mean square of the fit to the equation no longer changed within the precision of 32 bit floating point numbers, or for a maximum of 10 iterations. This software was developed by the author in Visual Basic 3.0 and produces an estimate of R, S, C, as well as the dispersion coefficient α.
The intra-abdominal fat was derived from CT scans using the open source VolView 3.4 software (http://www.kitware.com/products/vvdownload.html), isolating a 3D region of interest (ROI) 10 cm above and below the umbilicus on axial sections, and defined by a manually drawn boundary marking the junction of the abdominal wall musculature and the subcutaneous fat. A preliminary segmentation was carried out into 10 classes using a K-means clustering and Markov random field algorithm taking spatial coherence into account. This enabled counting of the voxels included within the region of interest (by excluding voxels allocated to −2048 = outside the ROI). A connected threshold region growing algorithm was then applied to the region of interest, using an arbitrary upper and lower bound of −30 and −190 Hounsfield units (generally accepted as representing the fat segment on CT scan), with a manually defined seed in an area of fat, and finally the segmentation was repeated to count the voxels meeting these bound criteria, to give a percentage of intra-abdominal fat (see Figure 3).
Figure 3.
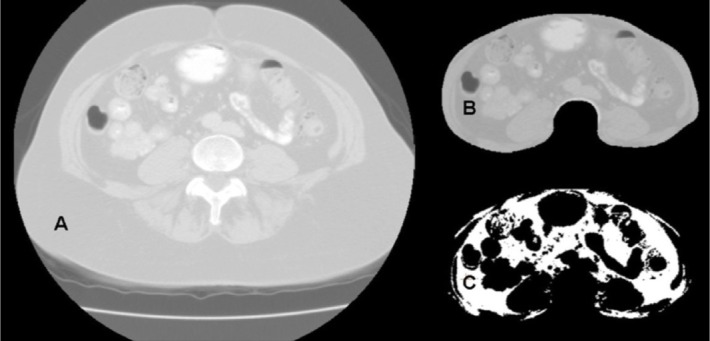
Segmentation process
A = Raw (2D) image; B = Cropped area to exclude subcutaneous fat; C = Segmentation of fat with bounds of −190 to −30 Hounsfield units.
The data obtained were analysed using Statistical Package for Social Sciences (SPSS) verson 3.1, using stepwise regression analysis using the IAF as the dependant variable and considering inclusion of age, gender (assigned 0 = female, 1 = male), mid-upper arm circumference, skin fold thickness, BMI, waist:hip ratio, and bioimpedance parameters R/S, C, frequency and dispersion coefficient α.
Results
Sixteen patients (14 female) were recruited, with a mean age of 62 years (range 37 to 83) and a mean BMI of 26.9 kg/m2 (range 19.4 to 40.1). All underwent routine diagnostic spiral CT scan with 3-mm slices covering the abdomen, with between 23 and 175 slices (median 136) depending on operating protocols and the clinical question posed, median acquisition time 60 seconds. The bioimpedance parameters R and S showed marked variability, particularly in the case of S (Rmean = 15.9, standard deviation [SD] 11.0; Smean = 82.1, SD 108.9) and there was a highly significant correlation between R and S (R = 0.918, P < 0.001), hence the ratio of R/S was used for subsequent analysis. A univariate correlation matrix analysis (Table 1) revealed correlations between IAF and MUAC + R/S ratio at the 0.01 significance level. For the anthropometric measures correlations at the 0.05 significance level were found between IAF and BMI + waist:hip ratio, between MUAC and BMI + waist:hip ratio, and between BMI and waist:hip ratio. For the bioimpedance measures correlations at the 0.05 significance level were also found between C and the dispersion coefficient α + R/S ratio.
Table 1.
Correlation matrix of R
| Age | Sex | MUAC | SFT | BMI | W:H | IAF | frequency | α | R/S | |
| C | −0.36 | 0.38 | 0.04 | 0.05 | −0.36 | −0.08 | −0.09 | 0.1 | †−0.52 | †0.53 |
| R/S | †−0.57 | −0.27 | −0.32 | −0.09 | †−0.50 | †−0.44 | *−0.66 | 0.2 | −0.01 | |
| α | 0.04 | −0.21 | −0.08 | −0.14 | 0.22 | −0.07 | −0.28 | 0.26 | ||
| frequency | 0.28 | −0.26 | −0.01 | 0.36 | −0.13 | −0.04 | −0.1 | |||
| IAF | 0.39 | 0.43 | *0.58 | 0.17 | †0.55 | †0.50 | ||||
| W:H | 0.15 | 0.39 | †0.56 | 0.24 | †0.48 | |||||
| BMI | 0.09 | 0.19 | †0.50 | 0.23 | ||||||
| SFT | 0.06 | −0.21 | 0.4 | |||||||
| MUAC | −0.06 | 0.43 | ||||||||
| Sex | −0.18 |
C = capacitance; MUAC = mid-upper arm circumference; SFT = skin fold thickness; BMI = body mass index; W:H = waist:hip ratio; IAF = intra-abdominal fat content; α = dispersion coefcient; R/S = extracellular/intracellular resistance
N = 16;
P < 0.01;
P < 0.05, one-tailed
Stepwise regression analysis with a dependant variable of IAF, and an inclusion probability criteria of P = 0.1, revealed only two significant independant correlates, MUAC and R/S ratio as shown in Table 2, F2,13 = 9.24, P < 0.01.
Table 2.
Stepwise regression analysis with a dependant variable of intra-abdominal fat (IAF)
| Included: | |||||
| Variable | B | SE B | Beta | t | P-value |
| R/S | −0.757 | 0.27 | −0.52 | −2.78 | 0.02 |
| MUAC | 0.020 | 0.01 | 0.42 | 2.23 | 0.04 |
| (Constant) | 0.036 | 0.29 | 0.12 | 0.90 | |
| Excluded: | |||||
| Age | 0.19 | 0.82 | 0.43 | ||
| Sex | 0.13 | 0.65 | 0.53 | ||
| SFT | −0.06 | −0.29 | 0.78 | ||
| BMI | 0.13 | 0.57 | 0.58 | ||
| W/H | 0.07 | 0.28 | 0.79 | ||
| R | −0.22 | −0.95 | 0.36 | ||
| S | −0.12 | −0.46 | 0.66 | ||
| frequency | 0.01 | 0.06 | 0.95 | ||
| α | −0.25 | −1.49 | 0.16 | ||
| C | 0.25 | 1.19 | 0.26 | ||
B = regression coefficient; SE B = standard error of coefficient estimate; Beta = standardised regression coefficient; R/S = extracellular/intracellular resistance; MUAC = mid-upper arm circumference; SFT = skin fold thickness; BMI = body mass index; W:H = waist:hip ratio; α = dispersion coefficient; C = capacitance
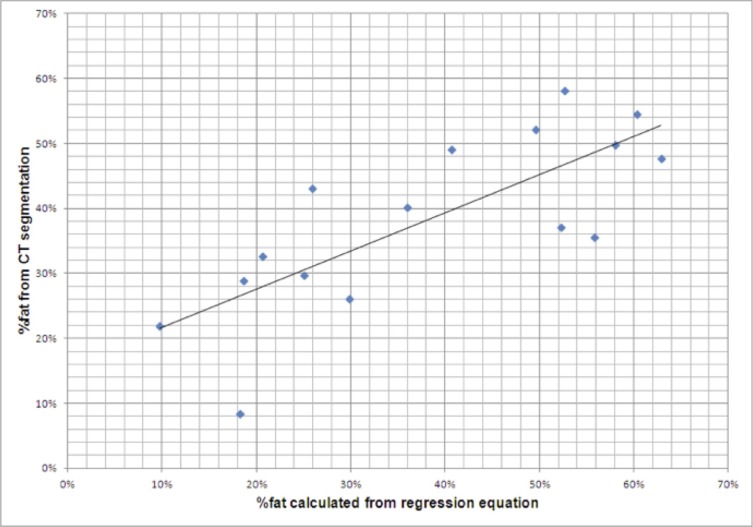
Figure 4 shows the scatterplot against percentage of intra-abdominal fat derived by CT fat segmentation for the resultant regression equation, correlation coefficient R2 = 0.587 (P < 0.01):
Figure 4.
Scatter diagram of % fat calculated from the regression equation against the % fat derived by computed tomography (CT) fat segmentation
Discussion
In this preliminary investigation of using circum-abdominal bioimpedance spectroscopy to measure intra-abdominal fat, a highly significant correlation was found between IAF (as estimated from CT scan segmentation) and the R/S bioimpedance parameter as well as mid arm circumference, and as could be expected a significance correlation between IAF and the conventional parameters of BMI and waist:hip ratio. However because of co-correlations between MUAC and BMI and waist:hip ratio, and between BMI and waist:hip ratio, a multivariate regression analysis showed that only MUAC and R/S ratio were independant covariates with IAF suggesting a simple equation could be used to derive a measure of IAF:
It should be noted that IAF was negatively correlated with the R/S ratio, and that the S parameter of the electrical model of impedance in biological tissues represents the intracellular component, while the R parameter represents the extracellular component, supporting the supposition that the R/S ratio represents the intracellular fat content.
For the purposes of this study, a bespoke device constructed by the Medical Physics department of Sheffield University was utilized in order to accurately measure the significantly lower impedance values obtained from a circum-abdominal acquisition, values in the range of 4 to 10 ohms, as opposed to the usual higher impedance found in whole body (usually wrist to ankle) impedance measured by commercially available instruments such as the Bodystat and Xitron machines, with values in the 500 to 600 ohm range (personal data). There is little reference in the literature of the use of localized bioimpedance measurements, but a new development by the Sheffield group has validated the use of a tetrapolar probe measuring cervical bioimpedance as a possible method of assessing cervical remodeling during labour.7
The α coefficient found in the Cole-Cole equation is a frequency dispersion in the Hz range resulting from differing mechanisms of structural relaxation in the human tissue under study. Other dispersions occurring at higher frequency include the β and γ dispersion, for instance the β dispersion represents the contribution of the cell membrane capacitance, and which may help to derive intra- and extra-cellular fluid compartments.8 However in this study, interest was centered on the intra- and extra-cellular impedance rather than capacitance and the α dispersion was modeled. However the α dispersion was not included in the final regression model at the level of significance employed, although α (and C, capacitance) had the next highest standardized regression coefficient of 0.25 (and −0,25) and may qualify for inclusion with a larger sample size. These results suggest that bioimpedance spectroscopy may prove a useful method of estimating intra-abdominal fat and hence health risks associated with obesity, and further studies are indicated to validate this, in particular paying more attention to the gender and age distribution, since in this preliminary study there was an predominance of female subjects (87.5%). Indeed it is known that in infants at least, using ultrasound of skinfold as a comparator, the bioimpedance regression equations need careful adjustment for age.9
A further aspect of this preliminary study which needs validation is the reproducibility of the measurements, particularly as the results of bioimpedance are known to be influenced by state of hydration and electrolyte shifts, for instance at the time of dialysis, both peritoneal10 and haemodialysis.11 Likewise the presence of ascites or oedema, either generalized or local will undoubtedly affect the interpretation of bioimpedance results.12 However none of the patients studied here had ascites or oedema.
The details of the algorithms used to perform the fat segmentation using a Markov Random Field are beyond the scope of this discussion, but suffice it to say they are widely used in medical segmentation, and take account of spatial interaction between neighboring pixels to counter image inhomogeneity.13 Likewise the selection of −190 to −30 Hounsfield units as representing the fat segment on CT scan is generally accepted14,15 but somewhat arbitrary, but this range is quite distinct from the ranges generally accepted for other body component segments (air < −220, fat −190 to −30, muscle 30 to 199, bone > 200).
In conclusion the measurement of circum-abdominal bioimpedance spectroscopy may prove a useful method of assessing intra-abdominal fat, an important factor in determining the metabolic syndrome and hence risk of cardiovascular death.16 Further studies are needed to validate the reproducibility and validity of this technique. In a low resource setting like Malawi, this bespoke machine operating at low impedance ranges at multiple frequencies is suitable for use in studies to enhance other measures of body fat composition such as mid upper arm circumference. Once available, such a machine has negligible operating costs.
Acknowledgements
The raw data for this study was acquired while the author was at Ashford and St Peter's NHS Trust, Surrey UK, with approval from the Medical Ethics committee of that hospital, and with support and advice from Prof. B.H. Brown of the University of Sheffield Medical Physics department. Dr Amitabh Naik of Ashford and St Peter's NHS Trust assisted in the measurement of bioimpedance.
Competing interests
The author declares that he has no competing interests related to this work.
References
- 1.Flegal KM, Caroll MD, Ogden CL, Curtin LR. Prevalence and Trends in Obesity Among US Adults, 1999–2008 (NHANES) JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 2.Calabro P, Yeh ETH. Intra-abdominal adiposity, inflammation, and cardiovascular risk: New insight into global cardiometabolic risk. Current Hypertension Reports. 2008;10:32–38. doi: 10.1007/s11906-008-0008-z. [DOI] [PubMed] [Google Scholar]
- 3.Brown B H, Seagar AD. The Sheffield data collection system. Clin Phys Physiol Meas. 1987;8:A91–A98. doi: 10.1088/0143-0815/8/4a/012. [DOI] [PubMed] [Google Scholar]
- 4.Rosell-Ferrer J, Garcia MA, Ramos J, et al. Heart Graft Rejection Assessed by Multi-Frequency Electrical Impedance: Human Results. IFMBE Proceedings. 2007;17:138–141. [Google Scholar]
- 5.Kotanko P, Levin NW, Zhu F. Current state of bioimpedance technologies in dialysis. Nephrol Dial Transplant. 2008;23:808–812. doi: 10.1093/ndt/gfm889. [DOI] [PubMed] [Google Scholar]
- 6.Cole KS, Cole RH. Dispersion and Absorption in Dielectrics I. Alternating Current Characteristics. J Chem Phys. 1941;9:341–351. [Google Scholar]
- 7.Jokhi RP, Ghule VV, Brown BH, Anumba DOC. Reproducibility and repeatability of measuring the electrical impedance of the pregnant human cervix-the effect of probe size and applied pressure. BioMedical Engineering OnLine. 2009;8:10. doi: 10.1186/1475-925X-8-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Van Loan MD, Withers P, Matthie J, Mayclin PL. Use of Bioimpedance Spectroscopy to Determine Extracellular Fluid, Intracellular Fluid, Total Body Water, and Fat-Free Mass Human Body Composition, Volume 60 of the series Basic Life Sciences. pp. 67–70. http://dx.doi.org/10.1007/978-1-4899-1268-8_13. [DOI] [PubMed] [Google Scholar]
- 9.Gridneva Z, Hepworth AR, Ward LC, Lai CT, Hartmann PE, Geddes DT. Determinants of body composition in breastfed infants using bioimpedance spectroscopy and ultrasound skinfolds - methods comparison. Pediatr Res. 2016 Nov 9; doi: 10.1038/pr.2016.235. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 10.Kotanko P, Levin NW, Zhu F. Current state of bioimpedance technologies in dialysis. Nephrol Dial Transplant. 2008;23:808–812. doi: 10.1093/ndt/gfm889. [DOI] [PubMed] [Google Scholar]
- 11.Lim PS, Chen CH, Zhu F, et al. Validating Body Fat Assessment by Bioelectric Impedance Spectroscopy in Taiwanese Hemodialysis Patients. J Ren Nutr. 2016 Sep 22; doi: 10.1053/j.jrn.2016.08.003. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 12.Seward C, Skolny M, Brunelle C, Asdourian M, Salama L, Taghian AG. A comprehensive review of bioimpedance spectroscopy as a diagnostic tool for the detection and measurement of breast cancer-related lymphedema. J Surg Oncol. 2016 Oct;114(5):537–542. doi: 10.1002/jso.24365. [DOI] [PubMed] [Google Scholar]
- 13.Azmi R, Norozi N. A New Markov Random Field Segmentation Method for Breast Lesion Segmentation in MR images. J Med Signals Sens. 2011 Jul-Sep;1(3):156–164. [PMC free article] [PubMed] [Google Scholar]
- 14.Kvist H, et al. Total and visceral adipose-tissue volumes derived from measurements with computed tomography in adult men and women: predictive equations. Am J Clin Nutr. 1988;48:1351. doi: 10.1093/ajcn/48.6.1351. [DOI] [PubMed] [Google Scholar]
- 15.Kim YJ, Lee SH, Kim TY, Park JY, Choi SH, Kim KG. Body Fat Assessment Method Using CT Images with Separation Mask Algorithm. J Digit Imaging. 2013 Apr;26(2):155–162. doi: 10.1007/s10278-012-9488-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Després JP, Lemieux I, Bergeron J, et al. Abdominal obesity and the metabolic syndrome: contribution to global cardiometabolic risk. Arterioscler Thromb Vasc Biol. 2008 Jun;28(6):1039–1049. doi: 10.1161/ATVBAHA.107.159228. [DOI] [PubMed] [Google Scholar]