Abstract
Introduction and Aims
Patterns of polydrug use among people who inject drugs (PWID) may be differentially associated with overdose and unique HIV risk factors. Subgroups of PWID in Tijuana, Mexico, were identified based on substances used, route of administration, frequency of use, and co-injection indicators.
Design and Methods
Participants were PWID residing in Tijuana age ≥ 18 sampled from 2011–2012 who reported injecting an illicit substance in the past month (N=735). Latent class analysis identified discrete classes of polydrug use characterised by 11 indicators of past 6 month substance use. Multinomial logistic regression examined class membership association with HIV risk behaviours, overdose and other covariates using an automated 3 step procedure in Mplus to account for classification error.
Results
Participants were classified into five subgroups. Two polydrug and polyroute classes were defined by use of multiple substances through several routes of administration and were primarily distinguished from each other by cocaine use (Class 1: 5%) or no cocaine use (Class 2: 29%). The other classes consisted primarily of injectors: cocaine, methamphetamine and heroin injection (Class 3: 4%); methamphetamine and heroin injection (Class 4: 10%); and heroin injection (Class 5: 52%). Compared to the heroin only injection class, memberships in the two polydrug and polyroute use classes were independently associated with both HIV injection and sexual risk behaviours.
Discussion and Conclusions
Substance use patterns among PWID in Tijuana are highly heterogeneous and polydrug and polyroute users are a high-risk subgroup who may require more tailored prevention and treatment interventions.
Keywords: polydrug, polyroute, latent class analysis, PWID, HIV risk behaviour
INTRODUCTION
Injection of illicit substances is a significant global public health problem associated with multiple negative health outcomes, including transmission of HIV, hepatitis B and C, as well as higher risk for overdose related morbidity and mortality [1]. Although most people who inject drugs (PWID) primarily inject heroin [2], PWID in the US-Mexico border region also inject methamphetamine and cocaine [3] and report use of these and other substances through smoking, snorting or ingestion routes of administration. There is growing recognition that substance use behaviours often involve use of multiple drugs and that descriptions of these patterns of use and their relationship to drug related harms warrant further study [2,4,5].
Assessments of variation in polydrug and polyroute use among PWID may shed further light on how substance use patterns are related to HIV transmission and overdose risk. While heroin users are at high risk for overdose because of the drug’s depressant effect on breathing [6, 7], mixing of opiates like heroin with stimulants like cocaine or methamphetamine can contribute to high risk for overdose through increased toxicity, decreased cognitive function, and cardiac stress [8]. The combined use of opioids and stimulants may also lead to higher consumption of each drug class. Although HIV risk among PWID is typically focused on the sharing of needles and syringes, stimulant and alcohol use lower inhibitions [9,10], which may increase HIV risk through unsafe sexual behaviours. However, less is known about how observed patterns with multiple overlapping risks are related to these negative health outcomes.
Latent class analysis (LCA) has been increasingly applied in recent years to examine patterns of substance use among both general and high risk populations [11], particularly among adolescents [12]. Several of these LCA studies have examined how distinct polydrug use classes are associated with HIV risk and overdose, finding that use of more substances was associated with greater risk for negative health outcomes [13–19]. However, most of these studies were conducted in high income countries and among adolescents, and therefore may not be generalisable to adults in lower and middle income countries such as Mexico.
Limited resources for health services, and high levels of social and economic inequality have contributed to a localised HIV epidemic in Tijuana, Baja California, Mexico [20,21]. Tijuana is also physically situated on a major drug trafficking route, which contributes to elevated rates of illicit drug use, especially among socially marginalised migrant, deportee and unstably housed populations.
Previous work investigating polydrug use and HIV and overdose risk among PWID in the US-Mexico border setting found that PWID differ with respect to which substances they inject or smoke and that these differences were associated with demographics, health status and HIV risk behaviours [22,23]. Applying latent class analysis, we previously identified three classes of polydrug use (primarily heroin injection, heroin + methamphetamine use, heroin + methamphetamine + cocaine use) among an earlier cohort of heroin injectors sampled from 2006–2007 in Tijuana [3]. This prior analysis did not assess use of tranquilizers or marijuana, co-injection of heroin with other substances, or frequency of use. Since the earlier study was conducted, Mexico enacted federal drug policy reforms that decriminalised possession of small amounts of drugs [24], which may affect the drugs used by this population. The present analysis expands on this earlier work by examining a more contemporary cohort (assessed 2011–2012) of PWID in Tijuana and a broader range of substance use indicators.
The objectives of the present analysis are to: (i) identify discrete classes of polydrug use in a cohort of PWID using 4 dimensions of indicators (substance, route of administration, co-injection and frequency); and (ii) determine the association of class membership with HIV risk behaviours and recent overdose, above background or pre-disposing individual-level demographic and risk environment covariates. It was hypothesised that classes characterised by more substances would be more likely to experience overdose than classes characterised by use of fewer substances; that classes with more stimulant use would be more likely to engage in HIV sexual risk behaviours than classes without stimulant use; and that classes with more frequent injection use would be more likely to engage in HIV injection risk behaviours than classes with less frequent injection use.
METHODS
Study Participants and Procedures
The present study sample consisted of 735 participants from the baseline assessment of Proyecto El Cuete Phase IV, a prospective cohort study of people who inject drugs in Tijuana [24]. Participants were recruited through convenience sampling using targeted street outreach from 2011––2012. Eligibility criteria included: (i) injecting illicit drugs within the past month, confirmed by track marks; (ii) age 18 or older; (iii) speaking Spanish or English; and (iv) current residence in Tijuana with no plans to move for 3 years. Trained interviewers administered quantitative surveys in English or Spanish using computer-assisted personal interview technology in a private room. All participants provided written informed consent and were reimbursed $20 USD for completing the baseline assessment. The University of California San Diego Human Research Protection Program and the Institutional Review Board for the Colegio de la Frontera Norte approved the study protocol.
Measures
Drug use indicators
Illicit drug use was assessed by asking participants about their frequency of use in the past 6 months for multiple drugs and routes of administration (dichotomised into no use vs. past 6 month use). Drugs included marijuana, heroin (both black tar and “china white”), methamphetamine, cocaine, OxyContin and other non-prescription opioids, hallucinogens, ketamine, ecstasy/MDMA, PCP, inhalants, tranquilizers and barbiturates. Co-injection of heroin, methamphetamine and cocaine was also assessed.
Drugs used by at least 5% of the sample were selected as drug use indicators. Due to a low prevalence of smoking or snorting routes of heroin and cocaine use, these non-injection routes of administration were combined into single indicators (i.e. heroin snorting/smoking and cocaine snorting/smoking). Three indicators (methamphetamine smoking, methamphetamine injection, and methamphetamine and heroin co-injection) had over 10% of the sample reporting daily use and were converted into an ordinal variable of daily use, less than daily use or no use in the past 6 months. (Table 2)
Table 2.
Substance use indicator prevalence and conditional response probabilities of 11 substance use indicators given class membership for 5 latent class model (N = 735 PWID in Tijuana)
| Classes | Overall | Class 1: Polydrug and polyroute + cocaine |
Class 2: Polydrug and polyroute |
Class 3: Stimulant and heroin injecting |
Class 4: Meth and heroin injecting |
Class 5: Heroin injecting |
|---|---|---|---|---|---|---|
| Probability of class membership | 0.05 | 0.29 | 0.04 | 0.10 | 0.52 | |
| Indicators | Prevalence | Conditional Response Probabilities | ||||
| 1. Heroin injecting | 0.95 | 1.00 | 0.90 | 1.00 | 1.00 | 0.96 |
| 2. Heroin and meth co-injecting, daily | 0.39 | 0.43 | 0.31 | 0.89 | 1.00 | 0.26 |
| 2. Heroin and meth co-injecting, < daily | 0.17 | 0.47 | 0.33 | 0.00 | 0.00 | 0.11 |
| 3. Methamphetamine smoking, daily | 0.13 | 0.28 | 0.17 | 0.04 | 0.27 | 0.07 |
| 3. Methamphetamine smoking, < daily | 0.28 | 0.72 | 0.57 | 0.00 | 0.12 | 0.14 |
| 4. Marijuana smoking | 0.31 | 0.81 | 0.65 | 0.17 | 0.15 | 0.13 |
| 5. Tranquilizer ingesting | 0.20 | 0.49 | 0.44 | 0.23 | 0.09 | 0.05 |
| 6. Methamphetamine injecting, daily | 0.16 | 0.35 | 0.09 | 0.47 | 0.92 | 0.01 |
| 6. Methamphetamine injecting, < daily | 0.12 | 0.39 | 0.26 | 0.15 | 0.08 | 0.03 |
| 7. Heroin and cocaine co-injecting | 0.14 | 1.00 | 0.14 | 0.87 | 0.00 | 0.03 |
| 8. Heroin smoking or snorting | 0.12 | 0.36 | 0.29 | 0.00 | 0.09 | 0.03 |
| 9. Methamphetamine snorting | 0.11 | 0.63 | 0.25 | 0.00 | 0.08 | 0.00 |
| 10. Cocaine smoking or snorting | 0.10 | 0.80 | 0.14 | 0.07 | 0.04 | 0.02 |
| 11. Cocaine injecting | 0.08 | 0.65 | 0.02 | 0.81 | 0.00 | 0.01 |
Bold = conditional response probabilities over 0.5 or over 0.33 for three-level frequency indicators (none vs. < daily vs. daily use). Conditional Response Probabilities are the probability of reporting indicator substance use behaviour given class membership.
PWID, people who inject drugs.
Primary covariates
HIV-associated injection behaviours included past 6 month engagement (yes/no) in receptive syringe sharing; distributive syringe sharing; and sharing of cookers, cotton or rinse water. HIV-associated sexual behaviours included past 6 month engagement (yes/no) in unprotected sex with a casual partner; having two or more casual partners; exchanging sex for food, money, drugs or shelter; and using drugs during or within two hours before having sex. Participants self-reported lifetime and past 6 month history of overdose (yes/no), which was defined as a time when the participant passed out due to drug use and could not wake or their lips turned blue. HIV testing was conducted with rapid Determine® HIV tests followed by a second, different rapid test for HIV-positive results. HIV-positive individuals were given referrals for free or reduced-cost healthcare.
Secondary covariates
Age, gender, education, deportation history from the US (yes/no), and lifetime residence in Tijuana (yes/no) were assessed. Participants reported their first illegal drug use (dichotomised into marijuana vs. other), age at first drug use, drug used at first injection (dichotomised into heroin vs. other), and age at first injection. Additional covariates included: lifetime history of ever being forced to have sex (yes/no), typical number of hours spent on the street, and monthly income (dichotomised into greater or less than $2,500 Mexican pesos/month, or about $200 USD in 2011). To assess interactions with their risk environment, participants reported detention or incarceration by the police in the past 6 months (yes/no) and in which neighbourhood they most often injected (dichotomised into Zona Norte/‘El Bordo’ vs. other). To determine need for harm reduction services, participants were asked to what degree they needed help for drug use (dichotomised into no need vs. some, great, or urgent need) and difficulty with obtaining sterile syringes (dichotomised into easy or very easy vs. hard or very hard). Lastly, participants reported whether they ever received methadone maintenance (yes/no).
Statistical Analysis
LCA is an exploratory person-centred nonparametric approach used to probabilistically determine and classify a heterogeneous population into more homogenous latent or unobserved subgroups, based on a set of observed indicator variables [25,26]. Compared to traditional approaches of assigning individuals to classes or estimating associations as part of the model fitting process, the three-step procedure improves efficiency and corrects for measurement and classification bias in determining associations between latent class membership and covariates. The three-step approach fixes, or constrains, the measurement relationship between assigned most likely class membership and latent class to account for classification error [27]. Below, we outline the three-step process.
LCA Measurement Model (Step 1)
First, latent class analysis was conducted in Mplus version 7.0 [28] to determine latent classes of polydrug use, using 11 indicators of past 6 month drug use (8 dichotomous indicators and 3 ordinal indicators). Models were fit with increasing number of classes until model fit statistics were no longer improving, using statistical fit indices of Akaike Information Criteria (AIC), BIC, sample size adjusted Bayesian Information Criteria (BIC), Lo-Mendell-Rubin adjusted Likelihood Ratio Test (LMRT), and descriptive fit index of entropy. The best fitting model was selected based on smallest AIC, BIC and sBIC; significant LMRT (P <0.05); highest entropy; classification quality; and substantive interpretability. Resulting conditional response probabilities (probability of endorsing an indicator given class membership) were used to characterise classes.
LCA with covariates
Logits of classification probabilities were extracted (Step 2) to incorporate measurement error for most likely class membership into an auxiliary model (Step 3) with most likely class and fixed measurement error using the automated 3 step approach in Mplus [27,29,30]. Resulting logit parameter estimates from univariate multinomial logistic regression analyses were converted into odds ratios to determine bivariate associations between most likely class membership and covariates, with the largest class as the reference group.
Multivariate model building
Covariates with P <0.25 in the bivariate analyses were selected for inclusion into multivariate models [31]. By starting with a bivariate screen, we were able to assess the overall relationships between latent classes and covariates without collinearity concerns, and to demonstrate differences between unadjusted and adjusted estimates. Blocks of covariates were entered in the model in a forward stepwise manner, starting with: (i) HIV risk behaviours and overdose (primary variables of interest); followed by (ii) background factors; and then (iii) risk environment factors. In order to present the most parsimonious adjusted model and avoid overfitting, covariates were selected for the final adjusted model if P <0.1 for any association between class membership and the given covariate. In order to test if eliminated HIV risk behaviours and overdose variables were potential confounders, they were added back into the model to see if coefficient estimates changed substantially (+/− 20%) and if so these variables were retained in the final model. Although confidence intervals for effect sizes are not reported in Mplus, we also compared standard errors for beta coefficients between unadjusted and adjusted models to further assess whether omitted covariates were potential confounders.
RESULTS
Sample characteristics
Among this sample of PWID (N=735), 38.0% were female and the median age was 37 years. Slightly over a third (36.2%) had spent their whole lives in Tijuana, while one-fifth (22.7%) came to Tijuana after being deported from the United States. (Table 3)
Table 3.
Bivariate associations between class membership and HIV risk behaviours, overdose, background, risk environment among PWID in Tijuana (N = 735)
| Class 1: Polydrug and polyroute + cocaine (5%) |
Class 2: Polydrug and polyroute (29%) |
Class 3: Stimulant and heroin injecting (4%) |
Class 4: Meth and heroin injecting (10%) |
||||||
|---|---|---|---|---|---|---|---|---|---|
| N (%) | OR | P-value | OR | P-value | OR | P-value | OR | P-value | |
| HIV injection risk behaviour (past 6 months) | |||||||||
| Receptive syringe sharing | 525 (71.4) | 3.66 | 0.016 | 3.20 | <0.001 | 1.07 | 0.87 | 1.26 | 0.43 |
| Distributive syringe sharing | 531 (72.2) | 5.34 | 0.006 | 3.43 | <0.001 | 1.40 | 0.45 | 1.49 | 1.81 |
| Cooker, cotton, rinse water sharing | 490 (66.9) | 5.39 | 0.002 | 4.48 | <0.001 | 1.89 | 0.15 | 1.46 | 0.19 |
| HIV sex risk behaviour (past 6 months) | |||||||||
| 2+ casual partners | 261 (35.9) | 2.38 | 0.026 | 1.55 | 0.05 | 0.91 | 0.83 | 1.23 | 0.48 |
| Unprotected sex with casual partner |
241 (33.1) | 3.08 | 0.004 | 2.31 | <0.001 | 1.01 | 0.99 | 1.24 | 0.48 |
| Exchanged sex | 226 (31.1) | 4.01 | <.001 | 2.55 | <0.001 | 0.61 | 0.38 | 1.42 | 0.25 |
| Drug use before or during sex | 567 (77.4) | 5.16 | 0.016 | 3.82 | <0.001 | 1.20 | 0.69 | 1.69 | 0.12 |
| HIV and overdose | |||||||||
| Ever overdose | 401 (54.6) | 1.63 | 0.20 | 1.04 | 0.87 | 2.71 | 0.04 | 1.27 | 0.39 |
| Past 6 months overdose | 74 (10.1) | 3.35 | 0.01 | 1.68 | 0.15 | 1.89 | 0.30 | 1.15 | 0.77 |
| HIV positive | 26 (3.5) | 2.04 | 0.291 | 0.63 | 0.47 | --a | <.001 | 0.25 | 0.30 |
| Background | |||||||||
| Age, mean (SD) | 37.0 (8.9) | 0.95 | 0.04 | 0.98 | 0.18 | 1.00 | 0.83 | 0.99 | 0.56 |
| Female | 279 (38.0) | 1.88 | 0.09 | 1.95 | 0.00 | 0.60 | 0.30 | 1.37 | 0.27 |
| Years education, mean (SD) | 7.9 (3.01) | 1.18 | 0.04 | 1.16 | <0.001 | 1.13 | 0.03 | 1.07 | 0.15 |
| Deported to Tijuana | 176 (22.7) | 0.94 | 0.91 | 1.36 | 0.57 | 1.46 | 0.55 | 1.15 | 0.79 |
| Whole life in Tijuana | 266 (36.2) | 0.41 | 0.04 | 0.45 | 0.00 | 1.38 | 0.43 | 1.28 | 0.37 |
| Ever experienced forced sex | 117 (15.9) | 3.23 | 0.01 | 3.35 | <0.001 | 1.81 | 0.29 | 1.07 | 0.89 |
| Age of first injection, mean (SD) | 21.2 (6.8) | 0.94 | 0.13 | 1.04 | 0.02 | 0.97 | 0.53 | 0.97 | 0.25 |
| Heroin first drug injected | 578 (78.6) | 0.53 | 0.14 | 0.53 | 0.02 | 0.23 | 0.00 | 0.64 | 0.18 |
| Age of first drug use, mean (SD) | 14.7 (4.4) | 0.82 | 0.19 | 0.97 | 0.20 | 0.91 | 0.04 | 0.99 | 0.66 |
| Marijuana first drug used | 464 (63.1) | 0.89 | 0.81 | 1.21 | 0.66 | 1.25 | 0.63 | 1.18 | 0.69 |
| Risk environment (past 6 months) | |||||||||
| Hours on street, mean (SD) | 13.2 (6.9) | 1.04 | 0.20 | 0.97 | 0.05 | 1.08 | 0.01 | 1.02 | 0.34 |
| Income over 2500 pesos/month | 362 (49.5) | 1.92 | 0.08 | 3.95 | <0.001 | 1.63 | 0.23 | 1.49 | 0.15 |
| Stopped or Arrested | 373 (50.8) | 1.26 | 0.52 | 1.73 | 0.01 | 1.54 | 0.29 | 1.02 | 0.95 |
| Inject most often in Zona Norte or El Bordo |
301 (41.8) | 0.89 | 0.77 | 1.60 | 0.03 | 0.66 | 0.36 | 1.31 | 0.34 |
| In jail past 6 months | 270 (36.7) | 2.52 | 0.01 | 2.11 | 0.00 | 0.93 | 0.88 | 0.88 | 0.67 |
| Hard to find sterile syringes | 136 (18.5) | 1.73 | 0.21 | 1.46 | 0.18 | 2.89 | 0.02 | 1.31 | 0.45 |
| Ever on methadone | 204 (27.8) | 2.58 | 0.01 | 1.91 | 0.01 | 0.84 | 0.73 | 1.44 | 0.24 |
| Currently on methadone | 35 (4.8) | 2.94 | 0.09 | 1.58 | 0.352 | 0.80 | 0.85 | 0.56 | 0.54 |
| Any need for help for drug use | 640 (87.2) | 1.49 | 0.51 | 1.33 | 0.40 | 0.85 | 0.77 | 2.86 | 0.08 |
Reference class: Class 5 Heroin injecting. Bivariate associations from univariate multinomial logistic regression with fixed measurement relationship between most likely latent class membership and latent class. a Odds ratio approached zero due to count of 0 for people with HIV and in class 3. Bold = P <0.05, Italics = P <0.10. OR, odds ratio; PWID, people who inject drugs.
Nearly all participants injected heroin (95.2%) and 90.0% injected heroin daily in the past 6 months. Over half reported co-injecting heroin and methamphetamine (55.9%), with over one-third injecting this combination daily (38.5%). More than a quarter (28.4%) injected methamphetamine alone, with 13.1% reporting daily injection. Two-fifths (41.4%) reported methamphetamine smoking, with 16.1% smoking daily. Nearly a third of participants smoked marijuana (31.6%), and although use of prescription opiates and hallucinogens was quite low (<5%), one in five (19.5%) ingested tranquillizers.
The majority of participants engaged in at least one HIV injection risk behaviour (66.9–72.2%) and over one-third engaged in at least one HIV sexual risk behaviour (31.1–77.4%) in the past 6 months. HIV prevalence was 3.5%. Over half the participants reported a history of overdose (54.6%), with 10.1% reporting an overdose in the past 6 months.
Determining number of latent classes
After comparing the fit indices across models, the 5 class solution was selected given a significant LMRT, highest entropy, low AIC and sBIC, classification quality, class size, and spread of conditional response probabilities relative to models with 4, 6, and 7 class solutions. (Table 1)
Table 1.
Fit statistics for latent class models fit to 2–7 classes (N = 735 PWID in Tijuana)
| Classes | AIC | BIC | sBIC | LMRT | Entropy |
|---|---|---|---|---|---|
| 2 | 7970.809 | 8104.205 | 8012.12 | <.0001 | 0.732 |
| 3 | 7818.46 | 8020.855 | 7881.14 | <.0001 | 0.792 |
| 4 | 7715.792 | 7987.184 | 7799.839 | 0.0074 | 0.786 |
| 5 | 7656.911 | 7997.302 | 7762.327 | 0.0089 | 0.851 |
| 6 | 7613.863 | 8023.251 | 7740.646 | 0.3231 | 0.833 |
| 7 | 7603.749 | 8082.135 | 7751.9 | 0.9622 | 0.825 |
AIC, Akaike Information Criteria; BIC, Bayesian Information Criteria; sBIC, sample size adjusted Bayesian Information Criteria; LMRT, Lo-Mendell-Rubin adjusted Likelihood Ratio Test P-value; PWID, people who inject drugs. Bold = Ideal number of classes given fit statistic. 5-class model selected for further analyses
Class descriptions
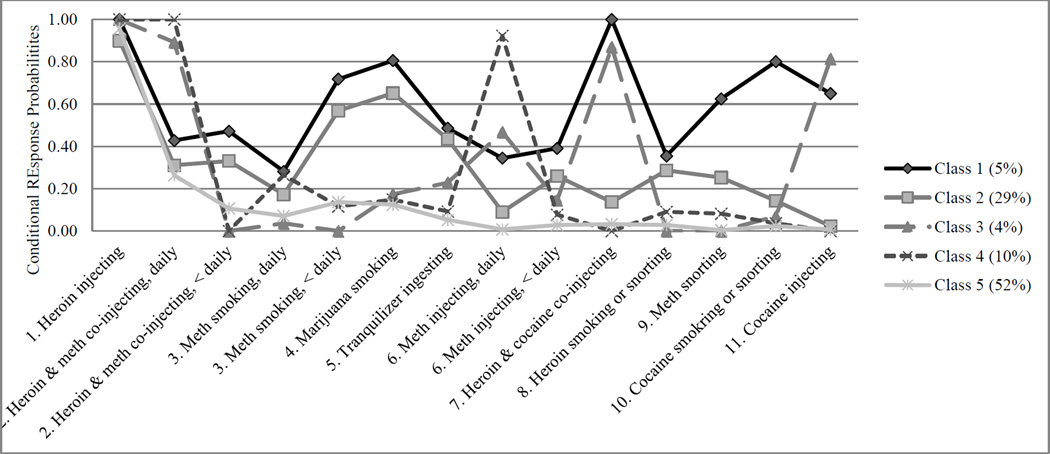
Class 1 (polydrug and polyroute + cocaine; 5% of sample). Participants in this class had the highest probabilities of non-injection use of heroin, methamphetamine, marijuana, tranquilizer, and cocaine use as well as high probabilities of injection and co-injection drug use. (Table 2, Figure 1)
Figure 1. Conditional response probabilities of 11 substance use indicators (N = 735 PWID in Tijuana).
Class 1: Polydrug and polyroute + cocaine, Class 2: Polydrug and polyroute, Class 3: Stimulant and heroin injecting, Class 4: Methamphetamine and heroin injecting, Class 5: Heroin injecting. PWID, people who inject drugs.
Class 2 (polydrug and polyroute; 29% of sample). In addition to high probabilities of methamphetamine and heroin injection, participants in this class had moderate to high probabilities of non-injection use of other substances, but in contrast to class 1, had much lower probabilities of any cocaine use. These two classes used multiple substances and routes of administration and had higher probabilities of less than daily use.
Class 3 (stimulant and heroin injection; 4% of sample) had high probabilities of injection, particularly heroin injection, heroin and cocaine co-injection, and daily heroin and methamphetamine co-injection. This class and the other two classes were characterised mainly by injection drug use, and were different from each other in the type of substances injected.
Class 4 (methamphetamine and heroin injection, 10% of sample) also had high probabilities of daily injection, but differed from class 3 in that they did not use cocaine.
Class 5 (predominantly heroin injection; 52% of sample) comprised the largest class and was characterised primarily by a high probability of injecting heroin.
Latent class analysis with covariates
In both bivariate and multivariate analyses, membership in the polydrug and polyroute using classes (classes 1 and 2) was significantly associated with HIV risk behaviours. In bivariate analyses (Table 3) compared to the predominantly heroin injection class (class 5), membership in classes 1 and 2 was significantly and positively associated with all injection and sexual risk behaviours. Membership in class 1 (polydrug and polyroute + cocaine) was significantly associated with having an overdose in the past 6 months, but only at the bivariate level. There were no significantly differences between classes 4 (heroin and methamphetamine injectors) and 5 with respect to HIV risk behaviours or overdose.
In the final multivariate model (Table 4), compared to heroin injecting (class 5), membership in the polydrug and polyroute classes (i.e. classes 1 and 2) was again independently associated with the following HIV risk behaviours and sexual history: sharing cookers, cotton or rinse water (class 1 adjusted odds ratio (AOR) = 7.22, class 2 AOR = 4.35), using drugs before or during sex (class 1 AOR = 7.31, class 2 AOR = 3.55), and ever experiencing forced sex (class 1 AOR = 3.70, class 2 AOR = 3.10). Additionally, higher income was independently associated with being in the polydrug and polyroute class (class 2). Injecting a drug other than heroin at first injection was independently associated with membership in the stimulant and heroin injection class (class 3).
Table 4.
Independent associations between class membership and covariates among PWID in Tijuana (N = 707)
| Class 1: Polydrug and polyroute + cocaine (5%) |
Class 2: Polydrug and polyroute (29%) |
Class 3: Stimulant and heroin injectors (4%) |
Class 4: Meth and heroin injectors (10%) |
|||||
|---|---|---|---|---|---|---|---|---|
| AOR | P-value | AOR | P-value | AOR | P-value | AOR | P-value | |
| Cooker, cotton, rinse water sharing | 7.22 | 0.005 | 4.35 | <0.001 | 1.54 | 0.349 | 1.30 | 0.399 |
| Drug use before or during sex | 7.31 | 0.022 | 3.55 | 0.002 | 1.15 | 0.767 | 1.64 | 0.152 |
| Years education | 1.18 | 0.053 | 1.09 | 0.048 | 1.12 | 0.086 | 1.06 | 0.306 |
| Age of first injection | 0.96 | 0.426 | 1.05 | 0.013 | 0.99 | 0.792 | 0.98 | 0.433 |
| Heroin first drug injected | 0.61 | 0.289 | 0.59 | 0.110 | 0.26 | 0.004 | 0.73 | 0.397 |
| Ever experienced forced sex | 3.70 | 0.008 | 3.10 | 0.003 | 1.68 | 0.380 | 0.90 | 0.845 |
| Hours on street | 1.06 | 0.057 | 0.98 | 0.243 | 1.09 | 0.009 | 1.03 | 0.239 |
| Income over 2500 pesos/month | 1.34 | 0.496 | 3.35 | <.001 | 1.64 | 0.258 | 1.45 | 0.210 |
| Any current need for help for drug use | 2.37 | 0.232 | 1.49 | 0.322 | 1.02 | 0.972 | 3.19 | 0.081 |
Reference class: Class 5 Heroin injecting. Adjusted associations from multivariate multinomial logistic regression with fixed measurement relationship between most likely latent class membership and latent class. Bold = P < 0.05, Italics = P<0.10. AOR, adjusted odds ratio; PWID, people who inject drugs.
DISCUSSION
This latent class analysis of drug use among PWID in Tijuana identified five classes of polydrug use that captured four dimensions of use: type of substance, route of administration, co-injection and frequency of use. The five classes were: polydrug and polyroute + cocaine use, polydrug and polyroute use, stimulant and heroin injection, methamphetamine and heroin injection, and heroin injection. Compared to the heroin injecting class, the two polydrug and polyroute classes (1 and 2) characterised by use of multiple substances and route of administration were more likely to report HIV risk behaviours. These polydrug and polyroute classes were both independently associated with sharing cookers, cotton, or rinse water and using drugs before or during sex. Findings are partially consistent with hypotheses that PWID using more substances, especially stimulants, would have higher HIV risk compared to heroin injectors (class 5). However, it was the polydrug and polyroute users in particular that had elevated HIV infection and sexual risk relative to heroin injectors (class 5).
Findings are largely consistent with existing literature from other settings, which demonstrated that polydrug using classes were more likely to report needle sharing [13] and overdose risk [15] when compared to mainly heroin or opiate using classes. Two studies of opioid users in treatment found that polydrug users [32] and illicit opioid users [33] were at higher risk for HIV than non-polydrug users.
Latent class analyses of polydrug use have also been associated with the HIV sexual risk behaviours examined in this study. In particular, classes with stimulant smoking were more likely to report inconsistent condom use [34], transactional sex [14], and sexual risk-taking [18,19]. Similarly, studies of drug use among men who have sex with men in the United States and Malaysia [35–38] also found that polydrug using classes were more likely to report unsafe sexual behaviours in comparison to low or single substance use classes. In our prior analysis with an earlier cohort of PWID in Tijuana, we found that a small class (6%) defined by use of heroin, methamphetamine, and cocaine exhibited higher-risk sexual practices.
Findings from this study add to the preceding literature by further demonstrating heterogeneity of drug use patterns in this population defined by its low resource setting and route of administration (i.e. injection) and replicating earlier findings that use of multiple substances through multiple routes is independently associated with elevated HIV risk. Polyroute users in particular might be in multiple drug using networks with non-injection drug users and therefore may act as a “bridge population” by introducing HIV to these other networks through unprotected sex or injection initiation. The sharing of injection equipment among the polydrug and polyroute users may be part of a “moral economy of sharing” [39], in which PWID share any available resources of drugs or injection equipment (in addition to food or shelter) to establish and maintain social and economic ties.
The strong association between history of forced sex and polydrug and polyroute use in this study may be indicative of drug use as a trauma coping mechanism. Polydrug and polyroute users may have specific needs that make them more susceptible to both more heterogeneous drug use and high risk behaviour [17,40], as well as have unique difficulties in opiate substitution therapy and other treatment retention. Research to determine those needs will help with designing interventions with the most likelihood of reducing their risk.
Most previous latent class analyses of polydrug use have used only a small number of binary indicators with at least 15–20% overall prevalence. For future latent class analyses, these findings demonstrate the feasibility of using indicators with less than 15% prevalence, ordinal indicators [12], and a large number of indicators [41].
The primary limitation of this study is that all substance use was self-reported, though several studies have demonstrated the general validity of self-report [42] and, to be eligible for this study, participants were already admitted illicit drug users. Second, the definition provided to participants about overdose is more descriptive of opioid related overdose and thus may have missed cases of stimulant related overdose thus resulting in small sample sizes and less power to detect independently significant odds of overdose for polydrug and polyroute + cocaine users. Third, given the cross-sectional nature of the data, associations are not causal. Fourth, although listwise deletion removed several cases in multivariable regression analyses, covariates were missing data for only 2–4 participants. Less than 5% of the sample was excluded from analysis due to missing data, which likely had an inconsequential effect on the regression estimates [43]. Another limitation is that confidence intervals are not provided by Mplus for this type of analysis. Lastly, quantity of substances consumed and concurrent alcohol use may also inform polydrug use profiles, however these factors were not assessed and neither was the presence of mental health comorbidities or severity of addiction.
Conclusions and Future Research
Findings from this analysis highlight the heterogeneity in substance use patterns among PWID in Tijuana and demonstrate that polydrug and polyroute users are a high-risk subgroup. To reduce HIV and overdose risk in resource limited settings, resources need to be targeted towards polydrug and polyroute users, and interventions should be focused on the motivations and rationales for using multiple substances and multiple routes of administration as distinct from those who only inject or, more specifically, only inject heroin. To address the historic underreporting of polydrug use among PWID, epidemiologic and treatment studies should assess and report substances used as well as non-injection substance use.
Acknowledgments
The authors gratefully acknowledge the contributions to this research by the study participants and staff. This research is funded by the National Institutes of Health grant R37 DA019829; MM was supported by T32 DA023356 and T32 DA007250 and TG was supported by K01 DA034523.
REFERENCES
- 1.Degenhardt L, Whiteford HA, Ferrari AJ, Baxter AJ, Charlson FJ, Hall WD, Freedman G, Burstein R. Global burden of disease attributable to illicit drug use and dependence: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382:1564–1574. doi: 10.1016/S0140-6736(13)61530-5. [DOI] [PubMed] [Google Scholar]
- 2.UNODC. World Drug Report. Vienna: United Nations Office of Drugs and Crime; 2014. [Google Scholar]
- 3.Meacham MC, Rudolph AR, Strathdee S, et al. Polydrug use and HIV risk among people who inject heroin in Tijuana, Mexico: A latent class analysis. Subst Use Misuse. 2015;50:1351–1359. doi: 10.3109/10826084.2015.1013132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Degenhardt L, Hall W. Extent of illicit drug use and dependence, and their contribution to the global burden of disease. Lancet. 2012;379:55–70. doi: 10.1016/S0140-6736(11)61138-0. [DOI] [PubMed] [Google Scholar]
- 5.Conway KP, Compton WM, Miller PM. Novel approaches to phenotyping drug abuse. Addict Behav. 2006;31:923–928. [Google Scholar]
- 6.Coffin PO, Galea S, Ahern J, Leon AC, Vlahov D, Tardiff K. Opiates, cocaine and alcohol combinations in accidental drug overdose deaths in New York City, 1990–98. Addiction. 2003;98:739–747. doi: 10.1046/j.1360-0443.2003.00376.x. [DOI] [PubMed] [Google Scholar]
- 7.Gossop M, Griffiths P, Powis B, Williamson S, Strang J. Frequency of non-fatal heroin overdose: survey of heroin users recruited in non-clinical settings. BMJ. 1996;164:660–664. doi: 10.1136/bmj.313.7054.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Davidson P. Circumstances of death: as assessment of the viability of using non-toxicological coronial data to investigate opiate overdose risk factors. National Centre for Research into the Prevention Of Drug Abuse; 1999. [Google Scholar]
- 9.Patterson TL, Semple SJ, Staines H, et al. Prevalence and correlates of HIV infection among female sex workers in 2 Mexico-US border cities. J Infect Dis. 2008;197:728–732. doi: 10.1086/527379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hahn JA, Woolf-King SE, Muyindike W. Adding fuel to the fire: alcohol's effect on the HIV epidemic in Sub-Saharan Africa. Curr HIV/AIDS Rep. 2011;8:172–180. doi: 10.1007/s11904-011-0088-2. [DOI] [PubMed] [Google Scholar]
- 11.Connor JP, Gullo MJ, White A, Kelly AB. Polysubstance use: diagnostic challenges, patterns of use and health. Curr Opin Psychiatry. 2014;27:269–275. doi: 10.1097/YCO.0000000000000069. [DOI] [PubMed] [Google Scholar]
- 12.Tomczyk S, Isensee B, Hanewinkel R. Latent classes of polysubstance use among adolescents—a systematic review. Drug Alcohol Depend. 2016;160:12–29. doi: 10.1016/j.drugalcdep.2015.11.035. [DOI] [PubMed] [Google Scholar]
- 13.Kuramoto SJ, Bohnert ASB, Latkin CA. Understanding subtypes of inner-city drug users with a latent class approach. Drug Alcohol Depend. 2011;118:237–243. doi: 10.1016/j.drugalcdep.2011.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harrell P, Mancha B, Petras H, Trenz R, Latimer W. Latent classes of heroin and cocaine users predict unique HIV/HCV risk factors. Drug Alcohol Depend. 2012;122:220–227. doi: 10.1016/j.drugalcdep.2011.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Monga N, El-Guebalyc N, Rehma LN, et al. Using latent class analysis (LCA) to analyze patterns of drug use in a population of illegal opioid users. Drug Alcohol Depend. 2007;88:1–8. doi: 10.1016/j.drugalcdep.2006.08.029. [DOI] [PubMed] [Google Scholar]
- 16.Patra J, Fischer B, Maksimowska S, Rehm J. Profiling poly-substance use typologies in a multi-site cohort of illicit opioid and other drug users in Canada – a latent class analysis. Addict Res Theory. 2009;17:168–185. [Google Scholar]
- 17.Trenz RC, Scherer M, Duncan A, Harrell PT, Moleko AG, Latimer WW. Latent class analysis of polysubstance use, sexual risk behaviors, and infectious disease among South African drug users. Drug Alcohol Depend. 2013;132:441–448. doi: 10.1016/j.drugalcdep.2013.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wechsberg WM, Myers B, Kline TL, Carney T, Browne FA, Novak SP. The relationship of alcohol and other drug use typologies to sex risk behaviors among vulnerable women in Cape Town, South Africa. J AIDS Clin Res. 2012;S1(15):pii: 015. doi: 10.4172/2155-6113.S1-015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morley KI, Lynskey MT, Moran P, Borschmann R, Winstock AR. Polysubstance use, mental health and high-risk behaviours: Results from the 2012 Global Drug Survey. Drug Alcohol Rev. 2015;34(4):427–437. doi: 10.1111/dar.12263. Epub 2015/04/14. [DOI] [PubMed] [Google Scholar]
- 20.Brouwer KC, Case P, Ramos R, et al. Trends in production, trafficking, and consumption of methamphetamine and cocaine inMexico. Subst UseMisuse. 2006;41:707–721. doi: 10.1080/10826080500411478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bucardo J, Brouwer KC, Magis-Rodriguez C, et al. Historical trends in the production and consumption of illicit drugs in Mexico: Implications for the prevention of blood borne infections. Drug Alcohol Depend. 2005;79:281–293. doi: 10.1016/j.drugalcdep.2005.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rusch M, Lozada R, Pollini R, et al. Polydrug use among IDUs in Tijuana, Mexico: correlates of methamphetamine use and route of administration by gender. J Urban Health. 2009;86:760–775. doi: 10.1007/s11524-009-9377-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Roth AM, Armenta RA, Wagner KD, et al. Patterns of drug use, risky behavior, and health status among persons who inject drugs living in San Diego, California: a latent class analysis. Subst Use Misuse. 2015;50:205–214. doi: 10.3109/10826084.2014.962661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Robertson A, Garfein R, Wagner K, et al. Evaluating the impact of Mexico's drug policy reforms on people who inject drugs in Tijuana, BC, Mexico, and San Diego, CA, United States: a binational mixed methods research agenda. Harm Reduct J. 2014;11(4) doi: 10.1186/1477-7517-11-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Collins L, Lanza S. Latent Class and Latent Transition Analysis. New Jersey: Wiley; 2010. [Google Scholar]
- 26.Flaherty BP, Kiff CJ. Cooper H, editor. Latent class and latent profile models. APA Handbook of Research Methods in Psychology Data Analysis and Research Publication. 2012 [Google Scholar]
- 27.Asparouhov T, Muthén B. Auxiliary Variables in Mixture Modeling: Three-Step Approaches Using Mplus. Structural Equation Modeling. 2014;21:329–341. [Google Scholar]
- 28.Muthén LK, Muthén BO. Mplus User's Guide. Seventh. Los Angeles, CA: Muthén & Muthén; 1998–2012. [Google Scholar]
- 29.Vermunt JK. Latent class modeling with covariates: two improved three-step approaches. Poltical Analysis. 2010;18:450–469. [Google Scholar]
- 30.Feingold A, Tiberio SS, Capaldi DM. New approaches for examining associations with latent categorical variables: applications to substance abuse and aggression. Psychol Addict Behav. 2014;28:257–267. doi: 10.1037/a0031487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hosmer DW, Lemeshow S, Sturdivant RX. Applied logistic regression. John Wiley & Sons; 2013. [Google Scholar]
- 32.Wu L-T, Ling W, Burchett B, et al. Use of item response theory and latent class analysis to link poly-substance use disorders with addiction severity, HIV risk, and quality of life among opioid-dependent patients in the Clinical Trials Network. Drug Alcohol Depend. 2011;118:186–193. doi: 10.1016/j.drugalcdep.2011.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Green TC, Black R, Serrano JMG, Budman SH, Butler SF. Typologies of prescription opioid use in a large sample of adults assessed for substance abuse treatment. PLoS One. 2011;6:e27244. doi: 10.1371/journal.pone.0027244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Roy É, Richera I, Arrudac N, Vandermeerschena J, Bruneaud J. Patterns of cocaine and opioid co-use and polyroutes of administration among street-based cocaine users in Montréal, Canada. Int J Drug Policy. 2013;24:142–149. doi: 10.1016/j.drugpo.2012.10.004. [DOI] [PubMed] [Google Scholar]
- 35.McCarty-Caplan D, Jantz I, Swartz J. MSM and drug use: a latent class analysis of drug use and related sexual risk behaviors. AIDS Behav. 2014;18:1339–1351. doi: 10.1007/s10461-013-0622-x. [DOI] [PubMed] [Google Scholar]
- 36.Wilkerson JM, Noor SW, Breckenridge ED, Adeboye AA, Rosser BS. Substance-use and sexual harm reduction strategies of methamphetamine-using men who have sex with men and inject drugs. AIDS care. 2015;27:1047–1054. doi: 10.1080/09540121.2015.1020280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lim SH, Cheung DH, Guadamuz TE, Wei C, Koe S, Altice FL. Latent class analysis of substance use among men who have sex with men in Malaysia: Findings from the Asian Internet MSM Sex Survey. Drug Alcohol Depend. 2015;151:31–37. doi: 10.1016/j.drugalcdep.2015.02.040. [DOI] [PubMed] [Google Scholar]
- 38.Yu G, Wall MM, Chiasson MA, Hirshfield S. Complex drug use patterns and associated HIV transmission risk behaviors in an Internet sample of US men who have sex with men. Arch Sex Behav. 2015;44:421–428. doi: 10.1007/s10508-014-0337-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bourgois P, Schonberg J. California series in public anthropology. Berkeley. CA: University of California Press; 2009. Righteous Dopefiend. [Google Scholar]
- 40.Drake S, Torok M. The association of child physical abuse with the onset and extent of drug use among regular injecting drug users. Addiction. 2014;109:610–614. doi: 10.1111/add.12428. [DOI] [PubMed] [Google Scholar]
- 41.Wurpts IC, Geiser C. Is adding more indicators to a latent class analysis beneficial or detrimental? Results of a Monte-Carlo study. Frontiers in psychology. 2014:5. doi: 10.3389/fpsyg.2014.00920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Darke S. Self-report among injecting drug users: a review. Drug Alcohol Depend. 1998;51:253–263. doi: 10.1016/s0376-8716(98)00028-3. [DOI] [PubMed] [Google Scholar]
- 43.Schafer JL. Multiple imputation: a primer. Stat Methods Med Res. 1999;8:3–15. doi: 10.1177/096228029900800102. [DOI] [PubMed] [Google Scholar]