Abstract
Background
Disparities in total joint arthroplasty (TJA) have largely been studied in single center studies and using administrative data. Our objective was to investigate differences in TJA outcomes in white men, black men, white women, and black women using a large international registry.
Methods
We used 2010–2013 data from the ACS-NSQIP to identify four groups of adults (white men, black men, white women, black women) who underwent primary total knee arthroplasty (TKA) or total hip arthroplasty (THA). We compared differences in: 1) surgical complications (mortality, pulmonary embolism, wound infection, sepsis, blood loss requiring transfusion, myocardial infarction, pneumonia, acute renal failure, and a composite representing occurrence of one-or-more adverse outcomes); 2) discharge to a nursing home.
Results
We identified 62,075 TKA and 39,334 THA patients. For TKA 35.3% were white men, 57.2% white women, 1.9% black men, and 5.6% black women. White and black women were significantly more likely to experience our composite outcome when compared to their male counterparts (16.5% and 14.1% for white women and white men; P<.001) (18.3% and 14.3% for black women and black men; P=.002); higher complications for women were explained by higher transfusion rates in women (14.9% vs 12.2% for white women and men, 16.4% vs 11.7% for black; P<.001 for both). For TKA blacks (compared to whites) and women (compared to men) were significantly more likely to be discharged to a nursing home. Results were similar for THA.
Conclusions
In contrast to prior studies, we found that complications after primary TJA were generally similar among white and black men and women with the exception of markedly higher transfusion rates among women of both racial groups.
Background
Disparities in healthcare according to both patient race and sex are well recognized. (1) The literature is particularly robust with respect to cardiovascular disease (2) but also strong in other areas including total joint arthroplasty (TJA). (3–6)
When thinking about disparities it can be useful to differentiate between studies focusing on differences in access/utilization of effective procedures (e.g., organ transplant, TJA) and studies focusing on differences in patient outcomes. (7, 8) In the case of TJA there is a large body of literature demonstrating lower rates of utilization in blacks as compared to whites and higher utilization in women as compared to men. (5, 9, 10) Interpretation of these sex-specific findings are complicated because women have a higher prevalence of OA, live longer than men (more opportunity for TJA), and tend to receive TJA at a more advanced stage of disease. (11)
Literature evaluating differences in complication rates after total knee arthroplasty (TKA) and total hip arthroplasty (THA) have typically demonstrated higher complication rates in blacks as compared to whites and men as compared with women. (10, 12, 13) For example, Ibrahim et al found higher complication rates for black TJA patients treated in the United States (US) Veterans Administration healthcare system when compared to whites. (12) Cai and colleagues found higher TKA complication rates in blacks were partially explained by differences in the quality of the hospitals where blacks and whites underwent surgery. (14) Bozic and colleagues used US Medicare data to explore racial disparities in TJA complication rates, finding only small differences in complication rates between hospitals that treated a higher and lower percentage of black patients. (15) Interestingly, while several studies have examined sex-based disparities in TJA utilization and functional outcomes (e.g., pain, mobility), very few studies have evaluated differences in complication rates between men and women. (15–18) Moreover, many of the available studies of TJA disparities utilized administrative data which lack clinical nuances important in assessing orthopaedic outcomes or relied upon small single-center registries.
We used data from a large multi-center clinical registry- the National Surgical Quality Improvement Project (NSQIP) from the American College of Surgeons- to examine whether there were differences in TJA complication rates according to patient sex and race. (19) Based upon our review of the prior literature, we hypothesized that in unadjusted analyses TJA complication rates would be higher for blacks when compared to whites and men compared to women. However, we expected that after adjustment for patient comorbidities, differences in complication rates would not be significant between groups.
Methods
Data
We used data from the 2010–2013 American College of Surgeons National Surgical Quality Improvement Project (ACS NSQIP) participant use files (PUF). Details of the NSQIP have been described previously. (19)
Briefly, ACS NSQIP is a voluntary registry encompassing data from more than 450 participating hospitals with most located within the US. (20) Participants are more likely to be high volume academic medical centers when compared to non-participants. (21) Participating hospitals designate one-or-more clinical reviewers who undergo rigorous training and are responsible for entering data into the NSQIP on-line web-based data repository. Data are collected from an array of sources including chart abstraction, hospital medical records and computer systems, and direct patient query. To maintain flexibility and maximize participation, NSQIP allows for several different options for hospital participation with respect to which surgical procedures are reported, the number of different variables submitted per-case, and the surgical volumes required for participation. Additional details are available from ACS NSQIP and have been described in prior papers. (19, 21)
NSQIP collects approximately 300 variables per patient including demographics (age, race, sex), principal procedure (coded using Current Procedural Terminology [CPT]) codes, comorbidities and clinical factors and surgical outcomes. (22) Comorbidities include variables such as coronary artery disease, chronic obstructive pulmonary disease, diabetes, and renal failure. Clinical factors include smoking status, weight and height, which allow for calculation of body mass index (BMI), and American Society for Anesthesiologists (ASA) score (scores range from 1 [least severe] to 6 [most severe]). Surgical outcomes include wound infection, hemorrhage, pulmonary embolism, myocardial infarction, pneumonia, and death.
Analytic cohort
We identified all primary total knee arthroplasty (TKA, CPT 27447) and total hip arthroplasty (THA, CPT 27130) procedures reported in the NSQIP PUF in 2010–2013. We limited our analysis to patients’ whose race was coded as either white or black to insure adequate sample sizes. In accordance with prior studies, and to create a homogeneous population, (13, 23) we limited our analysis to primary elective TKA or THA procedures. We excluded a number of patient subgroups including: emergent cases; patients with acute fracture or active infection; patients with disseminated cancer; patients who were critically ill at the time of their surgery (ASA class >4) because such patients would not be typical of an elective primary TJA; and patients with a hospital length-of-stay of ≤ 1-day because of concerns that such a short stay would not be consistent with TKA or THA. We also excluded patients with age less than 30 or greater than 89 years because primary TJA is uncommon at such extreme ages.
Outcomes
Primary outcomes evaluated at the patient-level included: 1) occurrence of 1-or-more surgical complications within 30-days of surgery; 2) hospital readmission within 30-days of surgery; and 3) discharge to a nursing home or skilled care after hospitalization. Hospital length of stay (LOS) was a secondary outcome. Individual complications included in our analyses included: mortality; pulmonary embolism; wound infection; sepsis; blood loss requiring transfusion; myocardial infarction; pneumonia; acute renal failure; and a composite representing occurrence of one-or-more of the 8 individual outcomes. The individual outcomes we selected are similar to those outcomes used by the US Centers for Medicare and Medicaid Innovation for assessing TJA and are also similar to those outcomes that we and others have used in prior research studies. (24) Likewise, our use of a composite outcome follows established methodological precedent. (25) All outcomes were assessed using standard definitions as defined by NSQIP. Of note, hospital readmission and discharge disposition analyses were limited to data from 2011–2013 when these variables first became available from NSQIP.
Patient involvement
This study involved a retrospective analysis of the NSQIP surgical registry. As such, patients were not involved in the conception, execution, or interpretation of our study results.
Statistical analyses
We stratified both our TKA and THA cohorts into 4 separate groups: white men, white women, black men, and black women. Analyses were conducted separately for TKA and THA patients.
We began by using bivariate methods (Chi square test, Kruskal-Wallace test) to examine unadjusted differences in demographics, clinical risk factors, and comorbidity between our 4 patient groups. Next, we used similar methods to compare unadjusted outcomes (complication rates, readmission, discharge disposition, LOS) across the 4 groups.
For adjusted analyses we used multiple logistic regression to calculate risk standardized rates of outcomes (and 95% confidence intervals) while controlling for differences in patient demographics, clinical factors and comorbidity. (26) Separate models were generated for each of 3 different outcomes: 1) our composite adverse outcome; 2) discharge to either a nursing home or skilled care after index hospitalization; and 3) hospital readmission within 30-days of surgery. For these models patient age, sex, race, BMI, ASA-class, and procedure (TKA or THA) were forced into our models; other covariates (e.g., comorbid conditions, calendar year) were selected using a mixed stepwise selection process (c-statistics for models ranging from 0.64– 0.71). Details of our models and full statistical code is available on request.
All analyses were conducted using R version 3.0.2 statistical software (https://www.r-project.org/) with P<.05 deemed statistically significant. (27, 28) This project was approved by the University Health Network Research Ethics Board (IRB). All authors have completed the ICMJE uniform disclosure form and declare no support from any organization for the submitted work. All statistical code is available from the authors by request.
Results
We identified 104,756 patients who underwent TJA between 2010–2013 (Figure 1). After excluding 3,347 cases our final analytic cohort consisted of 101,409 primary elective TJA patients (62,075 TKA; 39,334 THA). For TKA 35.3% were white men, 57.2% were white women, 1.9% were black men, and 5.6% were black women (Table 1). For THA 41.1% were white men, 51.7% white women, 3.4% black men, and 3.9% black women (Table 1).
Figure 1.
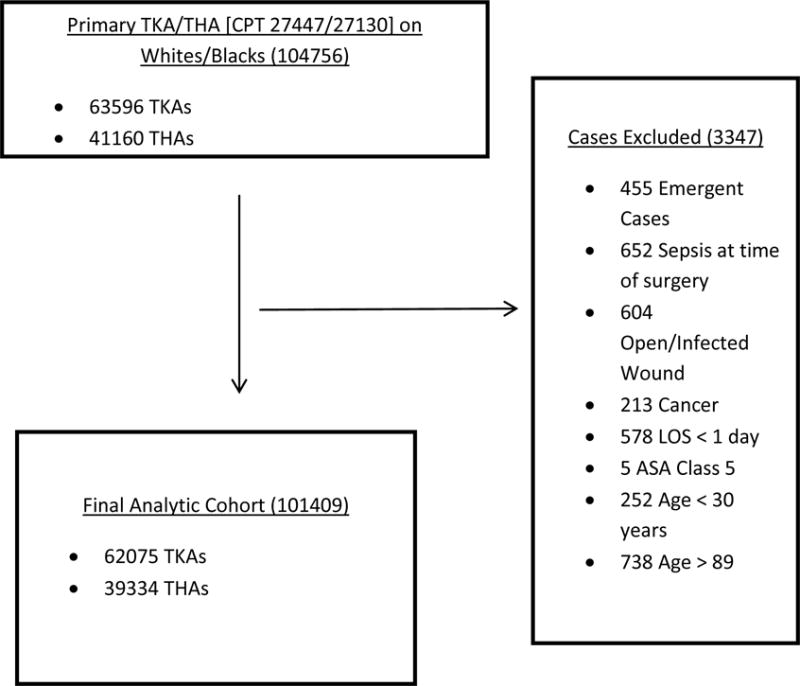
Generation of analytic cohorts for TKA and THA
TABLE 1.
Characteristics of patients undergoing primary TKA and THA in the NSQIP data 2010–2013
| TKA (N=62075) |
THA (N=39334) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Number, (%) | White Men 21900 (35.3) | White Women 35530 (57.2) | Black Men 1190 (1.9) | Black Women 3455 (5.6) | P-value | White Men 16167 (41.1) | White Women 20330 (51.7) | Black Men 1318 (3.4) | Black Women 1519 (3.9) | P-value |
| Age, years, mean (SD) | 66.8 (9.6) | 67.2 (9.8) | 62.5 (10.1) | 63.6 (9.9) | <.001 | 63.7 (11.2) | 66.7 (11.0) | 58.3 (11.0) | 62.3 (11.7) | <.001 |
| BMI, mean (SD) | 32.1 (6.3) | 33.2 (7.5) | 33.4 (7.1) | 36.3 (8) | <.001 | 30.7 (6) | 29.6 (6.9) | 30.6 (6.7) | 32.4 (7.2) | <.001 |
| Smoker, number (%) | 1962 (9.0) | 2677 (7.5) | 197 (16.6) | 454 (13.1) | <.001 | 2157 (13.3) | 2397 (11.8) | 360 (27.3) | 332 (21.9) | <.001 |
| Chronic steroid use, number (%) | 539 (2.5) | 1272 (3.6) | 31 (2.6) | 142 (4.1) | <.001 | 443 (2.7) | 774 (3.8) | 42 (3.2) | 100 (6.6) | <.001 |
| ASA class 3 or above, number (%) | 10569 (48.3) | 16297 (45.9) | 650 (54.6) | 2008 (58.1) | <.001 | 6831 (42.3) | 8022 (39.5) | 647 (49.1) | 787 (51.8) | <.001 |
| Hematocrit, mean (SD) | 42.5 (4.0) | 39.7 (3.6) | 40.8 (4.4) | 37.8 (3.5) | <.001 | 42.3 (4.2) | 39.4 (3.9) | 40.6 (4.5) | 37.6 (3.9) | <.001 |
| Comorbidities | ||||||||||
| Diabetes, number, (%) | 4030 (18.4) | 5472 (15.4) | 321 (27) | 821 (23.8) | <.001 | 2061 (12.7) | 1915 (9.4) | 249 (18.9) | 276 (18.2) | <.001 |
| Obesity, number, (%) | 12680 (58.0) | 22440 (63.3) | 775 (65.2) | 2681 (77.9) | <.001 | 7695 (47.7) | 8441 (41.6) | 636 (48.4) | 914 (60.3) | <.001 |
| Peripheral vascular disease, number, (%) | 37 (0.2) | 28 (0.1) | 3 (0.3) | 5 (0.1) | .032 | 37 (0.2) | 23 (0.1) | 5 (0.4) | 1 (0.1) | .009 |
| Hypertension, number, (%) | 14660 (66.9) | 23204 (65.3) | 918 (77.1) | 2746 (79.5) | <.001 | 9504 (58.8) | 11457 (56.4) | 868 (65.9) | 1115 (73.4) | <.001 |
| COPD, number, (%) | 851 (3.9) | 1205 (3.4) | 32 (2.7) | 135 (3.9) | .004 | 637 (3.9) | 924 (4.5) | 44 (3.3) | 60 (3.9) | .012 |
| CHF within last 30-days, number (%) | 56 (0.3) | 76 (0.2) | 6 (0.5) | 10 (0.3) | .166 | 63 (0.4) | 54 (0.3) | 9 (0.7) | 8 (0.5) | .014 |
Differences in patient characteristics by sex
Male TKA recipients were slightly younger than female TKA recipients among both whites and blacks (P<.001 for both). Male TKA recipients had slightly lower BMI than their female counterparts (P<.001 for both white and black) and men were significantly more likely to smoke than women (P<.001 for both). Looking at comorbid conditions among TKA recipients (Table 1) differences between sex (men and women) were clinically small (though often statistically significant [P<.05])). However, both black men and black women had clinically significantly higher rates of many comorbidities including hypertension, diabetes, and obesity (P<.001). Analyses focusing on sex differences in the THA cohort (Table 1) yielded generally similar results.
Differences in patient characteristics by race
Looking at differences in patient characteristics by race, both white men and white women receiving TKA were significantly older than their black counterparts (P<.001 for both). White men and white women who underwent TKA had significantly lower BMI than their black counterparts (P<.001 for both); differences in BMI were particularly large for white and black women. A significantly higher percentage of black men and black women who underwent TKA had an ASA class of 3-or-greater suggesting higher surgical risk when compared to their white counterparts (P<.001 for both). Analyses focusing on the THA cohort yielded similar findings.
Differences in unadjusted outcomes by sex
In analyses of unadjusted outcomes for TKA (Table 2), white women were significantly more likely to experience our composite outcome when compared to white men (16.5% and 14.1%; P<.001) and black women were significantly more likely to experience our composite outcome when compared to black men (18.3% and 14.3%; P=.002). The higher rate of the composite outcome in women as compared to men is almost entirely explained by higher rates of blood loss requiring transfusion in women (14.9% vs 12.2% for white women and white men, 16.4% vs 11.7% black women and men; P<.001 for both). Differences in other complications between men and women for TKA (e.g., pulmonary embolism, infection, renal failure) were minimal. Differences in hospital LOS for men as compared to women for TKA were small. However, white men and black men who underwent TKA were significantly less likely than white and black women to be discharged to a nursing home (P<.001 for both) and men were more likely to be readmitted to hospital within 30-days of surgery (P<.01 for both).
Table 2.
Incidence of selected outcomes within 30-days of surgery*
| TKA | THA | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| White Men (N=21900) | White Women (N=35530) | Black Men (N=1190) | Black Women (N=3455) | P-value | White Men (N=16167) | White Women (N=20330) | Black Men (N=1318) | Black Women (N=1519) | P-value | |
| Mortality, (%) | 38 (0.2) | 41 (0.1) | 0 (0.0) | 1 (0.0) | .044 | 31 (0.2) | 31 (0.2) | 3 (0.2) | 0 (0.0) | .294 |
| Pulmonary embolism, (%) | 120 (0.5) | 225 (0.6) | 15 (1.3) | 38 (1.1) | <.001 | 32 (0.2) | 47 (0.2) | 5 (0.4) | 6 (0.4) | .281 |
| Wound infection, (%) | 147 (0.7) | 233 (0.7) | 12 (1) | 15 (0.4) | .175 | 139 (0.9) | 175 (0.9) | 16 (1.2) | 18 (1.2) | .382 |
| Sepsis, number, (%) | 80 (0.4) | 75 (0.2) | 7 (0.6) | 13 (0.4) | .001 | 66 (0.4) | 64 (0.3) | 4 (0.3) | 12 (0.8) | .0211 |
| Bleeding requiring transfusion, (%) | 2674 (12.2) | 5292 (14.9) | 139 (11.7) | 567 (16.4) | <.001 | 1850 (11.4) | 4126 (20.3) | 171 (13) | 383 (25.2) | <.001 |
| Myocardial Infarction, (%) | 99 (0.5) | 86 (0.2) | 1 (0.1) | 12 (0.3) | <.001 | 58 (0.4) | 51 (0.3) | 4 (0.3) | 4 (0.3) | .308 |
| Pneumonia, number, (%) | 91 (0.4) | 102 (0.3) | 3 (0.3) | 14 (0.4) | .061 | 61 (0.4) | 62 (0.3) | 8 (0.6) | 6 (0.4) | .248 |
| Renal failure, number, (%) | 24 (0.1) | 20 (0.1) | 1 (0.1) | 3 (0.1) | .169 | 14 (0.1) | 5 (0.0) | 1 (0.1) | 2 (0.1) | .047 |
| Composite outcome, (%) | 3088 (14.1) | 5845 (16.5) | 170 (14.3) | 631 (18.3) | <.001 | 2117 (13.1) | 4380 (21.5) | 197 (14.9) | 406 (26.7) | <.001 |
| Composite outcome without bleeding, (%) | 500 (2.3) | 696 (2) | 36 (3) | 85 (2.5) | .003 | 344 (2.1) | 371 (1.8) | 34 (2.6) | 40 (2.6) | .020 |
| Hospital length-of-stay, mean (SD) | 3.1 (3.3) | 3.2 (4.1) | 3.2 (1.5) | 3.3 (1.5) | <.001 | 2.9 (4.6) | 3.2 (4.7) | 3.3 (3.7) | 3.4 (2.1) | <.001 |
| White Men (N=19759) | White Women (N=31956) | Black Men (N=1082) | Black Women (N=3118) | White Men (N=14845) | White Women (N=18562) | Black Men (N=1215) | Black Women (N=1385) | |||
| Discharge to nursing home or skilled care, (%) | 3268 (16.5) | 7998 (25.0) | 204 (18.9) | 879 (28.2) | <.001 | 2002 (12.4) | 4297 (21.1) | 197 (14.9) | 357 (23.5) | <.001 |
| Readmission within 30-days of surgery, (%) | 865 (4.4) | 1031 (3.2) | 63 (5.8) | 111 (3.6) | <.001 | 559 (3.8) | 684 (3.7) | 42 (3.5) | 65 (4.7) | .269 |
Discharge destination and readmission limited to patients who underwent procedures in 2011– 2013 when these variables became available in the NSQIP PUF.
Differences in unadjusted outcomes by race
In analyses of TKA unadjusted outcomes (Table 2) focusing on patient race, the incidence of our composite outcome was similar for white men and black men (14.1% and 14.3%; P=.89) but lower for white women compared to black women (16.5% and 18.3%; P=.007). White men had slightly higher incidence of both death and myocardial infarction compared to black men for TKA though these differences were not statistically significant (P=.19 and .26 respectively). White women hand slightly lower incidence of pulmonary embolism and bleeding compared to black women (P<.001 for both). White men and white women were less likely to be discharged to a nursing home or skilled care than black men and black women (16.5% vs 18.9% for white and black men; P=.05: 25.0% vs 28.2%; P<.001 for white and black women). Hospital readmission within 30-days of TKA was more common for blacks when compared to whites of the same sex. Unadjusted results for THA were generally similar.
Differences in adjusted outcomes by sex
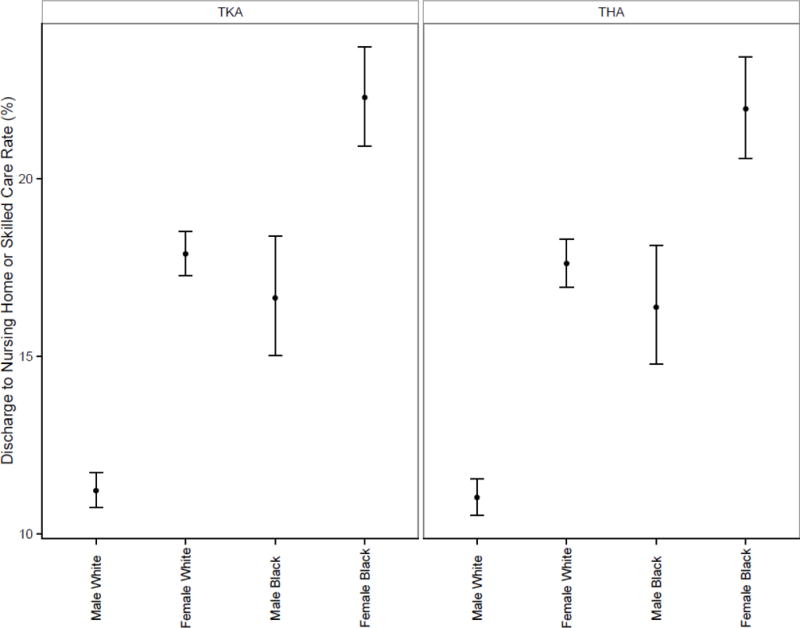
In adjusted analyses (Table 3 and Figure 2) white men and black men had significantly lower incidence of the composite outcome than women for both TKA and THA. Interestingly, men no longer had lower complication rates than women when receipt of transfusion was removed from our composite outcome (Table 3 and Figure 3). Moreover, differences in transfusion rates between men and women were no longer statistically significant in models that adjusted for pre-operative hematocrit levels. White men and black men were significantly less likely to be discharged to a nursing home or skilled care after TKA or THA (Table 3 and Figure 4) when compared to women of the same race; white men and black men were less likely to be readmitted to hospital when compared to women of the same race (Table 3), though the results were not all statistically significant.
Table 3.
Risk-standardized rates of adverse outcomes
| TKA | THA | ||
|---|---|---|---|
| Composite Outcome | Group | Estimate, 95%CI | Estimate, 95%CI |
| Male, White | 4.57 (4.24–4.92) | 5.35 (4.97–5.77) | |
| Female, White | 6.48 (6.05–6.94) | 7.57 (7.06–8.11) | |
| Male, Black | 5.18 (4.55–5.88) | 6.06 (5.33–6.88) | |
| Female, Black | 8.33 (7.59–9.13) | 9.7 (8.84–10.63) | |
| Composite Outcome, excluding bleeding | Male, White | 1.23 (1.08–1.4) | 1.26 (1.1–1.44) |
| Female, White | 1.05 (0.93–1.19) | 1.07 (0.94–1.22) | |
| Male, Black | 1.50 (1.14–1.95) | 1.52 (1.17–1.99) | |
| Female, Black | 1.22 (0.99–1.51) | 1.24 (1.00–1.55) | |
| Discharge to nursing home or skilled care* | Male, White | 11.22 (10.74–11.72) | 11.03 (10.53–11.56) |
| Female, White | 17.88 (17.26–18.51) | 17.61 (16.94–18.29) | |
| Male, Black | 16.64 (15.02–18.39) | 16.38 (14.78–18.12) | |
| Female, Black | 22.28 (20.91–23.7) | 21.96 (20.56–23.41) | |
| Readmission* within 30-days of surgery | Male, White | 2.21 (1.97–2.46) | 2.41 (2.15–2.71) |
| Female, White | 1.75 (1.57–1.94) | 1.91 (1.71–2.14) | |
| Male, Black | 2.28 (1.79–2.91) | 2.5 (1.96–3.19) | |
| Female, Black | 1.95 (1.61–2.36) | 2.13 (1.75–2.6) |
Discharge destination and readmission limited to patients who underwent procedures in 2011– 2013 when these variables became available in the NSQIP PUF.
Figure 2.
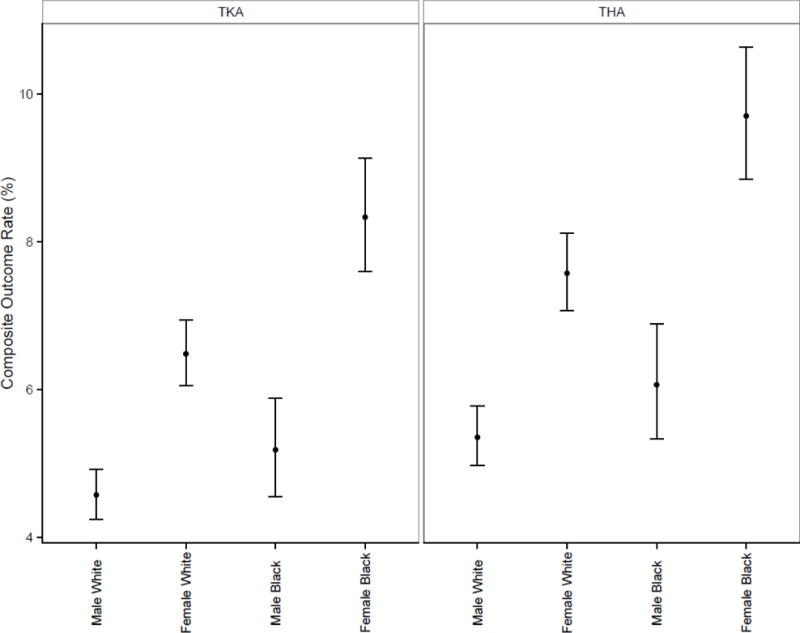
Figure 3.
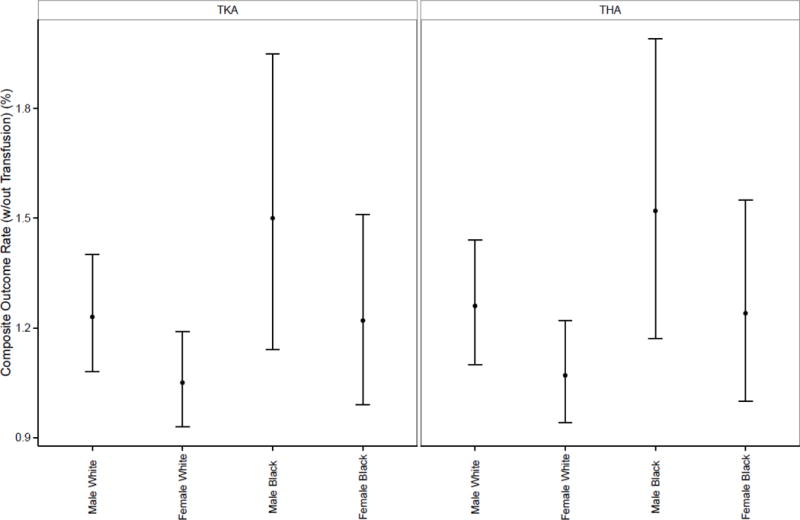
Figure 4.
Differences in adjusted outcomes by race
In adjusted outcomes focusing on race (Table 3 and Figure 2), white men and black men had statistically similar rates of the composite outcome for both TKA and THA; alternatively, white women had lower complication rates than black women for both TKA and THA.
In adjusted analyses for both TKA and THA white men and white women were both less likely to be discharged to a nursing home when compared to blacks (Table 3 and Figure 4). Readmission rates were generally similar for white men compared to black men and white women compared to black women for both TKA and THA (Table 3).
Discussion
In an analysis of data from the ACS-NSQIP registry, we examined disparities in TJA outcomes by sex and by race for white men, white women, black men, and black women. We found that differences in surgical complication rates between whites and blacks of the same sex were small. Alternatively, we found significantly higher incidence of complications for women when compared to men of the same race, but these sex-based differences were explained by higher rates of blood transfusions among women. We also found marked differences in the percentage of patients who were discharged to a nursing home after hospitalization with the lowest percentage for white men and the highest percentage for black women.
Several of our findings warrant discussion. First, we will discuss the differences that we found with respect to surgical complications. We found little evidence of racial disparities (or differences) in complication rates for TKA or THA for blacks as compared to whites of the same sex, particularly in adjusted analyses. Our findings of generally similar complication rates among blacks and whites differ somewhat from prior research which has generally shown higher complication rates among blacks. (10, 12, 14) Prior research on racial disparities in TKA and THA outcomes has often used administrative data and thus may lack the nuance and detail of the NSQIP registry; this may explain some of the differences between our research and prior findings. (10) Alternatively, hospitals participating in the NSQIP registry are self-selected and are known to differ from hospitals that do not participate; thus differences between our study and prior research may reflect difference between the hospitals included in our analysis and prior research. (21) Either way, our results are modestly encouraging by demonstrating similar outcomes for whites and blacks who underwent TKA or THA in hospitals participating in NSQIP.
Alternatively, we found larger disparities when looking at disparities through the lens of patient sex. White women and black women had markedly higher complication rates than their male counterparts but these differences were driven almost entirely by higher rates of blood transfusions among women. In turn, higher transfusion rates for women were entirely explained by differences in baseline hematocrit. In recent years transfusion guidelines have recommended progressively lower thresholds at which transfusion should be initiated based upon data that excessive blood transfusions can cause harm. (29) Such guidelines do not provide separate transfusion thresholds for men and women despite the fact that women tend to have lower baseline hemoglobin levels. (30) Interestingly, there are relatively few studies describing differences in rates of blood transfusions by patient race or sex. (31, 32) Our study suggests that women are being transfused more often than men after TJA; if our results were confirmed in subsequent studies, it might be reasonable to consider whether sex-specific transfusion thresholds might be warranted.
Second, it is important to comment on the differences we observed in percentages of patients discharged to nursing homes after hospitalization; specifically, black women were most likely followed by white women, black men, and finally white men. Prior studies have reported that anywhere from 30%–50% of TJA patients in the US are discharged to inpatient rehabilitation and/or nursing homes, (23, 33) with lower rates in Canada. (34) The disparities literature with respect to discharge disposition after TJA is extremely limited, but supports our findings of blacks being more likely to be discharge to nursing homes when compared to whites. (10) A clinical prediction rule designed to guide choice of discharge disposition after TJA – the RAPT score- explicitly recognizes that female sex is a risk-factor for patient’s being unable to return home after surgery. (35) Women tend to undergo TKA and THA at an older age when compared to men; thus, age and frailty are likely part of the explanation for why women are more likely to require post-acute care after TJA. In addition, women undergoing TJA are more likely to be living alone at the time of their surgery, having been predeceased by their husbands; thus women are less likely to have a partner living in the home to assist in post-operative recovery. (36)
Third, it is important to comment upon our findings with respect to readmission rates. In unadjusted analyses we found that readmission rates were higher for blacks (compared to whites of the same sex) and women (compared to men of the same race). Our findings of higher unadjusted readmission rates for blacks generally reinforces prior studies, (37, 38) though our finding of higher readmission rates for men is somewhat new. When considering the higher readmission rate for men, it is interesting note that men may be more likely to be readmitted because men are more likely to be discharged home after surgery; conversely, since women are more likely to be discharged to skilled care, the opportunity for readmission may be reduced. It might be reasonable to consider enhanced post-discharge follow-up care (e.g., visiting home-health aids) particularly for patients who are being discharged home under the care of an often elderly spouse or partner as part of efforts to reduce hospital readmissions.
A number of other findings warrant brief mention. Our finding that the overall risk of surgical complication within 30-days of TJA was approximately 3% after excluding the need for transfusion is consistent with prior studies and reinforces the safety of TJA. Alternatively, the finding that more than 25% of women and 15% of men were discharged to a nursing home or skilled care is a reminder that TJA recovery time is often protracted.
Our study has a number of limitations that warrant mention. First, it is important to note that hospitals participating in NSQIP tend to be large academic hospitals and are not be representative of all US hospitals where TJA is performed. Second, we lack information on patient reported outcomes such as pain and ambulation which are key outcomes for TKA and THA. Third, the PUF files lack both hospital and physician identifiers; thus, we were unable to account for clustering of patients within hospitals or hospital or physician volume in our analyses. Fourth, we lacked information on complications occurring greater than 30-days after surgery.
In conclusion, among NSQIP participants, we found similar complication rates after TKA and THA for whites and blacks and little in the way of racial disparities. While women had markedly higher complication rates than men, differences were driven almost entirely by higher rates of blood transfusion in women. Finally, we found marked differences in the percentages of patients requiring discharge to nursing homes after surgery, likely reflecting differences in support available at home after surgery.
Acknowledgments
Funding/Support: Dr. Cram is supported by a K24 AR062133 award from NIAMS at the NIH.
Role of the Sponsor: Neither NIH nor any other external agencies had any role in the design and conduct of the study; collection, management, analysis, and interpretation of data; preparation, review, or approval of the manuscript; or, decision to submit the manuscript for publication.
Footnotes
Author Contributions: Cram and Matelski had full access to all the data in the study. Dr Cram takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Cram, Hawker, Ravi, Gandhi, Jackson
Acquisition of data: Cram, Matelski, Jackson
Analysis and interpretation of data: Cram, Matelski, Hawker, Ravi, Gandhi, Jackson
Drafting of the manuscript: Cram, Matelski, Hawker, Ravi, Pugely, Gandhi, Jackson
Critical revision of the manuscript: Cram, Matelski, Hawker, Ravi, Pugely, Gandhi, Jackson
Statistical analysis: Cram, Matelski
Obtained funding: Cram, Jackson
Conflict of Interest: Drs. Cram, Matelski, Hawker, Ravi, Pugely, and Jackson have nothing to disclose. Dr. Gandhi reports that his employer receives grant funding from Biomet and Smith and Nephew.
References
- 1.Smedley BD, Stith AY, Nelson AR, editors. Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, D.C.: National Academies Press; 2003. [PubMed] [Google Scholar]
- 2.Cooke CR, Nallamothu B, Kahn JM, Birkmeyer JD, Iwashyna TJ. Race and timeliness of transfer for revascularization in patients with acute myocardial infarction. Med Care. 2011;49(7):662–7. doi: 10.1097/MLR.0b013e31821d98b2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fraenkel L, Suter L, Weis L, Hawker GA. Variability in recommendations for total knee arthroplasty among rheumatologists and orthopedic surgeons. J Rheumatol. 2014;41(1):47–52. doi: 10.3899/jrheum.130762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Borkhoff CM, Hawker GA, Kreder HJ, Glazier RH, Mahomed NN, Wright JG. The effect of patients’ sex on physicians’ recommendations for total knee arthroplasty. Cmaj. 2008;178(6):681–7. doi: 10.1503/cmaj.071168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blum MA, Ibrahim SA. Race/ethnicity and use of elective joint replacement in the management of end-stage knee/hip osteoarthritis: a review of the literature. Clin Geriatr Med. 2012;28(3):521–32. doi: 10.1016/j.cger.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 6.Mota RE, Tarricone R, Ciani O, Bridges JF, Drummond M. Determinants of demand for total hip and knee arthroplasty: a systematic literature review. BMC Health Serv Res. 2012;12:225. doi: 10.1186/1472-6963-12-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schneider EC, Leape LL, Weissman JS, Piana RN, Gatsonis C, Epstein AM. Racial differences in cardiac revascularization rates: does “overuse” explain higher rates among white patients? Annals of Internal Medicine. 2001;135(5):328–37. doi: 10.7326/0003-4819-135-5-200109040-00009. [DOI] [PubMed] [Google Scholar]
- 8.Moylan CA, Brady CW, Johnson JL, Smith AD, Tuttle-Newhall JE, Muir AJ. Disparities in liver transplantation before and after introduction of the MELD score. Jama. 2008;300(20):2371–8. doi: 10.1001/jama.2008.720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Skinner J, Weinstein JN, Sporer SM, Wennberg JE. Racial, ethnic, and geographic disparities in rates of knee arthroplasty among Medicare patients. N Engl J Med. 2003;349(14):1350–9. doi: 10.1056/NEJMsa021569. [DOI] [PubMed] [Google Scholar]
- 10.Singh JA, Lu X, Rosenthal GE, Ibrahim S, Cram P. Racial disparities in knee and hip total joint arthroplasty: an 18-year analysis of national Medicare data. Ann Rheum Dis. 2014;73(12):2107–15. doi: 10.1136/annrheumdis-2013-203494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Borkhoff CM, Hawker GA, Kreder HJ, Glazier RH, Mahomed NN, Wright JG. Influence of patients’ gender on informed decision making regarding total knee arthroplasty. Arthritis Care Res (Hoboken) 2013;65(8):1281–90. doi: 10.1002/acr.21970. [DOI] [PubMed] [Google Scholar]
- 12.Ibrahim SA, Stone RA, Han X, Cohen P, Fine MJ, Henderson WG, et al. Racial/ethnic differences in surgical outcomes in veterans following knee or hip arthroplasty. Arthritis Rheum. 2005;52(10):3143–51. doi: 10.1002/art.21304. [DOI] [PubMed] [Google Scholar]
- 13.Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR. Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991–2010. JAMA. 2012;308(12):1227–36. doi: 10.1001/2012.jama.11153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cai X, Cram P, Vaughan-Sarrazin M. Are African American patients more likely to receive a total knee arthroplasty in a low-quality hospital? Clin Orthop Relat Res. 2012;470(4):1185–93. doi: 10.1007/s11999-011-2032-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bozic KJ, Grosso LM, Lin Z, Parzynski CS, Suter LG, Krumholz HM, et al. Variation in hospital-level risk-standardized complication rates following elective primary total hip and knee arthroplasty. J Bone Joint Surg Am. 2014;96(8):640–7. doi: 10.2106/JBJS.L.01639. [DOI] [PubMed] [Google Scholar]
- 16.Kamath AF, Horneff JG, Gaffney V, Israelite CL, Nelson CL. Ethnic and gender differences in the functional disparities after primary total knee arthroplasty. Clin Orthop Relat Res. 2010;468(12):3355–61. doi: 10.1007/s11999-010-1461-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Novicoff WM, Saleh KJ. Examining sex and gender disparities in total joint arthroplasty. Clin Orthop Relat Res. 2011;469(7):1824–8. doi: 10.1007/s11999-010-1765-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liebs TR, Herzberg W, Roth-Kroeger AM, Ruther W, Hassenpflug J. Women recover faster than men after standard knee arthroplasty. Clin Orthop Relat Res. 2011;469(10):2855–65. doi: 10.1007/s11999-011-1921-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cohen ME, Ko CY, Bilimoria KY, Zhou L, Huffman K, Wang X, et al. Optimizing ACS NSQIP modeling for evaluation of surgical quality and risk: patient risk adjustment, procedure mix adjustment, shrinkage adjustment, and surgical focus. J Am Coll Surg. 2013;217(2):336–46 e1. doi: 10.1016/j.jamcollsurg.2013.02.027. [DOI] [PubMed] [Google Scholar]
- 20.surgeons. Aco;PagesAvailable at: https://www.facs.org/quality-programs/acs-nsqip [Accessed October 3, 2015]
- 21.Osborne NH, Nicholas LH, Ryan AM, Thumma JR, Dimick JB. Association of hospital participation in a quality reporting program with surgical outcomes and expenditures for Medicare beneficiaries. Jama. 2015;313(5):496–504. doi: 10.1001/jama.2015.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.surgeons. Aco;PagesAvailable at: https://www.facs.org/~/media/files/quality%20programs/nsqip/acs_nsqip_puf_user_guide_2013.ashx[Accessed October 5, 2015]
- 23.Cram P, Lu X, Kaboli PJ, Vaughan-Sarrazin MS, Cai X, Wolf BR, et al. Clinical characteristics and outcomes of Medicare patients undergoing total hip arthroplasty, 1991–2008. JAMA. 2011;305(15):1560–7. doi: 10.1001/jama.2011.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Centers for Medicare and medicaid Innovation (CMMI) CMMI Comprehensive Care for Joint Replacement Model: Quality Measures, Voluntary Data, Public Reporting Processes for Preview Reports. Washington, DC: Center for Medicare and Medicaid Services (CMS); 2015. [Google Scholar]
- 25.Wolf BR, Lu X, Li Y, Callaghan JJ, Cram P. Adverse outcomes in hip arthroplasty: long-term trends. J Bone Joint Surg Am. 2012;94(14):e1038. doi: 10.2106/JBJS.K.00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Agresti A. Categorical Data Analysis. New York, NY: John Wiley and Sons, Inc; 1990. [Google Scholar]
- 27.Guolo A. A double SIMEX approach for bivariate random-effects meta-analysis of diagnostic accuracy studies. BMC Med Res Methodol. 2017;17(1):6. doi: 10.1186/s12874-016-0284-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jiang Y, Guarino P, Ma S, Simon S, Mayo MS, Raghavan R, et al. Bayesian accrual prediction for interim review of clinical studies: open source R package and smartphone application. Trials. 2016;17(1):336. doi: 10.1186/s13063-016-1457-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carson JL, Grossman BJ, Kleinman S, Tinmouth AT, Marques MB, Fung MK, et al. Red blood cell transfusion: a clinical practice guideline from the AABB*. Ann Intern Med. 2012;157(1):49–58. doi: 10.7326/0003-4819-157-1-201206190-00429. [DOI] [PubMed] [Google Scholar]
- 30.Alghamdi AA, Davis A, Brister S, Corey P, Logan A. Development and validation of Transfusion Risk Understanding Scoring Tool (TRUST) to stratify cardiac surgery patients according to their blood transfusion needs. Transfusion. 2006;46(7):1120–9. doi: 10.1111/j.1537-2995.2006.00860.x. [DOI] [PubMed] [Google Scholar]
- 31.Wall PL, Glawe BJ, Sahr SM, Baker JL, Leib CJ, Renner CH, et al. Gender differences in blood transfusions after trauma related to ages and mechanisms. Am Surg. 2014;80(5):E141–3. [PubMed] [Google Scholar]
- 32.Menendez ME, Ring D. Minorities are less likely to receive autologous blood transfusion for major elective orthopaedic surgery. Clin Orthop Relat Res. 2014;472(11):3559–66. doi: 10.1007/s11999-014-3793-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jain NB, Higgins LD, Ozumba D, Guller U, Cronin M, Pietrobon R, et al. Trends in epidemiology of knee arthroplasty in the United States, 1990–2000. Arthritis and Rheumatism. 2005;52(12):3928–33. doi: 10.1002/art.21420. [DOI] [PubMed] [Google Scholar]
- 34.Hart A, Bergeron SG, Epure L, Huk O, Zukor D, Antoniou J. Comparison of US and Canadian Perioperative Outcomes and Hospital Efficiency After Total Hip and Knee Arthroplasty. JAMA Surg. 2015 doi: 10.1001/jamasurg.2015.1239. [DOI] [PubMed] [Google Scholar]
- 35.Oldmeadow LB, McBurney H, Robertson VJ. Predicting risk of extended inpatient rehabilitation after hip or knee arthroplasty. J Arthroplasty. 2003;18(6):775–9. doi: 10.1016/s0883-5403(03)00151-7. [DOI] [PubMed] [Google Scholar]
- 36.Mahomed NN, Davis AM, Hawker G, Badley E, Davey JR, Syed KA, et al. Inpatient compared with home-based rehabilitation following primary unilateral total hip or knee replacement: a randomized controlled trial. J Bone Joint Surg Am. 2008;90(8):1673–80. doi: 10.2106/JBJS.G.01108. [DOI] [PubMed] [Google Scholar]
- 37.Li Y, Cai X, Glance LG. Disparities in 30-Day Rehospitalization Rates Among Medicare Skilled Nursing Facility Residents by Race and Site of Care. Med Care. 2015;53(12):1058–65. doi: 10.1097/MLR.0000000000000441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tsai TC, Orav EJ, Joynt KE. Disparities in surgical 30-day readmission rates for Medicare beneficiaries by race and site of care. Ann Surg. 2014;259(6):1086–90. doi: 10.1097/SLA.0000000000000326. [DOI] [PMC free article] [PubMed] [Google Scholar]


