Abstract
For decades, anastomoses between unpaired branches of the abdominal aorta have attracted the attention of anatomists, surgeons and radiologists, due to their significance in many clinical procedures. This report presents a rare anastomosis between the common hepatic artery and the superior mesenteric artery, which gave off three branches to the jejunum. The diameter of the anastomosis measured at the point of its branching off the common hepatic artery and at the level of union with the superior mesenteric artery was 4.46 and 4.19 mm, respectively. Moreover, the anastomosis gave off the branch to the head of the pancreas. Both embryological background and potential clinical implications of this variation are discussed. Knowledge of these vascular connections may be important for diagnostic and surgical procedures.
Keywords: Anastomosis, Common hepatic artery, Superior mesenteric artery
Introduction
For decades, anastomoses between unpaired branches of the abdominal aorta have attracted the attention of anatomists, surgeons and radiologists, due to their prominent significance in many clinical procedures such as surgery of aneurysms or radiological transarterial chemoembolization procedures for tumors [1–4]. The common hepatic artery (CHA) is a short blood vessel that supplies the liver, the pylorus, the pancreas and the duodenum [5]. It arises from the coeliac trunk and divides into the gastroduodenal artery (GDA) and the proper hepatic artery (PHA) [1, 6]. The superior mesenteric artery (SMA) arises from the anterior surface of the abdominal aorta, 1–2 cm lower than the celiac trunk, and gives off five sets of branches: the inferior pancreaticoduodenal artery, the intestinal arteries, the ileocolic artery, the right colic artery and the middle colic artery [5]. The SMA supplies the lower part of the duodenum, the jejunum, the ileum, the cecum, the appendix, the ascending colon and two third of the transverse colon, as well as the pancreas [5].
Several anatomic variations of the celiac trunk, superior mesenteric artery, the right and left hepatic arteries, and the accessory hepatic artery have been described [2, 7–15]. However, few reports exist concerning the variants of the common hepatic artery [16]. This case report describes a rare anastomosis between the common hepatic artery and the superior mesenteric artery. It highlights the importance of knowledge of the arterial supply in the abdominal cavity.
Case report
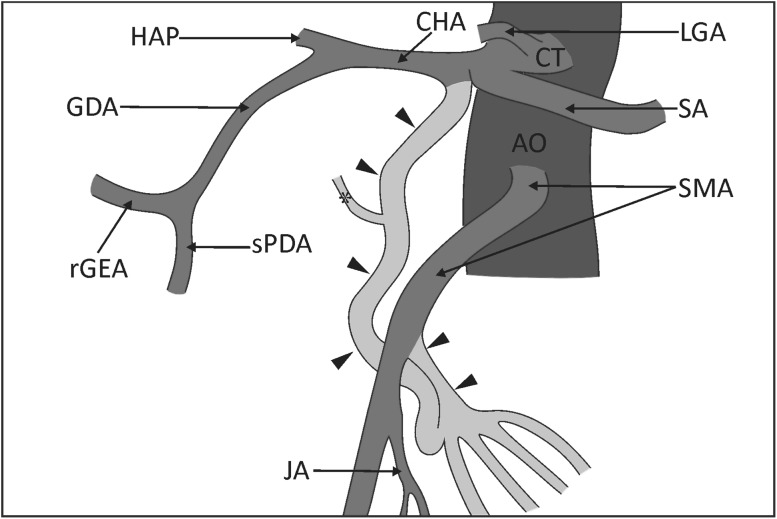
The cadaver of a 58-year-old woman was subjected to routine anatomical dissection for research and teaching purposes at the Department of Normal and Clinical Anatomy of the Medical University of Lodz. The dissection was performed in the abdominal cavity. After a careful resection of the interrupting tissues, a rare anastomosis between the common hepatic artery and the superior mesenteric artery was observed (Figs. 1, 2, 3).
Fig. 1.
Anastomosis between the common hepatic artery and the superior mesenteric artery (white arrowheads present the anastomosis). L liver, S stomach, P pancreas, CT coeliac trunk, SMA superior mesenteric artery, LGA left gastric artery, CHA common hepatic artery, SA splenic artery, HAP hepatic proper artery, GDA gastroduodenal artery, rGEA right gastroomental artery, sPDA superior pancreaticoduodenal artery, JA jejunal artery, bJA branches to the jejunum. Asterisk branch to the head of the pancreas
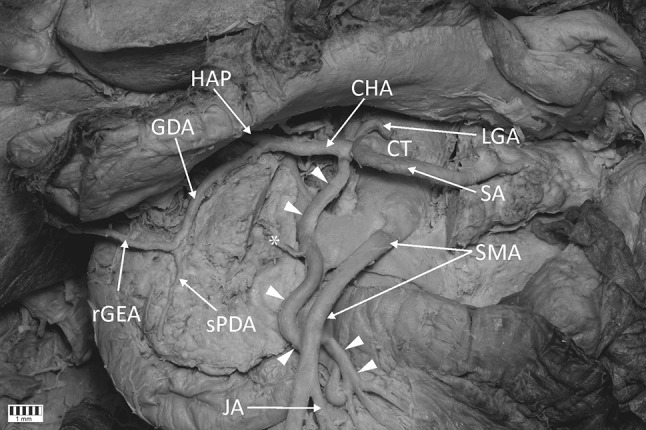
Fig. 2.
Anastomosis. View of the branches for the jejunum and the connection with the superior mesenteric artery. White arrowheads present the anastomosis between the common hepatic artery and the superior mesenteric artery. Asterisk branch for the head of the pancreas. P pancreas, SMA superior mesenteric artery, iPDA inferior pancreaticoduodenal artery, JA jejunal artery, bJA branches for the jejunum
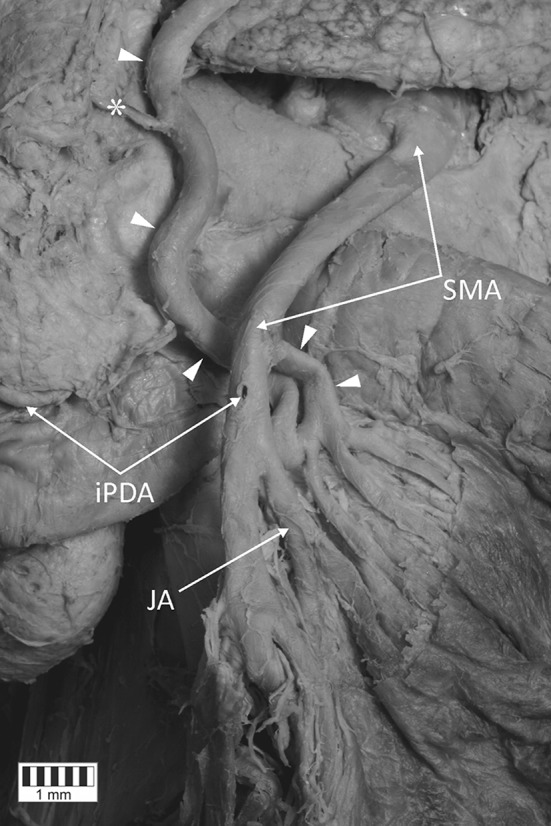
Fig. 3.
Schematic drawing of the structures of the anastomosis between the superior mesenteric artery and the common hepatic artery. Black arrowheads indicate the anastomosis. CT coeliac trunk, LGA left gastric artery, CHA common hepatic artery, SA splenic artery, HAP hepatic proper artery, GDA gastroduodenal artery, rGEA right gastroomental artery, sPDA superior gastroduodenal artery, AO abdominal aorta, SMA superior mesenteric artery, JA jejunal artery. Asterisk branch to the head of the pancreas
The measurements of the arteries were taken from digital photographic documentation processed through MultiScanBase 18.03 software (Computer Scanning System II, Warsaw, Poland). The value and precision of this method have been confirmed in a previous study [10]. A detailed analysis found that the anastomosing vessel followed a spiral route. A loop connection with the superior mesenteric artery was observed in the distal part of this artery, and the branches of the jejunum (diameters: 3.11/2.25/1.81 mm) rooted from the convex part of this connection (Fig. 2). The main arterial trunk of the jejunum branched off below the anastomosis site with a diameter of 3.36 mm (Fig. 2). Furthermore, it was observed that the branch ran from the said artery towards the head of the pancreas (Figs. 1, 2). The main trunk of the anastomosis was 4.46 mm in diameter at the common hepatic artery and 4.19 mm at the superior mesenteric artery. The external diameter of the cross point of the common hepatic artery and the superior mesenteric artery was 4.55 mm.
Discussion
Since the coeliac vascularization is complex, its anatomical variations should be known by hepatic surgeon during transplant procedure. There are several classifications regarding the origin and topography of abdominal arteries [7, 13, 17–21]. The most common are various types of the celiac trunk branches [6–9, 14, 17, 22], atypical liver vascularization [3, 17, 20] and differences in the territory of the mesenteric arteries [8, 14, 17, 23]. The typical ‘natural’ anastomosis between the superior pancreaticoduodenal artery and the inferior pancreaticoduodenal artery forms an arterial communication named the anterior and posterior pancreaticoduodenal arcade [15, 22, 24].
The variants of the celiac trunk and the superior mesenteric artery are thought to have an embryological basis. Developmentally, the superior mesenteric artery is considered to be a part of the celiac complex, and therefore, variants of the SMA are connected to a large extent on the CT [25]. Tandler [25] suggests that a ‘longitudinal anastomosis’ unites the roots of the ventral segmental arteries. Several anatomical variants of the unpaired arteries of the abdominal aorta develop, depending on the extent of resorption or retention of different parts of the longitudinal anastomosis and ventral segmental roots. Accordingly, the 10th primitive root of the ventral segmental artery becomes the left gastric artery; the 11th becomes the splenic artery; the 12th becomes the common hepatic artery; the 13th becomes the superior mesenteric artery, and the 19th primitive root becomes the inferior mesenteric artery with separate origins from the abdominal aorta [9, 18, 25]. While the celiac trunk is formed by the fusion of first three roots and becomes separated from the fourth root, the superior mesenteric artery develops from the fourth root, which later migrates caudally with the ventral migration of the gut [13]. It is likely that incomplete fusion or malfusion of these arteries during the developmental stage may be responsible for the anastomosis observed in this study.
Lipschutz [21] first classified the celiac trunk in 1917, describing its four variants. In 1928, Adachi [17] also proposed a detailed classification of this region, defining the left gastric artery, splenic artery, common hepatic artery and superior mesenteric artery as the principal branches in this region. He also noted the existence of accessory hepatic arteries, classifying them into six types with 28 forms. Song et al. [26] classified 13 types of the celiac trunk in their studies. Some variants of the coeliac trunk were also described as case reports. Hirai et al. [8] described a case where two trunks replaced the celiac trunk: the hepato-spleno-mesenteric trunk and the gastro-phrenic trunk. Yan et al. [14] reported the celiac and superior mesenteric arteries arising with a common short trunk from the abdominal aorta. Iacob et al. [9] described an absence of the celiac trunk, with the left gastric and the common hepatic arteries originating directly from the anterior wall of the abdominal aorta. Çiçekcibaşi et al. [7] described a rare variation of the celiac trunk which gave rise to six arteries: the left gastric, common hepatic, splenic, left gastroepiploic, and the right and left inferior phrenic arteries.
Tandler [25] and Buhler [27] as first observed and described anastomosis between the celiac axis and the superior mesenteric artery. Buhler was a first, who described the retropancreatic anastomosis between the celiac trunk and middle colon artery [27]. Connection between the branches of the CT and the SMA include the pancreaticoduodenal arcades described by do Rio-Branco on the right side [28] and the Buhler arcade on the left side [27]. This “normal” SMA morphology may be present in as many as 68% of cases [29].
Despite having a normal or variable origin, the common hepatic artery may follow an unusual course. Yan et al. [14] found the artery to have a 13% probability of originating from the superior mesenteric artery. Okada et al. [30] observed the possibility of the common hepatic artery originating from the left gastric artery. Wang et al. [16] described the common hepatic artery originating from the celiac trunk, crossing the portal vein and positioning itself at the back of this structure. From the clinical point of view it is important to establish whether the numerous variants of the vascularization of the abdomen described above play a role in the formation of collateral circulation.
Negovanovic [31] describes the presence of an anastomosis between the common hepatic artery and the superior mesenteric artery in an adult female cadaver. This fusion directly connected the CHA and the SMA [31]. However, our case is quite different, insofar that the ‘connection trunk’ gave one branch to the pancreas and three branches to the jejunum. According to Rosenblum et al. [32], the sources of collateral circulation between the mesenteric and non-mesenteric arteries are numerous and clinically important. Such collateral of the circulatory system can be seen between the celiac trunk and the superior mesenteric artery, and between the superior mesenteric artery and inferior mesenteric artery [32]. The most common potential collateral flow paths between the CT and the SMA comprise the gastroduodenal artery and pancreaticoduodenal arteries [32]. An anastomosis known as the arc of Barkow may be present between the epiploic arteries of the splenic artery and the superior mesenteric artery [33–35]. A rare connection is the arc of Buhler [34, 36]. The presence of the arc of Buhler is on the level of 3.3% [34, 36, 37].
The connection described in this case is clinically important because three jejunal arteries arise from its distal part. Between these three arteries and the first jejunal artery arise several coexisting connections from the superior mesenteric artery. These connections may prevent the occurrence of mesenteric acute ischemia; in case of SMA occlusion. The arterial supply of the jejunum will be provided by this anastomosis, irrespective of the degree of SMA occlusion. As acute mesenteric ischemia accounts for 60–80% of all cases of mesenteric ischemia, and has a mortality rate between 59 and 93% [38–40], knowledge of such anatomical variation is important.
Conclusion
In conclusion, although the anastomosis between the common hepatic artery and the superior mesenteric artery presented in the case is very rare, it might be a highly significant factor in the arterial supply to this region. Preoperative knowledge of such rare anatomic variants is essential in planning some surgical procedures and liver transplantation.
Acknowledgements
The authors wish to express their gratitude to all those who donated their bodies to medical science.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Abdullah SS, Mabrut JY, Garbit V, De La Roche E, Rode A, Morin A, Berthezene Y, Baulieux J, Ducerf C. Anatomical variations of the hepatic artery: study of 932 cases in liver transplantation. Surg Radiol Anat. 2006;28:468–473. doi: 10.1007/s00276-006-0121-0. [DOI] [PubMed] [Google Scholar]
- 2.Paraskevas GK, Raikos A. Multiple aberrant coeliac trunk ramifications. Singap Med J. 2011;52:e147–e149. [PubMed] [Google Scholar]
- 3.Polguj M, Gabryniak T, Topol M. The right accessory hepatic artery; a case report and review of the literature. Surg Radiol Anat. 2010;32:175–179. doi: 10.1007/s00276-009-0536-5. [DOI] [PubMed] [Google Scholar]
- 4.Polguj M, Podgórski M, Hogendorf P, Topol M. Variations of the hepatobiliary vasculature including coexistence of accessory right hepatic artery with unusually arising double cystic arteries: case report and literature review. Anat Sci Int. 2014;89:195–198. doi: 10.1007/s12565-013-0219-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bergman RA, Afifi AK, Miyauchi R (2015) Illustrated encyclopedia of human anatomic variation. http://www.anatomyatlases.org/AnatomicVariants/AnatomyHP.shtml. Accessed 6 Feb 2017
- 6.Araujo Neto SA, Franca HA, de Mello Júnior CF, Silva Neto EJ, Negromonte GR, Duarte CM, Cavalcanti Neto BF, Farias RD. Anatomical variations of the celiac trunk and hepatic arterial system: an analysis using multidetector computed tomography angiography. Radiol Bras. 2015;48:358–362. doi: 10.1590/0100-3984.2014.0100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Çiçekcibaşi AE, Uysal II, Şeker M, Tuncer I, Büyükmumcu M, Salbacak A. A rare variation of the coeliac trunk. Ann Anat. 2005;187:387–391. doi: 10.1016/j.aanat.2005.02.011. [DOI] [PubMed] [Google Scholar]
- 8.Hirai Y, Yamaki K, Saga T, Hirata T, Yoshida M, Soejima H, Kanazawa T, Araki Y, Yoshizuka M. An anomalous case of the hepato-spleno-mesenteric and the gastro-phrenic trunks independently arising from the abdominal aorta. Kurume Med J. 2000;47:189–192. doi: 10.2739/kurumemedj.47.189. [DOI] [PubMed] [Google Scholar]
- 9.Iacob N, Sas I, Joseph SC, Pleş H, Miclăuş GD, Matusz P, Tubbs RS, Loukas M. Anomalous pattern of origin of the left gastric, splenic, and common hepatic arteries arising independently from the abdominal aorta. Rom J Morphol Embryo. 2014;55:1449–1453. [PubMed] [Google Scholar]
- 10.Polguj M, Jȩdrzejewski KS, Topol M. Angioarchitecture of the bovine spermatic cord. J Morphol. 2011;272:497–502. doi: 10.1002/jmor.10929. [DOI] [PubMed] [Google Scholar]
- 11.Prakash Rajini T, Mokhasi V, Geethanjali BS, Sivacharan PV, Shashirekha M. Coeliac trunk and its branches: anatomical variations and clinical implications. Singap Med J. 2012;53:329–331. [PubMed] [Google Scholar]
- 12.Sebben GA, Rocha SL, Sebben MA, Parussolo Filho PR, Gonçalves BH. Variations of hepatic artery: anatomical study on cadavers. Rev Col Bras Cir. 2013;40:221–226. doi: 10.1590/S0100-69912013000300010. [DOI] [PubMed] [Google Scholar]
- 13.Selvaraj L, Sundaramurthi I. Study of normal branching pattern of the coeliac trunk and its variations using CT angiography. J Clin Diagn Res. 2015;9:AC01–AC04. doi: 10.7860/JCDR/2015/12593.6523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yan J, Nagasawa Y, Nakano M, Hitomi J. Origin of the celiac and superior mesenteric arteries in a common trunk: description of a rare vessel variation of the celiacomesenteric trunk with a literature review. Okajimas Folia Anat Jpn. 2014;91:45–48. doi: 10.2535/ofaj.91.45. [DOI] [PubMed] [Google Scholar]
- 15.Zarzavadjian Le Bian A, Costi R, Blangy S, Sbai-Idrissi MS, Smadja C. Pancreaticoduodenectomy in the presence of a common hepatic artery originating from the superior mesenteric artery. Technical implications. Int J Surg. 2015;17:1–4. doi: 10.1016/j.ijsu.2015.03.010. [DOI] [PubMed] [Google Scholar]
- 16.Wang MJ, Cheng Z, Wang R, Li Y, Zhou ZG. Unusual course of the common hepatic artery originating from the celiac trunk. Surg Radiol Anat. 2010;32:883–885. doi: 10.1007/s00276-010-0632-6. [DOI] [PubMed] [Google Scholar]
- 17.Adachi B. Das Arteriensystem der Japaner. Kyoto: Verlag der Kaiserlich-Japanichen Universitat zu Kyoto; 1928. [Google Scholar]
- 18.Babu ED, Khrab P. Coeliac trunk variations: review with proposed new classification. Int J Anat Res. 2013;1:165–170. [Google Scholar]
- 19.Bastos-Neves D, da Silva Alves JA, Guedes Dias LG, de Rezende MB, Salvalaggio PR. Right accessory hepatic artery arising from celiac trunk-case report of a variation that must be looked for during multiorgan procurement. Transplant Proc. 2016;48:2387–2388. doi: 10.1016/j.transproceed.2016.06.025. [DOI] [PubMed] [Google Scholar]
- 20.Hiatt JR, Gabbay J, Busuttil RW. Surgical anatomy of the hepatic arteries in 1000 cases. Ann Surg. 1994;220:50–52. doi: 10.1097/00000658-199407000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lipshutz B. A composite study of the coeliac axis artery. Ann Surg. 1917;65:159–169. doi: 10.1097/00000658-191702000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pintilie DG, Zamfir CL, Păduraru D, Răileanu RC. Characteristics of anastomoses between the celiac trunk. Rev Med Chir Soc Med Nat Iasi. 2003;107:826–830. [PubMed] [Google Scholar]
- 23.Matsui Y, Mimura H, Fukazawa T, Morita I, Suehiro M, Kawamoto H, Naomoto Y. A case of acute superior mesenteric artery embolism with severe ischemic liver injury successfully treated by endovascular treatment. Acta Med Okayama. 2013;67:397–402. doi: 10.18926/AMO/52014. [DOI] [PubMed] [Google Scholar]
- 24.Kimura W, Nagai H. Study of surgical anatomy for duodenum-preserving resection of the head of the pancreas. Ann Surg. 1995;221:359–363. doi: 10.1097/00000658-199504000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tandler J. Über die Varietäten der Arteria coeliaca und deren Entwickelung. Anat Hefte. 1904;25:473–500. doi: 10.1007/BF02300762. [DOI] [Google Scholar]
- 26.Song SY, Chung JW, Yin YH, Jae HJ, Kim HC, Jeon UB, Cho BH, So YH, Park JH. Celiac axis and common hepatic artery variations in 5002 patients: systematic analysis with spiral CT and DSA. Radiology. 2010;255:278–288. doi: 10.1148/radiol.09090389. [DOI] [PubMed] [Google Scholar]
- 27.Buhler A. Über eine Anastomose zwischen den Stämmen der Art. Celiaca und Art. mesenterica superior. Morpholog Jahrb. 1904;32:185–188. [Google Scholar]
- 28.do Rio-Branco P. Essai sur l’anatomie et la médecine opératoire du tronc coeliaque et de ses branches de l’artère hépatique en particulier. Paris: University of Paris; 1912. [Google Scholar]
- 29.Valentine RJ, Martin JD, Myers SI, Rossi MB, Clagett GP. Asymptomatic celiac and superior mesenteric artery stenoses are more prevalent among patients with unsuspected renal artery stenoses. J Vasc Surg. 1991;14:195–199. doi: 10.1067/mva.1991.29423. [DOI] [PubMed] [Google Scholar]
- 30.Okada Y, Nishi N, Matsuo Y, Watadani T, Kimura F. The common hepatic artery arising from the left gastric artery. Surg Radiol Anat. 2010;32:703–705. doi: 10.1007/s00276-010-0662-0. [DOI] [PubMed] [Google Scholar]
- 31.Negovanovic B. On the anastomosis between the common hepatic artery and the superior mesenteric artery. Srp Arh Celok Lek. 1959;87:655–658. [PubMed] [Google Scholar]
- 32.Rosenblum JD, Boyle CM, Schwartz LB. The mesenteric circulation. Anatomy and physiology. Surg Clin N Am. 1997;77:289–306. doi: 10.1016/S0039-6109(05)70549-1. [DOI] [PubMed] [Google Scholar]
- 33.McNulty JG, Hickey N, Khosa F, O’Brien P, O’Callaghan JP. Surgical and radiological significance of variants of Bühler’s anastomotic artery: a report of three cases. Surg Radiol Anat. 2001;23:277–280. doi: 10.1007/s00276-001-0277-6. [DOI] [PubMed] [Google Scholar]
- 34.Saad WE, Davies MG, Sahler L, Lee D, Patel N, Kitanosono T, Sasson T, Waldman D. Arc of Buhler: incidence and diameter in asymptomatic individuals. Vasc Endovasc Surg. 2005;39:347–349. doi: 10.1177/153857440503900407. [DOI] [PubMed] [Google Scholar]
- 35.Walker TG. Mesenteric vasculature and collateral pathways. Semin Intervent Radiol. 2009;26:167–174. doi: 10.1055/s-0029-1225663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.O’Brien K, Ferral H. Lessons learned from a case of multivessel median arcuate ligament syndrome in the setting of an Arc of Buhler. Radiol Case Rep. 2016;11:182–185. doi: 10.1016/j.radcr.2016.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schneider TA, Longo WE, Ure T, Vernava AM. Mesenteric ischemia. Acute arterial syndromes. Dis Colon Rectum. 1994;37:1163–1174. doi: 10.1007/BF02049824. [DOI] [PubMed] [Google Scholar]
- 38.Adaba F, Rajendran A, Patel A, Cheung YK, Grant K, Vaizey CJ, Gabe SM, Warusavitarne J, Nightingale JM. Mesenteric infarction: clinical outcomes after restoration of bowel continuity. Ann Surg. 2015;262:1059–1064. doi: 10.1097/SLA.0000000000001100. [DOI] [PubMed] [Google Scholar]
- 39.Oldenburg WA, Lau LL, Rodenberg TJ, Edmonds HJ, Burger CD. Acute mesenteric ischemia: a clinical review. Arch Intern Med. 2004;164:1054–1062. doi: 10.1001/archinte.164.10.1054. [DOI] [PubMed] [Google Scholar]
- 40.Van De Winkel N, Cheragwandi A, Nieboer K, van Tussenbroek F, De Vogelaere K, Delvaux G. Superior mesenteric arterial branch occlusion causing partial jejunal ischemia: a case report. J Med Case Rep. 2012;6:48. doi: 10.1186/1752-1947-6-48. [DOI] [PMC free article] [PubMed] [Google Scholar]