Abstract
Background
Insomnia treatment using an internet-based cognitive–behavioural therapy for insomnia (CBT-I) program reduces depression symptoms, anxiety symptoms and suicidal ideation. However, the speed, longevity and consistency of these effects are unknown.
Aims
To test the following: whether the efficacy of online CBT-I was sustained over 18 months; how rapidly the effects of CBT-I emerged; evidence for distinct trajectories of change in depressive symptoms; and predictors of these trajectories.
Method
A randomised controlled trial compared the 6-week Sleep Healthy Using the Internet (SHUTi) CBT-I program to an attention control program. Adults (N=1149) with clinical insomnia and subclinical depression symptoms were recruited online from the Australian community.
Results
Depression, anxiety and insomnia decreased significantly by week 4 of the intervention period and remained significantly lower relative to control for >18 months (between-group Cohen’s d=0.63, 0.47, 0.55, respectively, at 18 months). Effects on suicidal ideation were only short term. Two depression trajectories were identified using growth mixture models: improving (95%) and stable/deteriorating (5%) symptoms. More severe baseline depression, younger age and limited comfort with the internet were associated with reduced odds of improvement.
Conclusions
Online CBT-I produced rapid and long-term symptom reduction in people with subclinical depressive symptoms, although the initial effect on suicidal ideation was not sustained.
Declaration of interest
P.J.B. has received grants from the National Health and Medical Research Council (NHMRC) during the conduct of the study. H.C. has received grants from the NHMRC and the Australian Research Council during the conduct of the study. L.M.R. receives research funding from the National Institutes of Health (NIH) that, in part, focuses on insomnia. F.P.T. and L.M.R. have equity ownership in BeHealth Solutions (Charlottesville, VA, USA), a company that develops and makes available products related to the research reported in this manuscript. BeHealth Solutions has licensed the SHUTi program and the software platform on which it was built from the University of Virginia. The terms of this arrangement have been reviewed and approved by the University of Virginia in accordance with its conflict of interest policy. N.G. has received grants from the NHMRC during the conduct of the study and personal fees from Lundbeck, Servier and Janssen outside the submitted work.
Copyright and usage
© The Royal College of Psychiatrists 2017. This is an open access article distributed under the terms of the Creative Commons Non-Commercial, No Derivatives (CC BY-NC-ND) license.
Major depressive disorder (MDD) is a common mental health problem with considerable disease burden.1 Although a proportion of MDD cases can be prevented using cognitive–behavioural therapy (CBT) for depression,2 a number of factors, including the stigma associated with psychological treatment, operate as barriers to individuals at risk of depression receiving appropriate intervention before symptoms reach clinical levels.3 Because of the overlap of insomnia with a broad range of mental health problems, treatment of insomnia has been suggested as a potential transdiagnostic approach to treating and preventing mental health problems such as MDD.4 Insomnia and MDD often co-occur.5–7 Insomnia is a common symptom of MDD,5 and a considerable proportion of people with insomnia also have MDD. Insomnia is also a risk factor for the onset of MDD,8,9 complicates depression treatment10 and increases risk of depression relapse.11 Insomnia also co-occurs with a range of other mental health problems, including anxiety disorders and psychosis, as well as suicide.8,12–14
Given the extensive evidence for the role of insomnia in the development and maintenance of depression, there is clear potential for CBT for insomnia (CBT-I) in the prevention of depression provided that it is delivered in an accessible and affordable form. The uptake of a CBT-I intervention may be higher than for a depression-focused intervention, as insomnia is less stigmatised in the community than depression.15 In addition, delivering CBT–I interventions using an internet-based program may further maximise accessibility and the potential for dissemination of effective interventions.16 Although there have been trials testing the effectiveness of CBT-I in individuals with depression,17–20 the trial reported in this article was the first to assess whether CBT-I is effective for preventing depression in an at-risk sample. The internet-based automated intervention Sleep Healthy Using the Internet (SHUTi) was used in this study. SHUTi has previously been demonstrated to be effective in treating insomnia symptoms.21
Initial outcomes of the present randomised controlled trial (RCT) have already been reported, with depression, insomnia and anxiety symptoms significantly decreasing in the CBT-I group relative to an attention control condition (Cohen’s d=0.48, 0.36 and 0.83, respectively) at 6 months post-intervention.22 Depression criteria on the Patient Health Questionnaire-9 (PHQ-9)23 were met by 6% in the CBT-I condition and 14% in the control condition at 6 months.22 Data are now available on long-term (12- and 18-month) outcomes from this trial. This paper reports on these long-term outcomes, testing the effectiveness of the SHUTi program in preventing depression in a population-based sample of individuals with clinical insomnia and elevated but subclinical depression symptoms. Few trials have examined the longevity of effects, that is, whether positive outcomes of health interventions are sustained in the long term.24 Longevity of effects is important, as depression can be a chronic and recurrent condition, with many individuals experiencing relapse or residual subclinical symptoms.25
This study also examined when change occurred during the course of the intervention. Participants were assessed every 2 weeks while completing the intervention. Interventions may have an immediate or delayed impact, and effects may endure or subside over time.26 Rapid initial effects may also be predictive of long-term response to treatment.27 By better understanding how depression symptoms change during the course of the intervention, it may be possible to identify the ‘dose–response’ profile of the intervention for clinical improvement and to intervene early with individuals who do not rapidly respond.28,29 Finally, the study identified whether there were distinct trajectories of depression symptoms in the participants who received the CBT-I program. Using growth mixture models, it is possible to identify subgroups of participants on the basis of latent change trajectories in depression scores.30 Predictors of subgroup membership can then be used to identify characteristics of participants who had limited depression response to the intervention. This information may be used to further inform the delivery of targeted or tailored interventions.
In summary, the aim of this article is first to present the long-term outcomes of the GoodNight Study, an RCT that tested the effectiveness of the SHUTi online CBT-I program on the indicated prevention of MDD. Second, this study aims to test how rapidly depression symptoms change in response to CBT-I. Third, this study aims to identify trajectories of change in depression symptoms and to assess predictors of these trajectories to determine whether response to CBT-I might be moderated by individual characteristics.
Method
Participants
Australian adults aged 18–64 years were recruited online between April 2013 and June 2014, with follow-up data collection completed by September 2015. Advertisements were delivered through a social network site (Facebook), websites of sleep or mental health associations, and media releases. Initial inclusion criteria, via online self-report screening, were the presence of depression symptoms, as measured by scores >4 and <20 on the PHQ-9,23 and the presence of significant insomnia symptoms, as measured by a score ≥3 on at least one of the first four items of the Bergen Insomnia Scale and a score ≥3 on at least one of the last two items.31 Absence of a 2-week (current) diagnosis of MDD or lifetime bipolar disorder, and diagnostic confirmation of insomnia were established via the telephone-administered Mini-International Neuropsychiatric Interview (MINI)32 and Morin’s modified diagnostic insomnia interview.33,34 These criteria include (a) sleep-onset insomnia and/or sleep-maintenance insomnia (>30 min for at least 3 nights/week); (b) insomnia symptoms lasting at least 1 month; and (c) sleep disturbance (or associated daytime fatigue) causing significant distress or impairment in social, occupational or other areas of functioning.
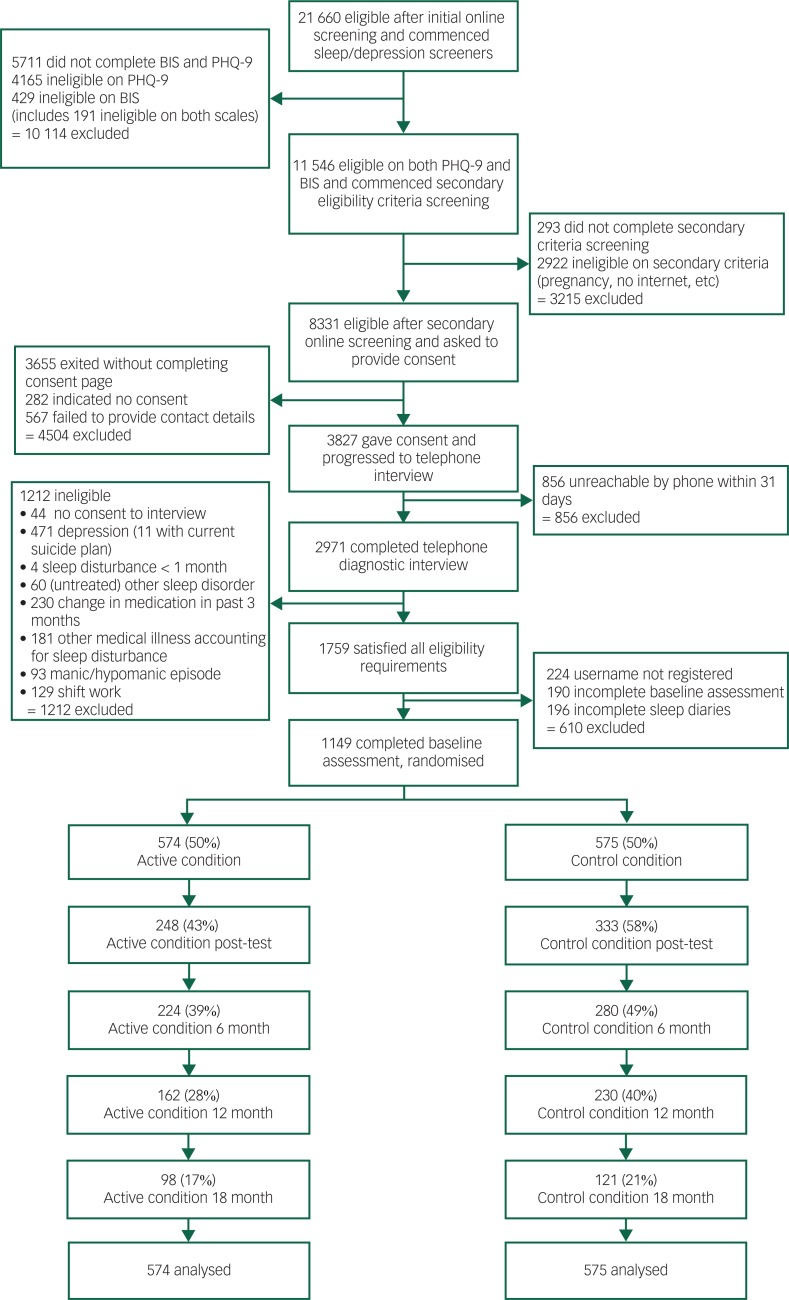
Exclusion criteria included shift work, pregnancy, or work, family or other commitments that interfered with regular night-time sleep patterns, or time of awakening outside the hours of 4 am and 10 am, or bedtime outside the hours of 8 pm and 2 am, more than twice a week. Other exclusion criteria were absence of reliable internet access; difficulty reading English; reported diagnosis of psychosis, schizophrenia or bipolar disorder by a psychiatrist; or current involvement in a non-medication treatment program for insomnia with a health professional. We also excluded individuals with an untreated sleep disorder other than insomnia, medication changes in the past 3 months, a medical disorder accounting for their insomnia or reported suicidal plans or attempts in the previous 2 weeks. Participants who did not complete 10 online sleep diaries within a 14-day period, within 21 days of sleep-diary commencement, did not proceed to randomisation. A CONSORT diagram of the study flow is provided in Fig. 1. The target sample size of 972 participants was exceeded. This target was based on detecting our secondary outcome of MDD with 80% power and a 40% reduction in risk in a sample with a baseline incidence of 15%. The study was approved by the Australian National University Human Ethics Committee. All participants provided informed consent. The study protocol and 6-month outcomes have been published.22,35
Fig. 1. CONSORT diagram of participant flow in the trial.
Randomisation and masking
Participants were randomly assigned on a 1:1 basis to receive either SHUTi,21 a 6-week, modular, online insomnia program based on CBT-I, or HealthWatch,36 an interactive, attention-matched, internet-based placebo control program. Randomisation was computer-generated and integrated into the trial management software, stratified by age and gender. Telephone-based interviewers, statisticians and chief investigators were masked to group allocation.
Procedure and intervention
Participants visited a web portal that managed screening, consent, randomisation, delivery of sleep diaries and all assessments, delivery of HealthWatch and linkage to SHUTi. Participants submitted sleep diaries for a period of 2 weeks before randomisation and start of the study program. All assessment surveys were completed online, except for the diagnostic interviews, which were administered via telephone. SHUTi provides six sequential modules consisting of an overview of insomnia, two behavioural modules focusing on sleep restriction and stimulus control, cognitive restructuring, sleep hygiene and relapse prevention.34 An 11-item daily sleep diary,37 completed on at least 5 of 7 days, was required to advance from the first to the second module so the system could establish an algorithmically defined sleep window. Ongoing sleep diaries were also required for the participant to receive updated sleep window recommendations. The comparison arm received the online HealthWatch program, which has no specific mental health or sleep-related content and is not associated with therapeutic reductions in depression.36,38 Modules contained information about environmental health, nutrition, heart health, activity, medication, oral health, blood pressure and cholesterol, calcium and back pain, in addition to weekly surveys of these topics. Once a participant was randomly assigned to their respective web program, email reminders were sent to notify participants of availability of program modules, sleep diaries and assessments when appropriate. A telephone call was also made at the time of the 6-month follow-up to conduct a MINI assessment and remind non-responders to complete the assessment. Participants received two automated email reminders to complete each of the 12- and 18-month follow-up assessments. No additional reminders were given to complete assessments.
Measures
The primary outcome was depression symptoms, as measured with the PHQ-923 excluding the sleep item (henceforth referred to as the PHQ-9NS). Secondary outcomes included insomnia severity, suicidal ideation and generalised anxiety symptoms. Potential moderators of depression outcome were assessed at baseline and included severity of depression symptoms, initial insomnia severity, presence of suicidal ideation, generalised anxiety symptoms, treatment preference, medication use, age, gender and education. Insomnia severity was assessed with the Insomnia Severity Index (ISI),39 a 7-item scale with scores ranging from 0 to 28; scores of 15 or more are indicative of clinical insomnia. Suicidal ideation was measured using the Psychiatric Symptom Frequency scale (PSF).40 Symptoms of generalised anxiety disorder were measured with the Generalized Anxiety Disorder 7-item scale (GAD-7),41 with scores ranging from 0 to 21.
Predictors of depression symptom trajectories were also examined. Potential predictors included symptom variables (symptoms of depression, GAD, insomnia, suicidality), age, gender, years of education, marital status (partnered v. not), location (rural v. non-rural), comfort with the internet and participant preference for treatment allocation. Comfort with the internet was based on a single question, ‘How familiar and comfortable are you with using the internet?’, rated on a four-choice Likert scale, with ‘very comfortable’ v. to ‘fairly/not particularly/not at all comfortable’. Participant preference for the allocated treatment program was based on which of the two conditions the participant preferred to receive, assessed before randomisation: ‘Monitoring your sleep activity and then doing online training so that you can change your sleep routine’ or ‘Monitoring your sleep activity, being provided with health information, and being asked your views about the possible causes of your sleep problems’. Participants whose allocated program matched their preference and those who chose ‘no preference’ were classified as ‘matched preference’, whereas the remainder were classified as ‘mismatched preference’.
Analysis
Effectiveness of the SHUTi program relative to the HealthWatch attention control was assessed using mixed model repeated measures ANOVA (MMRM)42 to account for missing data and to include all available data for participants analysed in the trial. This approach provides an intention-to-treat analysis, yielding unbiased estimates of intervention effects. An unstructured variance–covariance matrix was assumed, and degrees of freedom (d.f.) were estimated using Satterthwaite’s method. Outcomes were assessed at time points before (baseline), within (2/4/6/8 weeks of intervention, excluding the PSF) and after (immediate/6-/12-/18-month follow-up) the delivery of the intervention. MMRM analyses were repeated with adjustment for factors that were significantly different between groups at baseline and factors associated with differential attrition.
To examine trajectories of change in depression, a linear growth mixture model was estimated in the SHUTi subsample. This analysis identifies latent classes (subgroups) of participants with distinct trajectories of change. Within-class variation is represented by random effects, and all available data are used for the estimation. We first specified a one-class model, repeating analyses until the addition of classes was found to have no significant improvement on model fit, based on the Bootstrap Likelihood Ratio Test (BLRT).43 The BLRT method uses bootstrap samples to estimate the distribution of the log likelihood difference test statistic, where the P value is used to compare the increase in model fit between models. Predictors of class membership were then examined using logistic regression. All analyses were conducted using SPSS version 23 (IBM Corp., Chicago, IL, USA), except for the growth mixture model, conducted using Mplus Version 7.4 (Muthen & Muthen, Los Angeles, CA, USA). The trial is registered with the Australian and New Zealand Clinical Trials Registry, number ACTRN12611000121965.
Results
Baseline sample characteristics are provided in Table DS1. The only characteristic with significant differences between intervention groups was preference match (P<0.001), reflecting greater preferences in both groups for the SHUTi condition. Mean PHQ-9 scores were in the mild-range for both intervention groups. Participants had a mean age of 43 years (s.d.=12), 74% were female, 62% were in a relationship, 78% were employed and 53% had completed a bachelor’s degree or more. Fig. 1 presents the CONSORT flowchart of participants through the trial. Only 34% of participants completed the 12-month assessment, and 19% of participants completed the 18-month assessment, with an additional eight participants providing primary outcome data at each time point (although not completing the full assessment). Based on logistic regression models that included symptom measures, demographics, preference match and condition, factors significantly associated with assessment attrition included younger age (P<0.001 at 12/18 months), less educational attainment (P=0.044 at 12 months, P=0.015 at 18 months) and being in the SHUTi condition (P<0.001 at 12 months, P=0.032 at 18 months).
Changes during the intervention and long-term outcomes
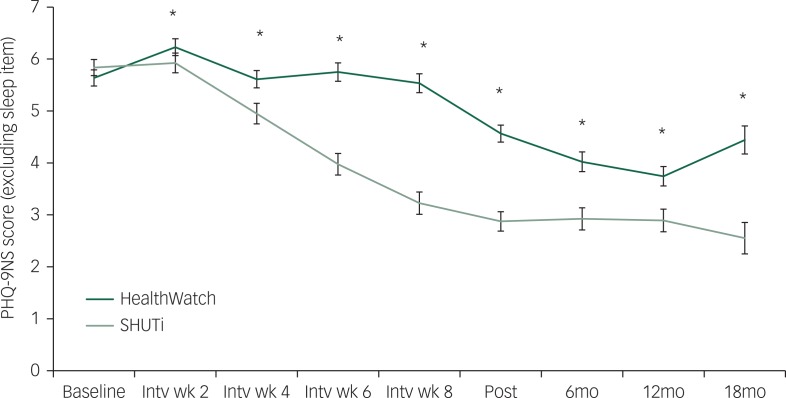
Fig. 2 displays the primary depression outcome based on estimated marginal means (s.e.) from the MMRM analyses. As indicated in Fig. 2, the interaction between condition and time was significant for depression symptoms (F8, 543.8=13.9, P<0.001), with significant differences observed at every time point during and after the delivery of the intervention. However, post hoc within-group tests indicated that significant declines in depression symptoms occurred in the SHUTi condition only at 4 weeks and beyond, with no significant change at 2 weeks (t326.6=0.62, P=0.54), suggesting that the between-group depression effect may have reflected early deterioration in the control group. The between-group interaction effects of the intervention on insomnia severity (F8, 539.4=34.6, P<0.001) and generalised anxiety symptoms (F8, 526.3=11.3, P<0.001) were robust across all time points, with significant reductions from baseline to every time point during and after the intervention delivery. These effects demonstrate that the SHUTi program was effective in significantly reducing depression, generalised anxiety and insomnia symptoms by 4 weeks.
Fig. 2. Mean depression scores for PHQ-9NS (PHQ-9 without sleep item) over time in the SHUTi and HealthWatch conditions, estimated from mixed model repeated measures analysis. *P<0.05 for group×time interaction effect; ‘intv wk’: intervention week; ‘mo’: month; error bars represent standard errors of the marginal mean estimates.
Long-term effects of the intervention on symptoms of depression and generalised anxiety, along with insomnia severity, were observed at both 12 and 18 months. At 12 months, 3% of SHUTi group completers had PHQ-9 scores ≥10, compared with 13% of HealthWatch completers (Fisher’s exact P=0.001). At 18 months, the disparity was greater (2% v. 19% in SHUTi v. HealthWatch, P<0.001). However, the effect of SHUTi on suicidality was not significant overall (F4, 459.5=2.2, P=0.069), with a significant difference only at post-test (t698.3=−2.68, P=0.007). Between-group effect sizes (Cohen’s d) are reported in Table 1. For depression, anxiety and insomnia, effect sizes were greatest at Week 8 of the intervention, decreasing gradually to the 18-month assessment. Table DS2 provides both estimated marginal means (s.e.) and observed means (s.d.) for each of the four outcomes at each time point. Inclusion of factors associated with differential attrition (age, education) or between-group baseline differences (preference match) in these models did not change the significance of effects on depression, anxiety or insomnia at any time point, nor on suicidality at post-test.
Table 1. Effect sizes and P-values testing the effectiveness of SHUTi versus HealthWatch at each time point, relative to baseline (n=1149).
| PHQ-9NS depression | GAD-7 anxiety | ISI insomnia | PSF suicidality | |||||
|---|---|---|---|---|---|---|---|---|
| d | P | d | P | d | P | d | P | |
| Intervention week 2 | 0.17 | 0.028 | 0.23 | 0.003 | 0.30 | <0.001 | ||
| Intervention week 4 | 0.34 | <0.001 | 0.38 | <0.001 | 0.78 | <0.001 | ||
| Intervention week 6 | 0.68 | <0.001 | 0.61 | <0.001 | 1.06 | <0.001 | ||
| Intervention week 8 | 0.78 | <0.001 | 0.65 | <0.001 | 1.27 | <0.001 | ||
| Post-test | 0.60 | <0.001 | 0.50 | <0.001 | 1.10 | <0.001 | 0.13 | 0.007 |
| 6 months | 0.41 | <0.001 | 0.36 | <0.001 | 0.83 | <0.001 | 0.08 | 0.303 |
| 12 months | 0.43 | 0.001 | 0.39 | 0.001 | 0.73 | <0.001 | 0.20 | 0.092 |
| 18 months | 0.63 | <0.001 | 0.47 | 0.002 | 0.55 | <0.001 | 0.25 | 0.171 |
PHQ-9NS, Patient Health Questionnaire-9 depression score excluding sleep disturbance item; GAD-7, Generalized Anxiety Disorder-7; ISI, Insomnia Severity Index; PSF, Psychiatric Symptom Frequency scale; bold values indicate P<0.05 from mixed model repeated measures analyses for time×condition interaction effects; Cohen’s d represents between-groups effect size estimates based on observed means/s.d.; refer to Table DS2 for estimated means (s.e.) and observed means (s.d.) at each time point.
Trajectories of change
Distinct trajectories of change in depression symptoms within the CBT-I condition were identified using growth mixture modelling. Based on the BLRT, there was a significant difference in fit for two classes v. one (P<0.001) and for three classes v. two (P<0.001). However, one of the three classes included only 3% of participants, whereas the two-class solution included 5% of participants in the smaller class. The two-class model also had acceptable entropy (0.82) and was consequently selected. Depression scores over time within the two classes are shown in Fig. DS1. Based on the trajectories observed, the classes were labelled as ‘stable/deteriorating’ (5% of the sample) and ‘improving’ (95%) depression symptoms. The ‘improving’ group demonstrated significant symptom improvement relative to ‘stable/deteriorating’ at 4 weeks and beyond. The within-group effect sizes were consistent and large within the ‘improving’ class: d=0.92, 0.94, 0.93 and 1.01 at post, 6, 12 and 18 months, respectively. In contrast, the within-group effect size in the ‘stable/deteriorating’ class was d=0.43 at post-test but virtually zero at follow-ups (−0.03, 0.03, −0.04).
Baseline factors associated with class membership were estimated using binary logistic regression analysis (Table 2). Factors significantly associated with membership of the stable/deteriorating depression class were higher baseline depression scores, younger age and limited comfort with using the internet. The Nagelkerke R2 for the model was 0.28, suggesting other unmeasured factors may be associated with class membership.
Table 2. Logistic regression testing predictors of latent class membership (improving v. stable/deteriorating) in the SHUTi condition (n=574).
| Unstandardised estimate | s.e. | χ2 | d.f. | OR | P | |
|---|---|---|---|---|---|---|
| Intercept | −1.68 | 1.45 | 1.35 | 1 | 0.245 | |
| Age | −0.05 | 0.02 | 5.29 | 1 | 0.95 | 0.021 |
| Depression symptoms | 0.35 | 0.07 | 22.77 | 1 | 1.42 | <0.001 |
| Insomnia symptoms | 0.05 | 0.05 | 0.85 | 1 | 1.05 | 0.356 |
| Anxiety symptoms | −0.11 | 0.06 | 3.15 | 1 | 0.90 | 0.076 |
| Suicidality score | 0.00 | 0.09 | 0.00 | 1 | 1.00 | 0.974 |
| Gender: female v. male | −0.52 | 0.48 | 1.18 | 1 | 0.59 | 0.278 |
| Educational attainment | 5.53 | 4 | 0.237 | |||
| Less than high school v. higher degree | −1.19 | 0.92 | 1.67 | 1 | 0.30 | 0.197 |
| High school grad v. higher degree | −0.95 | 0.90 | 1.12 | 1 | 0.39 | 0.289 |
| Certificate/diploma/trade v. higher degree | −1.42 | 0.63 | 5.09 | 1 | 0.24 | 0.024 |
| Bachelor degree v. higher degree | −0.97 | 0.58 | 2.80 | 1 | 0.38 | 0.094 |
| Married or de facto relationship v. not | −0.27 | 0.45 | 0.36 | 1 | 0.76 | 0.551 |
| High comfort with internet v. less than high | −1.33 | 0.61 | 4.67 | 1 | 0.26 | 0.031 |
| Preference match v. mismatch | 0.15 | 0.46 | 0.10 | 1 | 1.16 | 0.750 |
| Rural v. non-rural location | 0.49 | 0.51 | 0.93 | 1 | 1.63 | 0.335 |
PHQ-9NS, Patient Health Questionnaire-9 without sleep item; GAD-7, Generalized Anxiety Disorder-7; ISI, Insomnia Severity Index; PSF, Psychiatric Symptom Frequency scale; OR, odds ratio; bold values indicate P<0.05.
Discussion
The SHUTi online CBT-I program was effective for reducing depression within the first 4 weeks of delivery and continued to be effective in reducing symptoms of depression, anxiety and insomnia for at least 18 months beyond completion of the program. Effect sizes were moderate to large, suggesting the effect of CBT-I on depression symptoms, in addition to insomnia severity and anxiety symptoms, was substantial and likely to be clinically meaningful in a prevention context. The magnitude of the depression effects was consistent with internet-based treatment programs for depression (d=0.56),44 similar to face-to-face depression treatment programs (g=0.80)45 and greater than most online depression prevention programs (d=0.32).46,47 Effects on anxiety symptoms were also moderate, although more modest than those seen in internet-based anxiety treatment trials (d=0.96),46 whereas insomnia effects were marginally stronger than those found in a meta-analysis of internet interventions for insomnia (g=0.60).16 Few depression prevention programs collect long-term follow-up data to demonstrate enduring effectiveness. By contrast, the current findings indicate that insomnia treatment is associated with sustained improvements in depression symptoms, in addition to insomnia and anxiety, in a community-based setting.
The effects of CBT-I on suicidal ideation were not sustained at follow-up. This finding may reflect a baseline restriction of range, as individuals who initially reported recent suicide plan or attempt were excluded from the study. Some depression programs have shown subsidiary effects on suicidality,48,49 and insomnia has associations with suicidal ideation13,14 with a plausible biological basis.50 The prevalence of suicidality in this study may have been too low and transitory to find robust long-term effects, relative to symptoms of depression and anxiety. Nevertheless, given the short-term effects of insomnia treatment on suicidal ideation in this program, further research is warranted on whether insomnia treatment might be an effective approach for the prevention of suicide attempts.
Using growth mixture models, this study identified two trajectories of depression symptoms within the intervention condition, labelled ‘improving’ and ‘stable/deteriorating’. The vast majority of participants (95%) were in the ‘improving’ depression class. More severe depression symptoms, although still subclinical, were associated with approximately 42% higher odds of being in the stable/deteriorating class, per one-unit increase on the PHQ-9NS. This association suggests that individuals with more severe subclinical depression symptoms may require adjunctive intervention elements targeting depression to achieve a better depression outcome. This finding is in contrast to a previous meta-analysis that found greater depression severity to be associated with increased treatment response.51 It may be that the current sample, which excluded participants with clinical depression, responded differently to those in treatment trials. Alternatively, the growth mixture modelling methodology may have identified characteristics of non-improving participants that are obscured within aggregated data. Further research may be required to better understand this divergence. There was also a significant effect of greater comfort with the internet being associated with greater likelihood of depression symptoms improving from online CBT-I, suggesting that discomfort with the internet may reduce efficacy of online treatment. An independent effect of younger age on membership of the stable/deteriorating class was also observed, suggesting that some young people may have engaged less with the program.22
This study was the first to trial the long-term outcomes of an insomnia program in preventing depression, using a large community-based sample. Importantly, the intervention was fully automated, providing significant potential for widespread scalability. However, some limitations should be acknowledged in interpreting the findings. First, there was high attrition from assessments at later time points, particularly in the active treatment group. Nevertheless, the study remained powered to find significant moderate effects between conditions at 18 months. Second, emergence of clinical depression was low in the sample22 and no clinical assessment was conducted at later time points. Consequently, the degree to which reductions in symptoms translated into prevention of new cases of major depression remains unclear. A related limitation was that some participants may have met criteria for mild depression, potentially blurring the distinction between prevention and treatment.
In conclusion, this study indicated that internet-based CBT treatment for insomnia provided an effective approach to preventing depression, which was sustained for at least 18 months. The effects of CBT-I on depression, anxiety and insomnia emerged rapidly in the first 4 weeks of the program. Growth mixture modelling indicated 95% of community-based participants receiving CBT-I showed improving depression trajectories, with participants with less severe depression, greater comfort with the internet or older age being more likely to have a positive trajectory. There is a need for further translational research to identify optimal or tailored approaches to engage users in evidence-based prevention programs such as SHUTi. Implementing indicated prevention programs that focus on treating insomnia may result in considerable gains in the prevention of depression within the community.
Acknowledgements
The authors thank Kanupriya Hehir, Marina Talevski and Jade Chan for providing research assistance; Kylie Bennett and Anthony Bennett for helping design the flow of the trial and the software for the assessment and administration components; Professor John Cunningham for his supervisory input; the interviewers who collected data; and Dr Fiona Shand for offering clinical support services to participants who sought further treatment.
Funding
This trial was funded by NHMRC project grant 1005867. H.C. is supported by NHMRC fellowship 1056964. P.J.B. is supported by NHMRC fellowship 1083311, and at the time of the study, K.M.G. was supported by NHMRC fellowship 1059620. The funding body had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the manuscript; and decision to submit the manuscript for publication. The study was approved by the Australian National University Human Ethics Committee (protocol number 2011/041). The trial is registered with the Australian and New Zealand Clinical Trials Registry, number ACTRN12611000121965.
References
- 1.Ferrari AJ, Charlson FJ, Norman RE, Patten SB, Freedman G, Murray CJ, et al. Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS Med 2013; 10: e1001547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.van Zoonen K, Buntrock C, Ebert DD, Smit F, Reynolds CF 3rd, Beekman AT, et al. Preventing the onset of major depressive disorder: a meta-analytic review of psychological interventions. Int J Epidemiol 2014; 43: 318–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gulliver A, Griffiths KM, Christensen H. Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatry 2010; 10: 113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harvey AG. A transdiagnostic approach to treating sleep disturbance in psychiatric disorders. Cogn Behav Ther 2009; 38 (Suppl 1): 35–42. [DOI] [PubMed] [Google Scholar]
- 5.Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA 1989; 262: 1479–84. [DOI] [PubMed] [Google Scholar]
- 6.Franzen PL, Buysse DJ. Sleep disturbances and depression: risk relationships for subsequent depression and therapeutic implications. Dialogues Clin Neurosci 2008; 10: 473–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Taylor DJ, Lichstein KL, Weinstock J, Sanford S, Temple JR. A pilot study of cognitive-behavioural therapy of insomnia in people with mild depression. Behav Ther 2007; 38: 49–57. [DOI] [PubMed] [Google Scholar]
- 8.Batterham PJ, Glozier N, Christensen H. Sleep disturbance, personality and the onset of depression and anxiety: prospective cohort study. Aust N Z J Psychiatry 2012; 46: 1089–98. [DOI] [PubMed] [Google Scholar]
- 9.Baglioni C, Battagliese G, Feige B, Spiegelhalder K, Nissen C, Voderholzer U, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord 2011; 135: 10–9. [DOI] [PubMed] [Google Scholar]
- 10.Dew MA, Reynolds CF 3rd, Houck PR, Hall M, Buysse DJ, Frank E, et al. Temporal profiles of the course of depression during treatment. Predictors of pathways toward recovery in the elderly. Arch Gen Psychiatry 1997; 54: 1016–24. [DOI] [PubMed] [Google Scholar]
- 11.Dombrovski AY, Cyranowski JM, Mulsant BH, Houck PR, Buysse DJ, Andreescu C, et al. Which symptoms predict recurrence of depression in women treated with maintenance interpersonal psychotherapy? Depress Anxiety 2008; 25: 1060–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cohrs S. Sleep disturbances in patients with schizophrenia: impact and effect of antipsychotics. CNS Drugs 2008; 22: 939–62. [DOI] [PubMed] [Google Scholar]
- 13.Goldstein TR, Bridge JA, Brent DA. Sleep disturbance preceding completed suicide in adolescents. J Consult Clin Psychol 2008; 76: 84–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bernert RA, Kim JS, Iwata NG, Perlis ML. Sleep disturbances as an evidence-based suicide risk factor. Curr Psychiatry Rep 2015; 17: 554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stinson K, Tang N, Harvey A. Barriers to treatment seeking in primary insomnia in the United Kingdom: a cross-sectional perspective. Sleep 2006; 29: 1643–6. [DOI] [PubMed] [Google Scholar]
- 16.Zachariae R, Lyby MS, Ritterband LM, O’Toole MS. Efficacy of internet-delivered cognitive-behavioural therapy for insomnia – a systematic review and meta-analysis of randomized controlled trials. Sleep Med Rev 2016; 30: 1–10. [DOI] [PubMed] [Google Scholar]
- 17.Ashworth DK, Sletten TL, Junge M, Simpson K, Clarke D, Cunnington D, et al. A randomized controlled trial of cognitive behavioural therapy for insomnia: an effective treatment for comorbid insomnia and depression. J Couns Psychol 2015; 62: 115–23. [DOI] [PubMed] [Google Scholar]
- 18.Manber R, Edinger JD, Gress JL, San Pedro-Salcedo MG, Kuo TF, Kalista T. Cognitive behavioural therapy for insomnia enhances depression outcome in patients with comorbid major depressive disorder and insomnia. Sleep 2008; 31: 489–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wagley JN, Rybarczyk B, Nay WT, Danish S, Lund HG. Effectiveness of abbreviated CBT for insomnia in psychiatric outpatients: sleep and depression outcomes. J Clin Psychol 2013; 69: 1043–55. [DOI] [PubMed] [Google Scholar]
- 20.Watanabe N, Furukawa TA, Shimodera S, Morokuma I, Katsuki F, Fujita H, et al. Brief behavioural therapy for refractory insomnia in residual depression: an assessor-blind, randomized controlled trial. J Clin Psychiatry 2011; 72: 1651–8. [DOI] [PubMed] [Google Scholar]
- 21.Ritterband LM, Thorndike FP, Gonder-Frederick LA, Magee JC, Bailey ET, Saylor DK, et al. Efficacy of an internet-based behavioural intervention for adults with insomnia. Arch Gen Psychiatry 2009; 66: 692–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Christensen H, Batterham PJ, Gosling JA, Ritterband LM, Griffiths KM, Thorndike FP, et al. Effectiveness of an online insomnia program (SHUTi) for prevention of depressive episodes (the GoodNight Study): a randomised controlled trial. Lancet Psychiatry 2016; 3: 333–41. [DOI] [PubMed] [Google Scholar]
- 23.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA 1999; 282: 1737–44. [DOI] [PubMed] [Google Scholar]
- 24.Griffiths KM, Farrer L, Christensen H. The efficacy of internet interventions for depression and anxiety disorders: a review of randomised controlled trials. Med J Aust 2010; 192: S4–11. [DOI] [PubMed] [Google Scholar]
- 25.Hunkeler EM, Katon W, Tang L, Williams JW Jr, Kroenke K, Lin EH, et al. Long term outcomes from the IMPACT randomised trial for depressed elderly patients in primary care. BMJ 2006; 332: 259–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hollon SD, Stewart MO, Strunk D. Enduring effects for cognitive behavior therapy in the treatment of depression and anxiety. Annu Rev Psychol 2006; 57: 285–315. [DOI] [PubMed] [Google Scholar]
- 27.Renaud J, Brent DA, Baugher M, Birmaher B, Kolko DJ, Bridge J. Rapid response to psychosocial treatment for adolescent depression: a two-year follow-up. J Am Acad Child Adolesc Psychiatry 1998; 37: 1184–90. [DOI] [PubMed] [Google Scholar]
- 28.Masheb RM, Grilo CM. Rapid response predicts treatment outcomes in binge eating disorder: implications for stepped care. J Consult Clin Psychol 2007; 75: 639–44. [DOI] [PubMed] [Google Scholar]
- 29.Andrews G, Cuijpers P, Craske MG, McEvoy P, Titov N. Computer therapy for the anxiety and depressive disorders is effective, acceptable and practical health care: a meta-analysis. PLoS One. 2010; 5: e13196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Muthen B, Muthen LK. Integrating person-centered and variable-centered analyses: growth mixture modeling with latent trajectory classes. Alcohol Clin Exp Res 2000; 24: 882–91. [PubMed] [Google Scholar]
- 31.Pallesen S, Bjorvatn B, Nordhus IH, Sivertsen B, Hjornevik M, Morin CM. A new scale for measuring insomnia: the Bergen Insomnia Scale. Percept Mot Skills 2008; 107: 691–706. [DOI] [PubMed] [Google Scholar]
- 32.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998; 59 (Suppl 20): 22–33. [PubMed] [Google Scholar]
- 33.Morin CM. Insomnia: Psychological Assessment and Management. Guilford Press, 1993. [Google Scholar]
- 34.Thorndike FP, Saylor DK, Bailey ET, Gonder-Frederick L, Morin CM, Ritterband LM. Development and perceived utility and impact of an internet intervention for insomnia. E J Appl Psychol Clin Soc Issues 2008; 4: 32–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gosling JA, Glozier N, Griffiths K, Ritterband L, Thorndike F, Mackinnon A, et al. The GoodNight study – online CBT for insomnia for the indicated prevention of depression: study protocol for a randomised controlled trial. Trials 2014; 15: 56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Griffiths KM, Crisp D, Christensen H, Mackinnon AJ, Bennett K. The ANU WellBeing study: a protocol for a quasi-factorial randomised controlled trial of the effectiveness of an internet support group and an automated internet intervention for depression. BMC Psychiatry 2010; 10: 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Carney CE, Buysse DJ, Ancoli-Israel S, Edinger JD, Krystal AD, Lichstein KL, et al. The consensus sleep diary: standardizing prospective sleep self-monitoring. Sleep 2012; 35: 287–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Glozier N, Christensen H, Naismith S, Cockayne N, Donkin L, Neal B, et al. internet-delivered cognitive behavioural therapy for adults with mild to moderate depression and high cardiovascular disease risks: a randomised attention-controlled trial. PLoS One 2013; 8: e59139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med 2001; 2: 297–307. [DOI] [PubMed] [Google Scholar]
- 40.Lindelow M, Hardy R, Rodgers B. Development of a scale to measure symptoms of anxiety and depression in the general UK population: the psychiatric symptom frequency scale. J Epidemiol Community Health 1997; 51: 549–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Spitzer RL, Kroenke K, Williams JW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006; 166: 1092–7. [DOI] [PubMed] [Google Scholar]
- 42.Verbeke G, Molenberghs G. Linear Mixed Models for Longitudinal Data. Springer, 2000. [Google Scholar]
- 43.Nylund KL, Asparouhov T, Muthen BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct Equat Model 2007; 14: 535–69. [Google Scholar]
- 44.Richards D, Richardson T. Computer-based psychological treatments for depression: a systematic review and meta-analysis. Clin Psychol Rev 2012; 32: 329–42. [DOI] [PubMed] [Google Scholar]
- 45.Newby JM, McKinnon A, Kuyken W, Gilbody S, Dalgleish T. Systematic review and meta-analysis of transdiagnostic psychological treatments for anxiety and depressive disorders in adulthood. Clin Psychol Rev 2015; 40: 91–110. [DOI] [PubMed] [Google Scholar]
- 46.Spek V, Cuijpers P, Nyklicek I, Riper H, Keyzer J, Pop V. internet-based cognitive behaviour therapy for symptoms of depression and anxiety: a meta-analysis. Psychol Med 2007; 37: 319–28. [DOI] [PubMed] [Google Scholar]
- 47.Calear AL, Christensen H. Review of internet-based prevention and treatment programs for anxiety and depression in children and adolescents. Med J Aust 2010; 192: S12–4. [DOI] [PubMed] [Google Scholar]
- 48.Christensen H, Batterham PJ, O’Dea B. E-health interventions for suicide prevention. Int J Environ Res Public Health 2014; 11: 8193–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Weitz E, Hollon SD, Kerkhof A, Cuijpers P. Do depression treatments reduce suicidal ideation? The effects of CBT, IPT, pharmacotherapy, and placebo on suicidality. J Affect Disord 2014; 167: 98–103. [DOI] [PubMed] [Google Scholar]
- 50.Bernert RA, Joiner TE. Sleep disturbances and suicide risk: a review of the literature. Neuropsychiatr Dis Treat. 2007; 3: 735–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bower P, Kontopantelis E, Sutton A, Kendrick T, Richards DA, Gilbody S, et al. Influence of initial severity of depression on effectiveness of low intensity interventions: meta-analysis of individual patient data. BMJ 2013; 346: f540. [DOI] [PMC free article] [PubMed] [Google Scholar]