Abstract
Exposure-based psychological treatments for anxiety have high efficacy. However, a substantial proportion of patients do not respond to therapy. Research examining the potential biological underpinnings of therapy response is still in its infancy, and most studies have focussed on candidate genes. To our knowledge, this study represents the first investigation of genome-wide expression profiles with respect to treatment outcome. Participants (n=102) with panic disorder or specific phobia received exposure-based cognitive behavioural therapy. Treatment outcome was defined as percentage reduction from baseline in clinician-rated severity of their primary anxiety diagnosis at post treatment and 6 month follow-up. Gene expression was determined from whole blood samples at three time points using the Illumina HT-12v4 BeadChip microarray. Linear regression models tested the association between treatment outcome and changes in gene expression from pre-treatment to post treatment, and pre-treatment to follow-up. Network analysis was conducted using weighted gene co-expression network analysis, and change in the detected modules from pre-treatment to post treatment and follow-up was tested for association with treatment outcome. No changes in gene expression were significantly associated with treatment outcomes when correcting for multiple testing (q<0.05), although a small number of genes showed a suggestive association with treatment outcome (q<0.5, n=20). Network analysis showed no association between treatment outcome and change in gene expression for any module. We report suggestive evidence for the role of a small number of genes in treatment outcome. Although preliminary, these findings contribute to a growing body of research suggesting that response to psychological therapies may be associated with changes at a biological level.
Introduction
Anxiety disorders are some of the most common mental health disorders, affecting a sizable proportion of the population.1 It is estimated that over 25% of people will be diagnosed with an anxiety disorder at some point during their lifetime, reflecting a considerable economic cost to society.1, 2 In addition to the emotional discomfort and distress central to the diagnosis, anxiety disorders are associated with numerous negative consequences for many areas of everyday functioning.3 Psychological therapies such as cognitive behavioural therapy (CBT) and exposure therapy in particular have a relatively high efficacy for treating anxiety.4, 5, 6 Meta-analyses have demonstrated large effect sizes for a range of anxiety diagnoses, and treatment response shows substantial continuity across long-term outcomes.7, 8
Therapygenetics is a relatively new area of research that investigates genetic predictors of response to psychological therapies.9 Most studies have focussed on candidate gene predictors of treatment response, although results have been inconsistent.10 In addition, recent preliminary research has identified epigenetic changes in genes of interest during psychological therapies that may be associated with outcome. Studies thus far have focussed on BDNF in adults with borderline personality disorder,11 SERT in children with anxiety disorders,12 MAOA in adults with panic disorder13 and the HPA-axis-related genes FKBP5 and GR in children with anxiety disorders14 and in veterans with posttraumatic stress disorder.15 Interestingly, in the latter study, changes in FKBP5 methylation during exposure therapy were found to be associated with FKBP5 expression at follow-up.
A small number of further studies have examined the role of gene expression and response to a psychological therapy. Gene expression levels are a useful indicator of gene activity and function as they are known to be highly dynamic. They are also susceptible to genetic, epigenetic and environmental influences, and therefore may provide insight into the potential mechanisms of therapy response. Two studies have demonstrated that FKBP5 expression may be associated with outcome following CBT in participants with posttraumatic stress disorder, with both finding that increases in gene expression during therapy were associated with symptom improvement.16, 17 Another two studies have taken a broader approach, assessing gene expression levels of panels of genes in major depressive disorder before and after CBT.18, 19 In the first of these studies, 10 genes were assayed before and after treatment using the BioM-10 panel, which consists of five genes associated with high mood states and five genes associated with low mood states.18 Clinical improvement after CBT was associated with an increase in the high mood markers relative to the low mood markers. The second study identified gene expression networks predictive of remission, whereby significant co-expression networks of genes before treatment were identified in remitters but not in patients who remained depressed.19 Although preliminary, these studies suggest that gene expression levels may be indicative of response to treatment.
To date, no studies have utilised a genome-wide approach to study whether gene expression changes are associated with response to a psychological therapy. Such hypothesis-free analysis allows for the testing of a wider range of novel genomic targets, including rare variants, as well as the opportunity to identify networks of genes with similar activity. Here we assess gene expression levels across the genome to examine transcriptomic changes that may be associated with response to psychological therapy. We examined the association between clinical symptomatology and change in probe-level gene expression from pre-treatment to post treatment and follow-up. Biological pathway enrichment analysis was performed using the ranked gene list, in order to identify known pathways and functions represented in the top results. Further data-driven clustering techniques were used to identify networks of co-expressed genes in the data set, and the trajectory of these modules across the course of treatment was examined. Co-expression network analysis using weighted gene co-expression network analysis (WGCNA) is a powerful approach, even in relatively small data sets, as it describes the correlation patterns among genes and therefore reduces the multiple testing burden associated with genome-wide data. This is the largest study of gene expression and treatment response, and, to our knowledge, the first to include transcriptomic data at follow-up as well as pre- and post treatment.
Materials and methods
Participants
Participants (n=102) were recruited at the Mental Health Research and Treatment Center, Ruhr-Universität Bochum, Germany (n=56) or the Dental Clinical Bochum, Germany (n=46). Age at baseline ranged from 19 to 68 years (mean=39.8), and 66.7% of the sample were female. At baseline, 27.5% were smokers, 5.9% were using a form of psychoactive medication, and 32.4% took other regular medications. All participants were treated for panic disorder with agoraphobia, or agoraphobia alone (28.4%) or specific phobia (71.6% including dental fear—45.1% of total). Diagnoses were made according to DSM-IV criteria by trained clinicians using the Diagnostisches Interview bei Psychischen Störungen (DIPS) and Mini-DIPS,20, 21, 22 structured interviews with well-established reliability, validity and patient acceptance.23, 24, 25, 26 At least one comorbid diagnosis was present in 38.2% of participants. All participants completed one of four exposure therapy or exposure-based CBT treatment programmes as detailed below. A diagram of treatment protocols can be found in Supplementary Figure S1. All treatments were regularly supervised by experienced senior clinicians using audiovisual recordings in order to ensure treatment protocol integrity.
Treatment was administered at the Mental Health Research and Treatment Centre in three groups. All participants received five preliminary sessions covering diagnosis and psychoeducation before starting therapy. Participants with a primary diagnosis of panic disorder/agoraphobia were randomized either to exposure-based CBT (akin to the specific phobia group above) or to an exposure-alone condition without any element of cognitive restructuring (Clinical Trials: NCT01680327). Participants with specific phobia (not primarily associated with dental fear) were treated in a long-term programme of up to 25 sessions of in vivo exposure. Participants in these groups were excluded if they were using anxiolytic medication.
Individuals with high levels of dental fear were treated in a dental anxiety-specific programme.27 Treatment was given in five sessions, including an initial diagnostic and psychoeducation session, and a session developing relaxation techniques and focussing on helpful thoughts. These coping strategies were then encouraged in three sessions consisting of exposure scenarios such as video exposure, noise exposure and in sensu exposure (virtual reality or visualisation). Concurrent psychoactive medication was not an exclusion criterion.
Outcome measures
Severity—clinical global impression
Treatment response was defined as percentage improvement in clinician-rated severity of the treated diagnosis, as determined using the Clinical Global Impression—Severity (CGI-S) scale.28 The CGI-S consists of a scale of 1–7, with a score of 1 indicating that the patient is healthy, and 7 indicating that the patient is extremely ill. Mean CGI-S score at baseline was 4.46 (s.d.=1.14), signifying that the sample was moderate to markedly ill. Scores were rescaled from 1–7 to 0–6 and percentage improvement from pre-treatment to post treatment and pre-treatment to follow-up was calculated for all participants.
Ethics statements
This study was conducted in accordance with the principles outlined by the Declaration of Helsinki. Site-specific trials and the collection of samples were approved by local Human Ethics and Biosafety Committees, and all participants provided informed consent. The receipt, storage and analyses of samples were approved by the London-Bentham NRES Committee and the King’s College London Psychiatry, Nursing and Midwifery Research Ethics Sub-Committee.
Genome-wide expression data
Sample collection
Whole blood samples were drawn at pre-treatment (before exposure), immediately post treatment and follow-up (~6 months following the conclusion of treatment) using PAXgene blood RNA tubes. Blood RNA was isolated and purified using the PAXgene Blood miRNA Kit (Qiagen, Hilden, Germany) according to the manufacturer’s protocol using the Qiagen Qiacube. RNA quality and integrity were measured using both the Nanodrop 1000 spectrophotometer (Nanodrop 1000, Nanodrop, Wilmington, DE, USA) and the Agilent 2100 Bioanalyzer (Agilent, Santa Clara, CA, USA). Genome-wide expression levels were measured from 750 ng total RNA using the Illumina HumanHT-12v4 Expression BeadChip (Illumina, San Diego, CA, USA).
Quality control
Initial processing of data was performed using GenomeStudio to identify samples with detection rates dissimilar to the rest of the project (GenomeStudio, Illumina). Stringent quality control processing of the data was conducted using the standardised procedures from internal pipelines (available at https://github.com/snewhouse/BRC_MH_Bioinformatics). Expression data were background-corrected using module-based background correction for Beadarray.29 Probes were then filtered by selecting probes with expression levels >2 s.d. greater than the mean intensity of the negative control (background) beads. Reported gender was compared to XIST gene expression (female specific) and Y chromosome gene expression (male specific). Each probe was then transformed and normalised using log2 transformation and robust-spline normalisation.30, 31 Sample relationships within the co-expression network were assessed and outliers were removed.32 Following sample outlier removal, 95 samples at pre-treatment, 99 samples at post treatment and 97 samples at follow-up remained. Probes detected in <80% of the sample were removed. Following quality control procedures, 4381 probes with high-quality data were available for analysis. All quality control was performed in R33 making use of the lumi package.31
Batch effects
In order to minimise potential batch effects, all three time points per participant were extracted in the same batch and run on the same array. Technical batch variables (hybridisation, sample position on microarray, RNA integrity number (RIN), overall processing batch, date of RNA extraction, date of amplification, date of microarray processing and cRNA concentration) were assessed for association with the first principal component of the expression data using stepwide linear regression bootstrapped 100 times (with covariate order randomised). The data were then adjusted for the associated batch variables. ComBat (from the sva package) was used to control for hybridisation (expression microarray, 27 chips), with fixed effects of RIN and cRNA concentration.34 The data were then adjusted for RIN and cRNA concentration using multivariate linear regressions (RcppArmadillo).35 Nine technical replicates (three participant sample sets) were included as quality checks. Duplicate samples showed very high consistency, with an average concordance of r=0.986.
Cell-type composition
Cell-type proportions (lymphocyte, neutrophils and monocytes) were estimated using deconvolution methods implemented in CellMix36 based on previously reported whole blood cell composition values.37 Change in lymphocyte, neutrophil and monocyte proportions were calculated for pre- to post treatment, and pre-treatment to follow-up.
Analyses
Probe level analyses
Change in expression from pre- to post treatment and pre-treatment to follow-up were calculated for all probes (total n=4381) after quality control.
Confounding factors
Age, body mass index, gender, comorbidities, smoking status, psychoactive medication, other medications and cell-type composition changes were tested for association with outcome. Population stratification was tested for association with outcome using the first two principal components from genome-wide genotyping data (‘PC1’, ‘PC2’).38 Treated diagnosis was not associated with outcome at post treatment (F=0.44, P=0.644) or at follow-up (F=0.74, P=0.480).
Gene expression and treatment outcome
The association between change in expression values and percentage reduction in CGI-S was tested using linear regression models for post treatment and follow-up. Time (number of days since pre-treatment) and number of sessions were included as covariates to account for variability in treatment length as well as baseline CGI-S and psychoactive medication status. Robust standard errors and clustering by treatment group were used to account for differences between treatment conditions. In these analyses, a negative β-value indicates that a greater percentage reduction in severity is associated with a decrease in gene expression over time. Linear regression analyses were conducted in Stata.39
Functional annotation and enrichment analysis
Illumina microarray probes were annotated using the Bioconductor package lumiHumanIDmapping. Probes were ranked according to linear regression analysis uncorrected P-value, and assessed for enrichment of biological pathways using GOrilla.40 Where probes mapped to the same gene, the highest-ranked was retained. This method performs Gene Ontology (GO) enrichment analyses on ranked probe lists to identify known pathways more strongly associated with the outcome of interest. Further information on this analysis is provided in the Supplementary Information.
Multiple testing correction
The P-values for probe-wise analyses were corrected for multiple testing using the method defined by Benjamini and Hochberg41 to give a test q-value. False discovery rate statistics (FDR; q-values) were calculated using the qvalue package in R. Probes associated with treatment outcome with a FDR-corrected q<0.05 were considered significant. Probes associated with treatment outcome with a FDR-corrected q<0.5 are reported as suggestive.
Network-based analyses
Data-driven clustering was performed using weighted gene co-expression network analysis on pre-treatment samples to create signed co-expression networks (WGCNA).42 Modules detected at pre-treatment were forced onto the data at the post treatment and follow-up time points using the module preservation function43 in order to examine changes across the course of treatment.
Module eigengenes, equivalent to the first principal component of each module, were used as a proxy for module expression. The association between change in CGI-S and change in module expression was tested using linear regression models for post treatment and follow-up as previously described. The grey module was not included in any analyses as it consisted of genes that were unable to be assigned to a module.
Code and data availability
Code used for data QC can be accessed at https://github.com/snewhouse/BRC_MH_Bioinformatics. All analysis scripts are available on request. The data discussed in this publication have been deposited in NCBI’s Gene Expression Omnibus44 and are accessible through GEO Series accession number GSE94119 (https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE94119).
Results
Clinical characteristics
As expected, there was a significant change in CGI-S from pre-treatment to post treatment (pre-treatment=4.46, post treatment=2.04; t=17.831, df=99, P<0.001) with a mean percentage change in severity of 53.14%. There was also a significant change in CGI-S from pre-treatment to follow-up (follow-up=2.36; t=12.140, df=93, P<0.001) where the mean percentage change in severity was 45.80%.
Confounding factors
There was no association between treatment outcome and baseline severity, age, body mass index, gender, comorbidities, smoking status, other (non-psychoactive) medications, cell-type proportion changes and population stratification values. However, a significant association was reported between psychoactive medication and percentage reduction in CGI-S from pre- to post treatment and follow-up (Table 1—participants on psychoactive medications showed a poorer response to treatment), and was therefore included as a covariate in linear regression analyses.
Table 1. Associations between percentage change in CGI-S and clinical factors.
| Clinical factor | Percentage change in CGI-S | |||
|---|---|---|---|---|
|
Post treatment |
Follow-up |
|||
| r | P | r | P | |
| Baseline severity | −0.051 | 0.616 | 0.148 | 0.157 |
| Age | −0.120 | 0.234 | −0.015 | 0.887 |
| BMI | 0.010 | 0.921 | −0.003 | 0.976 |
| t(df) | P | t(df) | P | |
| Gender | −0.913 (98) | 0.364 | −0.104 (91) | 0.917 |
| Smoking status | 0.390 (98) | 0.698 | 0.500 (91) | 0.618 |
| Comorbidities | 1.126 (98) | 0.263 | 1.120 (91) | 0.235 |
| Psychoactive medication | 3.498 (98) | 7E−04* | 2.287 (91) | 0.025* |
| Other medications | 1.266 (98) | 0.209 | 0.823 (91) | 0.413 |
| Population stratification | r | P | r | P |
| PC1 | −0.178 | 0.082 | −0.003 | 0.981 |
| PC2 | −0.078 | 0.451 | 0.033 | 0.758 |
| Cell proportion changes | r | P | r | P |
| Lymphocytes | ||||
| Pre- to post treatment | 0.047 | 0.657 | — | — |
| Pre-treatment to follow-up | — | — | 0.079 | 0.481 |
| Neutrophils | ||||
| Pre- to post treatment | 0.040 | 0.710 | — | — |
| Pre-treatment to follow-up | — | — | 0.040 | 0.720 |
| Monocytes | ||||
| Pre- to post treatment | 0.030 | 0.780 | — | — |
| Pre-treatment to follow-up | — | — | −0.097 | 0.399 |
Abbreviation: BMI, body mass index; CGI-S, Clinical Global Impression—Severity. NB: factors that were nominally significant (*) at either time point were included as covariates in linear-mixed models.
Probe level analyses
Post treatment
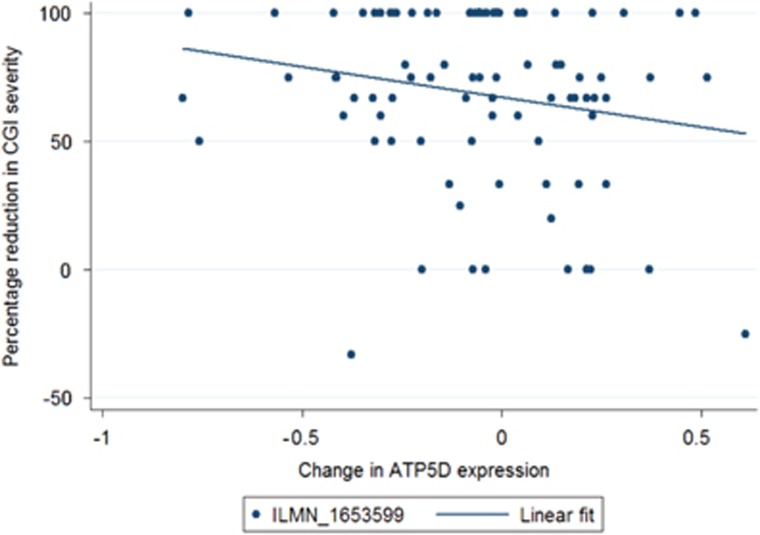
Of the 4381 probes tested, 171 showed a nominally significant association between changes in expression and percentage improvement in symptoms from pre-treatment to the post-treatment time point (P<0.05). Table 2 shows the top 10 probes ranked by uncorrected P-value including standardised test statistics. No probes showed a significant association with treatment outcome when corrected for multiple testing (q<0.05). One probe reached a suggestive threshold (q<0.5); ILMN_1653599 (Figure 1, q=0.38, P=8.90 × 10−5). Annotation showed that this probe mapped to the gene ATP5D. Further top-ranked probes are detailed in Supplementary Table S1.
Table 2. Top genes ranked by association with treatment outcome (percentage improvement in CGI-S).
| Time | Gene symbol | Probe ID | Test β | P-value | q-value |
|---|---|---|---|---|---|
| Post treatment | ATP5D | ILMN_1653599 | −0.373 | 8.90E−05 | 0.353 |
| HBA2 | ILMN_2127842 | 0.670 | 3.87E−04 | 0.767 | |
| ATP5H | ILMN_1794912 | −0.795 | 8.12E−04 | 0.890 | |
| LOC646630 | ILMN_1691449 | −0.588 | 1.06E−03 | 0.890 | |
| HSP90AB1 | ILMN_1673711 | −0.543 | 1.90E−03 | 0.890 | |
| TMEM160 | ILMN_1704024 | −0.609 | 2.37E−03 | 0.890 | |
| NT5C3 | ILMN_2352121 | −0.204 | 2.57E−03 | 0.890 | |
| RPL23A | ILMN_1788607 | −0.960 | 2.84E−03 | 0.890 | |
| F2R | ILMN_2221507 | 0.496 | 4.06E−03 | 0.890 | |
| NDUFA12 | ILMN_1737738 | −0.885 | 4.77E−03 | 0.890 | |
| Follow-up | PTBP1 | ILMN_2333319 | 0.715 | 4.11E−04 | 0.499 |
| DAGLB | ILMN_1658885 | 0.713 | 6.02E−04 | 0.499 | |
| FCER1G | ILMN_2123743 | −1.176 | 6.33E−04 | 0.499 | |
| LOC647506 | ILMN_3240375 | 0.228 | 6.65E−04 | 0.499 | |
| LOC652493 | ILMN_1739508 | 0.184 | 1.18E−03 | 0.499 | |
| IFI30 | ILMN_1807277 | −0.677 | 1.12E−03 | 0.499 | |
| S100A10 | ILMN_1796712 | −0.428 | 1.24E−03 | 0.499 | |
| LOC642113 | ILMN_1652199 | 0.198 | 1.25E−03 | 0.499 | |
| ACP1 | ILMN_2344956 | −0.633 | 1.59E−03 | 0.499 | |
| SPCS2 | ILMN_1809488 | −0.547 | 1.69E−03 | 0.499 | |
| SRRM1 | ILMN_1697670 | 0.705 | 1.74E−03 | 0.499 | |
| PIK3R1 | ILMN_1760303 | 0.808 | 1.90E−03 | 0.499 | |
| HNRPA1P4 | ILMN_1690586 | 0.562 | 2.10E−03 | 0.499 | |
| STUB1 | ILMN_1756126 | −0.429 | 2.10E−03 | 0.499 | |
| PCM1 | ILMN_1690487 | 0.869 | 2.34E−03 | 0.499 | |
| OCIAD1 | ILMN_1799604 | 0.462 | 2.36E−03 | 0.499 | |
| PSMB10 | ILMN_1683026 | −0.685 | 2.38E−03 | 0.499 | |
| STAT1 | ILMN_1691364 | −0.230 | 2.48E−03 | 0.499 | |
Abbreviation: CGI-S, Clinical Global Impression—Severity. NB: probe ID=Illumina HumanHT12 v4 expression BeadChip array ID, ‘Test β’=test statistic for association with treatment outcome, values in bold indicates probes significant at a suggestive level.
Figure 1.
Change in gene expression and percentage reduction in Clinical Global Impression—Severity (CGI-S) at post treatment. ATP5D; β=−0.373, P=8.90E−05.
Enrichment analyses
Enrichment analysis of the ranked probes from the post-treatment analyses using GOrilla yielded nine significant GO terms at q<0.05, with some terms depicting related functions. The top reported pathway was ‘establishment of protein localisation to endoplasmic reticulum’ (P=3.51 × 10−6, q=0.03). A full list of pathways can be found in Supplementary Table S2.
Follow-up
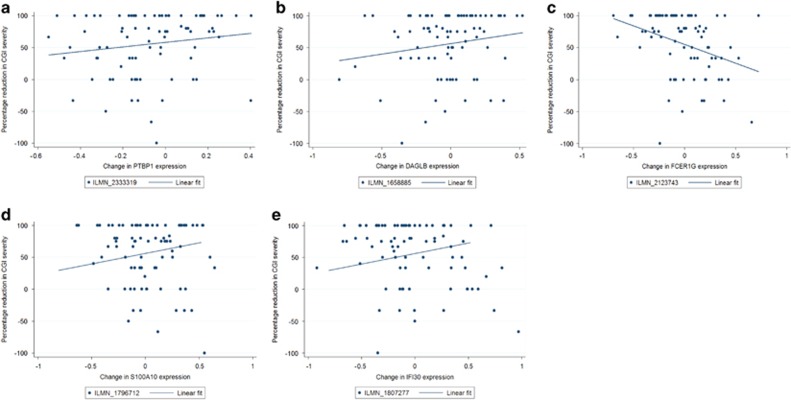
In total, 225 probes showed a nominally significant association between changes in expression and percentage improvement in symptoms from pre-treatment to the follow-up time point. Table 2 shows the top 20 probes ranked by uncorrected P-value including standardised test statistics. Similarly to the findings for the post-treatment analyses, no probes showed a significant association when correcting for multiple testing. However, 19 probes reached a suggestive threshold (Table 2). Figure 2 shows the top five gene-labelled probes; ILMN_2333319 (q=0.49, P=2.01 × 10−4), ILMN_1658885 (q=0.49, P=4.33 × 10−4), ILMN_2123743 (q=0.49, P=5.73 × 10−4), ILMN_1807277 (q=0.49, P=1.12 × 10−3) and ILMN_1796712 (q=0.49, P=1.24 × 10−3). These probes corresponded with the genes PTBP1, DAGLB, FCER1G, IFI30 and S100A10. Further top-ranked probes are detailed in Supplementary Table S3.
Figure 2.
Change in gene expression and percentage reduction in Clinical Global Impression—Severity (CGI-S) at follow-up for five gene-labelled probes significant at a suggestive level. (a) PTBP1; β=0.715, P=4.11E−05. (b) DAGLB; β=0.713, P=6.02E−04. (c) FCER1G; β=−1.176, P=6.33E−04. (d) S100A10; β=−0.428, P=1.24E−03. (e) IFI30; β=−0.677, P=1.12E−03.
Enrichment analyses
Enrichment analysis of the ranked probes from the follow-up analyses using GOrilla yielded a number of significant GO terms at q<0.05, with many terms depicting processes related to regulation of cell cycle pathways. The top-reported pathway was ‘negative regulation of apoptotic process’ (P=5.07 × 10−6, q=0.043). A full list of identified pathways can be found in Supplementary Table S4.
Network-based analyses
Six co-expression modules were detected at pre-treatment (excluding the grey module). Modules were well preserved at post treatment and follow-up, indicating little change in the composition of modules across the treatment time points (module details can be found in the Supplementary Information). No significant association was found between percentage reduction in CGI-S and change in module eigengene for any module at post treatment or follow-up (result tables provided in Supplementary Information).
Discussion
To our knowledge, this is the first study to examine genome-wide gene expression profiles and psychological treatment response. We examined the relationship between transcriptomic changes across the full course of treatment (pre-treatment, post treatment and follow-up) and treatment outcome in 102 adults receiving exposure-based CBT. Although no probes reached significance when correcting for multiple testing (q<0.05), expression changes in a small number of probes were associated with changes in symptom severity from pre-treatment to post treatment and pre-treatment to follow-up at a suggestive level (q<0.5).
In the post-treatment analyses, the top nominally significant probe was in a gene related to mitochondrial ATP synthase (ATP5D). A further related gene (ATP5H) was also within the top probes. The function of these genes is moderately well characterised. Recently, it has been suggested that mitochondrial dysfunction may play a role in disorders such as schizophrenia45 although the importance of these processes for mental health outcomes such as anxiety and depression is not clear.
A small number of interesting probes reached a suggestive threshold in the follow-up analyses. The top nominally significant probe was related to the gene PTBP1, which plays a functional role in pre-mRNA processing and the regulation of splicing events. Recent research has suggested that downregulation of the gene may be a risk factor for Parkinson’s disease,46 however there is little evidence as yet for the role of the gene in psychiatric outcomes.
A key probe of interest at follow-up was part of the diacylglycerol lipase beta gene (DAGLB). DAGLB is known to be involved in the biosynthesis of 2-arachidonoyl-glycerol (2-AG), a key endogenous endocannabinoid in the endocannabinoid signalling system.47, 48 Interestingly, the role of the endocannabinoid system in anxiety and anxious behaviours is supported by a considerable body of research in both human and animal studies.49, 50, 51 In this study, we found an increase in DAGLB expression with greater treatment response. Previous research has demonstrated that reduced 2-AG levels are associated with increased risk of outcomes such as post-traumatic stress disorder and major depression,52, 53, 54 while animal studies have demonstrated that increases in 2-AG through pharmacological intervention may reduce anxiety-like behaviours.55, 56 Given the role of DAGLB in the synthesis of 2-AG, it is therefore of great interest that increases in DAGLB expression corresponded with greater reductions in severity, while decreases in DAGLB expression corresponded with lower reductions in severity. Genetic variation in the endocannabinoid system has also been investigated with respect to psychological therapy response, whereby several polymorphisms demonstrated a nominally significant association with outcome, although findings did not reach significance after correcting for multiple testing.57
The suggestive probe with the largest effect size at follow-up was part of the high-affinity IgE receptor FCER1G gene, which is known to be a key unit in allergic reactions and regulates several aspects of the immune response. Interestingly, this was not the only immune-related gene implicated in the top probes, with IFI30 (associated with immune regulation and previously implicated in posttraumatic stress disorder; Neylan et al.58) and STAT1 (regulation of immune related signalling; Hu and Ivashkiv59) both showing suggestive results. Previous research has implicated immune pathways as an important biological system involved in many mental health outcomes60, 61, 62 and as such this represents a plausible candidate for psychological therapy response.
Another interesting probe detected at follow-up was part of the S100A10 gene, which encodes for the p11 protein. The gene is thought to play a role in serotonergic signalling through interaction with serotonin receptors, and has also been linked to response to stress via regulation by glucocorticoids (Svenningsson et al.63). Downregulation of p11 mRNA and protein levels has been implicated in depressive behaviours and risk of suicide, and several categories of antidepressants have been shown to increase p11 expression in brain tissues (Svenningsson et al.63). Conversely, in the sample presented here, a decrease in S100A10 expression was observed corresponding with a better response to treatment. Also, it should be noted that gene expression in the current study was determined from peripheral blood samples (not brain regions). Nevertheless, while the role of this gene in response to psychological therapies is unclear, expression of the S100A10 gene represents an interesting potential target for further research.
Previous studies examining candidate gene expression and response to a psychological therapy have predominantly focussed on the HPA-axis-related gene FKBP5.16, 17 Notably, gene expression changes in FKBP5 were not associated with treatment outcome at post treatment in our sample, and were only nominally associated with outcome at follow-up. In fact, contrary to previous reports, participants with a better treatment outcome at follow-up displayed a reduction in FKBP5 expression. However, there were some differences between these studies and the current report. Namely, previous research used a candidate gene approach, compared to the genome-wide approach utilised in the current study. Sample sizes were also smaller (n=39, n=20), and both studies focussed on adults with posttraumatic stress disorder rather than the range of anxiety diagnoses reported here.
As discussed in the Introduction, the majority of studies examining genetic and epigenetic correlates of response to psychological therapy currently also focus on candidate genes. The first genome-wide association study of therapy response (in children with anxiety disorders64) found no genetic variants significantly associated with psychological treatment outcome. In addition, previously implicated candidate genes (where available in the array data) were not replicated, suggesting that the effect of individual genes on treatment response is likely to be small. Studies of DNA methylation predictors of treatment response and changes during treatment have yielded moderate effect sizes, though to date few samples have more than 100 participants, and as yet no study has used epigenome-wide data in the context of psychological treatment response.
As well as the known mechanistic relationship between epigenetic patterns and gene expression, research has demonstrated that underlying genetic variation has the potential to influence both DNA methylation (for example, allele-specific methylation65) and gene expression (for example, eQTL66). Recent work examining factors associated with response to negative environmental influences (such as abuse) has suggested that epigenetic changes associated with psychological outcomes may be influenced by genotype.67 To this end, a study from our team showed genotype-dependent changes in FKBP5 DNA methylation associated with treatment outcome.14 However, in a companion paper to this article combining genome-wide genetic and transcriptomic data (including an extended sample from this cohort38), a number of eQTLs (DNA sequence variation associated with gene expression) were identified, but interactions between genetic variants and treatment response were not significantly associated with expression levels. Nonetheless, future therapygenetics research would benefit from the continued use of genome-wide protocols, and the integration of genetic, epigenetic and transcriptomic information in order to elucidate the potential biological mechanisms underlying psychological treatment response.
In this study, we also performed data-driven clustering using WGCNA methods (detailed in the Supplementary Information42) but results from these analyses were not informative. Six network modules were identified within the pre-treatment data, but did not show any substantial changes in composition across the treatment period, indicating a largely similar molecular landscape across the treatment period. Changes in the expression profiles of these modules were not found to be associated with treatment outcome at post treatment or at follow-up. We also examined potential biological pathways by conducting enrichment analysis of the probe-level results. The results implicated that a number of functional processes such as cell cycle regulation were overrepresented in the top-ranked genes.
To our knowledge, this is the first study to examine gene expression profiles at a genome-wide level with respect to treatment outcome following a psychological therapy. However, the top results discussed here do not reach statistical significance, and should be considered preliminary. In addition, there are a number of caveats in the design that should be considered. Firstly, while the work presented here represents the largest study of gene expression with respect to psychological therapy outcomes, the sample size is still relatively small. Effect sizes for changes in symptoms are likely to be larger than for the corresponding changes in gene expression. Using the gene with the largest effect size in the suggestive results reported here as an example (FCER1G), statistical power analyses suggest that a sample size greater than 230 would be required to accurately detect an effect of the same size with 80% power (conducted using powerreg in Stata). Using a threshold of α=1.4 × 10-5 (reflecting the 4381 gene probes considered), the current sample was large enough to detect a variant explaining 23% of the variance in change in symptoms with 80% power (conducted using the pwr package in R). Statistical power is enhanced by the use of network-based approaches such as WGCNA. However, our sample was still only large enough to detect a module explaining 11% of the variance in change in symptoms with 80% power. Given that treatment response is thought to be influenced by a number of factors of small effect, it is likely that the current study is underpowered, and much greater sample sizes are needed. Linked to this issue, this sample had a moderate level of heterogeneity, with variability in treatment specifics (such as length) and diagnoses that may have affected the results. In addition, no control group (who had not received treatment) was available for this study. Therefore, it is possible that any changes detected in our sample may be explained by other factors. Future studies in this growing area would benefit from a focus on collecting much larger samples, preferably with control groups for comparison. The expansion of internet-based CBT trials and large CBT services, enabling therapists and treatment centres to reach a wider number of participants, are likely to be a useful resource for research examining predictors of treatment response. Greater sample sizes may also be achieved through large-scale collaborations, combining data from multiple treatment sites, treatment protocols and diagnoses. Although these approaches will likely lead to greater heterogeneity in the sample, for a predictor or biological correlate of treatment response to have a potential clinical utility it must be able to rise above this noise robustly in a range of treatment settings.
Secondly, in this study we have used clinician-rated severity of the treated diagnosis as the primary treatment outcome. Although the CGI is a well recognised and validated measure, it only concerns the severity of disorder. Another important aspect of treatment outcome in mental disorders, particularly in fear-related disorders such as anxiety, is reduction in impairment. Further work in this area should consider changes in levels of impairment as well as diagnosis severity. Finally, this study was conducted in a clinical setting with live participants, and therefore required the use of peripheral samples. However, whilst peripheral samples may not be wholly representative of brain expression patterns, transcriptomic comparisons in previous research have indicated that the expression of over 80% of genes is shared between peripheral blood and other tissues (including brain).68 In addition, the use of peripheral tissue is a necessity of biomarker and treatment response studies.
Conclusion
In summary, this study represents the first report of genome-wide expression profiles with respect to response to a psychological therapy. We find suggestive evidence for the role of gene expression changes in a small number of biologically plausible candidate genes, although none reach a corrected level of significance. If replicated, these findings have the potential to further our understanding of the biological changes underlying response to psychological therapies.
Acknowledgments
Study was supported by an Alexander von Humboldt-Professorship to JM. KJL was supported by grants from the Jacobs Foundation and the UK Medical Research Council (MR/J011762/1). RK was supported by a UK Medical Research Council Grant (MR/K021281/1). SDJ was supported by NARSAD Young Investigator Grant (YI 60373). JRIC and SR were supported by the Alexander von Humboldt Foundation (subcontract to TCE from an Alexander von Humboldt Professorship awarded to JM). This study presents independent research part-funded by the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Footnotes
Supplementary Information accompanies the paper on the Translational Psychiatry website (http://www.nature.com/tp)
GB is a consultant in pre-clinical genetics for Eli Lilly. All other authors declare no financial interests.
Supplementary Material
References
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry 2005; 62: 593–602. [DOI] [PubMed] [Google Scholar]
- Fineberg NA, Haddad PM, Carpenter L, Gannon B, Sharpe R, Young AH et al. The size, burden and cost of disorders of the brain in the UK. J Psychopharmacol 2013; 27: 761–770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendlowicz MV, Stein MB. Quality of life in individuals with anxiety disorders. Am J Psychiatry 2000; 157: 669–682. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Sijbrandij M, Koole SL, Andersson G, Beekman AT, Reynolds CF. The efficacy of psychotherapy and pharmacotherapy in treating depressive and anxiety disorders: a meta-analysis of direct comparisons. World Psychiatry 2013; 12: 137–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norton PJ, Price EC. A meta-analytic review of adult cognitive-behavioral treatment outcome across the anxiety disorders. J Nerv Ment Dis 2007; 195: 521–531. [DOI] [PubMed] [Google Scholar]
- Stewart RE, Chambless DL. Cognitive–behavioral therapy for adult anxiety disorders in clinical practice: a meta-analysis of effectiveness studies. J Consult Clin Psychol 2009; 77: 595–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler AC, Chapman JE, Forman EM, Beck AT. The empirical status of cognitive-behavioral therapy: A review of meta-analyses. Clin Psychol Rev 2006; 26: 17–31. [DOI] [PubMed] [Google Scholar]
- Olatunji BO, Cisler JM, Deacon BJ. Efficacy of cognitive behavioral therapy for anxiety disorders: a review of meta-analytic findings. Psychiatr Clin North Am 2010; 33: 557–577. [DOI] [PubMed] [Google Scholar]
- Eley TC. The future of therapygenetics: where will studies predicting psychological treatment response from genomic markers lead? Depress Anxiety 2014; 31: 617–620. [DOI] [PubMed] [Google Scholar]
- Lester KJ, Eley TC. Therapygenetics: using genetic markers to predict response to psychological treatment for mood and anxiety disorders. Biol Mood Anxiety Disord 2013; 3: 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perroud N, Salzmann A, Prada P, Nicastro R, Hoeppli M, Furrer S et al. Response to psychotherapy in borderline personality disorder and methylation status of the BDNF gene. Transl Psychiatry 2013; 3: e207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts S, Lester KJ, Hudson JL, Rapee RM, Creswell C, Cooper PJ et al. Serotonin transporter methylation and response to cognitive behaviour therapy in children with anxiety disorders. Transl Psychiatry 2014; 4: e444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziegler C, Richter J, Mahr M, Gajewska A, Schiele MA, Gehrmann A et al. MAOA gene hypomethylation in panic disorder[mdash]reversibility of an epigenetic risk pattern by psychotherapy. Transl Psychiatry 2016; 6: e773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts S, Keers R, Lester KJ, Coleman JRI, Breen G, Arendt K et al. HPA axis related genes and response to psychological therapies: genetics and epigenetics. Depress Anxiety 2015; 32: 861–870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yehuda R, Daskalakis NP, Desarnaud F, Makotkine I, Lehrner A, Koch E et al. Epigenetic biomarkers as predictors and correlates of symptom improvement following psychotherapy in combat veterans with PTSD. Front Psychiatry 2013; 4: 118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy-Gigi E, Szabó C, Kelemen O, Kéri S. Association among clinical response, hippocampal volume, and FKBP5 gene expression in individuals with posttraumatic stress disorder receiving cognitive behavioral therapy. Biol Psychiatry 2013; 74: 793–800. [DOI] [PubMed] [Google Scholar]
- Szabó C, Kelemen O, Kéri S. Changes in FKBP5 expression and memory functions during cognitive–behavioral therapy in posttraumatic stress disorder: a preliminary study. Neurosci Lett 2014; 569: 116–120. [DOI] [PubMed] [Google Scholar]
- Kéri S, Szabó C, Kelemen O. Blood biomarkers of depression track clinical changes during cognitive-behavioral therapy. J Affect Disord 2014; 164: 118–122. [DOI] [PubMed] [Google Scholar]
- Redei EE, Andrus BM, Kwasny MJ, Seok J, Cai X, Ho J et al. Blood transcriptomic biomarkers in adult primary care patients with major depressive disorder undergoing cognitive behavioral therapy. Transl Psychiatry 2014; 4: e442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider S, Margraf J, Barlow D, DiNardo P, Becker E. Diagnostisches Interview bei Psychischen Störungen (DIPS). Springer: Berlin, 2006. [Google Scholar]
- Margraf J, Schneider S, Ehlers A. DIPS: Diagnostisches Interview bei Psychischen Störungen. Springer-Verlag: Berlin, 2013. [Google Scholar]
- Margraf J. Diagnostisches Kurz-Interview bei psychischen Stoerungen (Testmappe mit Handbuch und Interviewleitfaden). Springer: Berlin, 1994 (Mini-DIPS).
- In-Albon T, Suppiger A, Schlup B, Wendler S, Margraf J, Schneider S. Validität des Diagnostischen Interviews bei psychischen Störungen (DIPS für DSM-IV-TR). Zeitschrift klinische Psychol Psychother 2008; 37: 33–42. [Google Scholar]
- Bruchmüller K, Margraf J, Suppiger A, Schneider S. Popular or unpopular? Therapists’ use of structured interviews and their estimation of patient acceptance. Behav Ther 2011; 42: 634–643. [DOI] [PubMed] [Google Scholar]
- Suppiger A, In-Albon T, Hendriksen S, Hermann E, Margraf J, Schneider S. Acceptance of structured diagnostic interviews for mental disorders in clinical practice and research settings. Behav Ther 2009; 40: 272–279. [DOI] [PubMed] [Google Scholar]
- Suppiger A, In-Albon T, Herren C, Bader K, Schneider S, Margraf J. Reliabilität des Diagnostischen Interviews bei Psychischen Störungen (DIPS für DSM-IV-TR) unter klinischen Routinebedingungen. Verhaltenstherapie 2008; 18: 237–244. [Google Scholar]
- Wannemüller A, Sartory G, Jöhren H-P, Margraf J. Ein Fünf-Sitzungsprogramm zur Behandlung von Zahnbehandlungsangst. Verhaltenstherapie Verhaltensmedizin 2015; 36: 177–196. [Google Scholar]
- Guy W. ECDU Asessment Manual for Psychopharmacology, Revised. US Department of Health, Education, and Welfare: Bethesda. 1976.
- Ding L-H, Xie Y, Park S, Xiao G, Story MD. Enhanced identification and biological validation of differential gene expression via Illumina whole-genome expression arrays through the use of the model-based background correction methodology. Nucleic Acids Res 2008; 36: e58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmid R, Baum P, Ittrich C, Fundel-Clemens K, Huber W, Brors B et al. Comparison of normalization methods for Illumina BeadChip HumanHT-12 v3. BMC Genomics 2010; 11: 349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du P, Kibbe WA, Lin SM. lumi: a pipeline for processing Illumina microarray. Bioinformatics 2008; 24: 1547–1548. [DOI] [PubMed] [Google Scholar]
- Oldham MC, Langfelder P, Horvath S. Network methods for describing sample relationships in genomic datasets: application to Huntington’s disease. BMC Syst Biol 2012; 6: 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Team RC. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing: Vienna, Austria, 2015. [Google Scholar]
- Johnson WE, Li C, Rabinovic A. Adjusting batch effects in microarray expression data using empirical Bayes methods. Biostatistics 2007; 8: 118–127. [DOI] [PubMed] [Google Scholar]
- Eddelbuettel D, Sanderson C. RcppArmadillo: Accelerating R with high-performance C++ linear algebra. Comput Stat Data Anal 2014; 71: 1054–1063. [Google Scholar]
- Gaujoux R, Seoighe C. CellMix: a comprehensive toolbox for gene expression deconvolution. Bioinformatics 2013; 29: 2211–2212. [DOI] [PubMed] [Google Scholar]
- Abbas AR, Wolslegel K, Seshasayee D, Modrusan Z, Clark HF. Deconvolution of blood microarray data identifies cellular activation patterns in systemic lupus erythematosus. PLoS ONE 2009; 4: e6098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman JRI, Lester KJ, Roberts S, Keers R, Lee Sh, De Jong S et al. Separate and combined effects of genetic variants and pre-treatment whole blood gene expression on response to exposure-based cognitive behavioural therapy for anxiety disorders. World J Biol Psychiatry 2016; 18: 215–226. [DOI] [PubMed] [Google Scholar]
- StataCorpStata Statistical Software: Release 11. StataCorp LP: College Station, TX, 2009. [Google Scholar]
- Eden E, Navon R, Steinfeld I, Lipson D, Yakhini Z. GOrilla: a tool for discovery and visualization of enriched GO terms in ranked gene lists. BMC Bioinformatics 2009; 10: 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B Methodol 1995; 57: 289–300. [Google Scholar]
- Langfelder P, Horvath S. WGCNA: an R package for weighted correlation network analysis. BMC Bioinformatics 2008; 9: 559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langfelder P, Luo R, Oldham MC, Horvath S. Is my network module preserved and reproducible. PLoS Comput Biol 2011; 7: e1001057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edgar R, Domrachev M, Lash AE. Gene Expression Omnibus: NCBI gene expression and hybridization array data repository. Nucleic Acids Res 2002; 30: 207–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajasekaran A, Venkatasubramanian G, Berk M, Debnath M. Mitochondrial dysfunction in schizophrenia: pathways, mechanisms and implications. Neurosci Biobehav Rev 2015; 48: 10–21. [DOI] [PubMed] [Google Scholar]
- Santiago JA, Potashkin JA. Network-based metaanalysis identifies HNF4A and PTBP1 as longitudinally dynamic biomarkers for Parkinson’s disease. Proc Natl Acad Sci USA 2015; 112: 2257–2262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bisogno T, Howell F, Williams G, Minassi A, Cascio MG, Ligresti A et al. Cloning of the first sn1-DAG lipases points to the spatial and temporal regulation of endocannabinoid signaling in the brain. J Cell Biol 2003; 163: 463–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jain T, Wager-Miller J, Mackie K, Straiker A. Diacylglycerol Lipaseα (DAGLα) and DAGLβ cooperatively regulate the production of 2-arachidonoyl glycerol in autaptic hippocampal neurons. Mol Pharmacol 2013; 84: 296–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lafenêtre P, Chaouloff F, Marsicano G. The endocannabinoid system in the processing of anxiety and fear and how CB1 receptors may modulate fear extinction. Pharmacol Res 2007; 56: 367–381. [DOI] [PubMed] [Google Scholar]
- Ashton CH, Moore PB. Endocannabinoid system dysfunction in mood and related disorders. Acta Psychiatr Scand 2011; 124: 250–261. [DOI] [PubMed] [Google Scholar]
- Ruehle S, Rey AA, Remmers F, Lutz B. The endocannabinoid system in anxiety, fear memory and habituation. J Psychopharmacol 2012; 26: 23–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill MN, Bierer LM, Makotkine I, Golier JA, Galea S, McEwen BS et al. Reductions in circulating endocannabinoid levels in individuals with post-traumatic stress disorder following exposure to the world trade center attacks. Psychoneuroendocrinology 2013; 38: 2952–2961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill MN, Miller GE, Carrier EJ, Gorzalka BB, Hillard CJ. Circulating endocannabinoids and N-acyl ethanolamines are differentially regulated in major depression and following exposure to social stress. Psychoneuroendocrinology 2009; 34: 1257–1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parolaro D, Realini N, Vigano D, Guidali C, Rubino T. The endocannabinoid system and psychiatric disorders. Exp Neurol 2010; 224: 3–14. [DOI] [PubMed] [Google Scholar]
- Busquets-Garcia A, Puighermanal E, Pastor A, de la Torre R, Maldonado R, Ozaita A. Differential role of anandamide and 2-arachidonoylglycerol in memory and anxiety-like responses. Biol Psychiatry 2011; 70: 479–486. [DOI] [PubMed] [Google Scholar]
- Sciolino NR, Zhou W, Hohmann AG. Enhancement of endocannabinoid signaling with JZL184, an inhibitor of the 2-arachidonoylglycerol hydrolyzing enzyme monoacylglycerol lipase, produces anxiolytic effects under conditions of high environmental aversiveness in rats. Pharmacol Res 2011; 64: 226–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lester KJ, Coleman JR, Roberts S, Keers R, Breen G, Bögels S et al. Genetic variation in the endocannabinoid system and response to cognitive behavior therapy for child anxiety disorders. Am J Med Genet B Neuropsychiatr Genetics 2016; 174: 144–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neylan TC, Sun B, Rempel H, Ross J, Lenoci M, O'Donovan A et al. Suppressed monocyte gene expression profile in men versus women with PTSD. Brain Behav Immun 2011; 25: 524–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu X, Ivashkiv LB. Cross-regulation of signaling pathways by interferon-γ: implications for immune responses and autoimmune diseases. Immunity 2009; 31: 539–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mondelli V, Dazzan P, Pariante CM. Immune abnormalities across psychiatric disorders: clinical relevance. BJPsych Adv 2015; 21: 150–156. [Google Scholar]
- Jones KA, Thomsen C. The role of the innate immune system in psychiatric disorders. Mol Cell Neurosci 2013; 53: 52–62. [DOI] [PubMed] [Google Scholar]
- Capuron L, Miller AH. Immune system to brain signaling: neuropsychopharmacological implications. Pharmacol Ther 2011; 130: 226–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Svenningsson P, Kim Y, Warner-Schmidt J, Oh Y-S, Greengard P. p11 and its role in depression and therapeutic responses to antidepressants. Nat Rev Neurosci 2013; 14: 673–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman JRI, Lester KJ, Keers R, Roberts S, Curtis C, Arendt K et al. Genome-wide association study of response to cognitive–behavioural therapy in children with anxiety disorders. Br J Psychiatry 2016; 209: 236–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schalkwyk LC, Meaburn EL, Smith R, Dempster EL, Jeffries AR, Davies MN et al. Allelic skewing of DNA methylation is widespread across the genome. Am J Hum Genet 2010; 86: 196–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicolae DL, Gamazon E, Zhang W, Duan S, Dolan ME, Cox NJ. Trait-associated SNPs are more likely to be eQTLs: annotation to enhance discovery from GWAS. PLoS Genet 2010; 6: e1000888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klengel T, Mehta D, Anacker C, Rex-Haffner M, Pruessner JC, Pariante CM et al. Allele-specific FKBP5 DNA demethylation mediates gene–childhood trauma interactions. Nat Neurosci 2013; 16: 33–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liew CC, Ma J, Tang HC, Zheng R, Dempsey AA. The peripheral blood transcriptome dynamically reflects system wide biology: a potential diagnostic tool. J Lab Clin Med 2006; 147: 126–132. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.