Abstract
We present a 65-year-old diabetic patient with a complex liver abscess and bacteraemia from Lactobacillus paracasei. The abscess resulted in a prolonged hospital stay due to ongoing sepsis despite ultrasound-guided drainage and broad-spectrum antibiotics. Furthermore, the patient developed several secondary complications including a right-sided pleural effusion, an inferior vena cava thrombus and septic lung emboli. The abscess was eventually managed successfully with a prolonged course of antibiotics and multiple ultrasound-guided drainage procedures.
To our knowledge, this is the first reported case of probiotic consumption, confirmed by strain identification, as the likely source of a liver abscess. Probiotic products have been widely used for many years and are advocated to the general public for their health benefits with no warning of side effects. Lactobacilli are one group of bacteria commonly used in these products. Although rare, complications have been reported. Susceptible patients, such as those who are immunocompromised, should be advised against excessive consumption.
Keywords: infections, GI-stents, diabetes, diet, vitamins and supplements
Background
In recent years, there has been growing consumer and scientific interest in probiotic bacteria with the global market estimated to reach £29 billion by 2018.1 The term probiotic describes ‘live microorganisms which, when consumed in adequate amounts are thought to confer a health benefit on the host beyond basic nutrition’.2 3 Lactobacilli are Gram-positive bacilli which constitute commensal mucosal flora and are widely advocated as probiotics. Studies have suggested a role for probiotics in the prevention and management of specific conditions, particularly if there is an imbalance in gut microbiota.4–6 However, there are no robust clinical trials which validate these findings; the same applies to the benefits claimed in healthy adults who constitute the majority of consumers.7
There is little data on the efficacy or risk profile of probiotic consumption. A 2002 report released by the World Health Organisation (WHO) and the Food and Agriculture Organisation of the United Nations (FAO) outlines four theoretical risks of probiotic consumption: systemic infection, deleterious metabolic activities, excessive immune stimulation in susceptible individuals and gene transfer.2 3 We describe a case in which the theoretical risk of infection became a real one.
Case presentation
A 65-year-old female presented to our district general hospital with a two week history of worsening lethargy, poor appetite, vomiting and rigors. She denied pain, gastrointestinal disturbances or urinary symptoms.
The patient had a past medical history of type 2 diabetes mellitus (T2DM), hypertension and hypercholesterolaemia. Her regular medications consisted of gliclazide 80 mg and metformin 1 g twice a day, and omeprazole 40 mg, sitagliptin 100 mg, lisinopril 5 mg and simvastatin 40 mg once a day, respectively.
Her father died in his early 50s of a myocardial infarction. The patient was a non-smoker and admitted to occasionally drinking alcohol. The patient also reported consuming at least one bottle of Actimel probiotic drink daily. There was no recent foreign travel.
On initial assessment, the patient was found to be hypotensive, tachycardic and febrile, with right upper quadrant tenderness on abdominal examination. There was no guarding or rebound tenderness.
Investigations
On admission, C reactive protein (CRP) was raised at 227 mg/L with a white cell count of 6.8×109/L. Liver function was deranged with alkaline phosphatase 220 U/L, alanine aminotransferase 317 U/L and gamma-glutamyl transpeptidas 444 U/L. In terms of synthetic liver function, albumin was 30 g/L and international normalized ratio 1.4. Additional findings included a serum glucose of 14.6 mmol/L and haemoglobin A1c (HbA1c) level of 7.2%, as well as acute kidney injury.
A CT abdomen demonstrated a large multilocular liver abscess measuring 87×54 mm in the right hepatic lobe (figure 1). Small volume para-aortic lymph nodes were also noted. The presence of a liver abscess was confirmed with an abdominal ultrasound and subsequent drain insertion. Admission blood cultures and subsequent drain culture were both positive for Lactobacillus paracasei.
Figure 1.
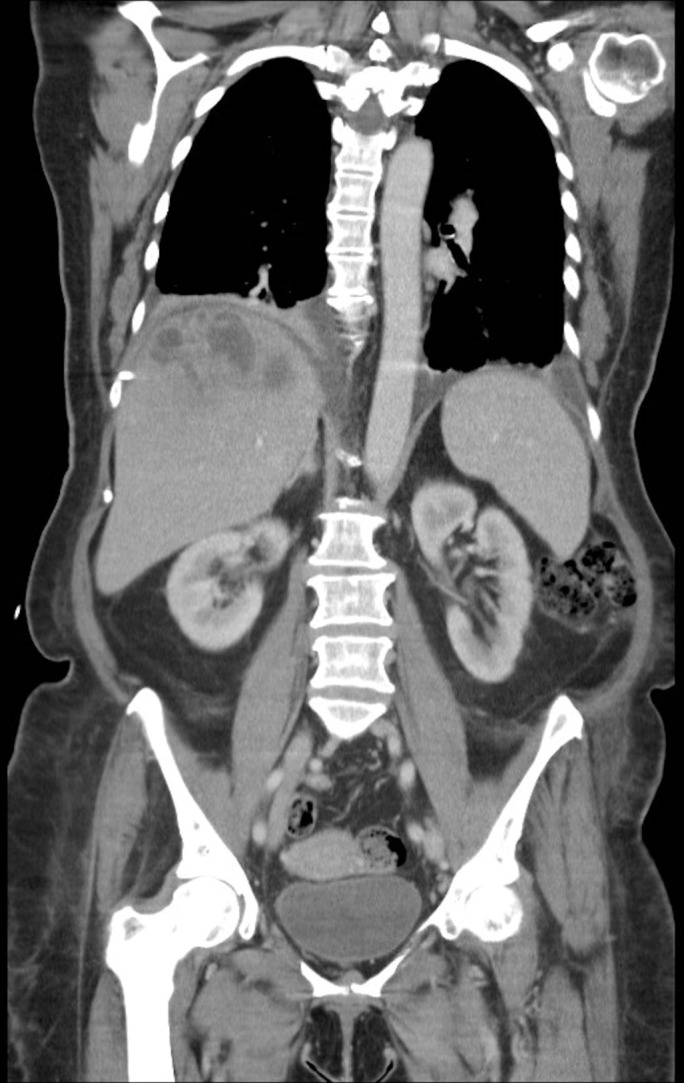
CT chest, abdomen and pelvis (coronal view) demonstrating large multilocular liver abscess in the right hepatic lobe and bilateral pleural effusion.
A week later, a CT chest and abdomen revealed multiple septic emboli in the lungs and a bilateral pleural effusion more marked on the right, with no change in the size of the liver abscess. Repositioning of the drain allowed more effective draining of the abscess, which was confirmed with further imaging.
Five weeks into the admission, a repeat CT abdomen revealed a filling defect within the inferior vena cava (IVC) suspicious for a thrombus.
Differential diagnosis
When the patient was initially admitted with sepsis and right upper quadrant tenderness, the following differential diagnoses were considered:
intra-abdominal sepsis
acute cholecystitis
acute hepatitis
pyelonephritis
Treatment
On admission, the patient was transferred to ITU for management of sepsis. She was commenced on piperacillin–tazobactam, metronidazole and gentamicin, as well as sliding-scale insulin therapy. After identifying a liver abscess with drain culture positive for L. paracasei, antibiotics were switched to co-amoxiclav. The patient was successfully stepped down to ward-based care at this point.
Despite antibiotics and abscess drainage, the patient continued to have episodes of swinging pyrexia, tachycardias and rigors. After a discussion with a consultant microbiologist, it was decided to switch antimicrobials to linezolid, metronidazole, amikacin and fluconazole.
The initial intrahepatic drain was not able to relieve all of the multiloculated liver collections due to the presence of septae. A new drain with additional fenestrations was inserted traversing the largest abscess cavities. This drain aspirate (taken 35 days into admission) cultured positive for Klebsiella pneumonia. Appropriate antibiotics were commenced. One month after initiating treatment a repeat US abdomen showed significant reduction in the size of the liver abscesses.
The IVC thrombus was treated with a treatment dose of low-molecular-weight heparin for 3 months.
Outcome and follow-up
The patient recovered well after the change of antibiotics and successful drainage of the abscess with drain flushes four times a day. The admission totalled 6 weeks with intravenous antibiotics throughout and the patient was eventually discharged with oral antibiotics and outpatient review 6 weeks later.
In view of the patient’s reported history of probiotic consumption, routine cultures were taken from a new bottle of Actimel. These cultures also grew an organism identified as L. paracasei in pure growth. Both the patient’s and the probiotic lactobacilli strains were identified in the laboratory by phenotypic appearances and matrix-assisted laser desorption-ionisation time-of-flight mass spectrometry system (Bruker) (figures 2 and 3). Reference laboratory analyses confirmed both the patient’s and the probiotic lactobacilli isolates to be identical by pulsed-field gel electrophoresis.
Figure 2.
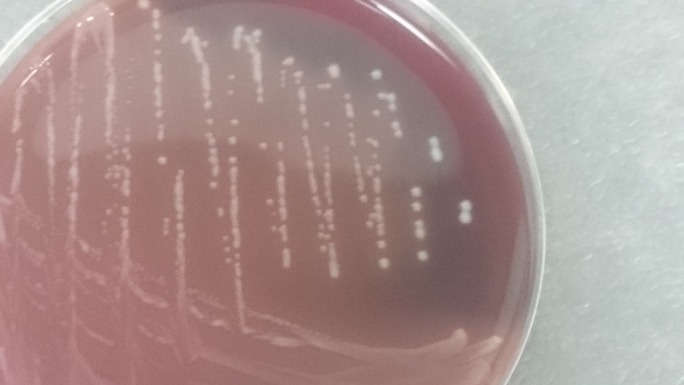
Blood agar plate with lactobacilli colonies (patients isolate).
Figure 3.

Blood agar plate with lactobacilli colonies close up view (Actimel isolate).
Discussion
Lactobacilli have been identified as potential infectious microorganisms in both immunocompetent and immunocompromised individuals.8–16 T2DM is an important cause of immune dysfunction and one that is drastically increasing in incidence.17 18
Although generally weak pathogens, the ability of lactobacilli to bind protein, collagen and extracellular matrix may in the context of immune dysfunction facilitate their ability to translocate across boundaries such as the gut wall.19 In our patient, diabetes mellitus with poor glycaemic control, as evidenced by a HbA1C level of 7.2%, and regular consumption of probiotic products is likely to have driven this process.20 Once bacteraemic there may be haematogenous seeding or even direct transfer or passage of bacteria via the portal circulation to the liver (and in our case lungs).
Why specifically abscess formation, and why at this site (other than its proximity to and direct blood supply from the gut) is unclear. Some papers have demonstrated that extracellular Gram positive bacteria including lactobacilli are able to activate transcription factors involved in cytokine signalling pathways in human macrophages, perhaps facilitating abscess formation.21
To our knowledge, this is the first reported case of probiotic consumption, confirmed by strain identification, as the likely source of a liver abscess. Other cases of serious infection secondary to lactobacillus strains have also been reported.22-26 A 1999 report presents a 74-year-old woman with non-insulin-dependent diabetes mellitus presenting with a hepatic abscess.19 Aspiration of the lesion demonstrated L. rhamnosus on a background of daily consumption of dairy products containing this pathogen. The patient also developed a right pleural effusion which was treated with a thoracotomy and surgical decortication together with management of the hepatic abscess with antibiotic therapy and abscess drainage.19 20-23 Another case report describes descending necrotising mediastinitis, a condition with a high mortality rate, to be associated with L. plantarum in a patient with advanced laryngeal cancer and untreated diabetes mellitus. The patient was managed successfully with a surgical drain and antibiotics.23 Sherid et al recently reported an 82 year old diabetic female who developed a hepatic abscess positive for lactobacillus species. Interestingly the patient also had a recent history of clostridium difficile infection and probiotic consumption as well as a previous cholecystectomy.27 The authors propose that the inflamed colonic mucosa may have further driven the mechanism described above.
Nonetheless, the aforementioned pathogens have all been reported as lactobacilli, suggesting that infection can be associated with prolongued hospital admission and significant morbidity. These cases suggest a need to adopt caution in the consumption of probiotic products particularly in the immunocompromised patient.
Patient’s perspective.
I noticed that the whites of my eyes had slowly got more yellow over the previous 12 months, although with all my regular checks with the diabetic nurse at the GP practice, my diabetic eye clinic appointments, but no one made any comment about the yellowness. Since receiving the courses of antibiotics in hospital and my continuing treatment, the whites of my eyes have completely recovered.
Since Christmas 2015, I had noticed that I seemed very tired and that getting around the house, the stairs and shopping seemed to be taking a lot more energy than before. I thought perhaps I was slowing down through old age.
I became more seriously ill about 4 weeks before I was admitted to the hospital. I was unable to enjoy my food and coffee, and started to feel ill after eating or drinking and not enjoying meals, as much as previously.
Two weeks before being admitted this deteriorated and I was being sick after food and could not drink coffee. I would feel really ill on one day but would feel slightly better the next day.
Because I was being sick after breakfast I was bringing up all the tablets I was taking for my diabetes, and the same applied to lunch and my evening meal. I made an appointment with the doctors' surgery to see the doctor on the Monday afternoon 21 March 2016 which was never attended due to being admitted on Friday 18 March 2016.
In the 2 weeks before being admitted I was still able to go out shopping but I was very slow in walking around having no energy to do things in the normal manner.
On the morning of Friday 18 March 2016, I woke up feeling absolutely exhausted, it was even hard to open my eyes I felt really worn out. I came down stairs from bed and sat on the settee in my normal corner and told my husband and children that I was just going to sit there and do nothing. Other than going to the toilet, I remained on the settee with my eyes closed and felt very ill and very hot although my hands and feet felt cold and could not bother to get washed and dressed. My son was keeping a close eye on me as requested by my husband, and when I tried to get up just before 2 o’clock, he noticed that I could not keep my balance and immediately rang his dad.
My husband came in and saw my condition and immediately took me into the bathroom and washed and dressed me, and rushed me into A&E. Once we were booked in at reception it was only a few minutes before I was first assessed, ready to see the triage nurse when my name was called. When I was called to go in to see the triage nurse, who took my details, did a sugar test for my diabetes, and told us to wait for a minute before she called my name and I was taken to the A&E Resuscitation.
Learning points.
We present a rare case of liver abscess caused by Lactobacillus paracasei. To our knowledge, this is the first reported case of probiotic consumption, confirmed by strain identification, as the source of a liver abscess. The infection was associated with significant morbidity and a prolonged hospital admission.
Probiotic microorganisms have long been considered innocuous, but more recent data suggest that these microbes have an important pathogenic potential. Consumers should be informed of the risk, perhaps through health warnings issued on product labelling or advertisements. There may also be a role for medical professionals in advising patients against excessive consumption, particularly those who are immunocompromised. But how much is too much?
Taking a thorough history, particularly in those who are immunocompromised is vital and should include consumption of probiotic products and their timing relative to symptoms onset.
Footnotes
Contributors: AP: completion of case report and approval of final version to be published. JU and the Microbiology department at Queen Elizabeth Hospital: contribution to case report and approval of final version to be published.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Robinson N. Probiotic industry value set to reach £29bn. Food Manufacture 2015. http://www.foodmanufacture.co.uk/Ingredients/Probiotics-on-the-rise-at-Probiota-in-Amsterdam (accessed 10 Aug 2016). [Google Scholar]
- 2.Food and Agriculture Organization of the United Nations (FAO); World Health Organization (WHO). Report of a joint FAO/WHO expert consultation on the evaluation of health and nutritional properties of probiotics in food including powder milk with live lactic acid bacteria, 2001. http://www.fao.org/3/a-a0512e.pdf (accessed 05 Jul 2016).
- 3.Food and Agriculture Organisation of the United Nations (FAO); World Health Organisation (WHO). Guidelines for the evaluation of probiotics in food. Report of a joint FAO/WHO working group on drafting guidelines for the evaluation of probiotics in food, 2002. http://www.who.int/foodsafety/fs_management/en/probiotic_guidelines.pdf (accessed 05 Jul 2016).
- 4.Hao Q, Dong BR, Wu T. Probiotics for preventing acute upper respiratory tract infections. Cochrane Database Syst Rev 2015:CD006895 10.1002/14651858.CD006895.pub3 [DOI] [PubMed] [Google Scholar]
- 5.Schwenger EM, Tejani AM, Loewen PS. Probiotics for preventing urinary tract infections in adults and children. Cochrane Database Syst Rev 2015:CD008772 10.1002/14651858.CD008772.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singh S, Stroud AM, Holubar SD, et al. . Treatment and prevention of pouchitis after ileal pouch-anal anastomosis for chronic ulcerative colitis. Cochrane Database Syst Rev 2015:CD001176 10.1002/14651858.CD001176.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kristensen NB, Bryrup T, Allin KH, et al. . Alterations in fecal microbiota composition by probiotic supplementation in healthy adults: a systematic review of randomized controlled trials. Genome Med 2016;8:52 10.1186/s13073-016-0300-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kochan P, Chmielarczyk A, Szymaniak L, et al. . Lactobacillus rhamnosus administration causes sepsis in a cardiosurgical patient--is the time right to revise probiotic safety guidelines? Clin Microbiol Infect 2011;17:1589–92. 10.1111/j.1469-0691.2011.03614.x [DOI] [PubMed] [Google Scholar]
- 9.Luong ML, Sareyyupoglu B, Nguyen MH, et al. . Lactobacillus probiotic use in cardiothoracic transplant recipients: a link to invasive Lactobacillus infection? Transpl Infect Dis 2010;12:561–4. 10.1111/j.1399-3062.2010.00580.x [DOI] [PubMed] [Google Scholar]
- 10.Zein EF, Karaa S, Chemaly A, et al. . Lactobacillus rhamnosus septicemia in a diabetic patient associated with probiotic use: a case report]. Ann Biol Clin 2008;66:195–8. [DOI] [PubMed] [Google Scholar]
- 11.Ledoux D, Labombardi VJ, Karter D. Lactobacillus acidophilus bacteraemia after use of a probiotic in a patient with AIDS and Hodgkin's disease. Int J STD AIDS 2006;17:280–2. 10.1258/095646206776253507 [DOI] [PubMed] [Google Scholar]
- 12.Land MH, Rouster-Stevens K, Woods CR, et al. . Lactobacillus sepsis associated with probiotic therapy. Pediatrics 2005;115:178–81. 10.1542/peds.2004-2137 [DOI] [PubMed] [Google Scholar]
- 13.De Groote MA, Frank DN, Dowell E, et al. . Lactobacillus rhamnosus GG bacteremia associated with probiotic use in a child with short gut syndrome. Pediatr Infect Dis J 2005;24:278–80. 10.1097/01.inf.0000154588.79356.e6 [DOI] [PubMed] [Google Scholar]
- 14.Kunz AN, Noel JM, Fairchok MP. Two cases of Lactobacillus bacteremia during probiotic treatment of short gut syndrome. J Pediatr Gastroenterol Nutr 2004;38:457–8. 10.1097/00005176-200404000-00017 [DOI] [PubMed] [Google Scholar]
- 15.Young RJ, Vanderhoof JA. Two cases of Lactobacillus bacteremia during probiotic treatment of short gut syndrome. J Pediatr Gastroenterol Nutr 2004;39:436–7. 10.1097/00005176-200410000-00027 [DOI] [PubMed] [Google Scholar]
- 16.Mackay AD, Taylor MB, Kibbler CC, et al. . Lactobacillus endocarditis caused by a probiotic organism. Clin Microbiol Infect 1999;5:290–2. 10.1111/j.1469-0691.1999.tb00144.x [DOI] [PubMed] [Google Scholar]
- 17.Muller LM, Gorter KJ, Hak E, et al. . Increased risk of common infections in patients with type 1 and type 2 diabetes mellitus. Clin Infect Dis 2005;41:281–8. 10.1086/431587 [DOI] [PubMed] [Google Scholar]
- 18.Koh GC, Peacock SJ, van der Poll T, et al. . The impact of diabetes on the pathogenesis of sepsis. Eur J Clin Microbiol Infect Dis 2012;31:379–88. 10.1007/s10096-011-1337-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harty DW, Oakey HJ, Patrikakis M, et al. . Pathogenic potential of lactobacilli. Int J Food Microbiol 1994;24:179–89. 10.1016/0168-1605(94)90117-1 [DOI] [PubMed] [Google Scholar]
- 20.Geerlings SE, Hoepelman AI. Immune dysfunction in patients with diabetes mellitus (DM). FEMS Immunol Med Microbiol 1999;26:259–65. 10.1111/j.1574-695X.1999.tb01397.x [DOI] [PubMed] [Google Scholar]
- 21.Miettinen M, Lehtonen A, Julkunen I, et al. . Lactobacilli and Streptococci activate NF-kappa B and STAT signaling pathways in human macrophages. J Immunol 2000;164:3733–40. 10.4049/jimmunol.164.7.3733 [DOI] [PubMed] [Google Scholar]
- 22.Rautio M, Jousimies-Somer H, Kauma H, et al. . Liver abscess due to a Lactobacillus rhamnosus strain indistinguishable from L. rhamnosus strain GG. Clin Infect Dis 1999;28:1159–60. 10.1086/514766 [DOI] [PubMed] [Google Scholar]
- 23.Isobe H, Fukai T, Iwamoto H, et al. . Liver abscess complicating intratumoral ethanol injection therapy for HCC. Am J Gastroenterol 1990;85:1646–8. [PubMed] [Google Scholar]
- 24.Larvol L, Monier A, Besnier P. Abcѐs hѐpatique a Lactobacillus acidophilus. Gastroenterol Clin Biol 1996;20:193–5. [PubMed] [Google Scholar]
- 25.Klein N, Schoch PE, Cunha BA. Lactobacillus acidophilus liver abscess. Infectious Diseases Newsletter 1991;10:101–2. 10.1016/0278-2316(91)90030-4 [DOI] [Google Scholar]
- 26.Nei T, Inai S, Mikami I, et al. . Descending necrotizing mediastinitis associated with Lactobacillus plantarum. BMC Infect Dis 2013;13:398 10.1186/1471-2334-13-398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sherid M, Samo S, Sulaiman S, et al. . Liver abscess and bacteremia caused by lactobacillus: role of probiotics? Case report and review of the literature. BMC Gastroenterol 2016;16:138 10.1186/s12876-016-0552-y [DOI] [PMC free article] [PubMed] [Google Scholar]


