Abstract
Comparative Medicine is typically defined as a discipline which relates and leverages the biological similarities and differences among animal species to better understand the mechanism of human and animal disease. It has also been defined as a field of study concentrating on similarities and differences between human and veterinary medicine and is increasingly associated with animal models of human disease, including the critical role veterinarians, animal resource centers, and Institutional Animal Care and Use Committees play in facilitating and ensuring humane and reproducible laboratory animal care and use. To this end, comparative medicine plays a pivotal role in reduction, refinement, and replacement in animals in biomedical research. On many levels, comparative medicine facilitates the translation of basic science knowledge into clinical applications; applying comparative medicine concepts throughout the translation process is critical for success. In addition to the supportive role of comparative medicine in the research enterprise, its role as a distinct and independent scientific discipline should not be lost. Although comparative medicine’s research “niche” is not one particular discipline or disease process, rather, it is the investigative mindset that seeks to reveal common threads that weave different pathophysiologic processes into translatable approaches and outcomes using various models.
Keywords: Comparative Medicine, Translation, Animal Models, Veterinarians, One Health
Comparative medicine has historically been at the center of scientific advancements as evidenced by Jenner, Koch, and Sabin. Edward Jenner studied animal models of rabies and observed that previously infected dogs were protected and, likewise, people milking cows were protected against cowpox, culminating into seminal vaccine studies [1]. Robert Koch discovered the organisms causing anthrax, tuberculosis, cholera. His focus on culture techniques to propagate organisms and transmission studies in animal models led to Koch’s Postulates which set forth four criteria to determine the causal relationship of a specific microorganism to a disease [2]. In a 1956 paper Albert Sabin underscored the importance of comparative medicine by stating “approximately 9,000 monkeys, 150 chimpanzees and 133 human volunteers have been used thus far in the quantitative studies of various characteristics of different strains of polio virus. [These studies] were necessary to solve many problems before an oral polio vaccine could become a reality.” [3].
In fact, the importance of comparative medicine was understood early in biomedical research and likely got its roots from Erasmus Darwin’s publication “Zoonomia” where he discusses infectious disease of both humans and animals [4]. However, it was Claude Bourgelat, the founder of the first veterinary college in Lyon France in 1761, coined the term “comparative pathobiology” prior to the existence of the veterinary profession [1]. Today, however, comparative medicine is often plagued by an identity crisis. Clearly, the development and use of animal models transcends virtually all scientific disciplines seeking translational applications. Ironically, the broad dissemination of “comparative medicine” across scientific disciplines has bestowed a generic or dependent connotation—as if “comparative medicine” is an “adjective” rather than a “noun.” The placement of “comparative” before “medicine,” in itself, invites a wide array of interpretations, depending on who is interpreting. For example, a narrow interpretation could reference individual, ethnic, or other differences between individuals, rather than a broader intraspecies perspective. Interestingly, Sir Bradley, in 1927, articulated the importance of comparative medicine as a distinct discipline by characterizing it as the study of disease processes in all animals and potentially, plants, and with the help of all available means, is an instrument for the proper comprehension of problems of human and veterinary medicine [5]. He and several predecessors held a common belief that human and veterinary medicine were branches of a larger medicine, “One Medicine”, and that comparative medicine was the medicine of the future [5,6]. The Greek god of medicine and healing, Asklepios, was believed to treat both man and animals which is why the rod of Asklepios is used as a symbol of human medicine, pharmacy, and veterinary medicine [1]. One Medicine eventually gave rise to the present “One Health” initiative, which aims to unite human and veterinary medicine. This thinking foreshadowed the dominant role of animal models in “bench side to bedside” translation (Figure 1).
Figure 1.

The Unifying Symbolism of Human and Animal health.
Studying diseases of animals and humans has long history dating back to the 1200s and likely stemmed from several plagues during that time [1]. In contemporary times, the necessity of using animals in research came to light publicly as a result of the atrocities associated with experimentation on imprisoned adults and children during the Second World War (Figure 2). The outcome was the Nuremberg Code, which is a collection of ethical principles for human experimentation stemming from the outcome of Nuremberg “Doctors’” trials at the end of the war. Included in the measures aimed at protecting human subjects, the Code states “the experiment should be so designed and based on the results of animal experimentation and a knowledge of the natural history of the disease or other problem under study, that the anticipated results will justify the performance of the experiment” [7]. In essence, the Code was an early requirement to apply “comparative medicine” to the translation of animal study in order to better inform the appropriateness of human studies.
Figure 2.
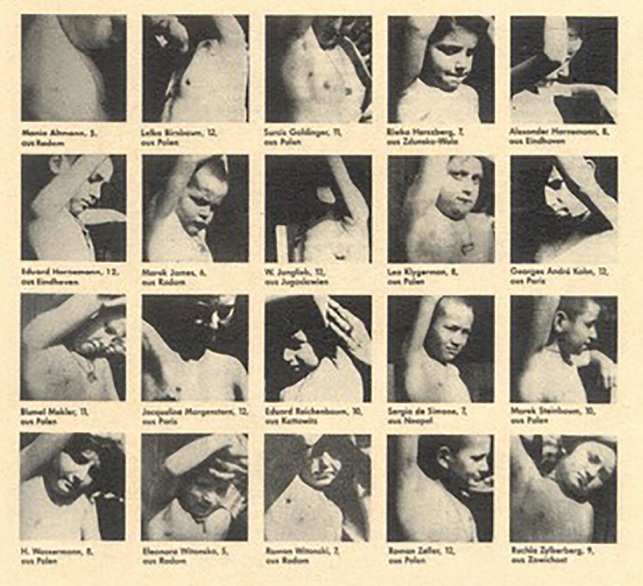
Children Being Used in Tuberculosis Studies.
In parallel, the Federal Food, Drug, and Cosmetic Act of 1938 and its subsequent amendments required new drugs to be shown safe before marketing. Drug development generally requires that two or more species (one rodent, one non-rodent) are tested because of the potential for a drug to impact one species differently than the other. Animal testing is used to determine the pharmokinetics of the drug, how it is metabolized, the toxicity of the drug and its breakdown products (metabolites), and how quickly the drug and its metabolites are excreted from the body [8]. More recently, in 2002, Congress authorized and FDA passed the Animal Efficacy Rule (“Animal Rule”), a regulation which permits the approval of some products based on safety testing in humans and efficacy testing in animals. The rule is meant to allow FDA to approve products for “serious or life-threatening conditions caused by exposure to lethal or permanently disabling toxic biological, chemical, radiological, or nuclear substances.” [9]. The Animal Rule states that for “drugs developed to ameliorate or prevent serious or life-threatening conditions caused by exposure to lethal or permanently disabling toxic substances, when human efficacy studies are not ethical and field trials are not feasible, FDA may grant marketing approval based on adequate and well-controlled animal efficacy studies when the results of those studies establish that the drug is reasonably likely to produce clinical benefit in humans.” The Animal Rule states that FDA will rely on evidence from animal studies to provide substantial evidence of effectiveness only when all of the following four criteria are met: 1. There is a reasonably well-understood pathophysiological mechanism of the toxicity of the substance and its prevention or substantial reduction by the product; 2. The effect is demonstrated in more than one animal species expected to react with a response predictive for humans, unless the effect is demonstrated in a single animal species that represents a sufficiently well-characterized animal model for predicting the response in humans; 3. The animal study endpoint is clearly related to the desired benefit in humans, generally the enhancement of survival or prevention of major morbidity; and 4. The data or information on the kinetics and pharmacodynamics of the product or other relevant data or information, in animals and humans, allows selection of an effective dose in humans. If all of these criteria are met, it is reasonable to expect the effectiveness of the drug in animals to be a reliable indicator of its effectiveness in humans. [10]. Furthermore, the reliance on direct, real-time translation value of animal studies will become increasingly important as therapeutic regimens testing patient derived xenografts in mice are becoming a personalized medicine approach. [11,12].
Collectively, the Nuremberg Code and the FDA fueled a movement to use animal studies to predict outcomes in human studies. These requirements fostered two important components that assimilates and applies comparative medicine’s intellectual diversity: analysis and synthesis. To establish safety, there is a heavy emphasis on comparative toxicologic “analysis” to ensure results are valid, reproducible, and applicable. With the animal rule, as well as most pre-clinical/research and development studies, there is a strong emphasis on developing, predicting, establishing, and understanding mechanisms that “translate” to effective human therapies. Given the continuum of complexity inherent in animal-to-human studies, “synthesis” of information and data across a broad array scientific and clinical disciplines is needed. As it was stated in the 1920s, we should view comparative medicine and applied medicine as standing in the same relationship to each other as do pure science and applied science, which is analogy that is still apropos to contemporary biomedical research [5].
An extension of the increasing reliance on animal-based research for discovery is the need for ensuring the appropriate care and use of animals. In 1963, the National Research Council first published The Guide for the Care and Use of Laboratory Animals, which has been revised seven times, including the current eighth edition. The purpose of “The Guide” is “to assist institutions in caring for and using animals in ways judged to be scientifically, technically, and humanely appropriate” [13]. With an increased emphasis on animal-based research, it is not surprising that public concerns about the well-being of laboratory animals began to emerge. In 1966, Life Magazine chronicled the very poor conditions that dogs were housed and cared for by dog dealers that sold these dogs to research facilities. As the result of public outcry, the Animal Welfare Act was passed by Congress in 1966. The AWA was amended many times to set forth federal regulations governing the care and use of laboratory animals. In an analogous manner, the Health Research Extension act of 1985 also set forth animal care and use requirements for all Public Health Service grant awardees [14]. These regulations were set forth to, a large extent, address public concerns about animals used in research and have a common thread of ensuring appropriate care and use of laboratory animals by requiring, in effect, a multidisciplinary team, including a veterinarian and scientists, among others, to oversee animal care use. Thus, comparative medicine has also taken on regulatory responsibilities that underscores the diversity and, sometimes, confusion over the role and mission of comparative medicine.
Comparative medicine is poised to face two significant issues endemic within research, in general, but particularly applicable to animal-based research; reproducibility and translatability. In recent years, there has been increasing awareness and concern about the difficulty in obtaining reproducible data when the same experiment is conducted in a laboratory other than the laboratory where the experiment was originally conducted. The extent of this problem is underscored by publications, surveys, and workshops devoted to this topic [15-17]. The problem extends beyond biomedical experimentation as similar concerns have been raised for research conducted in psychology [18], ecology [19], nutrition [20], bioinformatics [21], human clinical medicine [22], and homeopathic disciplines [23]. Using biological system models, in particular live, sentient animal models, introduces complex variables that complicate the potential for successful reproducibility of a study [17]. In conjunction with selecting the most appropriate model, ensuring consistent experimental protocols and procedures, involving adequately trained and skilled investigators, and controlling and reducing extraneous variables will help minimize the risk of not being able to successfully reproduce an experimental finding—but requires diligence and collaboration of the entire scientific community. It was also recognized that reporting consistency such as those suggested in the ARRIVE [24] and CONSORT [25] guidelines, which include details about animal care and use, will help improve reproducibility.
The scientific literature and clinical trials data base are plagued with examples of drugs that showed promise in laboratory animals but were not effective in clinical trials [16,26]. For example, translation of disease modifying therapies in neurodegenerative disease has been particularly disappointing [27]. For example, an analysis of 543 animal and human Parkinson’s studies demonstrated a translational gap for potentially disease-modifying interventions that resulted, in part, from mouse study designs that failed to model the progressive nature and typical late intervention timing or that relate mechanistic or neuropathological data to longitudinal outcomes. The authors conclude that this is a failure in translation and, in these cases, measures to improve reproducibility are not likely to help [27].
Funding agencies also recognize the translation gap. For example, Center for Cancer Research, National Cancer Institute recognize that a significant hurdle in the translation of information from the laboratory to the clinic is the availability of appropriate preclinical cancer models. To address this issue, the Comparative Oncology Program (COP) was established with a goal of including naturally occurring cancer seen in pet animals into studies of cancer biology and drug development. These studies benefit human as well as animals and epitomizes the One Health approach that is encoded in comparative medicine’s germline [28].
Clearly, reproducibility and translation depend on proper analysis. It is critical to the scientific process that is interwoven throughout the entire scientific process and it is analytical methodology that is often associated with comparative medicine. However, it is synthesis that is the origins of the analytical process and represents the true essence of “Comparative Medicine” as a distinct and independent discipline. Comparative medicine is naturally interdisciplinary and programmatic and this foreshadowed the functional organization of contemporary science into programs and centers. It is a “silent core” of the scientific enterprise. Unfortunately, its comparative medicine’s diversity that also favors having “too many intellectual irons in the fire at the expense of none getting hot.”
However, it may be the broad conceptual framework of comparative medicine that could offer an avenue to leave the quagmire behind in translational biomedicine. It can even be argued that the scope and partnerships of scientists and practicing veterinarians should be further extended. At present, the vast majority of apparent breakthroughs emerge from studies in various inbred rodent strains by scientists with training in natural sciences, biology, and medicine in particular. This, in itself, is extremely limiting and predicts likelihood of failure regarding translational value. First, inbred strain differences can have enormous impact on outcome of intervention. One of the best example for this is the outcome of calorie restriction on lifespan. It is now believed at the societal level, moderate and controlled calorie restriction in a chronic manner is beneficial on health and lifespan for humans [29]. However, it is less emphasized that it may not be the case, but only for some. Studies on the effect of calorie restriction on lifespan showed that there are certain strains of mice that have increased lifespan on calorie restrictions, while others have either no change or actually respond with shorter lifespan [30]. Similar ambiguity was found regarding the effect of calorie restriction on non-human primates [31,32]. Thus, it can be a gamble when somebody engages in voluntary calorie restriction to better health and prolong life. There is 33 percent chance for either scenario (longer lifespan, no change in lifespan, or shortened lifespan). In principle, every subject engaging in that lifestyle adjustment runs an experiment with n = 1, which by definition cannot be scientifically quantified. This simple equation is coming from the principles of comparative medicine and there are numerous examples for such ambiguities in any outcome measure in health. Beyond strain differences (genetic background differences), there are also fundamental differences between species and sexes. Exposure to various environmental factors during development and adulthood also skews genetic predisposition of a trait. If the goal of contemporary biomedicine is to deliver novel approaches for the enhancement of health of individual subjects, they need to embrace principles such as those governing the discipline of comparative medicine. This driving principle of comparative medicine delivers, by default, outcomes that are desirable both from health and societal perspectives. For example, over the last decade, Yale Comparative Medicine developed an interdisciplinary program that capitalizes on the interaction between faculty with diverse background, including animal and plant biology, human and veterinary medicine, mathematics, physics, economics, and the performing arts (http://medicine.yale.edu/compmed/icsnm/). The models of spans from humans, animals, and plants. One of the goals of this initiative is to bring together natural and social sciences to synergize in advancing each other’s goals. An underlying argument to support this effort is that the governing principles of a discipline (e.g., cellular biology) may have relevance to others (e.g., economics). The cross fertilization of disciplines with very different cultures may enable the effort of each to reach its goals more effectively.
As humans, we are, by nature, more likely to be concerned with the relationship of things to us rather than things to each other. It is easier to analyze, rather than synthesize [5]. Clearly, controlling and reducing factors affecting experimental reproducibility and optimizing experimental design underpin study validity. However, translating results from mechanistic animal-based study to strategies for human disease modulation is likely to require synthesis of mechanistically diverse models, species, and intervention approaches. With advances in genomics and access to “big data”, comparative medicine will continue to evolve.
Comparative medicine is functionally “peppered” throughout the scientific enterprise and is value added to biomedical research. However, if it is not otherwise anchored to a legitimate center, it undermines its visibility and potential for leveraging its independent contributions to model development and translation. We argue some of the barriers of bench side to bedside translation could be circumvented if comparative medicine was better entrenched within the foundation of the scientific enterprise. It is as if comparative medicine is often “by chance” rather than “by design.” We feel that this is manifested within the biomedical research enterprise, in part, as reproducibility and, importantly, translation failures that slow the pace of medical advancements. These medical advancements are often the only visible “return on investment” the public sees and is an important counterbalance to the “cost” of the research enterprise, both in terms of monetary investment and the philosophical price associated with use of animals. Ultimately, it must be remembered that public support is critical to continued “investments” in biomedical research.
Glossary
- COP
Comparative Oncology Program
Author Contributions
Macy and Horvath contributed equally to the manuscript.
References
- Jensen-Jarolim E. Comparative Medicine; Anatomy and Physiology, Definition of Comparative Medicine: History and New Identity, Springer-Verlag; Wien: 2014, pp. 1-18. [Google Scholar]
- Koch R. Verfahren zur Untersuchung, zum Conservieren und Photographiren der Bakterien. Beitrage zure Biologie der Pflanzen, 1877:2:399-434. [Google Scholar]
- Sabin AB. Oral Poliovirus Vaccine. JAMA. 1965;194:872–6. [DOI] [PubMed] [Google Scholar]
- Darwin EA. Zoonomia or the laws of organic life in three parts. 1796. Volume II 4th ed. US: Published by Edward Earl; 1818. p. 2213. [Google Scholar]
- Bradley C. What is Comparative Medicine? Proc R Soc Med. 1927. November;(1):129–34. [PMC free article] [PubMed] [Google Scholar]
- Mills W. Valedictory address to the graduates in comparative medicine and veterinary science. Journal for Comparative Medicine and Veterinary Archives. 1896;XVII:25. [PMC free article] [PubMed] [Google Scholar]
- Trials of War Criminals before the Nuremberg Military Tribunals under Control Council Law No. 10. Volume 2 Washington (D.C.): U.S. Government Printing Office; 1949. pp. 181–2. [Google Scholar]
- Product Development Under the Animal Rule Guidance for Industry. 2015 Available from: https://www.fda.gov/downloads/drugs/guidancecomplianceregulatoryinformation/guidances/ucm399217.pdf .
- Gaffney A. FDA releases new animal rule guidance with focus on vaccines and animal health. Raps. 2014. Available from: http://www.raps.org/regulatory-focus/news/2014/05/19022/FDA-New-Animal-Rule-Draft-Guidance/
- Malaney P, Nicosia SV, Davé V. One mouse, one patient paradigm: new avatars of personalized cancer. Cancer Lett. 2014. March;344(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hidaldo M, Amant F, Biankin AV, Budinska E, Byrne AT, Caldas C, et al. Patient derived xenograft models: an emerging platform for translational cancer research. Cancer Discov. 2014. September;(9):998–1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guide for the care and use of laboratory animals. 8th ed. Washington (DC): The National Academic Press; 2011. pp. 1–209. [Google Scholar]
- Public Health Service Policy on Humane Care and Use of Laboratory Animals Available from: https://grants.nih.gov/grants/olaw/references/phspolicylabanimals.pdf.
- Prinz F, Schlange T, Asadullah K. Believe it or not: how much can we rely on published data on potential drug targets. Nat Rev Drug Discov. 2011;10:712. [DOI] [PubMed] [Google Scholar]
- Begley CG, Ellis LM. Drug development: raise standards for preclinical cancer research. Nature. 2012;483:531–3. [DOI] [PubMed] [Google Scholar]
- Roundtable Workshop In Brief IL. The Missing “R”: Reproductibility in a changing research landscape. A workshop of the roundtable on science and welfare in laboratory animal use (an ILAR Roundtable series). 2015 Available from: http://www.nap.edu/21835 .
- Vergés A, Jackson KM, Bucholz KK, Trull TJ, Lane SP, Sher KJ. Personality disorders and the persistence of substance use disorders: A reanalysis of published NESARC findings. J Abnorm Psychol. 2014;123:809–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haddaway NR, Verhoeven JT. Poor methodological detail precludes experimental repeatability and hampers synthesis in ecology. Ecol Evol. 2015;5(19):4451-4454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorkin BC, Kuszak AJ, Williamson JS, Hopp DC, Betz JM. The challenge of reproducibility and accuracy in nutrition research: resources and pitfalls. Adv Nutr. 2016;7:383–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stegmayer G, Pividori M, Milone DH. A very simple and fast way to access and validate algorithms in reproducible research. Brief Bioinform. 2016;17:180–3. [DOI] [PubMed] [Google Scholar]
- Snider KT, Johnson JC, Degenhardt BF, Snider EJ, Burton DC. Association of low back pain, somatic dysfunction, and lumbar bone mineral density: reproducibility of findings. J Am Osteopath Assoc. 2014;114:356–67. [DOI] [PubMed] [Google Scholar]
- Weingärtner O. A formal approach to the problem of reproducing experimental effects with homeopathic potencies. J Altern Complement Med. 2009;15:287–91. [DOI] [PubMed] [Google Scholar]
- Kilkenny C, Browne WJ, Cuthill IC, Emerson M, Altman DG. Improving bioscience research reporting: the ARRIVE guidelines for reporting animal research. PLoS Biol. 2010;8:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz KF, Altman DG, Moher D. CONSORT Group. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. PLoS Med. 2010;7:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perrin S. Make mouse studies work. Nature. 2014;507:423–5. [DOI] [PubMed] [Google Scholar]
- Zeiss CJ, Allore HG, Beck AP. Established patterns of animal study design undermine translation of disease-modifying therapies for Parkinson’s disease. PLoS One. 2017;12(2):1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCI Center for Cancer Research. Comparative Oncology Program. Available from: https://ccrod.cancer.gov/confluence/display/CCRCOPWeb/Agreements.
- Most J, Tosti V, Redman LM, Fontana L. Calorie restriction in humans: An update. Ageing Res Rev. 2016;S1568-1637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao CY, Rikke BA, Johnson TE, Diaz V, Nelson JF. Genetic variation in the murine lifespan response to dietary restrict ion: from life extension to life shortening. Aging Cell. 2010;9:92–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattison JA, Roth GS, Beasley TM, Tilmont EM, Handy AM, Herbert RL, et al. Impact of caloric restriction on health and survival in rhesus monkeys from the NIA study. Nature. 2012;489:318–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemnitz JW. Calorie restriction and aging in nonhuman primates. ILAR J. 2011;52:66–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattison JA, Roth GS, Beasley TM, Tilmont EM, Handy AM, Herbert RL, et al. Impact of caloric restriction on health and survival in rhesus monkeys from the NIA study. Nature. 2012;489:318–21. [DOI] [PMC free article] [PubMed] [Google Scholar]


