Abstract
Purpose
While education-based disparities in health are common, the extent to which chronic conditions contribute to education gaps and to consequent health disparities is not fully understood. As such, we sought to investigate educational aspirations, expectations, and attainment among youth with and without chronic conditions, and to determine if these relationships mediated subsequent disparities in health and wellbeing.
Methods
Longitudinal data on 3518 youth are from the 1997–2013 Panel Study of Income Dynamics (PSID), a population-based survey. Multivariate regression was used to assess disparities in educational aspirations, expectations, and attainment by chronic conditions and the subsequent effects on health and wellbeing, adjusting for important potential confounders.
Results
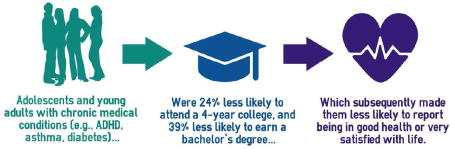
Youth with chronic medical conditions (YCMC) did not report significantly lower educational aspirations than their healthy peers; however, YCMC reported lower expectations for their educational attainment and fewer YCMC had earned their desired degree by the end of follow-up (e.g., ≥bachelor’s degree: 19.9% for YCMC vs 26.0% for peers, p<0.05). YCMC reported significantly worse general health, lower life satisfaction, and lower psychological wellbeing in young adulthood than did their healthy peers. These disparities persisted after adjustment for confounders; the association between chronic disease and health was partially, but significantly, mediated by actual educational attainment.
Conclusions
Findings suggest an important risk mechanism through which YCMC may acquire socioeconomic disadvantage as they develop and progress through educational settings. Disproportionate lags in education, from expectation to attainment, may in turn increase YCMC’s susceptibility to poor health and wellbeing in the future.
Keywords: Adolescent, Young Adult, Education, Educational Activities, Educational Attainment, Chronic Disease, Health, Wellbeing, Resilience, Psychological
Graphical Abstract
Introduction
The prevalence of pediatric-onset chronic medical conditions, such as type 1 diabetes and asthma, has been steadily rising over the past several decades, leading to an unprecedented number of youth, over 1-in-4, who must manage their condition1 and cope with the associated financial and psychosocial burdens.2 For youth with chronic medical conditions (YCMC), disease burden may interfere with normal developmental processes and negatively affect near-term as well as subsequent health and wellbeing. While psychosocial and health decrements are commonly observed among YCMC during emergent adulthood,3–10 mechanisms are unclear.
Life-course theory and a multiple determinants of health model highlight the importance of considering the dynamic circumstances and developing socioeconomic contexts bearing on youth as they mature into adulthood.11–13 Educational attainment, a critical component of socioeconomic status, has been shown to affect several health outcomes.14–16 Education-based gradients in health likely operate by affecting individuals’ ability to obtain and apply health-related knowledge, access health services, and regulate exposure to various health risks, all of which are especially critical for successful disease self-management among YCMC.17,18 There is some evidence to suggest that YCMC may experience gaps in educational attainment,19,20 although there is a paucity of evidence about longitudinal processes linking chronic disease, education (from aspirations to attainment), and health.
To address this gap, we sought to quantify disparities in educational aspirations, expectations, and attainment as they manifest longitudinally among adolescents and young adults with and without chronic conditions; we further sought to determine if disparities in educational attainment in adolescence mediate subsequent disparities in health and wellbeing during emergent adulthood. If empirically validated, this model might help explain why ‘down-stream’ adverse health outcomes are common among YCMC during emergent adulthood and guide the design and application of supportive interventions targeting ‘upstream’ causes during adolescence.
Methods
Data Source and Sample
Data are from the Panel Study of Income Dynamics (PSID), a nationally representative, longitudinal household survey. In 1997, children from birth to age 12 years residing in PSID households were recruited into the Child Development Supplement (CDS); repeat waves of the CDS were administered in 2002/3 and 2007/8. CDS participants who graduated or dropped out of high school and were at least 18 years old were interviewed for the Transition into Adulthood (TA) survey in 2005, 2007, 2009, 2011, and 2013. Respondents were eligible for this study if they were interviewed in the initial 1997 CDS wave and responded to questions about educational and health outcomes in a subsequent interview (N=2555); additionally, another 963 CDS respondents had a parent or self-report of educational aspirations or expectations and were also included in analyses for those outcomes. As data were already collected and de-identified, this study was exempted from IRB approval.
Dependent Variables
Educational Outcomes
Both parents and youth reported on educational preferences/aspirations (respectively) and expectations in the CDS when youth were <18, and youth further reported on these outcomes in the TA. In the CDS, parents reported their preferences (“In the best of all worlds, how much schooling would you like [your child] to complete?”) and expectations (“Sometimes children do not get as much education as we would like. How much schooling do you expect that [your child] will really complete?”), regarding their child’s educational attainment. In the CDS and TA, youth (ages 12 and older) reported their aspirations (“How far would you like to go in school?”) and expectations (“Many people do not get as much education as they would like. How far do you think you will actually go in school?”) for their own educational attainment. These outcomes were classified as follows: 1) Graduate from high school or less; 2) Post-high school vocational training or some college; 3) Graduate from a 2-year college; 4) Graduate from a 4-year college; 5) Earn a graduate degree (e.g., Master’s, MD, JD, PhD); or 6) Don’t know (youth respondents could additionally report wanting to “do something else”).
Youth’s self-reported educational attainment (including college enrollment status, receipt of academic degrees, and dates of matriculation and completion) was assessed at each TA administration and used to construct time-varying summary variables for attainment (Did not graduate from high school or earn a GED; Graduated from high school or earned a GED; Post-high school vocational training or some college; Graduated from a 2-year college; Graduated from 4-year college; or Any graduate school), and conditional indicators of academic progression (e.g., matriculation into a 4-year college among anyone with a high school degree/GED; completion of a bachelor’s degree among anyone who attended a 4-year college).
Health & Wellbeing
Health status was measured as an ordinal variable using Likert-type responses from the following question: “Would you say your health in general is excellent, very good, good, fair, or poor?” A continuous measure for psychological wellbeing was constructed by reverse coding Kessler-6 psychological distress scores.21 In the 2009–2013 administrations of the TA, respondents were asked to rate their life satisfaction on a Likert-scale: “How satisfied are you with [your life-as-a-whole]? Are you completely satisfied, very satisfied, somewhat satisfied, not very satisfied, or not at all satisfied?”
Independent Variables
Chronic Medical Conditions
Chronic conditions were conceptualized as those requiring regular, lifelong medical management with onset in childhood, and identified by report of ever being told by a doctor or other health professional that they had: ADHD/ADD; asthma; autism; birth defects; breathing problems; cancer; chronic hypertension (reported ≥2 times); diabetes; digestive problems; emotional or psychological problems; epilepsy; heart conditions; kidney disease; learning disability or developmental delays; migraines; orthopedic conditions; sickle cell anemia; skin disease; hearing, speech, or visual impairments; and other conditions. Youth who did not report any of the aforementioned chronic conditions or reported only acute or episodic conditions (e.g., allergies; jaundice) were considered to have no chronic conditions. Youth with a reported diagnosis of intellectual disability were excluded.
Reported age of diagnosis for each condition (or age at first report of each condition when age was missing) was used to construct time-varying indicators of chronic condition status at each follow-up survey. For descriptive purposes (i.e., Table 1), a summary of chronic condition status based on age of first diagnosis was used (any chronic condition diagnosed ≤14 years of age; any chronic condition diagnosed >14 years of age; no chronic conditions).
Table 1.
Cross-Sectional Associations between Sociodemographic Characteristics, Educational Attainment, and Health Status
| Chronic Condition Statusa | Highest Educational Attainmenta | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total | Dx ≤ 14 | Dx > 14 | None | p-val | Total | ≥BA/BS | College | ≤ HS | p-val | |
| Total N (unweighted) | 3,518 | 1,729 | 384 | 1,405 | 2,555 | 453 | 1,520 | 582 | ||
| Total % (weighted) | 50.0% | 11.5% | 38.5% | 21.9% | 58.2% | 20.0% | ||||
| Youth’s Age in 1997 | <0.001 | <0.001 | ||||||||
| Mean | 6.28 | 6.22 | 8.09 | 5.81 | 7.42 | 9.58 | 6.75 | 7.00 | ||
| Standard Deviation | 3.78 | 3.64 | 2.90 | 4.03 | 3.25 | 1.85 | 3.28 | 3.53 | ||
| Youth’s Age at Last Follow-Up | <0.001 | <0.001 | ||||||||
| Mean | 19.74 | 20.32 | 23.98 | 17.73 | 23.51 | 25.73 | 22.88 | 22.90 | ||
| Standard Deviation | 6.83 | 6.13 | 2.84 | 7.83 | 2.88 | 1.38 | 2.85 | 3.16 | ||
| Sex | <0.001 | 0.001 | ||||||||
| Female | 49.9% | 42.4% | 66.2% | 54.7% | 51.4% | 56.9% | 52.6% | 41.7% | ||
| Male | 50.1% | 57.6% | 33.8% | 45.3% | 48.6% | 43.1% | 47.4% | 58.3% | ||
| Race/Ethnicity | 0.049 | <0.001 | ||||||||
| White, non-Hispanic | 58.5% | 59.4% | 60.8% | 56.6% | 55.7% | 69.5% | 54.3% | 44.8% | ||
| Black, non-Hispanic | 14.6% | 14.9% | 10.5% | 15.4% | 14.9% | 7.4% | 14.5% | 24.3% | ||
| Asian, non-Hispanic | 3.3% | 2.3% | 2.5% | 4.9% | 3.4% | 5.0% | 2.9% | 2.8% | ||
| Other, non-Hispanic | 6.4% | 7.2% | 6.4% | 5.3% | 7.7% | 5.4% | 8.5% | 8.0% | ||
| Hispanic | 17.2% | 16.2% | 19.9% | 17.8% | 18.3% | 12.7% | 19.8% | 20.1% | ||
| Prenatal WIC/AFDC Participation | 0.002 | <0.001 | ||||||||
| Yes | 32.8% | 36.5% | 26.8% | 29.8% | 31.1% | 9.7% | 30.3% | 56.7% | ||
| No | 67.2% | 63.5% | 73.2% | 70.2% | 68.9% | 90.3% | 69.7% | 43.3% | ||
| Parent’s Marital Status in 1997 | <0.001 | <0.001 | ||||||||
| Single Parent Household | 22.6% | 26.4% | 16.6% | 19.6% | 23.6% | 13.3% | 22.3% | 39.0% | ||
| Two Parent Household | 77.4% | 73.6% | 83.4% | 80.4% | 76.4% | 86.7% | 77.7% | 61.0% | ||
| Parental Education | 0.014 | <0.001 | ||||||||
| Less than high school/GED | 22.3% | 22.2% | 15.5% | 24.5% | 20.8% | 4.1% | 23.7% | 30.3% | ||
| High school graduate/GED | 23.9% | 24.6% | 24.2% | 22.8% | 22.7% | 10.0% | 22.3% | 37.9% | ||
| Some college | 20.3% | 20.4% | 17.5% | 21.0% | 18.5% | 14.2% | 19.9% | 19.3% | ||
| College graduate or more | 33.5% | 32.8% | 42.8% | 31.7% | 38.0% | 71.8% | 34.0% | 12.5% | ||
| Educational Outcomes | N= | |||||||||
| Actual Education Attainmenta | 2,555 | 0.001 | -- | |||||||
| Did not graduate high school/GED | 5.0% | 6.5% | 2.7% | 3.6% | ||||||
| Graduated high school/GED | 14.9% | 17.2% | 10.7% | 13.2% | ||||||
| Some college or vocational training | 50.7% | 50.0% | 53.7% | 50.2% | ||||||
| Earned an associate’s degree | 7.5% | 7.7% | 8.0% | 6.9% | ||||||
| Earned a bachelor’s degree | 13.4% | 12.0% | 12.5% | 16.0% | ||||||
| Any graduate school | 8.5% | 6.4% | 12.4% | 10.0% | ||||||
| Youth’s Highest Expectationsa | 2,807 | 0.030 | <0.001 | |||||||
| ≤Graduate high school/GED | 2.5% | 2.6% | 1.3% | 2.9% | 1.1% | 0.0% | 0.3% | 4.5% | ||
| Some college or vocational training | 6.3% | 7.1% | 3.8% | 6.2% | 5.3% | 0.0% | 3.6% | 16.1% | ||
| Earn an associate’s degree | 13.1% | 14.5% | 12.6% | 11.1% | 13.2% | 0.0% | 13.0% | 28.2% | ||
| Earn a bachelor’s degree | 35.9% | 35.7% | 33.5% | 37.4% | 36.1% | 16.3% | 42.9% | 38.0% | ||
| Earn a graduate degree | 40.9% | 39.0% | 48.7% | 40.7% | 43.6% | 83.7% | 40.0% | 10.4% | ||
| Don’t know/Do something else | 1.2% | 1.2% | 0.0% | 1.8% | 0.6% | 0.0% | 0.1% | 2.9% | ||
| Youth’s Highest Aspirationsa | 2,807 | 0.242 | <0.001 | |||||||
| ≤Graduate high school/GED | 2.2% | 2.1% | 1.2% | 2.7% | 1.1% | 0.0% | 0.2% | 4.8% | ||
| Some college or vocational training | 4.3% | 5.1% | 2.3% | 3.8% | 3.4% | 0.0% | 2.4% | 10.1% | ||
| Earn an associate’s degree | 8.9% | 9.3% | 9.5% | 7.8% | 8.7% | 0.0% | 8.0% | 20.4% | ||
| Earn a bachelor’s degree | 33.5% | 34.2% | 29.7% | 34.2% | 33.3% | 12.5% | 38.6% | 40.5% | ||
| Earn a graduate degree | 49.6% | 47.9% | 56.3% | 49.3% | 52.7% | 87.5% | 50.6% | 20.7% | ||
| Don’t know/Do something else | 1.6% | 1.4% | 1.0% | 2.1% | 0.8% | 0.0% | 0.2% | 3.5% | ||
| Parent’s Highest Expectationsa | 3,518 | <0.001 | <0.001 | |||||||
| ≤Graduate high school/GED | 10.2% | 12.8% | 5.9% | 8.1% | 9.7% | 1.9% | 6.7% | 27.1% | ||
| Some college or vocational training | 4.2% | 4.2% | 4.8% | 4.0% | 3.9% | 0.6% | 3.0% | 10.3% | ||
| Earn an associate’s degree | 5.7% | 6.0% | 5.2% | 5.5% | 5.4% | 2.2% | 5.5% | 8.8% | ||
| Earn a bachelor’s degree | 53.9% | 50.1% | 55.3% | 58.6% | 53.5% | 54.3% | 56.8% | 43.0% | ||
| Earn a graduate degree | 25.8% | 26.7% | 27.9% | 23.8% | 27.1% | 40.3% | 27.8% | 10.6% | ||
| Don’t know | 0.2% | 0.3% | 0.8% | 0.0% | 0.3% | 0.6% | 0.2% | 0.3% | ||
| Parent’s Highest Preferencea | 2,999 | 0.051 | <0.001 | |||||||
| ≤Graduate high school/GED | 4.9% | 5.9% | 3.8% | 3.7% | 5.0% | 1.9% | 2.4% | 16.0% | ||
| Some college or vocational training | 3.3% | 3.6% | 1.3% | 3.6% | 3.3% | 1.2% | 3.1% | 5.8% | ||
| Earn an associate’s degree | 4.1% | 4.7% | 4.0% | 3.4% | 4.6% | 1.6% | 3.7% | 10.1% | ||
| Earn a bachelor’s degree | 51.8% | 48.9% | 54.4% | 55.2% | 52.0% | 46.6% | 54.0% | 51.7% | ||
| Earn a graduate degree | 35.7% | 36.9% | 36.1% | 33.8% | 35.1% | 48.8% | 36.5% | 16.3% | ||
| Unsure | 0.1% | 0.0% | 0.3% | 0.3% | 0.1% | 0.0% | 0.2% | 0.0% | ||
| Health & Wellbeing Outcomes | N= | |||||||||
| Health Statusa | 2,555 | <0.001 | <0.001 | |||||||
| Excellent | 22.3% | 19.5% | 18.3% | 28.8% | 22.3% | 30.7% | 19.9% | 20.1% | ||
| Very Good | 42.6% | 41.1% | 47.0% | 42.8% | 42.6% | 49.5% | 42.9% | 34.1% | ||
| Good | 26.8% | 29.4% | 23.4% | 24.1% | 26.8% | 16.0% | 28.9% | 32.3% | ||
| Fair | 7.4% | 8.5% | 10.1% | 4.2% | 7.4% | 3.8% | 7.1% | 12.2% | ||
| Poor | 1.0% | 1.5% | 1.2% | 0.0% | 1.0% | 0.0% | 1.2% | 1.3% | ||
| Life Satisfactiona | 2,483 | <0.001 | <0.001 | |||||||
| Completely satisfied | 17.7% | 19.2% | 11.1% | 18.5% | 17.7% | 17.7% | 18.1% | 16.6% | ||
| Very satisfied | 48.3% | 44.6% | 51.7% | 52.7% | 48.3% | 55.0% | 48.9% | 38.7% | ||
| Somewhat satisfied | 30.8% | 32.1% | 33.0% | 27.4% | 30.8% | 25.4% | 30.5% | 37.7% | ||
| Not very satisfied | 2.6% | 3.5% | 2.4% | 1.3% | 2.6% | 1.7% | 1.9% | 5.9% | ||
| Not at all satisfied | 0.6% | 0.6% | 1.8% | 0.1% | 0.6% | 0.2% | 0.6% | 1.2% | ||
| Psychological Wellbeinga | 2,555 | <0.001 | 0.002 | |||||||
| Mean | 19.15 | 18.83 | 18.67 | 19.94 | 19.15 | 19.63 | 19.20 | 18.52 | ||
| Standard Deviation | 3.68 | 3.79 | 3.72 | 3.27 | 3.70 | 2.83 | 3.70 | 4.56 | ||
Data are from the Panel Study of Income Dynamics, Child Development and Transition to Adulthood Supplements (1997–2013). Unweighted Ns and weighted percentages and means are presented.
Note that cross-sectional summaries of longitudinal/time-varying variables are presented and do not reflect the full distribution of responses across multiple assessments.
To assess if specific conditions demonstrated differential relationships with the dependent variables under investigation, we replicated analyses using four (non-mutually exclusive) chronic condition summary variables: 1) any emotional or psychological problems; 2) any learning disability, developmental delay, autism, or ADHD/ADD; 3) any sensory impairment (i.e., hearing, speech, or visual impairments); and 4) any of the other major medical conditions. We also investigated major medical conditions in (4) with an accompanying major activity limitation, defined by reports in the TA that selected conditions limit “normal daily activities” either “a lot” or “somewhat;” this follow-up limitation question was only asked for some conditions hence it may underestimate the prevalence of individuals with a limitation-causing condition.
Sociodemographic Factors
Data on child sociodemographic factors included: age (at each survey administration, treated as a time-varying covariate), sex (male vs female), and race/ethnicity (Hispanic; White, non-Hispanic; Black, non-Hispanic; Asian, non-Hispanic; Other, non-Hispanic). Several indicators of childhood socioeconomic status were constructed, including: 1) whether the mother participated in Women, Infants, and Children (WIC) or Aid to Families with Dependent Children (AFDC) programs during pregnancy; 2) whether or not both parents were present in the household in 1997; and 3) the highest educational attainment for either parent (less than high school degree/GED; high school degree or GED; some college or vocational school; and college graduate or beyond).
Statistical Analyses
Analyses were conducted using survey procedures from SAS version 9.4 (Cary, NC). The standard errors were corrected due to clustering within strata and the primary sampling unit, and PSID sampling weights were used to account for both attrition and the unequal household selection probabilities from the original PSID sampling frame. Statistical significance was considered at p<0.05.
Summary statistics were generated to describe sample characteristics; chi-square and Kruskall-Wallis tests were used to determine significant differences in sociodemographic characteristics by chronic condition status and by highest reported educational attainment (among youth interviewed in the TA). Multivariate generalized linear mixed models (GLMM) were used to account for the correlated nature of the data (given repeated measures over 10+ years of follow-up). Educational outcomes were modeled using GLMM with a multinomial distribution and generalized logit link function, where the odds of each level of educational attainment is compared against (≤) high school graduate/GED as the reference. General health and life satisfaction were treated as ordinal variables (higher values indicate better health, greater satisfaction) and modeled with a cumulative logit link function; psychological wellbeing was modeled with a Gaussian distribution.
Mediation of disparities by chronic condition status was evaluated with stepwise regression and application of the Sobel test.22 First, models adjusting only for age and chronic condition status were run (Model 1), followed by models additionally adjusting for sex, race/ethnicity, WIC/AFDC participation during pregnancy, parent marital status at baseline, and parental educational attainment (Model 2). For youth-reported educational attainment, Model 3 additionally adjusted for educational aspirations and expectations. For health and wellbeing outcomes, Model 3 additionally adjusted for actual educational attainment.
Results
Educational Outcomes
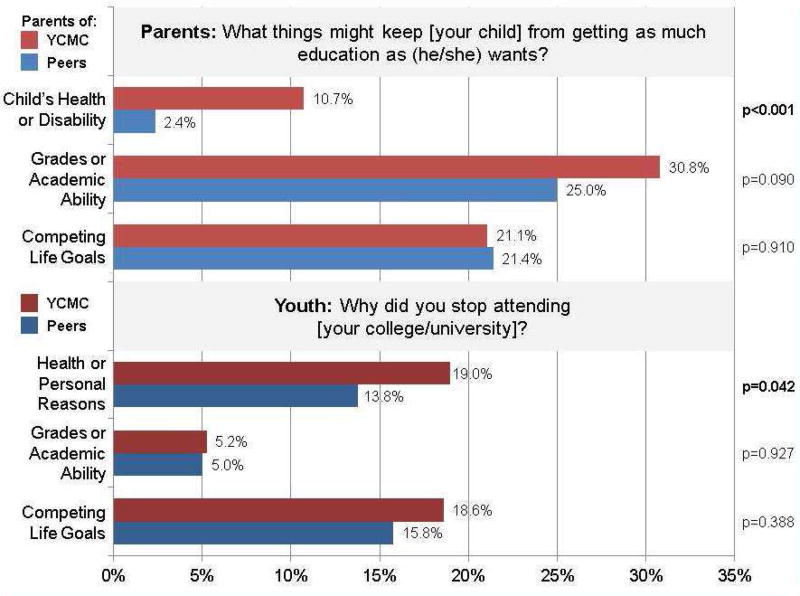
YCMC did not report significantly lower educational aspirations than their healthy peers (e.g., 83.1% of all youth reported aspiring to earn ≥bachelor’s degree; Table 1); however, compared to their counterparts, YCMC reported lower educational expectations (≥bachelor’s degree: 76.3% of YCMC vs 78.0% of peers) and evidenced lower educational attainment by the end of follow-up (≥bachelor’s degree: 19.9% of YCMC vs 26.0% of peers). Disparities in educational attainment persisted after adjustment for confounders, including aspirations and expectations; compared to their healthy peers, YCMC had: 24% lower odds of attending college, 24% lower odds of attending a 4-year college, and 39% lower odds of earning a bachelor’s degree (all p<0.05; Table 2, Model 3). Both aspirations and expectations were significant predictors of actual attainment (data not shown). Among those youth who dropped out of college prior to obtaining a degree, YCMC were more likely to cite personal/health reasons than their peers (19.0% vs 13.8%, p=0.04; Figure 1).
Table 2.
Effects of Chronic Condition Status on Educational Outcomes
|
Estimates for the Effect of Any Chronic Condition (vs None) |
Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Conditional Analyses | ||||||
| High School Grad/GED | 0.55 | (0.30–1.02) | 0.57 | (0.30–1.11) | 0.61 | (0.31–1.23) |
| Any College | High School Grad/GED | 0.69 | (0.54–0.88) | 0.69 | (0.55–0.88) | 0.76 | (0.59–0.97) |
| Earned a Degree | Any College & Age ≥20 years | 0.75 | (0.58–0.97) | 0.69 | (0.53–0.89) | 0.68 | (0.51–0.90) |
| Any 2-year College | High School Grad/GED | 1.01 | (0.82–1.25) | 1.04 | (0.84–1.28) | 1.04 | (0.81–1.33) |
| Earned Associate’s | Attended 2-year College | 0.91 | (0.61–1.37) | 0.84 | (0.56–1.26) | 0.86 | (0.53–1.39) |
| Attended 4-year College | High School Grad/GED | 0.73 | (0.60–0.89) | 0.71 | (0.57–0.88) | 0.76 | (0.60–0.95) |
| Earned Bachelor’s | Attended 4-year College | 0.69 | (0.49–0.97) | 0.62 | (0.45–0.87) | 0.61 | (0.44–0.84) |
| Any Graduate School | Earned Bachelor’s | 1.04 | (0.64–1.70) | 1.02 | (0.66–1.59) | 0.98 | (0.59–1.63) |
| Longitudinal Analyses | ||||||
| Youth’s Actual Educational Achievement | ||||||
| Did not graduate high school/GED | 1.58 | (0.58–4.29) | 1.46 | (0.59–3.62) | 1.63 | (0.70–3.79) |
| Graduated high school/GED | Reference | Reference | Reference | |||
| Some college or vocational training | 0.72 | (0.49–1.06) | 0.73 | (0.50–1.07) | 0.81 | (0.56–1.16) |
| Earned an associate’s degree | 1.10 | (0.37–3.29) | 1.10 | (0.38–3.21) | 1.05 | (0.38–2.88) |
| Earned a bachelor’s degree | 0.29 | (0.13–0.64) | 0.27 | (0.13–0.58) | 0.38 | (0.21–0.67) |
| Any graduate school | 0.23 | (0.04–1.17) | 0.32 | (0.08–1.30) | 0.29 | (0.12–0.74) |
| Youth’s Educational Expectations | ||||||
| ≤Graduate high school/GED | Reference | Reference | ||||
| Some college or vocational training | 0.79 | (0.53–1.18) | 0.79 | (0.54–1.15) | ||
| Earn an associate’s degree | 0.86 | (0.56–1.32) | 0.82 | (0.55–1.23) | ||
| Earn a bachelor’s degree | 0.63 | (0.42–0.94) | 0.66 | (0.45–0.97) | ||
| Earn a graduate degree | 0.62 | (0.39–1.00) | 0.64 | (0.41–1.01) | ||
| Youth’s Educational Aspirations | ||||||
| ≤Graduate high school/GED | Reference | Reference | ||||
| Some college or vocational training | 0.97 | (0.64–1.48) | 0.93 | (0.62–1.41) | ||
| Earn an associate’s degree | 0.86 | (0.55–1.33) | 0.82 | (0.53–1.26) | ||
| Earn a bachelor’s degree | 0.70 | (0.48–1.02) | 0.72 | (0.49–1.05) | ||
| Earn a graduate degree | 0.76 | (0.49–1.18) | 0.82 | (0.53–1.26) | ||
| Parent’s Expectations for Child | ||||||
| ≤Graduate high school/GED | Reference | Reference | ||||
| Some college or vocational training | 0.71 | (0.52–0.97) | 0.76 | (0.56–1.02) | ||
| Earn an associate’s degree | 0.75 | (0.54–1.05) | 0.80 | (0.59–1.09) | ||
| Earn a bachelor’s degree | 0.47 | (0.38–0.60) | 0.57 | (0.45–0.71) | ||
| Earn a graduate degree | 0.61 | (0.44–0.84) | 0.77 | (0.56–1.04) | ||
| Parent’s Preference for Child | ||||||
| ≤Graduate high school/GED | Reference | Reference | ||||
| Some college or vocational training | 0.62 | (0.35–1.08) | 0.67 | (0.35–1.29) | ||
| Earn an associate’s degree | 0.53 | (0.31–0.90) | 0.57 | (0.32–1.02) | ||
| Earn a bachelor’s degree | 0.40 | (0.26–0.61) | 0.48 | (0.31–0.73) | ||
| Earn a graduate degree | 0.54 | (0.34–0.85) | 0.67 | (0.42–1.08) | ||
Data are from the Panel Study of Income Dynamics, Child Development and Transition to Adulthood Supplements (1997–2013).
OR (odds ratio) refers to the effect of having a chronic condition (versus not) on the odds of each educational outcome, relative to the identified reference group. 95% Confidence Intervals (CI) are presented. Conditional analyses model the odds that an individual achieved each educational outcome, conditional on achieving the prior level of education (e.g., the odds of earning a bachelor’s degree among those who matriculated into a 4-year college). Longitudinal analyses present the estimates derived from the multivariate multinomial GLMM, which model highest reported educational attainment at each interview.
Model 1 adjusts for chronic condition status and age.
Model 2 additionally adjusts for sex, race/ethnicity, and socioeconomic status (AFDC/WIC participation; parent marital status; parent education).
Model 3 additionally adjusts for youth’s reported educational aspirations and expectations.
Figure 1.
Parents who reported that their expectations for their child were less than their preferences were asked the follow-up question: “What things might keep (CHILD) from getting as much education as (he/she) wants?” Parents’ verbatim responses were assigned to one of 24 single categories by PSID staff. For this question, ‘Child’s Health or Disability’ included parent’s responses that were classified as: “Learning disability,” “Physical disability,” “Emotional disability/Mental health problems,” “Child’s health,” pr “Disability - Not Specified.” The ‘Grades or Academic Ability’ category included: “Grades/Lack of studying/Doesn’t test well,” “(Lack of) Ambition/Motivation/Attitude/Focus/ Commitment,” or “Dropping out of high school.” The ‘Competing Life Goals’ category included: “Change in personal interests/goals,” “Marriage/relationship,” “Having children,” “Desire to travel,” “Gets a job instead/ Interested in non-academic fields.”
Youth who reported that they stopped attending a college/university without receiving a degree were asked the follow-up question: “Why did you stop attending this school?” Their verbatim responses were assigned to one of 11 single categories by PSID staff. For this question, ‘Health or Personal Reasons’ included responses that were classified as: “Personal reasons; health; pregnancy; marriage; substance use; family commitments.” The ‘Grades or Academic Ability’ category included: “Academic reasons: grades; too large a challenge.” The ‘Competing Life Goals’ category included: “Dissatisfied with school; bored; changed goals.”
Parents of YCMC reported similar preferences for their child’s educational attainment as did parents of healthy youth (e.g., 87.6% preferred their child earn ≥bachelor’s degree; Table 1) yet reported lower expectations for their child (≥bachelor’s degree: 78.0% of YCMC parents vs 82.4% of peer parents). Among parents whose expectations for their child’s education were less than their preferences, parents of YCMC were nearly five times as likely as parents of healthy youth to cite their child’s health or a disability as the reason why they believed their child would achieve less (10.7% vs 2.4%, p<0.01) but were equally likely to cite as reasons their child’s grades/ability (28.5%, p=0.09) or competing life goals (21.2%, p=0.91; Figure 1).
Health & Wellbeing
Compared to their peers, YCMC reported significantly worse general health in young adulthood (p<0.001), lower life satisfaction (p<0.001), and lower psychological wellbeing (p<0.001, Table 1); youth with lower educational attainment also reported significantly worse general health, lower life satisfaction, and lower psychological wellbeing (p<0.01). Disparities in health and wellbeing for YCMC persisted after adjustment for confounders (Table 3); these disparities were partially mediated by educational attainment (yet remain statistically significant) for all three health & wellbeing outcomes (Sobel test p<0.05).
Table 3.
Effects of Chronic Condition Status and Educational Attainment on Health & Wellbeing
| Model 1 | Model 2 | Model 3 | % Attenuation | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| (Better) Health Status | OR | 95% CI | OR | 95% CI | OR | 95% CI | & Sobel Test | |||
| Chronic condition status | ||||||||||
| Any prior diagnosis | 0.42 | (0.33–0.53) | 0.40 | (0.32–0.50) | 0.42 | (0.34–0.52) | 5.87% | |||
| No prior diagnoses | Reference | Reference | Reference | Z = 2.85 | ||||||
| Educational attainment | p = 0.002 | |||||||||
| Did not graduate high school/GED | 0.65 | (0.39–1.10) | ||||||||
| Graduated high school/GED | Reference | |||||||||
| Some college or vocational training | 1.51 | (1.13–2.02) | ||||||||
| Earned an associate’s degree | 1.40 | (0.92–2.14) | ||||||||
| Earned a bachelor’s degree | 3.03 | (2.04–4.50) | ||||||||
| Any graduate school | 3.23 | (1.93–5.41) | ||||||||
| (Higher) Life Satisfaction | OR | 95% CI | OR | 95% CI | OR | 95% CI | ||||
| Chronic condition status | ||||||||||
| Any prior diagnosis | 0.64 | (0.51–0.81) | 0.65 | (0.51–0.82) | 0.67 | (0.53–0.84) | 7.73% | |||
| No prior diagnoses | Reference | Reference | Reference | Z = 1.96 | ||||||
| Educational attainment | p = 0.025 | |||||||||
| Did not graduate high school/GED | 0.81 | (0.46–1.45) | ||||||||
| Graduated high school/GED | Reference | |||||||||
| Some college or vocational training | 1.43 | (1.01–2.03) | ||||||||
| Earned an associate’s degree | 2.14 | (1.29–3.54) | ||||||||
| Earned a bachelor’s degree | 1.75 | (1.11–2.75) | ||||||||
| Any graduate school | 2.31 | (1.30–4.08) | ||||||||
| Psychological Wellbeing | β | S.E. | p-val | β | S.E. | p-val | β | S.E. | p-val | |
| Chronic condition status | ||||||||||
| Any prior diagnosis | −1.13 | 0.17 | <0.001 | −1.18 | 0.17 | <0.001 | −1.14 | 0.17 | <0.001 | 3.68% |
| No prior diagnoses | Reference | Reference | Reference | Z = 2.30 | ||||||
| Educational attainment | p = 0.011 | |||||||||
| Did not graduate high school/GED | −0.47 | 0.36 | 0.200 | |||||||
| Graduated high school/GED | Reference | |||||||||
| Some college or vocational training | 0.56 | 0.20 | 0.005 | |||||||
| Earned an associate’s degree | 0.90 | 0.28 | 0.001 | |||||||
| Earned a bachelor’s degree | 0.85 | 0.27 | 0.002 | |||||||
| Any graduate school | 0.52 | 0.37 | 0.160 |
Data are from the Panel Study of Income Dynamics, Child Development and Transition to Adulthood Supplements (1997–2013).
OR (odds ratio) refers to the effect of having a chronic condition or educational attainment on the cumulative odds (across a 5-point Likert scale) of better general health (7,076 observations, 2,555 subjects) and higher life satisfaction (5,220 observations, 2,483 subjects), derived from the multivariate ordinal GLMM. 95% Confidence Intervals (CI) are presented. β refers to the effect of having a chronic condition or educational attainment on the continuous psychological wellbeing scale (higher values indicate greater wellbeing; 7,080 observations, 2,555 subjects).
Standard errors (S.E.) and the associated p-values for the point estimates are presented.
Model 1 adjusts for chronic condition status and age.
Model 2 additionally adjusts for sex, race/ethnicity, and socioeconomic status (AFDC/WIC participation; parent marital status; parent education).
Model 3 additionally adjusts for youth’s own educational attainment.
Attenuation was determined as the percent change in the coefficient for chronic condition status from model 2 to model 3; the Sobel test was used to evaluate mediation of the effect of chronic condition status on each health outcome by educational attainment.
Condition-Specific Analyses
Condition-specific analyses identified similar findings across all condition sub-types, including significant differences in odds of graduating high school or completing a GED for all condition categories except sensory impairments (Table 4). Youth with learning disabilities had the lowest odds of attending any or a 4-year college, youth with a limitation-causing condition had the lowest odds of completing a bachelor’s degree and greatest health disparities, and youth with psychological conditions had the greatest wellbeing disparities.
Table 4.
Investigation of Education and Health Outcomes by Chronic Condition Categories
| Any [condition] vs none | All conditions | Psychological/ emotional problem |
Developmental/ Learning disability |
Sensory impairment |
Major medical condition |
Major medical w/ activity limitation |
|---|---|---|---|---|---|---|
| Total with any diagnosis | N = 2,113 | N = 490 | N = 596 | N = 634 | N = 1,584 | N = 320 |
| Educational Outcomes | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) |
| Graduated high school or completed a GED | 0.57 (0.30–1.11) | 0.32 (0.15–0.68) | 0.30 (0.13–0.70) | 0.53 (0.21–1.36) | 0.54 (0.29–0.999) | 0.33 (0.16–0.68) |
| Any college | high school grad or GED | 0.69 (0.55–0.88) | 0.54 (0.37–0.80) | 0.44 (0.30–0.64) | 0.57 (0.42–0.76) | 0.71 (0.54–0.92) | 0.56 (0.38–0.83) |
| Attended 4-year college | high school grad or GED | 0.71 (0.57–0.88) | 0.58 (0.41–0.82) | 0.36 (0.27–0.48) | 0.75 (0.56–0.98) | 0.72 (0.56–0.92) | 0.63 (0.44–0.89) |
| Earned bachelor’s | Attended 4-year college | 0.62 (0.45–0.87) | 0.47 (0.30–0.74) | 0.41 (0.24–0.69) | 0.62 (0.41–0.95) | 0.68 (0.48–0.96) | 0.37 (0.22–0.63) |
| Health Outcomes | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) |
| (Better) Health status | 0.40 (0.32–0.50) | 0.20 (0.15–0.27) | 0.36 (0.26–0.50) | 0.45 (0.32–0.62) | 0.35 (0.28–0.45) | 0.12 (0.08–0.17) |
| (Higher) Life satisfaction | 0.65 (0.51–0.82) | 0.31 (0.22–0.44) | 0.60 (0.43–0.84) | 0.62 (0.45–0.87) | 0.68 (0.53–0.87) | 0.36 (0.25–0.53) |
| β (S.E.; p-value) | β (S.E.; p-value) | β (S.E.; p-value) | β (S.E.; p-value) | β (S.E.; p-value) | β (S.E.; p-value) | |
| Psychological wellbeing | −1.18 (0.17; <0.01) | −2.69 (0.23; <0.01) | −1.82 (0.25; <0.01) | −1.34 (0.24; <0.01) | −1.21 (0.18; <0.01) | −2.59 (0.30; <0.01) |
Data are from the Panel Study of Income Dynamics, Child Development and Transition to Adulthood (TA) Supplements (1997–2013).
- any psychological or emotional problem;
- any developmental delay, learning disability, autism, or ADHD/ADD;
- any sensory impairment (i.e., hearing, speech, or visual impairments);
- any of the other major medical conditions not included in (2), (3), or (4); and
- selected conditions identified in (5) for which the individual reported in the TA that their normal activities were “a lot” or “somewhat” limited by their condition.
All presented estimates thus compare each chronic condition type versus no condition of any kind, adjusting for age, sex, race/ethnicity, and socioeconomic status (AFDC/WIC participation; parent marital status; parent education).
For educational outcomes, results from multivariate conditional analyses are shown.
For health outcomes, results from multivariate ordinal GLMM are shown for health status and life satisfaction and results from multivariate Gaussian GLMM are shown for psychological wellbeing.
Discussion
Despite observing no significant difference in educational aspirations for youth with and without chronic medical conditions, YCMC’s expectations for their educational attainment and their actual attainment trailed behind their healthy peers during adolescence and emergent adulthood. Educational attainment was a strong predictor of later health and wellbeing, and gaps in attainment partially mediated the associations between having a pediatric-onset chronic condition and poor health/wellbeing later in life. Findings suggest an important mechanism through which medically vulnerable youth disproportionately acquire socioeconomic disadvantage as they mature, which in turn affects their future health and wellbeing. Both matriculation into college and completion of a bachelor’s degree are specific junctures where expectation and attainment gaps widen and supportive interventions may be especially helpful.
Prior studies have investigated educational attainment for YCMC and found similar gaps in attainment,17,20,23–26 although few studies have been able to assess the extent to which these disparities stem from underlying differences in educational aspirations or expectations, or pinpoint where in the educational trajectory YCMC are most likely to fall behind their peers. We identified that even prior to completing high school, YCMC and their parents report lower expectations for attainment. Diminished expectations may reflect an accurate anticipation of likely challenges to attainment in the post-secondary school setting given what may be a dearth of practical supports for managing symptoms, disease activity, treatment regimens, and other problems in the context of everyday demands for student life. Moreover, internalized expectations of low attainment, especially coupled with high aspirations, may additionally undermine academic success. Helpful interventions may involve provision of guidance and coaching in healthcare settings to help YCMC navigate educational environments, as well as developing plans to overcome likely challenges, including those stemming from the need to simultaneously balance academic and disease-specific demands. YCMC must constantly prioritize disease self-management to avoid adverse outcomes,13,27,28 yet competing life priorities may interfere with youth’s ability to engage in routine self-care and self-regulation of risk behaviors. Additional policy and program interventions may be needed to ensure that features of educational settings enable YCMC to fully participate (e.g., exchange of health records, flexible class/exam schedules to accommodate treatment regimens, medical leave without academic or financial penalty, residential and nutritional accommodations).
We found that YCMC are significantly less likely than their healthy peers to complete a bachelor’s degree after entering a 4-year college, and that earning a college degree is protective for future health and wellbeing. College constitutes a critical developmental opportunity for YCMC. This opportunity is precarious: College overlaps the period when transition from pediatric to adult-focused care is recommended,29 and when youth are most likely to fall out of contact with their healthcare provider.30 Movement away from established care relationships and supports, common for college attending youth, may undermine self-management and expose YCMC to environments conducive of risk behaviors;31–33 yet, evidence suggests that many colleges are not well equipped to identify and support the medical needs of YCMC.34,35 Lacking access to preventive and specialty care during college may explain the observed lower graduation rates among the YCMC who make it to college. Alternatively, increased exposure to stressful environments and risk behaviors during college may exacerbate chronic disease symptoms, which in turn may impede this group’s progression from matriculation to graduation. We currently have an incomplete understanding of the ways in which educational settings interact with the chronic illness experience to shape outcomes, but our findings suggest that inequalities build over various steps in the educational trajectory. Ensuring that YCMC are able to achieve their desired educational trajectory will likely require targeted efforts to support continued healthcare engagement throughout the transition period. For college-attending YCMC, additional structural supports may be needed to ensure access to necessary healthcare and other supportive services; ideally through creating a network of interconnected services and supports in order to eliminate administrative obstacles and facilitate shared information and responsibility.
Importantly, pediatric-onset chronic medical conditions were associated with subsequent worse general health, life satisfaction, and psychological wellbeing, while disparities in educational attainment appeared to partially mediate these associations. This pathway may stem from reinforcing vulnerability. For instance, impediments to disease self-management during college may explain why fewer college-attending YCMC complete a bachelor’s degree whereas additional educational attainment might promote improved self-efficacy in disease self-management skills, with each step contributing to widening gaps in effective self-care. For both YCMC and their healthy peers, college (and post-high school generally) is a time when youth develop increased autonomy and independence, skills that are important for all young adults but which may be particularly important for improved proficiency in self-care and the ability to self-advocate in the healthcare and broader social environments. Skills-based interventions may be one way to advance general competencies that could be doubly impactful for both scholastic and disease outcomes.36,37 Yet, addressing the intersection of education and health may require a broader, integrative approach.38 For instance, policy levers have been implemented to avoid discrimination on the basis of disability (Americans with Disabilities Act) and to promote equal educational opportunity (Individuals with Disabilities Education Act);39 such regulations have moved students toward parity in educational programs. Still, to identify and shrink lingering disparities there is a clear need to evaluate adequacy and variability in current practices for facilitating disease self-management and academic, social, and extracurricular engagement in educational settings. As well, it is worth considering how clinicians might help promote educational attainment of YCMC as a legitimate “health outcome.” Ultimately, because the burden of chronic disease appears to complicate and compound normal developmental needs for adolescents and young adults, interventions that buttress individual and system-level supports to address these life-course processes may strengthen youth resilience and maximize their potential to thrive.
This study contributes new information to the extant literature on developmental outcomes for YCMC. Longitudinal data allowed the examination of trajectories of educational attainment and health status over more than a decade of follow-up and the nationally representative cohort with high response rates and low rates of missing items enables generalizable estimates to US adolescents and young adult populations.40 Several important limitations also apply. Parent/self-report of chronic disease diagnosis is not an ideal proxy for clinical report. The high prevalence of conditions among youth in PSID cohorts may stem from the broad definition of conditions with potential for false positives; if present, such misclassification would likely bias findings toward the null. We note that the study sample has a high degree of shared ancestry,33 inflating the overall prevalence of youth with any condition. The low prevalence of many specific conditions precludes precise condition-specific estimates, a limitation, as is the lack of detailed information on condition severity or functional impairments. These issues should be priorities for future investigations. Many factors may contribute to education and health outcomes and while we adjusted for a number of established confounders, our estimates may still be subject to residual confounding. Finally, although 64.4% of youth included in the educational outcomes analyses were at least age 22 years at their last follow-up (38.2% were ≥25 years), many individuals obtain their terminal degrees later in life. Therefore, our view into lifetime educational attainment for a relatively young sample may be limited.
Conclusion
YCMC must navigate normal adolescent development in light of the burden of their disease and its treatment, but we have yet to fully understand the mechanisms through which developmental processes may be disrupted with consequences for health disparities. Findings from this study suggest an important mechanism through which YCMC are susceptible to acquiring socioeconomic disadvantage as they progress through normal development. Specifically, as lags in educational expectations and attainment manifest, we see increased future susceptibility to diminished health and wellbeing. Clinicians have an important opportunity to provide supportive guidance to YCMC and triage at-risk youth to psychosocial interventions to help them anticipate and navigate educational environments in a fashion that protects attainment and health. Policymakers and program developers from education and health sectors may have a role too, in advancing structural supports. Additional work is warranted to understand the complex relationship between the myriad of risk and protective factors in this stage of development to guide intervention and response, including during high-risk periods of healthcare transition and emergent adulthood.
Implications and Contribution: Findings suggest that youth with chronic conditions are susceptible to lower educational attainment, despite not having different educational aspirations from their healthy peers, and that these gaps in attainment partially contribute to the pathway leading from chronic disease to later adverse health and wellbeing.
Acknowledgments
We wish to acknowledge the generous funding support from the Harvard-wide Pediatric Health Services Research Fellowship (Agency for Healthcare Research and Quality (AHRQ) 5T32HS00063-21, PI: J. Finkelstein), the Thomas O. Pyle Fellowship (Department of Population Medicine), the National Institute on Alcohol Abuse and Alcoholism (NIAAA 1R01AA021913-01, PIs: E. Weitzman and S. Levy), the Conrad N. Hilton Foundation (grant # 20140273), Mentored Career Development for Child and Family Centered Outcomes Research (AHRQ K12HS022986, PI: J. Finkelstein), and BCH Awards Committee Pilot (FP01017994). The collection of data used in this study was partly supported by the National Institutes of Health (under grant number R01 HD069609) and the National Science Foundation (under award number 1157698). The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Abbreviations
- CDS
Child Development Supplement
- CI
Confidence Interval
- OR
Odds Ratio
- PSID
Panel Study of Income Dynamics
- SES
Socioeconomic Status
- TA
Transition into Adulthood
- YCMC
Youth with Chronic Medical Conditions
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The submitted research has never been published but earlier versions of this work have been presented at the 2016 annual meetings of the Society for Adolescent Health and Medicine, Pediatric Academic Societies, and AcademyHealth.
Financial disclosure: The authors have no financial relationships or conflicts of interest to disclose.
References
- 1.Van Cleave J, Gortmaker SL, Perrin JM. Dynamics of obesity and chronic health conditions among children and youth. JAMA. 2010;303(7):623–630. doi: 10.1001/jama.2010.104. [DOI] [PubMed] [Google Scholar]
- 2.Wisk LE, Witt WP. Predictors of delayed or forgone needed health care for families with children. Pediatrics. 2012;130(6):1027–1037. doi: 10.1542/peds.2012-0668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Palta M, LeCaire T. Managing type 1 diabetes: trends and outcomes over 20 years in the Wisconsin Diabetes Registry cohort. Wisconsin Medical Journal. 2009;108(5):231–235. [PMC free article] [PubMed] [Google Scholar]
- 4.Guerra S, Wright AL, Morgan WJ, Sherrill DL, Holberg CJ, Martinez FD. Persistence of asthma symptoms during adolescence: role of obesity and age at the onset of puberty. American Journal of Respiratory and Critical Care Medicine. 2004;170(1):78–85. doi: 10.1164/rccm.200309-1224OC. [DOI] [PubMed] [Google Scholar]
- 5.Sawyer SM, Rosier MJ, Phelan PD, Bowes G. The self-image of adolescents with cystic fibrosis. Journal of Adolescent Health. 1995;16(3):204–208. doi: 10.1016/1054-139X(94)00071-L. [DOI] [PubMed] [Google Scholar]
- 6.MacPhee M, Hoffenberg EJ, Feranchak A. Quality-of-life factors in adolescent inflammatory bowel disease. Inflammatory Bowel Diseases. 1998;4(1):6–11. doi: 10.1097/00054725-199802000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Mackner LM, Crandall WV. Brief report: psychosocial adjustment in adolescents with inflammatory bowel disease. Journal of Pediatric Psychology. 2006;31(3):281–285. doi: 10.1093/jpepsy/jsj023. [DOI] [PubMed] [Google Scholar]
- 8.Tucker LB, Cabral DA. Transition of the adolescent patient with rheumatic disease: issues to consider. Rheumatic Diseases Clinics of North America. 2007;33(3):661–672. doi: 10.1016/j.rdc.2007.07.005. [DOI] [PubMed] [Google Scholar]
- 9.Kellerman J, Zeltzer L, Ellenberg L, Dash J, Rigler D. Psychological effects of illness in adolescence. I. Anxiety, self-esteem, and perception of control. The Journal of Pediatrics. 1980;97(1):126–131. doi: 10.1016/s0022-3476(80)80152-1. [DOI] [PubMed] [Google Scholar]
- 10.Zeltzer L, Kellerman J, Ellenberg L, Dash J, Rigler D. Psychologic effects of illness in adolescence. II. Impact of illness in adolescents--crucial issues and coping styles. The Journal of Pediatrics. 1980;97(1):132–138. doi: 10.1016/s0022-3476(80)80153-3. [DOI] [PubMed] [Google Scholar]
- 11.Institute of Medicine. Investing in the Health and Well-Being of Young Adults. Washington, DC: National Academies of Sciences; 2015. 978-0-309-30995-0. [PubMed] [Google Scholar]
- 12.Layard R, Clark AE, Cornaglia F, Powdthavee N, Vernoit J. What Predicts a Successful Life? A Life-Course Model of Well-Being. Economic Journal (London) 2014;124(580):F720–F738. doi: 10.1111/ecoj.12170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lynch J, Smith GD. A life course approach to chronic disease epidemiology. Annual Review of Public Health. 2005;26:1–35. doi: 10.1146/annurev.publhealth.26.021304.144505. [DOI] [PubMed] [Google Scholar]
- 14.Hanson MD, Chen E. Socioeconomic status and health behaviors in adolescence: a review of the literature. Journal of Behavioral Medicine. 2007;30(3):263–285. doi: 10.1007/s10865-007-9098-3. [DOI] [PubMed] [Google Scholar]
- 15.Hayward MD, Hummer RA, Sasson I. Trends and group differences in the association between educational attainment and U.S. adult mortality: implications for understanding education’s causal influence. Social Science & Medicine. 2015;127:8–18. doi: 10.1016/j.socscimed.2014.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Masters RK, Link BG, Phelan JC. Trends in education gradients of ‘preventable’ mortality: a test of fundamental cause theory. Social Science & Medicine. 2015;127:19–28. doi: 10.1016/j.socscimed.2014.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sawyer SM, Drew S, Yeo MS, Britto MT. Adolescents with a chronic condition: challenges living, challenges treating. Lancet. 2007;369(9571):1481–1489. doi: 10.1016/S0140-6736(07)60370-5. [DOI] [PubMed] [Google Scholar]
- 18.Institute of Medicine. Living Well with Chronic Illness: A Call for Public Health Action. Washington, DC; National Academies of Sciences: 2012. [Google Scholar]
- 19.Champaloux SW, Young DR. Childhood chronic health conditions and educational attainment: a social ecological approach. Journal of Adolescent Health. 2015;56(1):98–105. doi: 10.1016/j.jadohealth.2014.07.016. [DOI] [PubMed] [Google Scholar]
- 20.Maslow GR, Haydon A, McRee AL, Ford CA, Halpern CT. Growing up with a chronic illness: social success, educational/vocational distress. Journal of Adolescent Health. 2011;49(2):206–212. doi: 10.1016/j.jadohealth.2010.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kessler RC, Barker PR, Colpe LJ, et al. Screening for serious mental illness in the general population. Archives of General Psychiatry. 2003;60(2):184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- 22.Mackinnon DP, Warsi G, Dwyer JH. A Simulation Study of Mediated Effect Measures. Multivariate Behavioral Research. 1995;30(1):41. doi: 10.1207/s15327906mbr3001_3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gurney JG, Krull KR, Kadan-Lottick N, et al. Social outcomes in the Childhood Cancer Survivor Study cohort. Journal of Clinical Oncology. 2009;27(14):2390–2395. doi: 10.1200/JCO.2008.21.1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hunt J, Eisenberg D, Kilbourne AM. Consequences of receipt of a psychiatric diagnosis for completion of college. Psychiatric Services. 2010;61(4):399–404. doi: 10.1176/ps.2010.61.4.399. [DOI] [PubMed] [Google Scholar]
- 25.Maslow G, Haydon AA, McRee AL, Halpern CT. Protective connections and educational attainment among young adults with childhood-onset chronic illness. The Journal of School Health. 2012;82(8):364–370. doi: 10.1111/j.1746-1561.2012.00710.x. [DOI] [PubMed] [Google Scholar]
- 26.Maslow GR, Haydon AA, Ford CA, Halpern CT. Young adult outcomes of children growing up with chronic illness: an analysis of the National Longitudinal Study of Adolescent Health. Archives of Pediatrics & Adolescent Medicine. 2011;165(3):256–261. doi: 10.1001/archpediatrics.2010.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Holmes CS, Chen R, Streisand R, et al. Predictors of youth diabetes care behaviors and metabolic control: a structural equation modeling approach. Journal of Pediatric Psychology. 2006;31(8):770–784. doi: 10.1093/jpepsy/jsj083. [DOI] [PubMed] [Google Scholar]
- 28.Stinson J, Wilson R, Gill N, Yamada J, Holt J. A systematic review of internet-based self-management interventions for youth with health conditions. Journal of Pediatric Psychology. 2009;34(5):495–510. doi: 10.1093/jpepsy/jsn115. [DOI] [PubMed] [Google Scholar]
- 29.American Academy of Pediatrics, American Academy of Family Physicians, American College of Physicians, Transitions Clinical Report Authoring Group. Cooley WC, Sagerman PJ. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. 2011;128(1):182–200. doi: 10.1542/peds.2011-0969. [DOI] [PubMed] [Google Scholar]
- 30.Wisk LE, Finkelstein JA, Sawicki GS, et al. Predictors of timing of transfer from pediatric- to adult-focused primary care. JAMA Pediatrics. 2015;169(6):e150951. doi: 10.1001/jamapediatrics.2015.0951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Patrick ME, Terry-McElrath YM. High-intensity drinking by underage young adults in the United States. Addiction. 2017;112(1):82–93. doi: 10.1111/add.13556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Patrick ME, Terry-McElrath YM, Kloska DD, Schulenberg JE. High-Intensity Drinking Among Young Adults in the United States: Prevalence, Frequency, and Developmental Change. Alcoholism, Clinical and Experimental Research. 2016;40(9):1905–1912. doi: 10.1111/acer.13164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wisk LE, Weitzman ER. Substance Use Patterns Through Early Adulthood: Results for Youth With and Without Chronic Conditions. American Journal of Preventive Medicine. 2016;51(1):33–45. doi: 10.1016/j.amepre.2016.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lemly DC, Lawlor K, Scherer EA, Kelemen S, Weitzman ER. College health service capacity to support youth with chronic medical conditions. Pediatrics. 2014;134(5):885–891. doi: 10.1542/peds.2014-1304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schwenk HT, Lightdale JR, Arnold JH, Goldmann DA, Weitzman ER. Coping with college and inflammatory bowel disease: implications for clinical guidance and support. Inflammatory Bowel Diseases. 2014;20(9):1618–1627. doi: 10.1097/MIB.0000000000000124. [DOI] [PubMed] [Google Scholar]
- 36.Maslow G, Adams C, Willis M, et al. An evaluation of a positive youth development program for adolescents with chronic illness. Journal of Adolescent Health. 2013;52(2):179–185. doi: 10.1016/j.jadohealth.2012.06.020. [DOI] [PubMed] [Google Scholar]
- 37.Maslow GR, Chung RJ. Systematic review of positive youth development programs for adolescents with chronic illness. Pediatrics. 2013;131(5):e1605–1618. doi: 10.1542/peds.2012-1615. [DOI] [PubMed] [Google Scholar]
- 38.Suris JC, Michaud PA, Viner R. The adolescent with a chronic condition. Part I: developmental issues. Archives of Disease in Childhood. 2004;89(10):938–942. doi: 10.1136/adc.2003.045369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Office for Civil Rights. [Accessed Feb 15, 2017];Protecting Students With Disabilities: Frequently Asked Questions About Section 504 and the Education of Children with Disabilities. 2015 https://www2.ed.gov/about/offices/list/ocr/504faq.html. US Department of Education.
- 40.McGonagle KA, Schoeni RF, Sastry N, Freedman VA. The Panel Study of Income Dynamics: Overview, Recent Innovations, and Potential for Life Course Research. Longitudinal and Life Course Studies. 2012;3(2) doi: 10.14301/llcs.v3i2.188. [DOI] [PMC free article] [PubMed] [Google Scholar]