Abstract
Plain english summary
The behaviour of people with diabetes (e.g. taking medication) and the behaviour of doctors and other healthcare professionals (e.g. checking patients’ blood sugar) are important. Our research group wanted to select one patient behaviour and one healthcare professional behaviour as topics to research in Ireland. Patients and healthcare professionals are not usually asked to help decide on research topics. In this study, we wanted to bring together patients, healthcare professionals and policy makers to help us decide on the most important target behaviours for research in diabetes in Ireland.
We worked with 24 participants, including people with diabetes, diabetes healthcare professionals and policy makers. First, participants suggested behaviours they thought were important to target for research in diabetes. Participants then attended a meeting and ranked which of the behaviours were the most important and discussed the results of the rankings as a group. We identified the most highly ranked patient and healthcare professional behaviours. The top ranked behaviour for people with Type 1 diabetes was to ‘take insulin as required’ and for people with Type 2 diabetes was to ‘attend and engage with structured education programmes’. ‘Engage in collaborative goal setting with patients’ was the top ranked behaviour for healthcare professionals.
Our study shows it is possible for researchers to work with people with diabetes, healthcare professionals and policy makers to decide on research topics. The top ranked behaviours will now be researched by our group in Ireland.
Abstract
Background
Working with patients, healthcare providers, and policy makers to prioritise research topics may enhance the relevance of research and increase the likelihood of translating research findings into practice. The aim of the present study was to work with key stakeholders to identify, and achieve consensus on, the most important target behaviours for research in diabetes in Ireland.
Methods
Twenty-four participants, including people with diabetes, diabetes healthcare professionals and policy makers, took part in a nominal group technique consensus process. Through an online survey, participants generated lists of important target behaviours in three areas: managing Type 1 diabetes, managing Type 2 diabetes and preventing Type 2 diabetes. Participants then attended a research prioritisation meeting and ranked target behaviours in two rounds, with group discussion between ranking rounds. For each of the three key areas, the six top ranked behaviours relevant to people with diabetes and healthcare professionals were identified.
Results
In most cases, the most highly ranked behaviour was the same for Ranking 1 and Ranking 2 and consensus increased in relation to endorsement of top ranked behaviours. However, some behaviours did change position between rankings. The top behaviour relevant to people with Type 1 diabetes was ‘taking insulin as required’ and for people with Type 2 diabetes was ‘attending and engaging with structured education programmes’. ‘Engage in collaborative goal setting with patients’ was the top ranked behaviour relevant to healthcare professionals for managing both Type 1 and Type 2 diabetes. For preventing Type 2 diabetes, 'engage in healthy behaviours as a family' was the highest ranked population behaviour and ‘attend and engage with behaviour change training’ was the highest ranked professional behaviour.
Conclusions
It is possible to work with a diverse group of stakeholders to inform the diabetes research agenda. The priorities identified were co-produced by key stakeholders, including patients, healthcare professionals and policy makers, and will inform the development of a programme of behavioural research in diabetes in Ireland. The study also provides a worked example of a research prioritisation process using the nominal group technique, and identified limitations, which may be useful for other researchers.
Keywords: Diabetes, Research prioritisation, Public and patient involvement, Research engagement, Behaviour change, Intervention development
Background
There is strong evidence that changing people’s health-related behaviour can impact the leading causes of mortality and morbidity [1]. Behaviour change is central in the treatment of chronic illness, and targeting behaviours to prevent and manage chronic illnesses is imperative to deal effectively with increasing numbers of patients and escalating costs [2]. Recent examples of successful interventions have targeted both the behaviour of people with diabetes (diet and activity behaviours) and healthcare professional behaviour (early intervention for diabetes foot ulcers) [3, 4]. Changing behaviour can improve outcomes, with increasing evidence that interventions targeting behaviour change in diabetes can be effective [5, 6].
Despite the potential for behaviour change to improve diabetes outcomes, developing effective interventions is challenging. Diabetes management is complex, encompassing many different behaviours, and patients often struggle to make and maintain the behavioural changes required to manage their condition [7]. As this programme of behavioural research within diabetes continues to grow, how should we decide which behaviours should be prioritised for research? It has been suggested that much health-related research does not address topics which are of importance to patients and clinicians [8]. Seeking the views of patients and healthcare providers should be an essential part of determining the behavioural research agenda, especially to ensure impact from publicly-funded research [9].
Changing diabetes care to implement evidence from research into routine practice is a major challenge within the constraints of the healthcare system [10–12]. Within diabetes, attempts have been made to reduce the research-evidence gap with initiatives such as the Bringing Research in Diabetes to Global Environments and Systems (BRIDGES) project supporting the development of interventions that can be adopted and disseminated in real world settings [13]. Qualitative work with BRIDGES project researchers pinpointed lack of stakeholder and diabetes community links as key barriers in the implementation of diabetes research [14]. Despite the identified need to increase stakeholder engagement, there are few published examples of methods to involve stakeholders in the research process in diabetes.
More recently, efforts have been made to involve stakeholders in the research process by seeking input from patients and healthcare professionals in the prioritisation of research. One approach to collaborative research prioritisation has been driven by the James Lind Alliance which provides guidance on the development of Priority Setting Partnerships [15]. The James Lind Alliance Priority Setting Partnerships aim to bring patient and clinicians together to prioritise treatment uncertainties for research. Treatment uncertainties have been identified and ranked for a range of conditions [16] including Type 1 diabetes [17].
The first step in James Lind Alliance Priority Setting Partnerships is to identify potential research questions of interest to patients and providers. However, involving service users solely in the prioritisation of research questions can be limiting, with evidence that patient suggestions frequently fail to meet the criteria of a researchable question [18]. In addition, focusing solely on treatment uncertainties can limit the scope of research prioritisation. Research exploring the translation of evidence-based behaviour change interventions into practice, for example, does not fall within the treatment uncertainty remit.
The aim of our research prioritisation was to move beyond a more narrow discussion of treatment uncertainties to identify and achieve consensus on shared priority areas for research in diabetes in Ireland. Both the Delphi and nominal group technique processes have been used for the development of consensus in health services research. We also wanted to increase engagement in our programme of research and to build links with relevant stakeholders in Ireland, and so the anonymous approach associated with the Delphi technique was not appropriate to our aims.
The nominal group technique is a controlled group process for the generation and ranking of ideas and for consensus development [19]. The nominal group technique generates a high number of ideas and includes social interaction and discussion while limiting normative pressure for conformity through the use of private individual ranking [19]. Each participant in a nominal group technique process has an equal private ranking vote which provides a democratic process to navigate mismatches between researcher, patient, provider and policy maker priorities [15]. The nominal group technique also avoids limiting patients’ contribution to priority setting by not requiring priorities to be articulated in the form of a researchable question [18].
The aim of the present study was to engage in a nominal group technique processwith key stakeholders to identify, and achieve consensus on, the most important target behaviours for research in diabetes in Ireland. By identifying behaviour change targets that address the needs of the diabetes community, we hoped to enhance the relevance of our programme of research to the Irish healthcare context and to increase the likelihood of future translation of the findings into practice. By focusing on target behaviours rather than tightly defined research questions or treatment uncertainties, we hoped to maximise the potential for patients and healthcare professionals to impact on the development of the research agenda. Finally, by clearly outlining a systematic approach to engaging with key stakeholders we hoped to provide a useful resource for other researchers seeking to engage patients, professionals and policy makers, in the design of research.
The study forms part of a programme of research to develop and evaluate two behaviour change interventions in diabetes in Ireland: one focusing on a behaviour relevant to people with diabetes, and one on a behaviour relevant to healthcare professionals. In identifying high priority behaviours for research, we focused on three key areas: managing Type 1 diabetes mellitus (Type 1 DM), managing Type 2 diabetes mellitus (Type 2 DM) and preventing Type 2 DM. Within each of these areas, we aimed to develop a prioritised list of the most highly ranked target behaviours relevant to people with diabetes and healthcare professionals. We aimed to get the views of people with diabetes, healthcare professionals with clinical experience of diabetes and policy makers working in the area of diabetes.
Methods
The nominal group technique (also known as an expert panel) was used to identify, and achieve consensus on, the most important target behaviours for research [20]. The nominal group technique was chosen as a systematic process that facilitates both idea generation and consensus development [19].
Participants
The nominal group technique is as a small group technique, recommended for use in groups of up to ten participants [19]. Our sample size was informed by a desire to maintain the group dynamic of the technique while still including a range of healthcare professional, patient and policy stakeholders. We set a limit of 25 total participants, to allow for manageable group feedback and discussion as part of the nominal group technique process. Participants were sampled purposively to represent the following groups: people with Type 1 DM and Type 2 DM, healthcare professionals with clinical experience of diabetes and policy makers working in the area of diabetes. Potential healthcare professional and policy maker participants were identified through peer consultation. Those who declined were asked to nominate an alternative in their place. People with diabetes were informed of the study through a flyer circulated through Diabetes Ireland, a national charity dedicated to supporting people with diabetes. Details of number of patients contacted were not available to the research team. Response was generally enthusiastic, ten patients, and an additional two parents of children with diabetes, contacted the research team. Parents of children with diabetes were not eligible for participation as the focus of this prioritisation exercise was on adult patients with diabetes. The research team sent on full details of the meeting, including the proposed date, to potential participants and answered any questions. Six of the ten participants were available and attended the meeting. As participants were engaged in public and patient involvement activities and contributing to research design rather than taking part in a research study, ethical approval was not sought.
Procedure
The nominal group technique begins with eliciting participant views on a topic. Similar suggestions are grouped together and a facilitated group discussion during a structured meeting allows for the clarification and evaluation of items. Each participant then privately ranks each item, the overall rankings are calculated, presented, and discussed and the items are privately re-ranked. The process of achieving consensus through an initial ranking, group discussion, and a second re-ranking was decided in advance and follows published nominal group technique guidance [19]. For the current study, a diabetes research prioritisation (DRP) meeting was organised in Galway, Ireland in October 2014. The study process is shown in Fig. 1 and each of the nominal group stages is outlined further below.
Fig. 1.
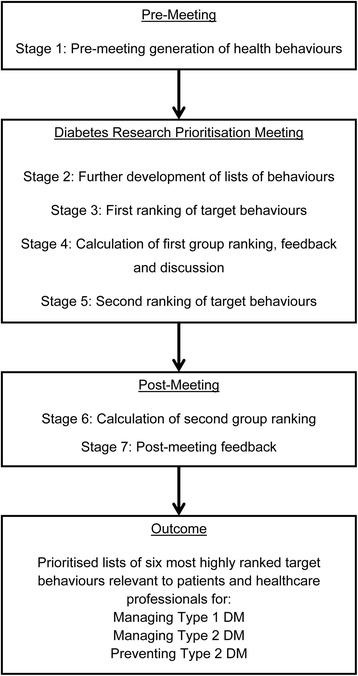
Diabetes Research Prioritisation Flow Chart
Pre-meeting
Stage 1: Pre-meeting generation and collation of health professional and patient behaviours
In advance of the DRP meeting, participants completed an online survey to generate lists of behaviours to target for research. Participants were asked to generate three health professional behaviours and three patient behaviours in each of the key diabetes areas (managing Type 1 DM, managing Type 2 DM, and preventing Type 2 DM). The importance of participants’ own views was emphasised and specific examples were provided for each category of behaviours.
The survey was administered using the Survey Monkey online tool and sent to participants one month in advance of the DRP meeting; a reminder was sent to all participants a week before the meeting. The research team collated all submitted responses by combining similar behaviours to avoid duplication, creating unique behaviours where original submissions included multiple behaviours and creating total lists of behaviours for each key diabetes area.
DRP meeting
Stage 2: Further development of lists of health professional and patient behaviours
Participants attended in person at a three hour DRP meeting and joined small group tables of four at random as they arrived. At the start of the meeting, the research team gave a short presentation outlining the format of the meeting and defined key terms. Participants were provided with the pre-generated lists of target behaviours and engaged in small group discussions to identify any additional behaviours. Small group tables included a mix of patients, healthcare professionals and policy makers. Each small group had an opportunity to feedback additional behaviours to the larger group, and these were added to the total lists. Group discussions were chaired by an experienced facilitator who aimed to ensure everyone had an opportunity to speak. This process was done six times during the meeting, for each of the three key diabetes areas (managing Type 1 DM, managing Type 2 DM, and preventing Type 2 DM), first for patient behaviours and then for health professional behaviours (see Fig. 2).
Fig. 2.
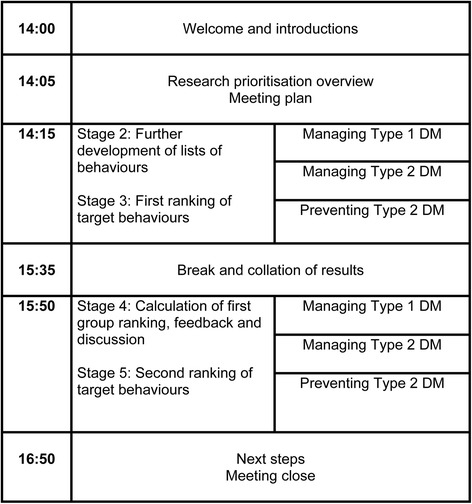
Diabetes Research Prioritisation Meeting Outline and Timings
Stage 3: First ranking of target health professional and patient behaviours
Total behaviour lists were presented back to participants on a screen at the front of the room. Participants privately ranked their top six health professional and top six patient behaviours on paper sheets which were collected by members of the research team.
Stage 4: Calculation of first group ranking, feedback and discussion
The results of the first ranking were manually entered into an excel spread sheet by members of the research team as the meeting progressed. Data entry was checked for accuracy after the meeting by a second researcher; minimal discrepancies were identified. Top ranked priority behaviours were assigned a score of 6, second ranked behaviours were assigned a score of 5 and so on. The total scores for each behaviour were calculated and the results were presented back to the group. The six most highly ranked health professional and patient behaviours in each key diabetes area were highlighted. In a group discussion, the facilitator asked participants to comment on the results, particularly focusing on behaviours whose rankings they found surprising or interesting.
Stage 5: Second ranking of target health professional and patient behaviours
Stage 5 followed a similar procedure as Stage 3 and participants were asked to privately re-rank top six health professional and top six patient behaviours on paper sheets in each of the three key areas.
Post meeting
Stage 6: Calculation of second group ranking
As before, top ranked priority behaviours were assigned a score of 6, second ranked behaviours were assigned a score of 5 and so on and the total scores for each behaviour were calculated. The number of times each behaviour was ranked in participants’ top six and the percentage of participants who ranked each behaviour within their top three priorities were also calculated.
Stage 7: Post-meeting feedback
A summary of the findings was sent to all participants three weeks after the DRP meeting. Participants were sent a link to an online questionnaire and asked to provide feedback on how interesting, enjoyable and useful they found the meeting and to give suggestions as to how the meeting could have been improved.
Results
Participants
Twenty-four people (10 male, 14 female) participated in the DRP process including hospital and primary care practitioners (n = 10), public health practitioners (n = 3), people with Type 1 DM (n = 3), people with Type 2 DM (n = 3), researchers in diabetes (n = 2), a policy leader, a patient organisation policy representative and a psychologist involved in diabetes care.
Development of lists of health professional and patient behaviours (Stages 1–2)
Sixteen participants, including seven hospital and primary care practitioners, one public health practitioner, one diabetes researcher, one psychologist, one patient organisation representative and five patients, completed the pre-meeting online task to generate initial behaviour lists. The numbers of behaviours generated through the survey in each of the three key diabetes areas, and the numbers of behaviours following collation and additional item generation during the meeting, are shown in Table 1.
Table 1.
Generation of health professional and patient behaviours in advance of, and during, the meeting
| Key diabetes area | Total number of behaviours generated at pre-meeting survey | Number of behaviours remaining following collation | Additional behaviours generated during meeting | Final number of behaviours for ranking |
|---|---|---|---|---|
| Managing Type 1 DM – Patients | 37 | 17 | 5 | 22 |
| Managing Type 1 DM – Healthcare Professionals | 42 | 25 | 7 | 32 |
| Managing Type 2 DM – Patients | 52 | 26 | 6 | 32 |
| Managing Type 2 DM – Healthcare Professionals | 47 | 26 | 5 | 31 |
| Preventing Type 2 DM – General Population | 46 | 30 | 8 | 38 |
| Preventing Type 2 DM – Healthcare Professionals/Health Services | 48 | 52 | 3 | 55 |
| Total number of behaviours | 272 | 176 | 34 | 210 |
Ranking of health professional and patient behaviours in three key diabetes areas (Stages 3–6)
Table 2 shows the final highest ranked behaviours, for patients and healthcare professionals, in each of the key diabetes areas. Some participants arrived at the meeting late or had to leave early which is reflected in the different numbers of participants reported in Tables 3, 4, 5, 6 and 7. Further details on ranking results are outlined below.
Table 2.
Highest ranked patient and health professional behaviours in three key diabetes areas
| Key diabetes area | Highest ranked behaviour in Ranking 2 |
|---|---|
| Managing Type 1 DM – Patients | Take insulin as required |
| Managing Type 1 DM – Healthcare Professionals | Engage in collaborative treatment goal setting with patients |
| Managing Type 2 DM – Patients | Attend and engage with structured education |
| Managing Type 2 DM – Healthcare Professionals | Engage in collaborative treatment goal setting with patients |
| Preventing Type 2 DM – General Population | Engage in healthy behaviours as a family |
| Preventing Type 2 DM – Healthcare Professionals/Health Services | Attend and engage with behaviour change training |
Table 3.
Ranking scores of patient behaviours within the area of managing Type 1 Diabetes Mellitus
| Ranking 1 (N = 22) | Ranking 2 (N = 22) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Rank | Behaviours | Total score | No. of top 6 rankings | % of participants with item in top 3 | Rank | Behaviours | Total score | No. of top 6 rankings | % of participants with item in top 3 |
| 1 | Take insulin as required | 60 | 12 | 40.9 | 1 | Take insulin as required | 75 | 14 | 59.1 |
| 2 | Test/monitor blood glucose as often as recommended | 41 | 10 | 31.8 | 2 | Take medication as prescribed | 39 | 9 | 31.8 |
| 3 | Match carbohydrates to insulin daily | 37 | 9 | 31.8 | 3 | Match carbohydrates to insulin daily | 35 | 8 | 27.3 |
| + | |||||||||
| Discussing having diabetes with others | 35 | 8 | 27.3 | ||||||
| 4 | Attend scheduled appointments and contacts in specialist clinic | 34 | 9 | 22.7 | 4 | Quit smoking | 28 | 10 | 13.6 |
| 5 | Discuss having diabetes with others | 30 | 9 | 22.7 | 5 | Attend and engage with structured education | 28 | 9 | 13.6 |
| 6 | Eat healthily | 29 | 8 | 22.7 | 6 | Test/monitor blood glucose as often as recommended | 27 | 8 | 13.6 |
Table 4.
Ranking scores of healthcare professional behaviours within the area of managing Type 1 Diabetes Mellitus
| Ranking 1 (N = 22) | Ranking 2 (N = 22) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Rank | Behaviours | Total score | No. of top 6 rankings | % of participants with item in top 3 | Rank | Behaviours | Total score | No. of top 6 rankings | % of participants with item in top 3 |
| 1 | Engage in collaborative treatment goal setting with patients | 74 | 16 | 59.1 | 1 | Engage in collaborative treatment goal setting with patients | 72 | 16 | 54.5 |
| 2 | Provide consultations that empower and motivate service users | 44 | 10 | 27.3 | 2 | Provide consultations that empower and motivate service users | 57 | 13 | 40.9 |
| 3 | Discuss a patient’s priorities in diabetes self-management | 38 | 11 | 27.3 | 3 | Offer structured patient education | 54 | 13 | 36.4 |
| 4 | Conduct annual patient screening for diabetes complications | 28 | 9 | 18.2 | 4 | Discuss a patient’s priorities in diabetes self-management | 46 | 12 | 31.8 |
| 5 | Provide more flexible services | 28 | 8 | 18.2 | 5 | Provide more flexible services | 37 | 11 | 27.3 |
| 6 | Offer structured patient education | 28 | 8 | 18.2 | 6 | Conduct annual patient screening for diabetes complications | 33 | 9 | 18.2 |
Table 5.
Ranking scores of patient behaviours within the area of managing Type 2 Diabetes Mellitus
| Ranking 1 (N = 24) | Ranking 2 (N = 22) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Rank | Behaviours | Total score | No. of top 6 rankings | % of participants with item in top 3 | Rank | Behaviours | Total score | No. of top 6 rankings | % of participants with item in top 3 |
| 1 | Attend and engage with structured education | 53 | 15 | 29.2 | 1 | Attend and engage with structured education | 62 | 15 | 40.9 |
| 2 | Eat healthily | 49 | 10 | 37.1 | 2 | Increase exercise | 45 | 11 | 31.8 |
| 3 | Engage in more self-management strategies | 43 | 12 | 25 | 3 | Engage in more self-management strategies | 42 | 12 | 31.8 |
| 4 | Increase exercise | 32 | 8 | 16.7 | 4 | Take medication as prescribed | 37 | 12 | 18.2 |
| + | |||||||||
| Monitor your mental health | 37 | 9 | 27.3 | ||||||
| 5 | Engage in physical activity, at least 30 min 5 days a week | 28 | 6 | 20.8 | 5 | Eat healthily | 35 | 14 | 27.3 |
| 6 | Take medication as prescribed | 27 | 7 | 16.7 | 6 | Set realistic goals for physical activity | 33 | 8 | 27.3 |
Table 6.
Ranking scores of healthcare professional behaviours within the area of managing Type 2 Diabetes Mellitus
| Ranking 1 (N = 23) | Ranking 2 (N = 21) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Rank | Behaviours | Total score | No. of top 6 rankings | % of participants with item in top 3 | Rank | Behaviours | Total score | No. of top 6 rankings | % of participants with item in top 3 |
| 1 | Conduct patient centred consultations, make sure that the patient’s needs are addressed instead of the professionals needs | 48 | 12 | 30.4 | 1 | Engage in collaborative treatment goal setting with patients | 57 | 14 | 42.9 |
| 2 | Engage at policy level | 45 | 12 | 30.4 | 2 | Conduct patient centred consultations, make sure that the patient’s needs are addressed instead of the professionals needs | 51 | 12 | 38.1 |
| 3 | Offer weight management/lifestyle modification educational programmes | 44 | 12 | 30.4 | 3 | Regularly assess patients medication, make sure patients are on optimal doses | 47 | 14 | 28.6 |
| 4 | Use a proactive preventative approach | 43 | 9 | 30.4 | 4 | Offer weight management/lifestyle modification educational programmes | 43 | 11 | 38.1 |
| 5 | Engage in collaborative treatment goal setting with patients | 37 | 10 | 21.7 | 5 | Use a proactive preventative approach | 42 | 11 | 33.3 |
| 6 | Conduct an annual examination of all people with Type 2 Diabetes their feet, legs and hypertension | 34 | 10 | 17.4 | 6 | Conduct an annual examination of all people with Type 2 Diabetes their feet, legs and hypertension | 38 | 8 | 33.3 |
| + | + | ||||||||
| Set more individual goals, relevant to the patient | 34 | 8 | 26.1 | Engage at policy level | 38 | 10 | 23.8 | ||
Table 7.
Ranking scores of population behaviours within the area of preventing Type 2 Diabetes Mellitus
| Ranking 1 (N = 23) | Ranking 2 (N = 21) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Rank | Behaviours | Total score | No. of top 6 rankings | % of participants with item in top 3 | Rank | Behaviours | Total score | No. of top 6 rankings | % of participants with item in top 3 |
| 1 | Engage in healthy behaviours as a family | 50 | 12 | 34.8 | 1 | Engage in healthy behaviours as a family | 64 | 13 | 50.4 |
| 2 | Increase exercise | 29 | 7 | 21.7 | 2 | Parental behaviours around diet and exercise for their children | 45 | 11 | 38.1 |
| 3 | Parental behaviours around diet and exercise for their children | 28 | 7 | 21.7 | 3 | Increase exercise | 41 | 10 | 38.1 |
| 4 | Reduce sedentary behaviour | 26 | 6 | 17.4 | 4 | Use smaller cups, bowls and plates to help reduce portion sizes at mealtimes | 33 | 9 | 19.1 |
| 5 | Use smaller cups, bowls and plates to help reduce portion sizes at mealtimes | 26 | 7 | 21.7 | 5 | Advocate for environmental change to support healthy behaviours | 25 | 7 | 19.1 |
| 6 | Advocate for compulsory physical education in school | 26 | 6 | 13 | 6 | Advocate for compulsory physical education in schools | 24 | 7 | 23.8 |
| + | |||||||||
| Increase cost of sugary foods | 24 | 5 | 19.1 | ||||||
Managing Type 1 DM
As show in Table 3 for patient behaviours in managing Type 1 DM, ‘Take insulin as required’ was by far the highest ranked patient behaviour during both Ranking 1 and Ranking 2. Greater consensus for this behaviour was achieved during Ranking 2 when 59.1 % of participants ranked this behaviour in their top three. Interestingly, the second highest (‘Take medication as prescribed’) and fourth highest (‘Quit smoking’) behaviours in Ranking 2 did not feature in the top 6 during Ranking 1.
For healthcare professional behaviours in managing Type 1 DM, ‘Engage in collaborative treatment goal-setting with patients’ was the highest ranked behaviour during both Ranking 1 and 2, but showed slightly lower consensus at Ranking 2 (see Table 4).
Managing Type 2 DM
‘Attend and engage with structured education’ was the highest ranked behaviour during both Ranking 1 and 2, for patient behaviours in managing Type 2 DM. At Ranking 2, there was greater consensus and this behaviour was ranked in the top 3 by 40.9 % of participants as compared to 29.2 % of participants in Ranking 1. ‘Monitor your mental health’ and ‘Set realistic goals for physical activity’ featured in the top 6 during Ranking 2 but had not been highly ranked during Ranking 1 (see Table 5).
Healthcare professional behaviours for the management of Type 2 DM was the only category where the top ranked behaviour changed from Ranking 1 to Ranking 2. At Ranking 2, ‘Engage in collaborative treatment goal setting with patients’ was the top ranked behaviour, a jump from being ranked fifth in Ranking 1. The percentage of people ranking this behaviour in their top 3 almost doubled from 21.7 % at Ranking 1 to 42.9 % in Ranking 2. ‘Conduct patient-centred consultations, make sure that the patient's needs are addressed instead of the professionals needs’ which was ranked first during Ranking 1 was a close second in Ranking 2. The number of participants ranking this item within their top 3 also increased from Ranking 1 to Ranking2 (see Table 6).
Preventing Type 2 DM
‘Engage in healthy behaviours as a family’ was the top ranked population behaviour to prevent Type 2 DM in both Ranking 1 and Ranking 2. As shown in Table 7, consensus in prioritisation of this behaviour increased in Ranking 2 where it had a higher total score and was ranked in a greater percentage of participants’ top three behaviours. ‘Reduce sedentary behaviour’ was ranked fourth in Ranking 1 but did not feature in the top six in Ranking 2 and was replaced by ‘Advocate for environmental change to support healthy behaviours’ and ‘Increase cost of sugary foods’.
‘Attend and engage with behaviour change training’ was the highest ranked healthcare professional/health service behaviour at both Ranking 1 and 2. However, there was not as clear a difference between the top ranked behaviour and the second ranked behaviour ‘GPs should use weight charts to estimate BMI of children more and advise parents on the best course of action when a child is at the overweight stage’ as there was in other categories (See Table 8). The remaining behaviours in the top six were the same between Ranking 1 and Ranking 2 albeit in a slightly different order.
Table 8.
Ranking scores of healthcare professional behaviours within the area of preventing Type 2 Diabetes Mellitus
| Ranking 1 (N = 23) | Ranking 2 (N = 18) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Rank | Behaviours | Total score | No. of top 6 rankings | % of participants with item in top 3 | Rank | Behaviours | Total score | No. of top 6 rankings | % of participants with item in top 3 |
| 1 | Attend and engage with behaviour change training | 38 | 9 | 21.7 | 1 | Attend and engage with behaviour change training | 43 | 9 | 38.9 |
| 2 | Lobby governments to fund community health programmes | 37 | 9 | 26.1 | 2 | GPs should use weight charts to estimate BMI of children more and advise parents on the best course of action when a child is at the overweight stage | 40 | 9 | 44.4 |
| 3 | Advocate for policy level health behaviour change | 36 | 9 | 21.7 | 3 | Advocate for policy level health behaviour change | 34 | 8 | 27.8 |
| 4 | Set specific targets for physical activity | 22 | 7 | 17.4 | 4 | Set specific targets for physical activity | 28 | 6 | 27.8 |
| 5 | GPs should use weight charts to estimate the BMI of children more and advise parents on the best course of action when a child is at the overweight stage | 21 | 5 | 13 | 5 | Provide education at schools | 24 | 6 | 22.2 |
| 6 | Provide education at schools | 20 | 7 | 13 | 6 | Lobby governments to fund community health programmes | 20 | 5 | 16.7 |
Post-meeting feedback (Stage 7)
Fifteen participants, including five hospital and primary care practitioners, two public health practitioners, one diabetes researcher, one psychologist, and four patients completed the post-meeting feedback questionnaire. Two of the respondents did not provide their details. On a scale from 1 to 5, the mean scores for how enjoyable, useful and interesting participants found the meeting were 3.9, 3.6, and 3.9 respectively (where higher scores indicate higher levels of these characteristics). Common suggestions for improvement included increasing the time for discussion, including more patients, and reducing the number of options by using broader umbrella terms to group similar behaviours together.
Discussion
This study demonstrates that it is possible to work with a group of diverse stakeholders - people with diabetes, healthcare professionals and policy makers - in a consensus process to co-produce a prioritised list of behaviours to target for intervention research. Key stakeholders are more likely to drive forward the implementation of research findings for research topics important to them and over which they feel ownership. By engaging with key stakeholders from the outset, we have begun developing strategic alliances with health partners and service users which will be maintained throughout the programme of research.
Utilizing a nominal group process approach resulted in the identification of priorities at a broader level than could have been achieved with a more narrow focus on treatment uncertainties. Attendance and engagement with structured education, for example, would not have been identified as a priority if we had followed the guidance provided for James Lind Alliance Priority Setting Partnerships as evidence on the efficacy of structured education programmes is already available. Our approach allowed stakeholders to identify behaviours where regular performance of the behaviour, rather than treatment uncertainty, is the major problem.
The nominal group process findings indicated that in most cases, the most highly ranked behaviour was the same for Ranking 1 and Ranking 2, suggesting that the discussion and re-ranking process did not significantly change participants’ views. However, there were examples where behaviours featured in the top 6 at Ranking 2 but not at Ranking 1, presumably reflecting the impact of suggestions and arguments offered by participants during group discussions. Details of the discussions that might have led to these changes were not recorded, but would make an interesting and useful addition to future nominal group exercises. As expected in a consensus building study, consensus generally increased in relation to endorsement of the most highly ranked behaviours between the first and second rankings.
A number of striking findings emerged in relation to the most highly ranked priorities. For people with Type 1 DM there was general consensus that targeting ‘taking insulin as required’ is the most important behaviour for research. Indeed, the top three highest ranked behaviours were related to effectively monitoring and managing blood glucose, by administering insulin and counting carbohydrates. The skills required for people with Type 1 DM to maintain good glucose control are complex and demanding [21]. A number of studies report that glucose control remains unsatisfactory despite close monitoring and participation in educational programmes by many people with Type 1 DM [22], although there is some evidence that training in flexible, intensive insulin treatment can improve glycaemic control [23]. Future research should focus on developing and delivering effective interventions to promote the skills needed by people with Type 1 DM to achieve good glycaemic control.
For people with Type 2 DM, attending and engaging with structured education programmes was most highly ranked. Research into structured education programmes for people with Type 2 DM in Ireland has been lacking, but recent studies have demonstrated the efficacy of structured education in Ireland [24]. However, a significant proportion of people with Type 2 DM are either not offered or do not attend structured education programmes [25]. Future research should focus on ways to engage people with Type 2 DM in education programmes, as well as ensuring that such programmes are as patient-centred as possible to increase the benefits to participants.
Interestingly, behaviours related to collaborative goal setting and patient-centred care were highly ranked. ‘Engage in collaborative treatment goal setting with patients’ was the top ranked healthcare professional behaviour for the management of both Type 1 DM and Type 2 DM. Among people with diabetes, patients’ perceptions of collaborative care (including collaborative goal setting) have been shown to be associated with patients’ reported self-management [26], however, the relationship between collaborative goal setting and clinical control among remains poorly understood [27]. Future research should focus on interventions to promote the use of collaborative goal setting among healthcare professionals and people with diabetes, and measuring the associated impact on clinical outcomes.
In relation to preventing Type 2 DM, the most highly ranked behaviours were promotion of healthy exercise and diet, with priority given to engaging in healthy behaviours as a family. There is considerable evidence that increased levels of physical activity are related to better clinical outcomes in diabetes, and additional evidence that physical activity interventions are particularly effective when combined with dietary advice [28]. There was much discussion at the meeting around the need to advocate for policy change and attempt to promote environmental change to support healthy behaviour. There is evidence that environmental and policy approaches lead to increases in physical activity [29], and future research should focus on finding ways to maximise the role of behavioural science theory in development and implementation of public health interventions [30].
For healthcare professionals’ behaviours to prevent Type 2 DM, the highest ranked behaviour was ‘attend and engage with behaviour change training’. Recent trials of behaviour change counselling have found limited effects on behaviour change outcomes [31]. Future research should focus on finding more effective ways to train healthcare professionals to promote behaviour change among their patients.
The current study forms the first step in a behaviour change intervention development process. One behaviour relevant to people with diabetes, and one behaviour relevant to healthcare professionals, will be selected as targets for intervention development. As per recommended guidance [32], the selection of target behaviours will be informed by the comparison of the top behaviours identified in each key area under criteria of the likely impact of changing the behaviour, the likelihood of change, the potential positive or negative spillover to other behaviours and the ease of measurement of each behaviour.
Limitations
Post-meeting feedback indicated that participants would have liked more time for discussion, although whether this would be best achieved through a longer meeting or additional meetings was unclear. Addressing priorities for both Type 1 DM and Type 2 DM on the same day may have been overly ambitious and at times the research team agreed that the meeting felt rushed. Covering Type 1 DM and Type 2 DM at the meeting reflected an attempt to reduce time and travel burden for participants who had experience of both conditions. More time for discussion might have resulted in slightly different priorities. However, when asked how they found the length of the meeting, one third of participants indicated that the meeting was too long. Finding balance between adequate time for discussion and reducing burden on participants with busy schedules is a challenge and should be considered in future research prioritisation exercises.
The nominal group technique has been recommended for groups no larger than ten people [19]. However, to ensure we addressed a range of stakeholder experiences we included different types of healthcare professionals, as well as patients and policy makers. Including this range required a larger number of participants. This may also have added to the sense of the process being rushed as group feedback took longer than with a smaller number of participants. Future nominal group technique processes that require larger numbers could consider guidance from Cantrill et al. [19] to split the sample into two or more groups and to pool results.
Consensus refers to level of agreement among participants in a given round and stability refers to level of agreement between rounds. We did not decide on a priori levels of agreement and stability required for consensus but instead chose to work through two ranking rounds within a one day meeting. The degree to which true consensus was reached is not clear, although in general the endorsement of the most highly ranked behaviours increased between the first and second rankings.
Previous discussions on the use of nominal group technique have debated the merits of mixed versus homogenous groups of participants [19, 33]. As our intention was to achieve consensus on the most important target behaviours for research in diabetes in Ireland we included a mix of patients, providers and policy makers, as each of these stakeholders have a role in behaviour change in diabetes. Despite the best efforts of the experienced facilitator, it is possible that patients may have felt less confident in voicing their opinions given the potentially hierarchical nature of provider-patient relationships. However, the initial generation of lists of behaviours and the actual ranking of behaviours were conducted privately to reduce social pressure and to allow the opinion of each participant to be given equal weighting.
Our nominal group technique process also lacks the representativeness that might be achieved with a large random sample. The overall number of participants was relatively small and, although we purposively sampled for diversity of expertise and experience, the views cannot be claimed to be nationally representative. The views of the 24 stakeholders who took part may not be typical of such a widespread condition and could not be expected represent all possible priorities. In particular, we felt it would have been beneficial to include more people with diabetes, as experiences can vary widely between individuals. Previous studies using the nominal group technique have found participants’ views to be an adequate representation of the views of the wider community [34]. However, these studies used the nominal group technique with healthcare professionals; as our process included healthcare professionals, patient and policy makers we cannot claim the 24 included participants were representative of each of these groups. Finally, the current study describes research priorities identified within the Irish health system, and caution should be used when generalising as priorities vary according to health system context [35].
Conclusion
To impact, and improve, health and healthcare, behavioural researchers need to engage with stakeholders outside of the research community. In the current study, we have demonstrated that it is possible to engage people with diabetes, healthcare professionals and policy makers working in the area of diabetes to generate and prioritise behavioural research topics. The priorities identified were co-produced by key stakeholders, including patients, healthcare professionals and policy makers, and will inform the development of a programme of behavioural research in diabetes in Ireland. We will continue to engage with these stakeholders by inviting patients, professionals and policy makers to sit on steering committees to move chosen priorities forward. The study also provides a worked example of a research prioritisation process using the nominal group technique which may be a useful for other researchers.
Acknowledgements
A`uthor funding
Health Research Board (Ireland) Research Leadership Award (RL/2013/8).
Manuscript Preparation Funding: Health Research Board (Ireland) Research Leadership Award (RL/2013/8).
The funders did not have a role in the design, collection, analysis, or interpretation of data.
Abbreviations
- DRP
Diabetes research prioritisation
- Type 1 DM
Type 1 Diabetes Mellitus
- Type 2 DM
Type 2 Diabetes Mellitus
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
JMS participated in the design and coordination of the study and helped to draft the manuscript. MF and LH entered data, participated in the coordination of the study and provided comments on the study manuscript. MB conceived of the study, participated in its design and coordination and helped to draft the manuscript. All authors read and approved the final manuscript.
Contributor Information
Jennifer Mc Sharry, Email: jenny.mcsharry@nuigalway.ie.
Milou Fredrix, Email: m.fredrix1@nuigalway.ie.
Lisa Hynes, Email: l.hynes2@nuigalway.ie.
Molly Byrne, Email: molly.byrne@nuigalway.ie.
References
- 1.National Institute of Health and Clinical Excellence (NICE). Behaviour change: general approaches (Public Health Guidance 6), 2007. London: NICE; 2007. Available from http://www.nice.org.uk/Guidance/PH6.
- 2.Newman S, Steed L, Mulligan K. Self-management interventions for chronic illness. Lancet. 2004;364(9444):1523–37. doi: 10.1016/S0140-6736(04)17277-2. [DOI] [PubMed] [Google Scholar]
- 3.Trief PM, Weinstock RS, Cibula D, Delahanty LM. Sustained weight loss one year after group telephone intervention: 3-Year results from the SHINE study. Diabetes Res Clin Pract. 2014;106(3):e74–e8. doi: 10.1016/j.diabres.2014.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hsu C-R, Chang C-C, Chen Y-T, Lin W-N, Chen M-Y. Organization of wound healing services: The impact on lowering the diabetes foot amputation rate in a ten-year review and the importance of early debridement. Diabetes Res Clin Pract. 2015;109(1):77–84. doi: 10.1016/j.diabres.2015.04.026. [DOI] [PubMed] [Google Scholar]
- 5.Avery L, Flynn D, van Wersch A, Sniehotta FF, Trenell MI. Changing Physical Activity Behavior in Type 2 Diabetes: A systematic review and meta-analysis of behavioral interventions. Diabetes Care. 2012;35(12):2681–9. doi: 10.2337/dc11-2452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weinger K, Beverly EA, Lee Y, Sitnokov L, Ganda OP, Caballero A. The effect of a structured behavioral intervention on poorly controlled diabetes: A randomized controlled trial. Arch Intern Med. 2011;171(22):1990–9. doi: 10.1001/archinternmed.2011.502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-Management education for adults with type 2 Diabetes A meta-analysis of the effect on glycemic control. Diabetes Care. 2002;25(7):1159–71. doi: 10.2337/diacare.25.7.1159. [DOI] [PubMed] [Google Scholar]
- 8.Partridge N, Scadding J. The James Lind Alliance: patients and clinicians should jointly identify their priorities for clinical trials. Lancet. 2004;364(9449):1923–4. doi: 10.1016/S0140-6736(04)17494-1. [DOI] [PubMed] [Google Scholar]
- 9.Buckley BS, Grant AM, Tincello DG, Wagg AS, Firkins L. Prioritizing research: Patients, carers, and clinicians working together to identify and prioritize important clinical uncertainties in urinary incontinence. Neurourol Urodyn. 2010;29(5):708–14. doi: 10.1002/nau.20816. [DOI] [PubMed] [Google Scholar]
- 10.Glasgow RE, Klesges LM, Dzewaltowski DA, Bull SS, Estabrooks P. The future of health behavior change research: what is needed to improve translation of research into health promotion practice? Ann Behav Med. 2004;27(1):3–12. doi: 10.1207/s15324796abm2701_2. [DOI] [PubMed] [Google Scholar]
- 11.Grimshaw JM, Eccles MP, Lavis JN, Hill SJ, Squires JE. Knowledge translation of research findings. Implement Sci. 2012;7(1):50. doi: 10.1186/1748-5908-7-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Colagiuri R. Implementing evidence based guidelines: Unlocking the secrets. Diabetes Res Clin Pract. 2009;85(2):117–8. doi: 10.1016/j.diabres.2009.06.011. [DOI] [PubMed] [Google Scholar]
- 13.Siminerio L, Mbanya JC. Translating diabetes research into global communities. Diabetes Res Clin Pract. 2011;93(3):443–5. doi: 10.1016/j.diabres.2011.07.010. [DOI] [PubMed] [Google Scholar]
- 14.de Quevedo IG, Siminerio L, L’Heveder R, Narayan KV. Challenges in real-life diabetes translation research: early lessons from BRIDGES projects. Diabetes Res Clin Pract. 2012;95(3):317–25. doi: 10.1016/j.diabres.2011.10.013. [DOI] [PubMed] [Google Scholar]
- 15.Petit-Zeman S, Firkins L, Scadding JW. The James Lind Alliance: tackling research mismatches. Lancet. 2010;376(9742):667–9. doi: 10.1016/S0140-6736(10)60712-X. [DOI] [PubMed] [Google Scholar]
- 16.Crowe S, Fenton M, Hall M, Cowan K, Chalmers I. Patients’, clinicians’ and the research communities’ priorities for treatment research: there is an important mismatch. Research Involvement and Engagement. 2015;1(1):1. doi: 10.1186/s40900-015-0005-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gadsby R, Snow R, Daly AC, Crowe S, Matyka K, Hall B, et al. Setting research priorities for Type 1 diabetes. Diabet Med. 2012;29(10):1321–6. doi: 10.1111/j.1464-5491.2012.03755.x. [DOI] [PubMed] [Google Scholar]
- 18.Snow R, Crocker J, Crowe S. Missed opportunities for impact in patient and carer involvement: a mixed methods case study of research priority setting. Research Involvement and Engagement. 2015;1(1):1–13. doi: 10.1186/s40900-015-0007-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cantrill J, Sibbald B, Buetow S. The Delphi and nominal group techniques in health services research. Int J Pharm Pract. 1996;4(2):67–74. doi: 10.1111/j.2042-7174.1996.tb00844.x. [DOI] [Google Scholar]
- 20.Jones J, Hunter D. Qualitative Research: Consensus methods for medical and health services research. BMJ. 1995;311(7001):376–80. doi: 10.1136/bmj.311.7001.376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.American Diabetes Association Standards of Medical Care in Diabetes—2010. Diabetes Care. 2010;33(Supplement 1):S11–S61. doi: 10.2337/dc10-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Charpentier G, Benhamou P-Y, Dardari D, Clergeot A, Franc S, Schaepelynck-Belicar P, et al. The diabeo software enabling individualized insulin dose adjustments combined with telemedicine support improves HbA1c in poorly controlled type 1 diabetic patients: A 6-month, randomized, open-label, parallel-group, multicenter trial (TeleDiab 1 study) Diabetes Care. 2011;34(3):533–9. doi: 10.2337/dc10-1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.DAFNE Study Group Training in flexible, intensive insulin management to enable dietary freedom in people with type 1 diabetes: Dose adjustment for normal eating (DAFNE) randomised controlled trial. BMJ. 2002;325(7367):746–9. doi: 10.1136/bmj.325.7367.746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Clarke A. Effectiveness of a community orientated diabetes education (CODE) programme for people with type 2 diabetes. European Diabetes Nursing. 2011;8(3):94–9a. doi: 10.1002/edn.188. [DOI] [Google Scholar]
- 25.Dinneen SF. Structured education for people with type 2 diabetes. BMJ. 2008;336(7642):459–60. doi: 10.1136/bmj.39478.693715.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Heisler M, Bouknight RR, Hayward RA, Smith DM, Kerr EA. The relative importance of physician communication, participatory decision making, and patient understanding in diabetes self-management. J Gen Intern Med. 2002;17(4):243–52. doi: 10.1046/j.1525-1497.2002.10905.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lafata JE, Morris HL, Dobie E, Heisler M, Werner RM, Dumenci L. Patient-reported use of collaborative goal setting and glycemic control among patients with diabetes. Patient Educ Couns. 2013;92(1):94–9. doi: 10.1016/j.pec.2013.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Umpierre D, Ribeiro P, Kramer C, et al. Physical activity advice only or structured exercise training and association with HbA1c levels in type 2 diabetes: A systematic review and meta-analysis. JAMA. 2011;305(17):1790–9. doi: 10.1001/jama.2011.576. [DOI] [PubMed] [Google Scholar]
- 29.Heath GW, Parra DC, Sarmiento OL, Andersen LB, Owen N, Goenka S, et al. Evidence-based intervention in physical activity: lessons from around the world. Lancet. 2012;380(9838):272–81. doi: 10.1016/S0140-6736(12)60816-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Glanz K, Bishop DB. The role of behavioral science theory in development and implementation of public health interventions. Annu Rev Public Health. 2010;31(1):399–418. doi: 10.1146/annurev.publhealth.012809.103604. [DOI] [PubMed] [Google Scholar]
- 31.Butler CC, Simpson SA, Hood K, Cohen D, Pickles T, Spanou C, et al. Training practitioners to deliver opportunistic multiple behaviour change counselling in primary care: a cluster randomised trial. BMJ. 2013;346:f1191. doi: 10.1136/bmj.f1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Michie S, Atkins L, West R. The behaviour change wheel: A guide to designing interventions. Silverback Publishing: London; 2014. [Google Scholar]
- 33.Wainwright D, Boichat C, McCracken LM. Using the nominal group technique to engage people with chronic pain in health service development. Int J Health Plann Manag. 2014;29(1):52–69. doi: 10.1002/hpm.2163. [DOI] [PubMed] [Google Scholar]
- 34.Vella K, Goldfrad C, Rowan K, Bion J, Black N. Use of consensus development to establish national research priorities in critical care. BMJ. 2000;320(7240):976–80. doi: 10.1136/bmj.320.7240.976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Byrne M, Campbell NC. Promoting behaviour change in patients with coronary heart disease--a consensus study in two countries with different healthcare systems. Eur J Gen Pract. 2003;9(4):134–40. doi: 10.3109/13814780309160422. [DOI] [PubMed] [Google Scholar]


