Abstract
Introduction:
Lifelong learning is an integral part of health professionals’ maintenance of competence. Several studies have examined the orientation toward lifelong learning at various stages of the education and career continuum; however, none has looked at changes throughout training and practice. The objective of the present study was to determine if there are differences between groups defined by their places on the education and career continuum.
Methods:
The authors performed a group-level meta-analysis on studies that used the 14-item Jefferson Scale of Physician Lifelong Learning or its variants. Eleven published articles, which reported on studies with post-secondary health professions students, residents, and practicing health professionals met the inclusion criteria. In total, there were 12 independent data sets, with four data sets per group.
Results:
In total, over seven thousand students, residents, and practicing health professionals responded to the Jefferson Scale (N=7.269). Individual study means tendency to be high, suggesting a high orientation toward lifelong learning among the trainees (students and residents) and practicing health professionals. Meta-analysis results indicated that the orientation toward lifelong learning tended to increase gradually along the education and career continuum. Significant differences in the group means were found between the trainees and practicing health professionals.
Conclusion:
In the reviewed studies, the orientation toward lifelong learning among students, residents, and practicing professionals was high. Nonetheless, although based on separate cohorts, it appears that the orientation toward lifelong learning continues to develop even after the completion of formal training.
Keywords: Lifelong learning , Health professions , Meta-analysis
Introduction
To stay up-to-date with new evidence and guidelines that are continuously being developed, health professionals must engage in ongoing professional development. To this end, professional organizations have identified lifelong learning as a core competency in health professions, with a recommendation to schools to provide training enabling trainees (students and residents) to become lifelong learners (1-3).
Hojat and colleagues (4-6) defined lifelong learning as an attribute involving a set of self-initiated activities and information-seeking skills with sustained motivation to learn and the ability to recognize one’s own learning needs. As such, lifelong learning has been recognized as an indicator of professionalism, competence, and critical competent of continuing professional development (1-3,7,8). Despite this, there has been a paucity of validated tools to assess lifelong learning, with most measuring attitudes and beliefs toward lifelong learning rather than demonstrated behaviors and skills (9-13). As such, guided by the above definition, Hojat and colleagues developed a 19-item instrument to measure the orientation toward lifelong learning among physicians (the Jefferson Scale of Physician Lifelong Learning; JeffSPLL) (4,5), with a subsequent revision to 14 items (6). The 14-itemJeffSPLL has also been modified for use with medical students (JeffSPLL-MS) (14) and with students in other health professions (JeffSLL-HPS) (15,16), and has been used with residents (17-20). The JeffSPLL encompasses four key concepts of the lifelong learning: self-initiated activities (behavioural aspect); information-seeking skills (capabilities); sustained motivation to learn (motivation); and ability to identify one’s own learning needs (cognition).
The total scores on the 14-item scale range from 14 to 56, with higher scores indicating a greater propensity or orientation toward lifelong learning. Validity evidence for the14-item Jeff SPLL and its student variants includes: sound psychometric properties (6,14,15); sensitivity to educational interventions targeting orientation toward lifelong learning (17); and most impressively, correlations with behavioral manifestations of lifelong learning and professional accomplishments of practicing health professionals (e.g. involvement in teaching, scholarly activities and outputs, receiving awards or honours) (6,21). In addition, a positive association was found between the orientation toward lifelong learning as measured by the Jeff SPLL and physicians’ career satisfaction (22).
In the studies in which the Jeff SPLL or its variants have been used, the focus was specifically on one group: students, residents, or practicing health professionals. None of the studies was longitudinal or compared orientation toward lifelong learning between different groups as defined by their places on the education and career continuum. Therefore, the objective of the present study was to determine if there are differences between these groups.
Methods
The present study conformed to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (23). Ethics approval was not required as this study used the data from published studies.
Study search
Studies were searched in electronic databases and database collections, including PubMed, MEDLINE, ERIC, OVID, PsycINFO, Scopus, Web of Science, CBCA Education, and Google Scholar. The following search terms and their variants were used: “Jefferson Scale of Physician Lifelong Learning”, “JeffSPLL”,“JeffSPLL for medical students”, “JeffSPLL-MS”,“Jefferson Scale of Lifelong Learning – Health Professions Students”, “JSLL-HPS”, “lifelong learning”, “measure”, “physician”, “clinician”, “resident”, “residency”, “student”, “medical”, “health professions”. In Google Scholar, the search was limited to the title only. The reference lists of the relevant studies were also examined. Searches for publications were conducted through December 2016. Studies published in languages other than English were translated using on-line translators.
Study selection
Studies were selected for the present review if they satisfied the following criteria: primary studies conducted with students pursuing higher education in health professions, residents, or practicing health professionals with higher education degrees; and studies in which the 14-item Jeff SPLL or its student variants (hereafter referred to as the Jefferson Scale) were used to assess the orientation toward lifelong learning in health professions.
Summary measures
Means and standard deviationsof the total scores on the Jefferson Scale, together with sample sizes, were extracted from each study that met the inclusion criteria (Table 1). If the item-level mean and standard deviation were reported (17), the mean and standard deviation for the total score were derived from the reported item-level values using standard formulas (24).
Table 1.
Group-level meta-analysis results: data sets within each group are organized in the descending order of the summary measures (mean scores on the Jefferson Scale), with the estimated group mean shown at the bottom of each group
| Author, year, country | S/R/P | N | Mean±SD (SE) | 95% CI | Relative Weight, % | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Wetzel, 2010, USA | S | 652 | 43.52±4.65 (0.18) | 43.16 | 43.88 | 28.44 |
| Novak, 2013, USA | S | 180 | 43.06±5.50 (0.41) | 42.26 | 43.86 | 23.47 |
| Mi & RD, 2016, USA (m) | S | 128 | 43.04±5.14 (0.45) | 42.15 | 43.93 | 22.38 |
| Mi & RD, 2016, USA (n) | S | 209 | 41.84±4.56 (0.32) | 41.22 | 42.46 | 25.71 |
| STUDENT | 1,169 | 42.87±(0.43) | 42.04 | 43.71 | 100 | |
| Mi &Halalau, 2016, USA | R | 29 | 46.48±5.32(0.98) | 44.54 | 48.42 | 20.41 |
| Lockspeiser, 2013, USA | R | 48 | 44.75±4.32 (0.62) | 43.53 | 45.97 | 24.78 |
| Li ST, 2010, USA | R | 992 | 43.00±4.80 (0.15) | 42.70 | 43.30 | 28.58 |
| Sockalingam, 2016, Canada | R | 105 | 41.08±4.99 (0.49) | 40.13 | 42.03 | 26.23 |
| RESIDENT | 1,174 | 43.64±(0.83) | 42.02 | 45.26 | 100 | |
| Ma, 2013, China | P | 933 | 46.97±5.50 (0.18) | 46.62 | 47.32 | 27.32 |
| Burman, 2014, USA | P | 57 | 46.30±3.90 (0.52) | 45.29 | 47.31 | 16.15 |
| Hojat, 2009, USA | P | 2,739 | 46.20±5.50 (0.11) | 45.99 | 46.41 | 29.16 |
| Li H, 2015, China | P | 1,197 | 45.56±6.17 (0.18) | 45.21 | 45.91 | 27.37 |
| PHYSICIAN | 4,926 | 46.25±(0.30) | 45.66 | 46.85 | 100 | |
S/R/P - Student/Resident/Physician; SD: Standard Deviation; SE: Standard Error
m -medical students; n -nursing students
Data extraction
The following information was extracted, if available, from the included studies: first author; year of publication; country; study participants (students, residents, practicing health professionals); program (e.g. medicine, nursing) and specialty (e.g.primary care, pediatrics, psychiatry); participant characteristics (e.g.age, proportion of female participants, year in medical school or residency or total years in practice for practitioners); type of practice and setting (e.g. rural/urban, hospital/clinic), methodological characteristics of each study (e.g. sample size, study design), and the reported values for the summary measures.
Statistical analysis
Given the objective of the present study, we performed group-level meta-analysis with the studies conducted with students, residents, and practicing health professionals. We used the random-effects model for pooling the observed study means in each group. Under the random-effects model, there is a distribution of the true study means that underlies the observed study means, with the mean of that distribution being the true grand mean. We used the Q-statistic to determine if the variation of the true study means in each group was within the range that could be attributed to chance or exceeded that range. The Q-statistic provides a test of the null hypothesis that all the studies share a common true grand mean. In this case, the expected value of Q-statistic would be equal to the degrees of freedom (df; equal to the number of studies in a given group minus 1). If the null hypothesis is rejected, this suggests that heterogeneity in the true study means is beyond chance; then the I2-statistic is used as an estimate of heterogeneity. A value of I2 over 50% indicates substantial heterogeneity in the true study means (25). Due to paucity of data, we were unable to stratify the analyses by year in school or residency program (year 1, year 2, etc.), specialty or geographical regions to explore the heterogeneity in individual study means.All analyses were conducted using Comprehensive Meta-Analysis software, version 3.3 (www.Meta-Analysis.com) (26).
Results
Following the examination of the titles and abstracts of the located published articles, 17 publications were determined as potentially relevant, of which 12 articles (6,13-21,27-28) metthe inclusion criteria. Upon further examination, one article (21) was excluded as it reported on the outcome measure for the same participants as in one of the articles already included in the review. In total, 11 studies (12 independent data sets) were used in the group-level meta-analysis (6,13-20,27-28). Each group of studies involving students, residents and practicing health professionals had four independent data sets. The group of practicing health professionals consisted of the studies that had been conducted with practicing physicians (Tables 1 and 2).
Table 2.
Study participant characteristics
| Author, year, country | S/R/P | N | Specialty/Setting | Age: M (SD), range, % | F: % | Yrs in practice / program |
|---|---|---|---|---|---|---|
| Wetzel, 2010, USA | S | 652 | Medicine | na | na | Y1-4 (% - na) |
| Novak, 2013, USA | S | 180 | Dental hygiene (3%), dental medicine (8%), medicine (45%), nursing (10%), occupational therapy (6%), physician assistant (10%), physical therapy (14%), respiratory therapy (3%) | na | na | na |
| Mi & RD, 2016, USA | S | 128 | Medicine | 84% 18-36 yrs | 77% | Y1-4 (40% Y1; 39% Y2; 21% Y3/Y4) |
| 209 | Nursing | Undergraduate (Ys - na) | ||||
| Mi &Halalau, 2016, USA | R | 29 | Internal medicine | 25-34 | 41% | 48% PGY1 |
| Lockspeiser, 2013, USA | R | 48 | Pediatrics | na | na | Finishing PGY3 |
| Li ST, 2010, USA | R | 992 | Pediatrics | na | 74% | PGY1-3 (35% PGY1; 33% PGY2; 32% PGY3 or higher) |
| Sockalingam, 2016, Canada | R | 105 | Psychiatry | 96% 26-35 yrs | 62% | PGY1-5 (19% PGY1; 17% PGY2; 24% PGY3; 19% PGY4; 19% PGY5) |
| Ma, 2013, China | P | 933 | Urban hospitals | na | na | na |
| Burman, 2014, USA | P | 57 | Pediatrics | na | 70% | Early career |
| Hojat, 2009, USA | P | 2,739 | Primary care specialties of general internal medicine, family medicine, and general pediatrics, obstetrics/gynecology, anesthesiology, psychiatry, and general surgery, pathology | 46 (7.3); 29-66 yrs | 26% | na |
| Li H, 2015, China | P | 1,197 | Rural physicians | 58% ≤ 40 yrs | 51% | 50% 0-15 yrs |
S/R/P - Student/Resident/Physician; M (SD) - mean (standard deviation); F - female
na - not available/not reported
Characteristics of the included studies
Eight studies were carried out in the USA (6,13-17,19,20), two in China, (27,28) , and one in Canada (18). All the studies were cross-sectional survey studies involving medical/health professions students, (14-16) residents (17-20), and practicing physicians (6,13,27,28). The sample size of the included studies ranged from 29 participants to 2,739 participants (17). In the studies in which the respondents’ gender was reported, the proportion of female participants ranged from 26% (6) to 77% (17).
In studies involving students, the following programs were represented: medicine (14,16) and nursing (16); one study was multi-program and included students in dental hygiene, dental medicine, medicine, nursing, occupational therapy, physician assistant, physical therapy, and respiratory therapy (15). Most studies with residents and practicing physicians focused on one specialty, with the following specialties represented: internal medicine (17); pediatrics (13,19,20); and psychiatry (18). One study was multi-specialty and included practicing physicians in anesthesiology, family medicine, general internal medicine, general pediatrics, general surgery, obstetrics/gynecology, pathology, and psychiatry (6). One study focused on rural physicians in China (27) and another on urban physicians in hospitals in China (28).
Orientation toward lifelong learning
In total, over seven thousand students, residents, and practicing physicians responded to the Jefferson Scale (N=7.269). The mean scores on the Jefferson Scale ranged between 41 and 47 across the individual studies (Table 1, 2).
Within each group, the individual study means on the Jefferson Scale varied more than what was expected due to chance (Figure 1; Q-values for students: 21.07, df=3, p<0.01; residents: 35.83, df=3, p<0.01; physicians: 31.01, df=3, p<0.01). Using the I2-statistic, around 90% of the variance of the observed study means was due to differences in the true study means in each group (students: I2=86%; residents: I2=92%; physicians: I2=90%).
Figure1.
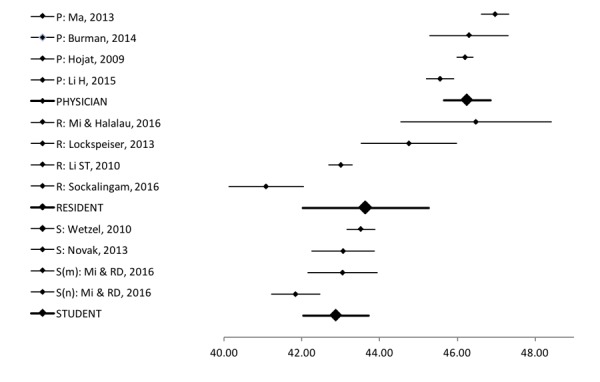
Forest plot of the summary measures (Jefferson Scale means and 95% CIs) for 12 independent data sets and the estimated group means: Student (S), Resident (R), Physician (P).
Note: S(m) – medical students; S(n) – nursing students.
Within each group, the individual study means on the Jefferson Scale varied more than what was expected due to chance (Figure 1; Q-values for students: 21.07, df=3, p<0.01; residents: 35.83, df=3, p<0.01; physicians: 31.01, df=3, p<0.01). Using the I2-statistic, around 90% of the variance of the observed study means was due to differences in the true study means in each group (students: I2=86%; residents: I2=92%; physicians: I2=90%).
As shown in , the estimated group means on the Jefferson Scalet ended to increasegradually:42.87 (95% CI: 42.04; 43.71) for students; 43.64 (95% CI: 42.02; 45.26) for residents; and 46.25 (95% CI: 45.66; 46.85) for physicians. The between-group Q-value indicated the overall significant difference in the estimated group means (44.60; df=2; p<0.05). Subsequent pair-wise comparisons (26) indicated significant mean differences between the students and physicians (z=6.42; p<0.001), and between residents and physicians (z=2.96, p=0.003).
Discussion
To measure trainees’ and practitioners’ orientation toward lifelong learning in health professions, the Jefferson Scale was developed and validated with these population (4-6,14-16) By examining the scale scores at various stages of the education and career continuum, the present study offers insights into the differences in the orientation toward lifelong learning between students, residents, and practicing health professionals. To the best of our knowledge, this is the only study in which the orientation toward lifelong learning in health professions has been examined along the education and career continuum. The findings of this study can be highlighted in three categories. First, the scores on the Jefferson Scale are optimistically high for all groups. Second, the scores were higher for practicing health professionals than trainees (students and residents). Third, of the three groups, residents had the greatest variability in their scores. These results are discussed in the light of the fact that medical schools and health professions programs are mandated by regulating bodies to foster trainees’ motivation to become lifelong learners, and health professionals are obligated to maintain expertise and acquire new knowledge.
The means on the Jefferson Scale for individual studies conducted with students, residents, and practicing health professionals ranged from 41-47, which is near the top of the scale given the maximum score on the Jefferson Scale is 56. One possible explanation for this is that individuals who choose to pursue education and career in health professions are already highly motivated and oriented toward lifelong learning. Future research should look for differences between university students in health professions and those in other programs.
Results of the group-level meta-analysis suggest that the orientation toward lifelong learning is higher for practicing health professionals than trainees (students and residents). Given the observed range of the individual study means, the differences in the estimated group means were relatively small. We did not find a significant difference in the group means between students and residents; however, both group means were significantly different from the physician group mean. One possible explanation for this finding is that trainees (students and residents) may tend to focus on their performance, including examinations, and not lifelong learning as much as practitioners. Nonetheless, although based on separate cohorts, it appears that the orientation toward lifelong learning continues to develop even after the completion of formal training.
We also observed a substantial variability in the individual study means within each group. Of note is somewhat larger variability in the orientation toward lifelong learning observed in residents compared to students and physicians. Considering that the Jefferson Scale encompasses four aspects of the orientation toward lifelong learning, specifically motivation, cognition, capabilities, and behavior, it would be informative to know which aspect(s) is/are responsible for the observed variation in the mean scores in the studies with residents. This, in turn, will have practical implications for the design and delivery of specific interventions in residency training, depending on the identified aspect(s).
Finally, several important limitations of this study are needed to be acknowledged to guide future research. The 14-item Jefferson Scale is relatively new and has been used in only a few studies so far. The overwhelming majority of the studies were from North America (8 USA and 1 Canada), which limits the generalizability of the findings to other countries and regions. Furthermore, the group of practicing health professionals was exclusively comprised of the studies conducted with practicing physicians. Future uses of the Jefferson Scale with learners and practitioners in a variety of health professions will allow for examining the orientation toward lifelong learning between and within health professions. Next, the studies included in each of the three groups had a substantial variability in participants’ characteristics (gender, years of practice, year in school, and residency program); however, due to the paucity of data, a meta-regression analysis to examine the effects of these characteristics could not be performed. If possible, future studies should also report scores on the Jefferson Scale for subgroups to be able to examine the differences within and between specific stages of education and career (e.g. pre-clinical and clinical; beginning, middle and end of residency training; by years of professional practice). Finally, reporting scores on the four key aspects of the Jefferson Scale - motivation, cognition, capabilities, and behavior - will provide granular insights into the orientation toward lifelong learning in health professionals.
Conclusions
In the reviewed studies, the orientation toward lifelong learning among students, residents, and practicing professionals was high and appeared to increase gradually along the education and career continuum. Although the link between the orientation toward lifelong learning and its behavioral manifestations in health professionals has been reported in the literature, much work in this area still needs to be done, including the examination of the impact oflifelong learning on patient care and positive clinical outcomes.
Footnotes
Funding/Support:This research was supported by the Social Sciences and Humanities Research Council (SSHRC), Grant # 430-2016-00267.
Conflict of interests: None declared.
References
- 1.Frank JR, Snell L, Sherbino J. CanMEDS 2015 Physician Competency Framework [internet]. Ottawa: Royal College of Physicians and Surgeons of Canada; [Accessed 6th January 2017] Available from: [http://canmeds.royalcollege.ca/uploads/en/framework/CanMEDS%202015%20Framework_EN_Reduced.pdf. ]
- 2.Interprofessional Education Collaborative Expert Panel. Core competencies for interprofessional collaborative practice: report of an expert panel [internet]. Washington, D.C.: Interprofessional Education Collaborative; 2011; [Accessed 6th January 2017] Available from: [https://members.aamc.org/eweb/upload/Core%20Competencies%20for%20Interprofessional%20Collaborative%20Practice%20(PDF).pdf. ]
- 3.American Association of Colleges of Nursing and Association of American Medical Colleges. Lifelong Learning in Medicine and Nursing [internet]. Washington, DC: American Association of Colleges of Nursing; 2010; [Accessed 6th January 2017] Available from: [http://www.aacn.nche.edu/education-resources/MacyReport.pdf. ]
- 4.Hojat M, Nasca TJ, Erdmann JB, Frisby A, Veloski JJ, Gonnella JS. An operational measure of physician lifelong learning: its development, components, and preliminary psychometric data. Med Teach. 2003;25:433–7. doi: 10.1080/0142159031000137463. [DOI] [PubMed] [Google Scholar]
- 5.Hojat M, Veloski JJ, Nasca TJ, Erdmann JB, Gonnella JS. Assessing physicians’ orientation toward lifelong learning. Journal of General Internal Medicine. 2006;21:931–6. doi: 10.1111/j.1525-1497.2006.00500.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hojat M, Veloski JJ, Gonnella JS. Measurement and correlates of physicians’ lifelong learning. Acad Med. 2009;84(8):1066–74. doi: 10.1097/ACM.0b013e3181acf25f. [DOI] [PubMed] [Google Scholar]
- 7.Murdoch-Eaton D, Whittle S. Generic skills in medical education: developing the tools for successful lifelong learning. Med Educ. 2012;46:120–8. doi: 10.1111/j.1365-2923.2011.04065.x. [DOI] [PubMed] [Google Scholar]
- 8.Duffy FD, Holmboe ES. Self-assessment in life-long learning and improving performance in practice: physician know thyself. JAMA. 2006;296:1137–9. doi: 10.1001/jama.296.9.1137. [DOI] [PubMed] [Google Scholar]
- 9.Hoban JD, Lawson SR, Mazmanian PE, Best AM, Seibel HR. The Self-Directed Learning Readiness Scale: a factor analysis study. Med Educ. 2005;39(4):370–9. doi: 10.1111/j.1365-2929.2005.02140.x. [DOI] [PubMed] [Google Scholar]
- 10.Schraw G, Dennison RS. Assessing metacognitive awareness. Contemporary Educational Psychology. 1994;19:460–75. [Google Scholar]
- 11.Bligh J. The S-SDLRS: A short questionnaire about self-directed learning. Postgraduate Education for General Practice. 1993;4:121–5. [Google Scholar]
- 12.Oddi LF. Development and validation of an instrument to identify self-directed continuing learners. Adult Education Quarterly. 1986;36:97–107. [Google Scholar]
- 13.Burman NJ, Boscardin CK, van Schaik SM. Career-long learning: relationship between cognitive and metacognitive skills. Med Teach. 2014;36:715–23. doi: 10.3109/0142159X.2014.909010. [DOI] [PubMed] [Google Scholar]
- 14.Wetzel AP, Mazmanian PE, Hojat M, Kreutzer KO, Carrico RJ, Carr C, et al. Measuring medical students orientation toward lifelong learning: a psychometric evaluation. Acad Med. 2010;85:S41–S44. doi: 10.1097/ACM.0b013e3181ed1ae9. [DOI] [PubMed] [Google Scholar]
- 15.Novak M, Palladino C, Ange B, Richardson D. Measuring health professions students’ orientation toward lifelong learning. Journal of Allied Health. 2014;43(3):146–9. [PubMed] [Google Scholar]
- 16.Mi M, Riley-Doucet C. Health professions students’ lifelong learning orientation: associations with information skills and self-efficacy. Evidence Based Library and Information Practice. 2016;11(2):121–35. [Google Scholar]
- 17.Mi M, Halalau A. A pilot study exploring the relationship between lifelong learning and factors associated with evidence-based medicine. International Journal of Medical Education. 2016;7:214–9. doi: 10.5116/ijme.576f.a2ca. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sockalingam S, Wiljer D, Yufe S, Knox MK, Fefergrad M, Silver I, et al. The relationship between academic motivation and lifelong learning during residency: a study of psychiatry residents. Acad Med. 2016;91(10):1423–30. doi: 10.1097/ACM.0000000000001256. [DOI] [PubMed] [Google Scholar]
- 19.Lockspeiser TM, Schmitter PA, Lane L, Hanson JL, Rosenberg AA, Park YS. Assessing residents’ written learning goals and goal writing skill: validity for the Learning Goal Scoring Rubric. Acad Med. 2013;88:1558–63. doi: 10.1097/ACM.0b013e3182a352e6. [DOI] [PubMed] [Google Scholar]
- 20.Li ST, Tancredi DJ, Co JP, West DC. Factors associated with successful self-directed learning using individualized learning plans during pediatric residency. Academic Pediatrics. 2010;10:124–30. doi: 10.1016/j.acap.2009.12.007. [DOI] [PubMed] [Google Scholar]
- 21.Hojat M, Kowitt B, Doria C, Gonnella JS. Career satisfaction and professional accomplishments. Med Educ. 2010;44:969–76. doi: 10.1111/j.1365-2923.2010.03735.x. [DOI] [PubMed] [Google Scholar]
- 22.Naing C, Wai VN, Durham J, Whittaker MA, Win NN, Aung K, et al. A systematic review and meta-analysis of medical students’ perspectives on the engagement in research. Medicine. 2015;94(28):1–9. doi: 10.1097/MD.0000000000001089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moher D, Liberati A, Tetzlaff J, Altman D. The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Medicine. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Glass G, Hoppkins K. Statistical methods in education and psychology. 3rd ed. Needham Heights, MA: Allyn & Bacon; 1996. [Google Scholar]
- 25.Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions Version 5.1.0. The Cochrane Collaboration; 2011; [Accessed 6th January 2017] [updated March 2011] Available from: [http://handbook.cochrane.org. ]
- 26.Borenstein M, Hedges L, Higgins J, Rothstein H. Comprehensive meta-analysis. 2nd ed. Englewood, NJ: Biostat; 2005. [Google Scholar]
- 27.Li H, Wang Z, Jiang N, Liu Y, Wen D. Lifelong learning of Chinese rural physicians: preliminary psychometrics and influencing factors. BMC Medical Education. 2015;15:192–202. doi: 10.1186/s12909-015-0460-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li H, Sun Y, Wen D. Investigation and influencing factors of clinicians’ orientation toward lifelong learning. China Higher Medical Education. 2013;9:5–6. [Google Scholar]


