Abstract
Gastrointestinal (GI) metastasis from a primary breast carcinoma is uncommon, with the rectum being one of the least reported sites in the literature. We report a case of a 79-year-old woman who underwent treatment for an infiltrative lobular carcinoma of the right breast with nodal involvement, and 10 years later developed recurrence in the form of rectal metastasis. Spread to the GI tract is most commonly seen with lobular breast carcinomas. Any patient with a history of breast cancer presenting typically or atypically with abdominal symptoms or altered bowel habit should raise a high index of suspicion for recurrent or metastatic disease.
Keywords: breast cancer, carcinogenesis, breast surgery
Background
Breast cancer is the the most common form of cancer affecting women and is known to spread to the bones, lungs, liver, brain and soft tissues.1 Gastrointestinal (GI) metastasis, however, is rarely seen in clinical practice, with spread to the rectum being particularly uncommon.2 Invasive lobular carcinoma (ILC) of the breast constitutes up to 10% of all breast cancers.3 They are the the most common subtype implicated in metastasis to the GI tract, with an incidence between 2% and 18%.2 3 These metastatic lesions can often masquerade as primary GI tumours and, therefore, pose an important diagnostic challenge, as the management of metastatic and primary tumours may differ. In this paper, we present a unique case of a 79-year-old woman who developed rectal metastasis after treatment for invasive lobular breast carcinoma. We believe that this report will educate the readership on this subject.
Case presentation
A 79-year-old woman underwent a left mastectomy in 1996 for a grade II infiltrating ductal carcinoma with vascular space infiltration (0 out of 12 lymph nodes involved). She completed 5-year treatment with tamoxifen and was followed up every 4–6 months. During follow-up in February 2005, she was found to have a lump in the right breast and subsequently underwent a right mastectomy with axillary node clearance. Histology revealed a 2.8 cm infiltrating lobular carcinoma (14 out of 17 lymph nodes involved), and immunochemistry for oestrogen receptor (OR) status was positive, which categorised the patient as ‘high risk’. Consequently, she had adjuvant radiotherapy to the chest wall and lymph node areas and was started on anastrozole (Arimidex). The patient was followed up in the oncology clinic on a yearly basis from 2006 to 2009 with no evidence of recurrence or metastasis. Anastrozole was discontinued in 2009 and she was discharged from follow-up.
On 22 May 2015, the patient was admitted to the hospital with a 2-month history of non-specific abdominal, lower back and anal pain. She reported significant weight loss and change in her bowel habit. Abdominal examination was unremarkable and there was no evidence of lymphadenopathy in the neck, axillae or groin. Digital rectal examination revealed some impacted stools but no palpable tumour.
Investigations
CT scan of her abdomen and pelvis showed diffuse wall thickening and areas of inflammatory change in the terminal ileum and proximal caecum, and a stricture of the transverse colon (figure 1). There were no focal lesions in the stomach or small bowel and no features of retroperitoneal or intra-abdominal lymphadenopathy. The CT scan also showed incidental findings of bilateral hydronephrosis and biliary duct dilatation. The patient was discharged with an appointment for an urgent outpatient colonoscopy and magnetic retrograde cholangiopancreatogram (MRCP) to assess bile duct dilatation.
Figure 1.
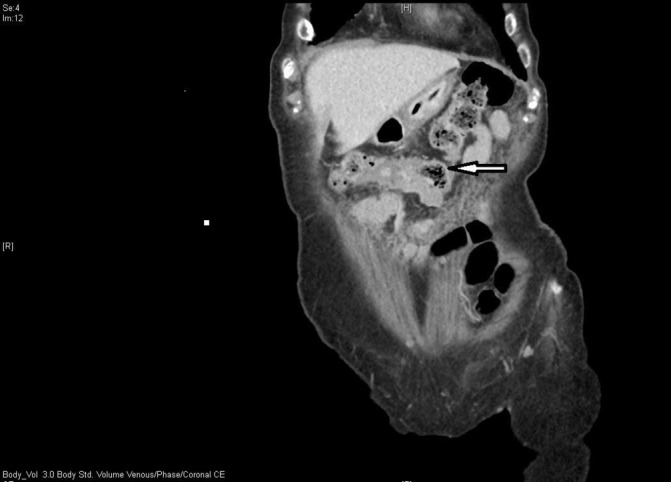
CT scan image of the large bowel stenosis (arrow).
MRCP showed a distended gall bladder with some sludge but no gallstones, and normal looking intrahepatic and extrahepatic bile ducts patterns. The patient presented for her colonoscopy but the procedure was abandoned as she became unwell with diarrhoea and vomiting, and was admitted to hospital. She underwent a successful colonoscopy, after several failed attempts due to poor tolerance to the procedure, in July 2015 which showed five rectal sessile polyps (the largest being 3 mm), three of which were excised (using cold biopsy) and sent for investigation. The histology revealed infiltration with metastatic lobular breast carcinoma, consistent with the histology of the lesion removed in the right breast in 2005. The cells were positive for cytokeratin AE1/AE3, GATA binding protein 3 and OR (Quick score 7—moderate intensity, >66% nuclear staining), and negative for the S100 protein, human melanoma black 45, leucocyte common antigen, CDX2 protein and CD68 glycoprotein. Unfortunately, there were insufficient cells for assessment of progesterone receptor and human epidermal growth factor receptor 2 status. This patient's blood tests in July 2015 were relatively unremarkable apart from a raised carbohydrate antigen 15–3 (572 kU/L) and faecal calprotectin (1195 ug/g), with mild renal impairment as shown by a low eGFR (estimated Glomerular Filteration Rate) of 58.8. In addition, a blood sample was sent for measurement of carcinoembryonic antigen but unfortunately, the sample was insufficient, and was not repeated. She had a further colonoscopy a few weeks later, which showed stenosis in the distal sigmoid colon with oedematous mucosa, from which biopsies were taken. Histology showed relatively unremarkable colon mucosa, however, immunochemistry revealed a few isolated tumour cells of breast origin.
Treatment
After discussion at the colorectal multidisciplinary meeting, the patient was started on hormone treatment (letrozole 2.5 mg once daily).
Outcome and follow-up
The patient did not wish to have any further treatment or surgical intervention. Therefore, she was discharged from the hospital and community palliative nurse follow-up was arranged. The patient passed away in September 2015. The exact cause of death is not known as the patient did not have a postmortem.
Discussion
The GI tract is a relatively uncommon site of metastasis for breast cancers, and accounts for less than 1% of all metastatic cases.4 Several papers have been published on gastric metastasis and their association with ILC of the breast.2 5 The reasons for this are not fully understood but could be related to the non-cohesiveness of lobular cells and increased tendency for infiltration.6 7 Few studies report spread to the rectum with only 14 cases found in a literature review in 2012.6 In many of these cases, including a further report in 2015,4 the lobular cell type has been implicated at histopathological diagnosis.3 8–12 Large bowel stenosis and stricture, as was evident on colonoscopy of our patient, has been described in several case reports and may be a reason for clinical presentation.4 6 11
In our case report, the patient presented to the hospital with GI metastasis almost 10 years following the initial diagnosis of lobular carcinoma of the right breast and subsequent mastectomy. A range as wide as 0 to 22 years from primary breast cancer diagnosis to GI metastasis has been reported in the literature.6 This highlights the need for a high index of suspicion of recurrence or metastasis in patients with a history of breast cancer, regardless of type or time of diagnosis. It also demands a long-term follow-up in this cohort of patients which would be of value despite the presence of remission. One case report has even suggested enrolling such patients into bowel cancer screening programmes at an earlier age.4
Survival following GI metastasis of breast origin has been varied according to the literature. Several studies have shown survival at 12 months, irrespective of whether operative or non-operative (ie, chemotherapy, hormonal therapy) management was used.1 6 In our case study, the patient died within 3 months of confirmed histological diagnosis, having only had hormonal treatment. Ambroggi et al6 showed a median overall survival of 16 months (range 5–41 months) following GI metastasis, which is lower than the median survival of all women with other metastatic disease secondary to breast cancer (range 24–36 months).
Learning points.
While the gastrointestinal tract is an uncommon site for metastasis from primary breast tumours, any patient with a history of breast cancer presenting with abdominal symptoms or altered bowel habit should raise suspicion of recurrent or metastatic disease.
New extra breast lesions in such patients should warrant timely and appropriate investigation to look for evidence of possible breast metastasis. Emphasis on histological and immunohistochemical evaluation may avoid delayed diagnosis and misdiagnosis as well as provide important information to guide management.
Long-term follow-up and screening in this patient group may have a valuable role in identifying early recurrent or metastatic colorectal disease.
Footnotes
Contributors: NC wrote the manuscript. CC helped with literature review. NAQ conceived the idea and reviewed/updated the manuscript. MS approved the final manuscript.
Competing interests: None declared.
Patient consent: Detail has been removed from this case description/these case descriptions to ensure anonymity. The editors and reviewers have seen the detailed information available and are satisfied that the information backs up the case the authors are making.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Théraux J, Bretagnol F, Guedj N, et al. Colorectal breast carcinoma metastasis diagnosed as an obstructive colonic primary tumor. A case report and review of the literature. Gastroenterol Clin Biol 2009;33:1114–7. 10.1016/j.gcb.2009.05.015 [DOI] [PubMed] [Google Scholar]
- 2.Rajan S, Saeed M, Mestrah M. Ductal carcinoma of the breast metastasizing to the rectum. J Surg Case Rep 2012;2012:12 10.1093/jscr/2012.5.12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arrangoiz R, Papavasiliou P, Dushkin H, et al. Case report and literature review: metastatic lobular carcinoma of the breast an unusual presentation. Int J Surg Case Rep 2011;2:301–5. 10.1016/j.ijscr.2011.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ng CE, Wright L, Pieri A, et al. Rectal metastasis from breast cancer: a rare entity. Int J Surg Case Rep 2015;13:103–5. 10.1016/j.ijscr.2015.06.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cormier WJ, Gaffey TA, Welch JM, et al. Linitis plastica caused by metastatic lobular carcinoma of the breast. Mayo Clin Proc 1980;55:747–53. [PubMed] [Google Scholar]
- 6.Ambroggi M, Stroppa EM, Mordenti P, et al. Metastatic breast cancer to the gastrointestinal tract: report of five cases and review of the literature. Int J Breast Cancer 2012;2012:1–8. 10.1155/2012/439023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stevens JD, Danks RR. Case report of mesenteric metastases from lobular breast carcinoma. J Am Osteopath Assoc 2011;111:180–2. [PubMed] [Google Scholar]
- 8.Eljabu W, Finch G, Nottingham J, et al. Metastatic deposits of breast lobular carcinoma to small bowel and rectum. Int J Breast Cancer 2011;2011:1–4. 10.4061/2011/413949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gerova VA, Tankova LT, Mihova AA, et al. Gastrointestinal metastases from breast cancer: report of two cases. Hepatogastroenterology 2012;59:178–81. 10.5754/hge10681 [DOI] [PubMed] [Google Scholar]
- 10.Saranovic D, Kovac JD, Knezevic S, et al. Invasive lobular breast cancer presenting an unusual metastatic pattern in the form of peritoneal and rectal metastases: a case report. J Breast Cancer 2011;14:247 10.4048/jbc.2011.14.3.247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bamias A, Baltayiannis G, Kamina S, et al. Rectal metastases from lobular carcinoma of the breast: report of a case and literature review. Ann Oncol 2001;12:715–8. 10.1023/A:1011192827710 [DOI] [PubMed] [Google Scholar]
- 12.Taal BG, den Hartog Jager FC, Steinmetz R, et al. The spectrum of gastrointestinal metastases of breast carcinoma: II. the colon and rectum. Gastrointest Endosc 1992;38:136–41. 10.1016/S0016-5107(92)70378-2 [DOI] [PubMed] [Google Scholar]


