Summary
Objectives
To describe our experience and success in the use of low cost mesh for the repair of inguinal hernias in consenting adult patients
Methods
A prospective study was carried out from August 2010 to December 2013 in ten district hospitals across Northern Ghana. The patients were divided into four groups according to Kingsnorth's classification of hernias. Low cost mesh was used to repair uncomplicated groin hernia. Those hernias associated with complications were excluded. We assessed the patients for wound infection, long term incisional pain and recurrence of hernia. The data collected was entered, cleaned, validated and analyzed.
Results
One hundred and eighty-four patients had tension-free repair of their inguinal hernias using non-insecticide impregnated mosquito net mesh. The median age of the patients was 51 years. The male to female ratio was 7:1. Using Kingsnorth's classification, H3 hernias were (62, 33.7%), followed by the H1 group (56, 30.4%). Local anaesthesia was used in 70% and less than 5% had general anaesthesia. The cost of low cost mesh to each patient was calculated to be $ 1.8(GH¢7.2) vs $ 45(GH¢ 180) for commercial mesh of same size. The benefit to the patient and the facility was enormous. Wound hematoma was noticed in 7% while superficial surgical site infection was 3%. No patient reported of long term wound pain. There was no recurrence of hernia.
Conclusion
Low cost mesh such as sterilized mosquito net mesh for use in hernioplasty in resource-limited settings is reasonable, acceptable and cost-effective, it should be widely propagated.
Funding
None declared
Keywords: low cost mesh, hernioplasty, Northern Ghana
Introduction
Inguinal hernias are common globally with varied incidence and prevalence. In the United States of America (USA) the incidence of inguinal hernia was estimated to be 217 per 100,000 person years1 while in United Kingdom(UK) the incidence was 130 per 100,000 population.2 The prevalence of inguinal hernia among men and women was 27% and 3% respectively in the UK.2 The incidence of inguinal hernia is 175 per 100,000 person years in Tanzania in East Africa.3 In the West African sub-region, the prevalence of inguinal hernia was reported to be 7.7% some three decades ago.4
Inguinal hernias, when not repaired electively, may be associated with adverse outcome and a mortality rate of 5.3–40%.5 In strangulated hernias, 24% require bowel resection.6 In Ghana, inguinal herniorrhaphy is the second most commonly performed surgical procedure after caesarean section in district hospitals.7
Suture repair techniques such as Bassini, MacVay and Nylon darn are most favoured methods of hernia repair across Africa because they are cheaper compared with hernioplasties using prosthetic mesh material.6,8–10 The polypropylene mesh material was an ideal material for hernioplasty over half a century ago.11–13
Further work to discover a cheaper alternative material because of the high cost of the polypropylene mesh, has been ongoing. In the past two decades several authors have demonstrated that low cost mesh such as the mosquito net mesh is safe, effective, affordable and readily available for use in humans.13–16
We demonstrate our experience with the use of sterilized low cost nylon mesh for tension-free repair of inguinal hernias in our subjects; its effectiveness and safety in elective surgeries in resource poor communities (low and middle income countries) is discussed.
Methods
A prospective study was carried out from August 2010 to December 2013 at the Tamale Teaching Hospital (TTH), and ten district hospitals across the Upper East and Upper West Regions of Ghana. Ethical clearance was sought from the TTH for the use of the material and written consent was also obtained from patients who had inguinal hernias and were twenty years of age or older. A data collection sheet was designed and each surgeon completed this for each inguinal hernia operated using a sterilized mosquito net mesh (low cost mesh).
The characteristics of the hernias were also categorized using the clinical classification system recommended by Kingsnorth. Sterilized, non-insecticide impregnated 100% nylon mosquito net mesh was used for hernioplasty (using Lichtenstein technique) under local, spinal or general anaesthesia, where appropriate. Intravenous ampicillin, two grams stat, was given as prophylaxis. The patients were detained for 24 hours postoperatively and then discharged home. The wounds were usually inspected on the third postoperative day.
The patients were followed up postoperatively for complications such as pain, seroma formation, wound infection, rejection, and recurrence after discharge of patient home. After discharge, follow up was by telephone for the next four weeks and subjects were instructed to report any complications related to the hernia repair. Patients with complicated hernias were excluded from the study. Data was entered in Epidata version 3.0, cleaned and validated. Basic statistical analysis including age distribution, frequencies and percentages were computed using SPSS version 16.0 for windows. The results are presented in text, tables and figures.
Results
Of the one hundred and eighty four (184) consecutive patients, 12 had bilateral hernias repaired at the same sitting; thus 196 sterilized pieces of nylon mesh were used. There were 161 males and 23 females.
This gives a male to female ratio of 7:1. Their ages ranged from 20–86 with a median age of 51, and interquartile range of 36–68 years. Their mean haemoglobin level was 13.3 ± 1.8 (SD) g/dl, and range 6.9–18.8 g/dl. The characteristics of the inguinal hernias are described in Table 1.
Table 1.
Baseline characteristics of inguinal hernias (n=184)
| Characteristic of hernia | Number of patients (%) |
| Side of hernia: Right Left Bilateral |
97 (52.7) 75 (40.8) 12 (5.5) |
| Type of hernia; Reducible Irreducible (incarcerated) Bilateral Recurrent Strangulated |
143 (77.7) 23 (12.6) 12 (6.5) 5 (2.7) 1 (0.5) |
Only one patient had strangulated hernia but did not require bowel resection. The distribution of the hernias as classified by Kingsnorth 17 is shown in Table 2.
Table 2.
Distribution of hernia as classified by Kingsnorth (n=184)
| Kingsnorth type of hernia | Number of patients | Percent of total |
| H1 | 56 | 30.4 |
| H2 | 45 | 24.5 |
| H3 | 62 | 33.7 |
| H4 | 21 | 11.4 |
| Total | 184 | 100.0 |
The type of hernia and choice of anaesthesia is shown in Table 3.
Table 3.
Type of hernia and choice of anaesthesia (n=184)
| Type of Hernia | Type of Anaesthesia Number of patients (%) |
||
| Local | Spinal | General | |
| Bilateral | 5 (2.7) | 6 (3.3) | 1 (0.5) |
| Reducible | 119 (64.7) | 23 (12.5) | 1 (0.5) |
| Irreducible | 6 (3.3) | 10 (5.4) | 7 (3.8) |
| Recurrent | 1 (0.5) | 4 (2.2) | 0 |
| Strangulated | 0 | 0 | 1 (0.5) |
| Total | 131 (71.2) | 43 (23.4) | 10 (5.4) |
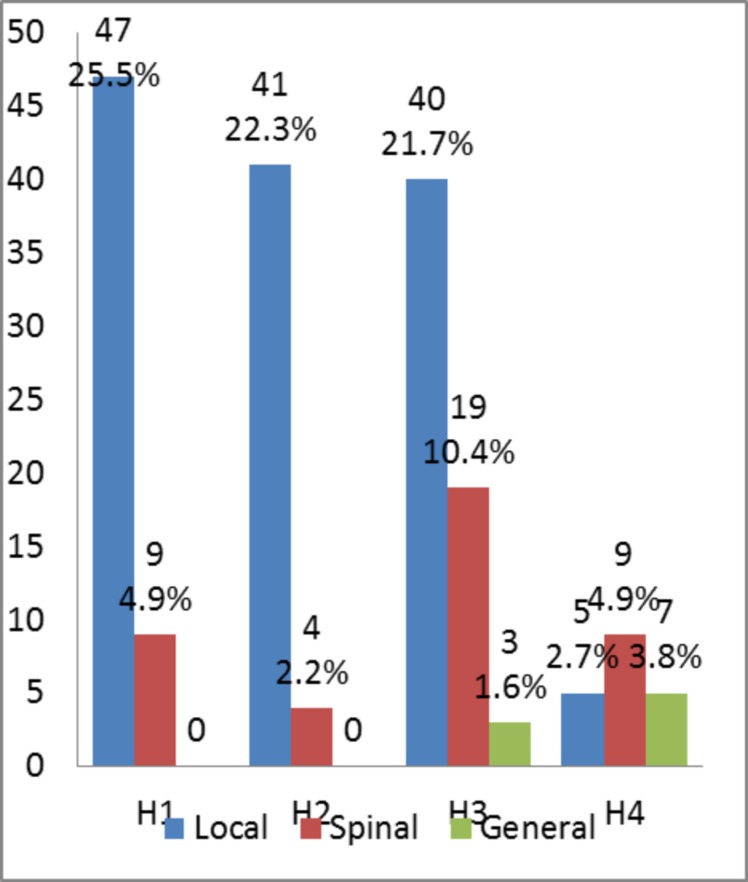
The relationship between Kingsnorth category of hernia and choice of anaesthesia is as shown in Figure 1. Local anaesthesia was used in 133 (72.3%), spinal anaesthesia in 42 (22.8%) and general anaesthesia in 9 (4.9%) patients.
Figure 1.
Relationship between Kingsnorth class of hernia and type of anaesthesia
Of the 184 patients who were operated using the low cost nylon mesh, only one had a strangulated hernia but did not require bowel resection. Postoperative scrotal hematoma occurred in 6.7% of our patients.
Some 2.9% of the study subjects had discharge of pus from the wound, which was successfully treated with antibiotics. We did not have to remove the mesh in any of the situations described above. No rejection of mesh or recurrence was recorded during the period of this study. No death was also recorded.
Discussion
This study demonstrates our experience with the low cost nylon mesh in the repair of inguinal hernia in elective situations in our environment. Our multicentre study showed the material was effective, and linked to minor wound complications.
Post-operative scrotal hematoma occurred in about 7% of our patients. About 3% of the patients had minor surgical site infections associated with discharge of pus, which were treated with antibiotic and wound dressing. We did not have to remove the mesh. No rejection of mesh or recurrence was recorded during the 4-year period of this study. Earlier report from scientific workers on the use of mosquito net mesh material showed wound infection rate of 2% to 4.7%13,14, hematoma of 4%–5%14,15, recurrence of 0.3%13 and no rejection of prosthetic material.
We found the complication rates of our study subjects were similar when compared with results from authors who used standard commercial prolene mesh. These authors observed no major complications except for hematoma formation in 6.9% and recurrence rate of 0.6%.18–21
Local anaesthesia has been recommended for elective hernia repair in resource poor settings because of its considerable advantages including its cost effectiveness.22–24 In this series, the majority of our patients (71.2%) were operated under local anaesthesia. Patients who presented with reducible hernias were mainly operated using local infiltration of lidocaine with adrenaline.
The cost of Ultrapro® a commercial mesh is $108 per patient. 16 In Ghana, VyPro™, a commercial mesh that is readily available cost about $45 for a 6 × 11cm size. The cost of locally made individual 10 × 15-cm mosquito net mesh was estimated to range between US$0.0043–0.014 14,16 and the cost of sterilization and packaging was US$1.46 per mesh. 14 Yang J et al in their review paper suggested that the price of low-cost mesh was generally less than 1/1,000 the price of commercial mesh.25 Ghana's National Health Insurance Scheme (NHIS) covers about 95% of diseases in the country.
The approved tariff of the National Health Insurance Scheme (NHIS) for an inguinal hernia repair at the district hospital in 2014 was Gh¢205.00 26 equivalent to $70.00. This amount does not include the cost of a mesh such as VyPro™. All our patients had valid NHIS cards and were operated using homemade sterilized nylon mosquito net mesh. If the standard mesh material were to be used, the cost of one (e.g VyPro™) measuring 6×11 cm, the same size as the mosquito net mesh, will be about GH¢135($45).
Thus the patient will have to pay an extra $45 if the standard mesh were to be used. When a sterilized mosquito net mesh of the same size as the standard VyPro™ is used, the patient paid only GH¢ 5.4 ($1.8) extra as compared to the $45 he/she paid for the standard commercial mesh. From this it is obvious what the financial benefits are to the patient. The end result of treatment with both meshes is the same from our experience so far. The use of sterilized mosquito net mesh in hernioplasty is not a novel idea as Stock in 1954 reported on its use for hernia repair with no complications and recommended it as a potential material for future use.27
Subsequently, several scientific authors have reported on the results of their work using sterilized mosquito net in hernia repair.13–16
The nylon mosquito net is made of material similar to the nylon suture which has been used by practicing surgeons in herniorrhaphy, especially in Africa, for many years.6,8,10,16 It is widely accepted that surgeons take responsibility for the sterility of instruments and other prosthetic materials that they use in their trade. In a similar fashion, surgeons who would wish to use these affordable homemade sterilized mosquito net meshes should comply with international quality assurance and sterility standards.16,28
An important epidemiologic feature of inguinal hernia is its sex and age distribution. Inguinal hernia is predominantly a male disease among the adult population.2,29,30 In our study male to female ratio was 7:1. While emergency inguinal hernia repair is common among adults between 21 and 41 years in Africa,6 European data suggest the rates of emergency surgery continue to increase with advancing age, with a mean age of 58 years.2 Among Europeans, Primatesta P and Goldacre MJ reported the mean age of elective hernia repair to be 53 years,2 while we found that the median age of our patients was 51 years.
The characteristics of inguinal hernias are not different in various communities.14–16 The characteristics of inguinal hernia seen and treated in our series are similar to findings from earlier series. Bilateral hernias were less common than unilateral hernias; most unilateral hernias were on the right side; reducible hernias formed a majority when compared with recurrent and irreducible (incarcerated) hernias.
We also found it useful to categorize the characteristics of the hernias using a system of clinical classification recommended by Kingsnorth.17 This classification enabled us to segregate the simple from the more complicated hernias. Groin only hernias (Kingsnorth H1 and H2) were operated using local infiltration with lidocaine as the preferred analgesic.
Of a total of 184 subjects the more difficult reducible inguino-scrotal hernias such as H3 category, were operated using local infiltration of lidocaine in (21.7%) as compared to those who were operated under spinal (10.4%) or general anaesthesia (1.6%). The more difficult hernias, namely H3 and H4, were assigned to experienced surgeons in the team for the tension-free mesh repair to be performed.
Only one patient had a strangulated inguinal hernia but did not require bowel resection.
Conclusion
Nylon mosquito net mesh is a suitable material for the repair of groin hernias in our environment.
It is effective, cheap and is linked to minor wound complications. We suggest a wider use of this material in low and middle-income countries, where the commercial mesh is rather expensive and unaffordable for most of our impoverished patients.
Acknowledgement
We express our sincere thanks to all APRIDEC Medical Outreach Group members who contributed in diverse ways to bring free medical services to the deprived areas in Northern Ghana. From your effort we obtained and now share data with the scientific community.
References
- 1.Zendejas B, Ramirez T, Jones T, Kuchena A, Ali SM, Hernandez-Irizarry R, et al. Incidence of inguinal hernia repairs in Olmsted County, MN: a population-based study. Ann Surg. 2013 Mar;257(3):520–526. doi: 10.1097/SLA.0b013e31826d41c6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Primatesta P, Goldacre MJ. Inguinal hernia repair: incidence of elective and emergency surgery, readmission and mortality. Int J Epidemiol. 1996 Aug;25(4):835–839. doi: 10.1093/ije/25.4.835. [DOI] [PubMed] [Google Scholar]
- 3.Nordberg EM. Incidence and estimated need of caesarean section, inguinal hernia repair, and operation for strangulated hernia in rural Africa. Br Med J Clin Res Ed. 1984 Jul 14;289(6437):92–93. doi: 10.1136/bmj.289.6437.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Belcher DW, Nyame PK, Wurapa FK. The prevalence of inguinal hernia in adult Ghanaian males. Trop Geogr Med. 1978 Mar;30(1):39–43. [PubMed] [Google Scholar]
- 5.Ohene-Yeboah M, Abantanga FA. Inguinal Hernia Disease in Africa: A Common but Neglected Surgical Condition. West Afr J Med. 2011;30(2):77–83. [PubMed] [Google Scholar]
- 6.Ohene-Yeboah M. Strangulated external hernias in Kumasi. West Afr J Med. 2003 Dec;22(4):310–313. doi: 10.4314/wajm.v22i4.28053. [DOI] [PubMed] [Google Scholar]
- 7.Abantanga FA, Hesse AJ, Sory E, Osen H, Choo S, Abdullah F, et al. Policies for improving access to and quality of essential basic surgical care at district hospitals in Ghana. PMJG. 2012;1(1):3–8. [Google Scholar]
- 8.Ramyil VM, Iya D, Ogbonna BC, Dakum NK. Safety of daycare hernia repair in Jos, Nigeria. East Afr Med J. 2000 Jun;77(6):326–328. doi: 10.4314/eamj.v77i6.46647. [DOI] [PubMed] [Google Scholar]
- 9.Fall B, Betel ME, Diarra O, Ba M, Dia A, Diop A. [Complications of treatment of adult's groin hernia: a report of 100 cases comparative study between Bassini and Mac Vay's technics] Dakar Méd. 2005;50(1):37–40. [PubMed] [Google Scholar]
- 10.Adesunkanmi AR, Agbakwuru EA, Badmus TA. Obstructed abdominal hernia at the Wesley Guild Hospital, Nigeria. East Afr Med J. 2000 Jan;77(1):31–33. doi: 10.4314/eamj.v77i1.46371. [DOI] [PubMed] [Google Scholar]
- 11.Watkin DFL, Kirk RM. Abdominal wall and groin. In: Kirk RM, editor. General surgical operations. 4th edition. London: Churchill Livingstone; 2000. pp. 118–127. [Google Scholar]
- 12.Amid PK, Shulman AG, Lichtenstein IL. Open “tension-free” repair of inguinal hernias: the Lichtenstein technique. Eur J Surg Acta Chir. 1996 Jun;162(6):447–453. [PubMed] [Google Scholar]
- 13.Tongaonkar RR, Reddy BV, Mehta VK, Singh NS, Shivade S. Preliminary Multicentric Trial of Cheap Indigenous Mosquito-Net Cloth for Tension-free Hernia Repair. Indian J Surg. 2003;65(1):89–95. [Google Scholar]
- 14.Clarke MG, Oppong C, Simmermacher R, Park K, Kurzer M, Vanotoo L, et al. The use of sterilised polyester mosquito net mesh for inguinal hernia repair in Ghana. Hernia. 2009 Jun;13(3):341–341. doi: 10.1007/s10029-008-0460-3. [DOI] [PubMed] [Google Scholar]
- 15.Kiss A. The Use of Mosquito-Net Cloths as Prosthesis in Inguinal Hernia Repair: An Experience in Southern Sudan. Surg Sci. 2012;3(3):155–157. [Google Scholar]
- 16.Freudenberg S, Sano D, Ouangré E, Weiss C, Wilhelm TJ. Commercial Mesh versus Nylon Mosquito Net for Hernia Repair. A Randomized Double-blind Study in Burkina Faso. World J Surg. 2006;30:1784–1789. doi: 10.1007/s00268-006-0108-3. [DOI] [PubMed] [Google Scholar]
- 17.Kingsnorth AN. A clinical classification for patients with inguinal hernia. Hernia. 2004:8. doi: 10.1007/s10029-004-0228-3. [DOI] [PubMed] [Google Scholar]
- 18.Ja C, Ja B, Jk C. Repair of inguinal hernia in the adult with Prolene mesh. Surg Gynecol Obstet. 1988;167:124–128. [PubMed] [Google Scholar]
- 19.Neumayer L, Giobbie-Hurder A, Jonasson O, Fitzgibbons R, Dunlop D, Gibbs J, et al. Open Mesh versus Laparoscopic Mesh Repair of Inguinal Hernia. N Engl J Med. 2004;350:1819–1827. doi: 10.1056/NEJMoa040093. [DOI] [PubMed] [Google Scholar]
- 20.Awad SS, Yallalampalli S, Srour AM, Bellows CF, Albo D, Berger DH. Improved outcomes with the Prolene Hernia System mesh compared with the time-honored Lichtenstein onlay mesh repair for inguinal hernia repair. Am J Surg. 2007;193:697–701. doi: 10.1016/j.amjsurg.2006.08.087. [DOI] [PubMed] [Google Scholar]
- 21.Yerdel MA, Akin EB, Dolalan S, Turkcapar AG, Pehlivan M, Gecim IE, et al. Effect of Single-Dose Prophylactic Ampicillin and Sulbactam on Wound Infection After Tension-Free Inguinal Hernia Repair With Polypropylene Mesh. Ann Surg. 2001;233:26–33. doi: 10.1097/00000658-200101000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stephenson BM, Kingsnorth AN. Inguinal hernioplasty using mosquito net mesh in low income countries: an alternative and cost effective prosthesis. BMJ. 2011;343:d7448–d7448. doi: 10.1136/bmj.d7448. [DOI] [PubMed] [Google Scholar]
- 23.Wilhelm TJ, Anemana S, Kyamanywa P, Rennie J, Post S, Freudenberg S. Anaesthesia for elective inguinal hernia repair in rural Ghana - appeal for local anaesthesia in resource-poor countries. Trop Doct. 2006;36:147–149. doi: 10.1258/004947506777978046. [DOI] [PubMed] [Google Scholar]
- 24.Kingsnorth A. Local Anesthetic Hernia Repair: Gold Standard for One and All. World J Surg. 2009;33:142–144. doi: 10.1007/s00268-008-9790-7. [DOI] [PubMed] [Google Scholar]
- 25.Yang J, Papandria D, Rhee D, Perry H, Abdullah F. Low-cost mesh for inguinal hernia repair in resource-limited settings. Hernia. 2011;15:485–489. doi: 10.1007/s10029-011-0827-8. [DOI] [PubMed] [Google Scholar]
- 26.NHIS, author. National Health Insurance Scheme, Tariffs for Private/Primary Care Hospitals(Catering inclusive) Accra, Ghana: NHIA; 2014. [Google Scholar]
- 27.Stock FE. Repair of large herniae with nylon mesh. Lancet. 1954;263:395–396. doi: 10.1016/s0140-6736(54)90930-7. [DOI] [PubMed] [Google Scholar]
- 28.Koukourou A, Lyon W, Rice J, Wattchow DA. Prospective randomized trial of polypropylene mesh compared with nylon darn in inguinal hernia repair. Br J Surg. 2001;88:931–934. doi: 10.1046/j.0007-1323.2001.01818.x. [DOI] [PubMed] [Google Scholar]
- 29.Ohene-Yeboah M, Abantanga F, Oppong J, Togbe B, Nimako B, Amoah M, et al. Some aspects of the epidemiology of external Hernias in Kumasi, Ghana. Hernia. 2009;13:529–532. doi: 10.1007/s10029-009-0491-4. [DOI] [PubMed] [Google Scholar]
- 30.Badoe EA B. External herniae in Accra—some epidemiological aspects. Afr J Med Sci. 1973;4:51–58. [PubMed] [Google Scholar]