Abstract
Background
Maternal obesity is increasingly prevalent in many westernised countries. Many studies report associations between maternal obesity and childhood wheeze or asthma but few have considered maternal obesity in relation to respiratory infections or symptoms other than wheeze during infancy. This study assesses the relationship between maternal BMI and reported wheeze, cough and respiratory infections during the first year of life.
Methods
In 2799 mother-child pairs we examined the relations between maternal pre-pregnancy BMI and pregnancy weight gain and reported offspring wheeze, prolonged cough, lower respiratory tract infection, croup and ear infection before age one year, along with reported diarrhoea or vomiting. Maternally-reported paternal BMI was included in the models as a proxy for unmeasured confounding by shared familial factors.
Results
Higher maternal BMI was associated with increased risks of offspring wheeze, prolonged cough and lower respiratory tract infection (relative risks (95% CI) per 5 kg m-2 1.09 (1.05-1.13), 1.09 (1.03-1.14) and 1.13 (1.07-1.20), respectively). These associations remained after adjusting for maternally-reported paternal BMI. No associations were found with croup, ear infection, or diarrhoea or vomiting. Pregnancy weight gain was not associated with any of the offspring symptoms or illnesses.
Discussion
Higher maternal BMI is associated with increased risk of wheeze, cough and maternally reported lower respiratory tract infection in infancy. These associations were independent of maternally-reported paternal BMI. These observations might be explained by intrauterine effects of maternal obesity upon respiratory or immune development.
Keywords: Asthma & Early Wheeze; Infections: Pneumonia, TB, Viral; Epidemiology; Pregnancy; Body mass index; Cough
Introduction
Maternal obesity is increasingly prevalent in westernised countries, including the UK, where over half of women of child-bearing age are either overweight or obese1. Obesity amongst pregnant women has significantly increased over time, with first trimester obesity more than doubling from 7.6% during the late 1980s to 15.6% two decades later2. There have been multiple reports of increased risk of wheeze3–7, and some of asthma8,9,10, in children born to obese mothers. Some studies suggest higher rates of gestational weight gain might also be associated with greater childhood wheeze risk11,12. Together these findings suggest maternal body composition during pregnancy might affect respiratory or immune development, or both. Adverse effects upon the developing immune system or upon infant lung structure and function might arise in utero due to inflammatory, metabolic or immunological consequences of maternal obesity13. Alternatively, postnatal socioeconomic and lifestyle factors shared within families might confound the relationship between maternal obesity and childhood wheeze.
We previously found greater maternal fat mass and body mass index (BMI) were associated with increased risk of the transient wheeze phenotype but not with atopy, wheeze or asthma at age 6 years5. The transient wheeze phenotype is associated with reduced lung function in early life and an increased risk of wheeze with respiratory infections during the preschool years14. The relative strength of the association with this phenotype suggests maternal obesity might be linked to childhood wheeze through adverse effects upon respiratory or immune development, leading to reduced lung function, increased susceptibility to infection, or both. An association between maternal pre-pregnancy obesity and reduced infant lung function has been reported using data from the Wheezing Illnesses Study Leidsche Rijn (WHISTLER)7. Whether maternal obesity is also associated with increased susceptibility to infections from early infancy is less clear, however10. It is not known whether maternal obesity is associated specifically with wheeze or also with other respiratory symptoms. Moreover, it is not clear whether maternal obesity is associated with increased infections in general or specifically with respiratory infections
This study examined the relationship between maternal pre-pregnancy obesity and illnesses during infancy, in particular maternal reports of symptoms and diagnoses associated with respiratory infections. The relationship between pregnancy weight gain and these outcomes was also examined. Shared familial variables might confound the associations found between maternal obesity and childhood respiratory outcomes. Potentially important familial factors include diet, physical activity or heritable propensity to obesity. Since factors associated with obesity in mothers might also be associated with obesity in fathers paternal BMI was considered a suitable proxy for unmeasured confounders influencing the relationship between maternal body composition and the risk of wheeze, cough and maternally-reported infections during infancy.
Materials and Methods
Participants
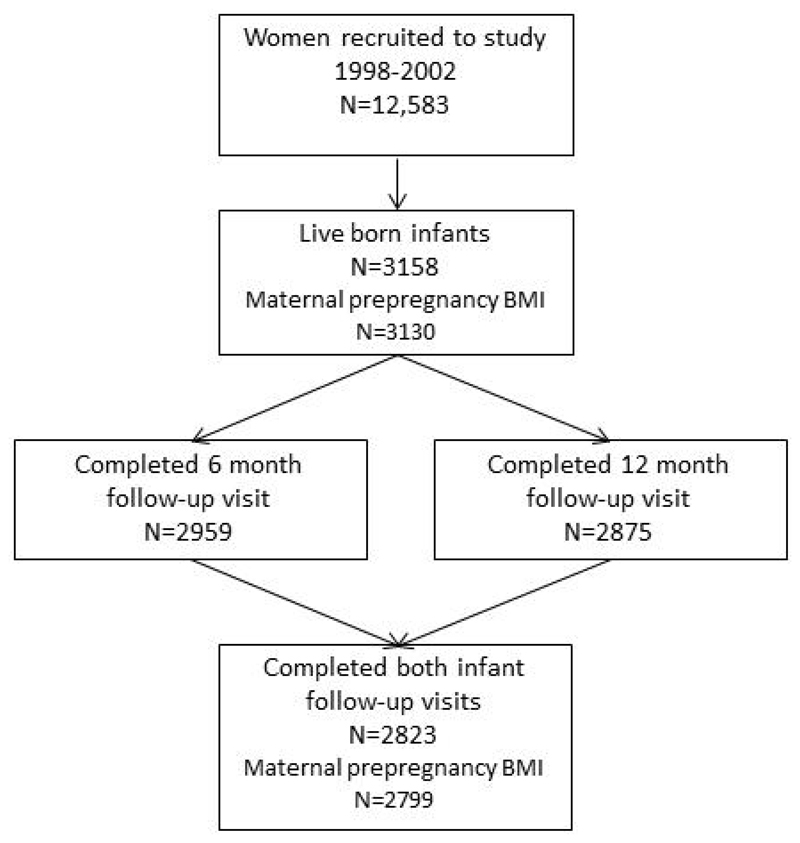
Participants were mothers, and children from the Southampton Women’s Survey cohort15. The survey recruited women aged 20-34 years during 1998-2002 when they were not pregnant. At recruitment, participating women were interviewed and anthropometric measurements were made, including height and weight. Women who subsequently became pregnant were interviewed at 11 and 34 weeks of pregnancy and childhood follow-up visits were scheduled at 6 and 12 months. Twins were excluded from the analysis and only the first child born to each woman after recruitment was followed within the study. Of 3158 live births, 2823 (89%) were seen at both 6 and 12 months of age (Figure 1). Maternal weights and heights were recorded for 2799 (99%) of the women whose children had complete follow up. These mother-child pairs formed the analytic sample. Parental consent was obtained and local ethics committee approval was granted by the Southampton and South West Hampshire Local Research Ethics Committee (LREC Numbers 276/97, 307/97, 089/99).
Figure 1.
Flow of participants through the study
Anthropometry
Maternal pre-pregnancy weight and height were measured at recruitment using portable Seca scales (Seca Ltd., Birmingham, UK) and Leicester stadiometers (Invicta Plastics Ltd., Leicester, UK). BMI was calculated as weight (kg)/(height (m))2. Paternal BMI estimates were available for 2445 (87%) of the analytic sample. Paternal BMI was calculated from paternal height and weight reported by the mother at 11 weeks of pregnancy. Child’s birthweight was measured using Seca scales (Seca Ltd., Birmingham, UK). Subscapular skinfold thicknesses were measured at birth and 6 months using Holtain skinfold calipers (Holtain Ltd., Dyfed, UK). Subscapular adiposity change conditional upon initial measurements was calculated using regression to account for exact age and for regression to the mean.
Childhood illnesses and respiratory symptoms
At the 6 and 12 month follow-up visits mothers were asked whether their child had suffered from either of the following symptoms since the last visit: ‘one or more episodes of chest wheezing/whistling’ or ‘waking at night coughing for three or more nights in a row’ (prolonged cough). Mothers were also asked if their child had suffered from ‘one or more episodes of croup or a croupy cough’, ‘bouts of vomiting or diarrhoea lasting 2 days or longer’, or ‘a doctor-diagnosed chest infection’, ‘bronchitis’, ‘bronchiolitis’, ‘pneumonia’ or ‘ear infection’. Chest infection, bronchitis, bronchiolitis and pneumonia were combined into one lower respiratory tract infection (LRTI) variable. Binary variables were created by combining responses to the 6 and 12 month questionnaires to indicate whether the child had suffered from each outcome during the first year of life.
Statistical methods
Relative risks for binary outcomes were modelled using Poisson regression with robust variance, this being an appropriate method for analysing common outcomes where odds ratios cannot be interpreted as relative risks16. Relative risks were expressed per 5 kg m-2 change in BMI. Analyses were also conducted considering maternal BMI classified according to the World Health Organisation scheme as either underweight (BMI < 18.5 kg m-2), normal weight (BMI 18.5-24.99 kg m-2), overweight (BMI 25-29.99 kg m-2) or obese (BMI ≥ 30 kg m-2); this was considered as both a categorical and continuous predictor in the models. Finally, maternal weight gain in pregnancy was classified according to Institute of Medicine categories of weight gain during pregnancy (inadequate, adequate or excessive)17, which are defined according to weight gained accounting for pre-pregnancy BMI.
Potential confounders were identified a priori and collected via nurse-administered questionnaires. Those considered initially were: maternal age, height, parity, education (this closely approximated and was collinear with socioeconomic status based upon occupation), late-pregnancy 25-hydroxyvitamin D status, smoking in pregnancy, smoking in child’s infancy, and asthma; paternal age, height, and asthma; and child’s birthweight, gestation, age at last breastfeed, exposure to smokers in the home other than the mother, and adiposity gain between birth and 6 months of age. Potential confounders were included in a directed acyclic graph (DAG) to identify the most appropriate adjustment set18; (Figure S1a) this set comprised: maternal age, education, parity, and smoking in pregnancy. To account for possible unmeasured genetic, environmental and lifestyle factors shared within families which might confound the relationship between maternal BMI and infant infections, maternally-reported paternal BMI was included in a second model as a descendant of unmeasured confounders (Figure S1b).
Our primary aim was to assess the overall impact of maternal obesity. However to assess the direct effect of maternal BMI we considered a further model adjusting for potential postnatal mediators of the effects of maternal obesity. In this model we adjusted for birthweight and adiposity gain in early infancy in addition to the adjustment set identified by the DAG andn paternal BMI. Finally, we excluded children born at less than 35 weeks’ gestation in a sensitivity analysis to address the possibility of effect modification by gestation.
Bonferroni correction was considered over-conservative since the analyses were designed a priori to test a limited number of hypotheses and not all the tests were independent19. We focused our interest on results with P-values ≤ 0.01 and considered consistency of the findings in our interpretation. Stata® 12 (Stata Corp., College Station, TX) was used for all analyses.
Results
Participants
Of the 3158 mother-child pairs in the Southampton Women’s Survey cohort, 2799 had both maternal BMI and infant 6 and 12 month follow-up data. These 2799 mother-child pairs were included in the analytic sample. Participant mothers had comparable BMIs to those not included within the analytic sample. Compared with non-included mothers, those included were of higher educational attainment, less likely to smoke in pregnancy and more likely to have a history of asthma; included infants were of greater birthweight than those not included in the analytic sample (Table 1). Sixty six children were born before 35 weeks’ gestation. The median (IQR) period between recruitment and the 11 week pregnancy interview was 1.8 (0.9-3.1) years.
Table 1.
Comparison of SWS mother-child pairs included in the analysis compared with those not included because of either incomplete follow up at 6 or 12 months or missing maternal BMI data.
| Participating mother-child pairs (n=2799) | Mother-child pairs with missing data (n=359) | P-value | ||
|---|---|---|---|---|
| Maternal characteristics | ||||
| Age at child’s birth, years (mean (SD)) | 30.7 (3.8) | 30.6 (4.0) | 0.8 | |
| Height, cm (mean (SD)) | 163.3 (6.5) | 162.7 (6.4) | 0.2 | |
| Primiparous (n (%)) | ||||
| No | 1445 (51.7) | 167 (46.7) | 0.07 | |
| Yes | 1352 (48.3) | 191 (53.4) | ||
| Qualifications (n (%)) | None | 81 (2.9) | 18 (5.0) | 0.02 |
| GCSE D-G | 252 (9.0) | 43 (12.0) | ||
| GCSE A*-C | 810 (29.0) | 101 (28.2) | ||
| A Level | 845 (30.3) | 108 (30.2) | ||
| HND | 183 (6.6) | 15 (4.2) | ||
| Degree | 620 (22.2) | 73 (20.4) | ||
| Smoked in pregnancy (n (%)) | ||||
| No | 2278 (84.5) | 227 (77.2) | 0.001 | |
| Yes | 418 (15.5) | 67 (22.8) | ||
| Maternal asthma (n (%)) | ||||
| No | 1949 (77.2) | 243 (82.9) | 0.03 | |
| Yes | 576 (22.8) | 50 (17.1) | ||
| Measured maternal BMI, kgm-2 (median, (IQR)) | 24.1 (21.9, 27.4) | 24.4 (21.7, 27.5) | 0.8 | |
| Paternal characteristics | ||||
| Age at child’s birth, years (mean (SD)) | 33.2 (5.4) | 33.0 (5.7) | 0.5 | |
| Height, cm (mean (SD)) | 179.1 (7.3) | 178.6 (6.8) | 0.2 | |
| Paternal asthma (n (%)) | ||||
| No | 2031 (81.3) | 242 (84.0) | 0.3 | |
| Yes | 466 (18.7) | 46 (16.0) | ||
| Paternal BMI, kg m-2 (median (IQR) | 25.5 (23.5, 27.8) | 25.5 (23.4, 27.6) | 0.9 | |
| Child’s characteristics | ||||
| Gender (n (%)) | ||||
| Male | 1445 (51.6) | 188 (53.1) | 0.6 | |
| Female | 1354 (48.4) | 166 (46.9) | ||
| Birth weight, kg (mean (SD)) | 3441 (547) | 3230 (676) | 0.005 | |
| Gestational age, weeks (median (IQR)) | 40.0 (39.1, 41.0) | 39.9 (38.9, 41.0) | 0.08 | |
Numbers do not always add to the full column totals due to missing data.
Binary outcomes were compared by χ2 test, categorical outcomes by a χ2 test for trend, and continuous variables using t-tests, after transformation where appropriate, or a Mann-Whitney U-test.
The median (IQR) maternal BMI measured at recruitment was 24.1 (21.9-27.4) kg m-2; 768 (27.4%) mothers were classified as overweight and 385 (13.8%) obese. Of the children with both 6 and 12 month follow-up data, 1551 (55.5%) experienced respiratory symptoms, 867 (31.1%) experienced prolonged cough and 1199 (42.9%) wheeze. Respiratory infections were reported for 1231 (44.1%) children, with 726 (26.0%) reported to have had a LRTI, 575 (20.6%) an ear infection and 282 (10.1%) a croupy cough. Vomiting or diarrhoea was reported by 1386 (49.6%).
Relationship between maternal BMI and infant respiratory symptoms
Maternal pre-pregnancy BMI was positively associated with both wheeze and prolonged cough in the first year of life (RR per 5 kg m-2, 95%CI 1.10 (1.06-1.14) and (1.10, (1.04-1.15)), both associations remained significant after adjusting for the relevant confounders (Model 1 RR 1.09, (1.05-1.13) and RR 1.09 (1.03-1.14)) and after adjusting for maternally-reported paternal BMI in addition to the DAG-identified confounders (Model 2 RR 1.09 (1.04-1.13) and RR 1.10 (1.04-1.16)) (Table 2). Similar positive associations were found in all models when children born before 35 weeks’ gestation were excluded from the analysis (RR for wheeze and cough after adjusting for DAG-identified confounders and paternal BMI 1.08 (1.04-1.13) and 1.10 (1.04-1.17)). Considering maternal BMI as a categorical variable reduced the power of the analysis but did not change the direction of effect. Children of obese mothers remained at increased risk of wheeze compared with children of mothers of a normal weight for height, ((RR 1.19, (1.06-1.34)); the test for trend across the BMI categories was significant for wheeze but not for cough (Table 3). The direction of effect was unchanged by including maternally-reported paternal BMI within the model (Table 3).
Table 2.
Relationship between maternal pre-pregnancy BMI and maternally-reported symptoms and infections during the first year of life
| Outcome | Unadjusted | Model 1 | Model 2 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RR | (95% CI) | P-value | N | RR | (95% CI) | P-value | N | RR | (95% CI) | P-value | N | |
| Wheeze | 1.10 | (1.06, 1.14) | <0.0001 | 2793 | 1.09 | (1.05, 1.13) | <0.0001 | 2682 | 1.09 | (1.04, 1.13) | 0.0001 | 2382 |
| Prolonged cough | 1.10 | (1.04, 1.15) | 0.0007 | 2792 | 1.09 | (1.03, 1.14) | 0.003 | 2681 | 1.10 | (1.04, 1.16) | 0.001 | 2381 |
| LRTI | 1.16 | (1.09,1.22) | <0.0001 | 2795 | 1.13 | (1.07, 1.20) | <0.0001 | 2684 | 1.11 | (1.04, 1.18) | 0.001 | 2384 |
| Croup | 1.01 | (0.90, 1.14) | 0.8 | 2796 | 1.01 | (0.90, 1.14) | 0.8 | 2685 | 0.99 | (0.86, 1.13) | 0.8 | 2385 |
| Ear infection | 1.04 | (0.97, 1.12) | 0.3 | 2795 | 1.04 | (0.96, 1.11) | 0.4 | 2684 | 1.03 | (0.95, 1.11) | 0.5 | 2385 |
| Diarrhoea/vomiting | 1.03 | (0.99, 1.07) | 0.1 | 2796 | 1.03 | (1.00, 1.08) | 0.08 | 2685 | 1.02 | (0.98, 1.06) | 0.3 | 2384 |
Model 1 adjusts for DAG-identified confounders (maternal age, education, parity, and smoking in pregnancy) whilst Model 2 adjusts for these confounders plus paternal BMI.
Table 3.
Relationship between maternal pre-pregnancy BMI category and maternally-reported symptoms and infections during the first year of life
| BMI category | RR (95% CI) | P-value | RR (95% CI) | P-value | RR (95% CI) | P-value | RR (95% CI) | P-value | RR (95% CI) | P-value | RR (95% CI) | P-value |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wheeze | Prolonged cough | LRTI | Croup | Ear infection | Diarrhoea / vomiting | |||||||
| Adjusting for DAG-identified confounders (Model 1 - maternal age, education, parity, smoking in pregnancy) | ||||||||||||
| Underweight | 0.70 (0.44, 1.11) | 0.1 | 1.09 (0.71, 1.68) | 0.7 | 0.71 (0.38, 1.34) | 0.3 | 1.58 (0.79, 3.15) | 0.2 | 0.83 (0.44, 1.54) | 0.5 | 1.00 (0.74, 1.35) | 0.99 |
| Normal | Reference | |||||||||||
| Overweight | 1.08 (0.98, 1.20) | 0.1 | 1.16 (1.02, 1.32) | 0.02 | 1.12 (0.96, 1.29) | 0.1 | 1.04 (0.80, 1.35) | 0.8 | 0.99 (0.83, 1.18) | 0.9 | 1.17 (1.07, 1.27) | <0.001 |
| Obese | 1.19 (1.06, 1.34) | 0.003 | 1.14 (0.97, 1.35) | 0.1 | 1.30 (1.10, 1.53) | 0.002 | 1.07 (0.77, 1.49) | 0.7 | 1.05 (0.85, 1.30) | 0.7 | 1.05(0.93, 1.18) | 0.4 |
| p-trend | 0.001 | 0.04 | 0.001 | 0.9 | 0.6 | 0.04 | ||||||
| Adjusting for DAG-identified confounders and paternal BMI (Model 2 – paternal BMI, maternal age, education, parity, smoking in pregnancy) | ||||||||||||
| Underweight | 0.71 (0.44, 1.15) | 0.2 | 0.94 (0.56, 1.55) | 0.8 | 0.79 (0.42, 1.47) | 0.5 | 1.21 (0.53, 2.77) | 0.7 | 0.77 (0.39, 1.52) | 0.5 | 0.97 (0.70, 1.33) | 0.8 |
| Normal | Reference | |||||||||||
| Overweight | 1.11 (0.99, 1.23) | 0.06 | 1.18 (1.03, 1.35) | 0.01 | 1.09 (0.94, 1.28) | 0.3 | 0.96 (0.72, 1.29) | 0.8 | 1.01 (0.84, 1.21) | 0.9 | 1.15 (1.06, 1.26) | 0.002 |
| Obese | 1.19 (1.05, 1.35) | 0.007 | 1.17 (0.98, 1.38) | 0.08 | 1.23 (1.03, 1.48) | 0.02 | 1.03 (0.72, 1.46) | 0.9 | 0.98 (0.78, 1.24) | 0.9 | 1.00(0.88, 1.14) | 0.98 |
| p-trend | 0.001 | 0.02 | 0.01 | 0.9 | 0.9 | 0.2 | ||||||
Relationship between maternal BMI and infant illnesses
Maternal pre-pregnancy BMI was positively associated with LRTI in crude analyses (RR 1.16, (1.09-1.22)) and after adjustment for both the set of DAG-identified confounders and this set plus maternally-reported paternal BMI (RR 1.13, (1.07-1.20) and 1.11, (1.04-1.18), respectively) (Table 2). Similar positive associations were found in all models when children born before 35 weeks’ gestation were excluded from the analysis (after adjusting for DAG-identified confounders and paternal BMI RR 1.11 (1.04-1.18)). There were no significant associations between maternal BMI and croup or ear infection during the first year of life and no linear association with diarrhoea or vomiting. Considering BMI as a categorical variable did not change these results; compared with children born to mothers of normal BMI the relative risk of LRTI in the first year of life for children of obese mothers was 1.30 (1.10-1.53) and there was a significant trend across BMI categories (Table 3). Maternal overweight and maternal obesity were positively associated with prolonged cough, but failed to meet significance (p≤0.01). There was an isolated association between maternal overweight but not obesity and diarrhoea or vomiting. The direction of these effects persisted after including maternally-reported paternal BMI in the model (Table 4).
Table 4.
Relationship between maternal weight gain in pregnancy and maternally-reported symptoms and infections during the first year of life adjusting for the minimum adjustment set
| Institute of Medicine Weight gain in pregnancy category | RR | (95% CI) | P-value | RR | (95% CI) | P-value | RR | (95% CI) | P-value |
|---|---|---|---|---|---|---|---|---|---|
| Wheeze | Prolonged cough | LRTI | |||||||
| Inadequate | 1.05 | (0.92, 1.19) | 0.4 | 0.93 | (0.78, 1.11) | 0.4 | 1.03 | (0.86, 1.24) | 0.7 |
| Adequate | Reference | ||||||||
| Excessive | 0.97 | (0.87, 1.09) | 0.6 | 0.99 | (0.86, 1.15) | 0.9 | 0.93 | (0.79, 1.09) | 0.3 |
| Croup | Ear infection | Vomiting or diarrhoea | |||||||
| Inadequate | 1.17 | (0.85, 1.61) | 0.3 | 0.94 | (0.74, 1.18) | 0.6 | 1.01 | (0.90, 1.14) | 0.9 |
| Adequate | Reference | ||||||||
| Excessive | 0.86 | (0.64, 1.15) | 0.3 | 1.14 | (0.95, 1.38) | 0. 2 | 1.05 | (0.96, 1.16) | 0.3 |
DAG-identified confounders maternal age, education, parity, and smoking in pregnancy
Relationship between maternal weight gain in pregnancy and infant symptoms and infections
No associations were found between maternal weight gain in pregnancy and risk of symptoms or infections during infancy in either the full cohort (Table 4) or after excluding children born before 35 weeks’ gestation (data not shown). Neither inadequate nor excessive weight gain was associated with risk significantly different from that of infants born to mothers with adequate weight gain.
Contribution of postnatal mediators
Significant positive associations were found between maternal BMI and infant wheeze, persistent cough and LRTI in an alternative model which adjusted for postnatal factors potentially mediating the effects of maternal obesity. After adjusting for the DAG-identified confounders, paternal BMI, child’s birthweight and adiposity gain during infancy the relative risks for wheeze, cough and LRTI were respectively 1.09 (1.05-1.14), 1.11 (1.05-1.18) and 1.11 (1.04-1.18).
Discussion
This study found greater maternal pre-pregnancy BMI to be associated with increased risk of maternally reported wheeze, cough and LRTI in the first year of life. These associations persisted after adjustment for maternal age, education, parity, and smoking in pregnancy, and also after adjustment for maternally-reported paternal BMI as a proxy for unmeasured shared familial confounding. The associations found between maternal BMI and maternally reported infections were minimally diminished by inclusion of potential postnatal mediators and are consistent with maternal obesity acting in utero to adversely affect respiratory or immune development, or both.
Guidelines from both the National Institute for Health and Care Excellence and the Royal College of Obstetricians and Gynaecologists recommend that women who are obese should be encouraged to lose weight before becoming pregnant in order to benefit their own health and that of their child20,21. This study extends the findings of previous studies reporting increased childhood wheeze risk in association with greater maternal BMI and provides further support for these recommendations. Of the many studies which have found associations between higher maternal BMI and increased childhood wheeze, most reported wheeze during infancy3,22, or during the preschool years4,6,23, periods when wheezing is frequently triggered by respiratory infections and may not persist. A smaller number of studies reported associations between maternal obesity and wheeze at school age9,12, or during adolescence8, when wheezing is more likely to be a feature of asthma. The mechanisms underlying these associations are unclear, although notably our previous study did not support anassociation between maternal obesity and atopy5.
Few studies have considered the relationship between maternal obesity and symptoms other than wheeze or investigated respiratory infections as an outcome. An obesogenic maternal diet, that is one high in carbohydrates but low in fruits and vegetables, has been linked with increased risk of life-threatening respiratory syncytial virus infection24. Moreover, a registry study has shown that maternal pre-pregnancy obesity is associated with a higher rate of admission for any respiratory diagnosis between birth and five years of age25. Although respiratory infections are a common cause of admission in this age range, the outcome was not restricted to infections and included non-infectious outcomes, including asthma, and diagnoses, such as hypoxemia and need for mechanical ventilation, which might arise as a consequence of significant illness of non-respiratory origin. The MoBa prospective cohort has, however, considered the risk of respiratory tract infection separately from that of wheeze, or other respiratory symptoms or diagnoses. Mothers in the MoBa study were asked to recall episodes of respiratory syncytial-virus, bronchiolitis, bronchitis or pneumonia between birth and 6 months and between 6 and 18 months. In contrast to our findings, although maternal obesity was related to maternally-reported LRTI in crude analyses, this association did not remain after adjusting for lifestyle and socioeconomic characteristics3. Differences in outcome reporting and classification, particularly with respect to age of assessment, might underlie the differences between this study and the MoBa study results. Moreover maternal anthropometry was reported rather than measured in the MoBa study which might have led to inaccuracy and weakening of any association.
There is mounting evidence to suggest that obese individuals are at increased risk of respiratory infection. During the 2009 H1N1 influenza pandemic, obese individuals were found to be more susceptible and to suffer more severe outcomes than those of normal weight26. Data linkage27 and prospective cohort studies28 have shown obese adults to be at increased risk of community-acquired pneumonia and there is also evidence that childhood obesity is associated with increased respiratory infections29. Mechanisms proposed to explain these associations include: mechanical effects of obesity, including increased risk of gastro-oesophageal reflux and aspiration, and effects of inflammatory mediators produced by adipose tissue 30. Inflammatory mechanisms might also mediate intergenerational effects of an obesogenic diet or of maternal obesity upon offspring development and later health. Alternatively, epigenetic effects, or changes to maternal or infant microbiomes might be responsible for the developmental consequences of maternal diet and body composition31,32.
In utero exposure to inflammatory states, such as chorioamnionitis and smoking, has been associated with both infant respiratory illness and childhood asthma33,34. Inflammatory mechanisms might also underlie the associations with maternal obesity since obese pregnant women have higher levels of proinflammatory cytokines in their serum and amniotic fluid than pregnant women of normal weight35,36. The Tucson Infant Immune Study reported that children of mothers in the highest third of pregnancy weight gain were at increased risk of developing asthma and had persistently elevated TNF-α in early life11, suggesting prenatal influences might, indeed, affect fetal immune development.
An alternative explanation for the associations we found could be that maternal obesity adversely affects lower airway development. Alterations in airway branching, compliance or calibre might predispose either to an increased risk of respiratory infection or to more severe and clinically apparent symptoms during episodes of respiratory infection. Developmental effects might affect the function of the smaller airways of the lower respiratory tract in particular due to the inverse relationship between airway resistance and airway radius. An effect upon the lower airway structure might occur independently from immune effects or increased vulnerability to infection per se. This is supported by our findings that other infections (croup, ear infection, and diarrhoea or vomiting) showed no associations with maternal obesity. This is also consistent with the WHISTLER study’s finding of decreased lung function in infants born to obese mothers7. Maternal obesity might be linked to structural change in the respiratory system by increased secretion of adipokines such as leptin. Leptin receptors are expressed in the lung37, leptin regulates fetal lung cell maturation38, and leptin levels have been shown to be inversely related to forced expiratory volume in children39.
This study’s strength lies in the measurement of maternal BMI in a longitudinal birth-cohort where many potential confounders are measured and maternally-reported paternal BMI serves as a proxy for unmeasured familial confounders. There was high participant retention within this study and maternal BMI did not differ significantly between participants and non-participants. The study has some limitations. Despite the high retention rate the number of women in the obese category was low which may have reduced the power to detect associations when considering BMI categories. This approach also increases the chance of type I error which might explain the isolated association between maternal overweight dn diarrhoea or vomiting, although this requires investigation in further cohorts. Infant symptoms, illnesses and infections were reported by the mother without laboratory confirmation of infections and could potentially be subject to bias. It is possible that mothers of higher BMI status are more likely to recognise4 or report respiratory infections in their children. Inclusion of a range of covariates, such as maternal education and smoking, within the adjusted models should help to reduce this potential bias, although it cannot be entirely ruled out. Paternal BMI was calculated from weight and height estimates reported by mothers questioned at 11 weeks of pregnancy. Although this is unlikely to be as accurate as measured values, many fathers are likely to have been present when the 11 week questionnaire was administered and therefore able to confirm the estimated measurements. Since maternal BMI was calculated from weight and height measured at recruitment, for some women, particularly those becoming pregnant later in follow up, these measurements could have been some years before pregnancy and potentially unrepresentative of BMI immediately prepregnancy. Potential misclassification of BMI would tend to bias the findings towards the null hypothesis. This means that the significant associations found with maternal BMI might underestimate the effect of maternal obesity. Finally, it is possible that the potentially lesser accuracy of the maternally-reported paternal BMI variable reduces its value as a proxy for unmeasured confounders.
In conclusion, we found that greater maternal BMI is associated with increased risk of cough, wheeze and lower respiratory tract infection in infancy. These associations remained after including paternal BMI in the model and the postnatal mediators birthweight and infant adiposity gain. Whilst these associations might still reflect unmeasured confounders, intrauterine effects of maternal obesity upon immune or respiratory development might also explain these observations.
Supplementary Material
Directed acyclic graph of the relationship between maternal obesity and infant infections
Directed acyclic graph of the relationship between maternal obesity and infant infections including paternal BMI as a proxy for unmeasured familial confounders
Acknowledgements
The research was supported by infrastructure provided by the NIHR Southampton Biomedical Research Centre, University of Southampton and University Hospital Southampton NHS Foundation Trust. Questionnaires and field work were conducted by the Southampton Women’s Survey Study Group.
Funding: This work within the Southampton Women’s Survey has been funded by grants from the Medical Research Council (MC_U147585827, MC_ST_U12055), British Heart Foundation (RG/07/009), Food Standards Agency (contract no N05071), Dunhill Medical Trust, the European Union's Seventh Framework Programme (FP7/2007-2013), projects EarlyNutrition and ODIN under grant agreement numbers 289346 and 613977 and Dr Katharine Pike was supported by a grant from the British Lung Foundation.
Elements of this research were presented at the ERS annual congress 2016
Footnotes
Data Availability: The study data are not freely available due to ethical restrictions. The SWS team will provide the data on request subject to appropriate approvals. For further information contact the corresponding author: Dr Katherine Pike. 1) Details of ethical restrictions behind these data: Local institutional ethics committee approval may be required. Data would be anonymised. 2) The procedure to obtain the data by the interested parties: Bona fide researchers would need to make a formal application to the SWS Steering Committee and Ethics Review Board through the cohort PI (Prof HM Inskip). The cohort investigators will provide the data to any interested party/parties on ethical approval. 3) Any other restrictions to these data: There are no further restrictions applicable to these data.
References
- 1.Moody A. Health Survey for England 2013: Chapter 10, Adult anthropometric measures, overweight and obesity. [accessed 2016 November 24]; c2014 http://content.digital.nhs.uk/catalogue/PUB16076/HSE2013-Ch10-Adult-anth-meas.pdf.
- 2.Heslehurst N, Rankin J, Wilkinson JR, Summerbell CD. A nationally representative study of maternal obesity in England, UK: trends in incidence and demographic inequalities in 619 323 births, 1989-2007. Int J Obes. 2010;34:420–428. doi: 10.1038/ijo.2009.250. [DOI] [PubMed] [Google Scholar]
- 3.Haberg SE, Stigum H, London SJ, Nystad W, Nafstad P. Maternal obesity in pregnancy and respiratory health in early childhood. Paediatr Perinat Epidemiol. 2009;23:352–362. doi: 10.1111/j.1365-3016.2009.01034.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kumar R, Story RE, Pongracic JA, Hong X, Arguelles L, Wang G, Kuptsova-Clarkson N, Pearson C, Ortiz K, Bonzagni A, et al. Maternal pre-pregnancy obesity and recurrent wheezing in early childhood. Pediatr Allergy Immunol Pulmonol. 2010;23:183–190. doi: 10.1089/ped.2010.0032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pike KC, Inskip HM, Robinson SM, Cooper C, Godfrey KM, Roberts G, Lucas JS, Southampton Women's Survey Study Group The relationship between maternal adiposity and infant weight gain, and childhood wheeze and atopy. Thorax. 2013;68:372–379. doi: 10.1136/thoraxjnl-2012-202556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leermakers ET, Sonnenschein-van der Voort AM, Gaillard R, Hofman A, de Jongste JC, Jaddoe VW, Duijts L. Maternal weight, gestational weight gain and preschool wheezing: the Generation R Study. Eur Respir J. 2013;42:1234–1243. doi: 10.1183/09031936.00148212. [DOI] [PubMed] [Google Scholar]
- 7.Eising JB, Uiterwaal CS, van der Ent CK. Maternal body mass index, neonatal lung function and respiratory symptoms in childhood. Eur Respir J. 2015;46:1342–1349. doi: 10.1183/13993003.00784-2014. [DOI] [PubMed] [Google Scholar]
- 8.Patel SP, Rodriguez A, Little MP, Elliott P, Pekkanen J, Hartikainen AL, Pouta A, Laitinen J, Harju T, Canoy D, et al. Associations between pre-pregnancy obesity and asthma symptoms in adolescents. J Epidemiol Community Health. 2012;66:809–814. doi: 10.1136/jech.2011.133777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Scholtens S, Wijga AH, Brunekreef B, Kerkhof M, Postma DS, Oldenwening M, de Jongste JC, Smit HA. Maternal overweight before pregnancy and asthma in offspring followed for 8 years. Int J Obes. 2010;34:606–613. doi: 10.1038/ijo.2009.194. [DOI] [PubMed] [Google Scholar]
- 10.Godfrey KM, Reynolds RM, Prescott SL, Nyirenda M, Jaddoe VWV, Eriksson JG, Broekman BFP. The influence of maternal obesity on the long-term health of the offspring. Lancet Diabetes Endocrinol. 2017;5:53–64. doi: 10.1016/S2213-8587(16)30107-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Halonen M, Lohman IC, Stern DA, Ellis WL, Rothers J, Wright AL. Perinatal tumor necrosis factor-alpha production, influenced by maternal pregnancy weight gain, predicts childhood asthma. Am J Respir Crit Care Med. 2013;188:35–41. doi: 10.1164/rccm.201207-1265OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harpsoe MC, Basit S, Bager P, Wohlfahrt J, Benn CS, Nohr EA, Linneberg A, Jess T. Maternal obesity, gestational weight gain, and risk of asthma and atopic disease in offspring: a study within the Danish National Birth Cohort. J Allergy Clin Immunol. 2013;131:1033–1040. doi: 10.1016/j.jaci.2012.09.008. [DOI] [PubMed] [Google Scholar]
- 13.Ramsay JE, Ferrell WR, Crawford L, Wallace AM, Greer IA, Sattar N. Maternal obesity is associated with dysregulation of metabolic, vascular, and inflammatory pathways. J Clin Endocrinol Metab. 2002;87:4231–4237. doi: 10.1210/jc.2002-020311. [DOI] [PubMed] [Google Scholar]
- 14.Martinez FD, Wright AL, Taussig LM, Holberg CJ, Halonen M, Morgan WJ. Asthma and wheezing in the first six years of life. The Group Health Medical Associates. N Engl J Med. 1995;332:133–138. doi: 10.1056/NEJM199501193320301. [DOI] [PubMed] [Google Scholar]
- 15.Inskip HM, Godfrey KM, Robinson SM, Law CM, Barker DJ, Cooper C, the Southampton Women’s Survey Study Group Cohort profile: The Southampton Women's Survey. Int J Epidemiol. 2006;35:42–48. doi: 10.1093/ije/dyi202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barros AJ, Hirakata VN. Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol. 2003;3:21. doi: 10.1186/1471-2288-3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Institute of Medicine. Weight gain during pregnancy: reexamining the guidelines. Washington DC (US): The National Academies Press; 2009. [PubMed] [Google Scholar]
- 18.Textor J, Hardt J, Knuppel S. DAGitty: a graphical tool for analyzing causal diagrams. Epidemiology. 2011;22:745. doi: 10.1097/EDE.0b013e318225c2be. [DOI] [PubMed] [Google Scholar]
- 19.Bland M. An introduction to statistics. Oxford(UK): Oxford University Press; 2000. [Google Scholar]
- 20.National Institute for Health and Care Excellence. Public health guideline [PH27] Weight management before, during and after pregnancy. [accessed 2016 November 24]; c2010 https://www.nice.org.uk/guidance/ph27/chapter/1-Recommendations.
- 21.Royal College of Obstetricians and Gynaecologists. Management of Women with Obesity in Pregnancy. [accessed 2016 November 24]; c2010. https://www.rcog.org.uk/globalassets/documents/guidelines/cmacercogjointguidelinemanagementwomenobesitypregnancya.pdf.
- 22.de Vries A, Reynolds RM, Seckl JR, van der Wal M, Bonsel GJ, Vrijkotte TG. Increased maternal BMI is associated with infant wheezing in early life: a prospective cohort study. J Dev Orig Health Dis. 2014;5:351–360. doi: 10.1017/S2040174414000312. [DOI] [PubMed] [Google Scholar]
- 23.Reichman NE, Nepomnyaschy L. Maternal pre-pregnancy obesity and diagnosis of asthma in offspring at age 3 years. Matern Child Health J. 2008;12:725–733. doi: 10.1007/s10995-007-0292-2. [DOI] [PubMed] [Google Scholar]
- 24.Ferolla FM, Hijano DR, Acosta PL, Rodriguez A, Duenas K, Sancilio A, Barboza E, Caria A, Gago GF, Almeida RE, et al. Macronutrients during pregnancy and life-threatening respiratory syncytial virus infections in children. Am J Respir Crit Care Med. 2013;187:983–990. doi: 10.1164/rccm.201301-0016OC. [DOI] [PubMed] [Google Scholar]
- 25.Parsons EC, Patel K, Tran BT, Littman AJ. Maternal pre-gravid obesity and early childhood respiratory hospitalization: a population-based case-control study. Matern Child Health J. 2013;17:1095–1102. doi: 10.1007/s10995-012-1092-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fuhrman C, Bonmarin I, Bitar D, Cardoso T, Duport N, Herida M, Isnard H, Guidet B, Mimoz O, Richard JC, et al. Adult intensive-care patients with 2009 pandemic influenza A(H1N1) infection. Epidemiol Infect. 2011;139:1202–1209. doi: 10.1017/S0950268810002414. [DOI] [PubMed] [Google Scholar]
- 27.Campitelli MA, Rosella LC, Kwong JC. The association between obesity and outpatient visits for acute respiratory infections in Ontario, Canada. Int J Obes. 2014;38:113–119. doi: 10.1038/ijo.2013.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Baik I, Curhan GC, Rimm EB, Bendich A, Willett WC, Fawzi WW. A prospective study of age and lifestyle factors in relation to community-acquired pneumonia in US men and women. Arch Intern Med. 2000;160:3082–3088. doi: 10.1001/archinte.160.20.3082. [DOI] [PubMed] [Google Scholar]
- 29.Jedrychowski W, Maugeri U, Flak E, Mroz E, Bianchi I. Predisposition to acute respiratory infections among overweight preadolescent children: an epidemiologic study in Poland. Public Health. 1998;112:189–195. doi: 10.1038/sj.ph.1900438. [DOI] [PubMed] [Google Scholar]
- 30.Falagas ME, Kompoti M. Obesity and infection. Lancet Infect Dis. 2006;6:438–446. doi: 10.1016/S1473-3099(06)70523-0. [DOI] [PubMed] [Google Scholar]
- 31.Collado MC, Isolauri E, Laitinen K, Salminen S. Effect of mother's weight on infant's microbiota acquisition, composition, and activity during early infancy: a prospective follow-up study initiated in early pregnancy. Am J Clin Nutr. 2010;92:1023–1030. doi: 10.3945/ajcn.2010.29877. [DOI] [PubMed] [Google Scholar]
- 32.Martino D, Prescott S. Epigenetics and prenatal influences on asthma and allergic airways disease. Chest. 2011;139:640–647. doi: 10.1378/chest.10-1800. [DOI] [PubMed] [Google Scholar]
- 33.Getahun D, Strickland D, Zeiger RS, Fassett MJ, Chen W, Rhoads GG, Jacobsen SJ. Effect of chorioamnionitis on early childhood asthma. Arch Pediatr Adolesc Med. 2010;164:187–192. doi: 10.1001/archpediatrics.2009.238. [DOI] [PubMed] [Google Scholar]
- 34.Haberg SE, Stigum H, Nystad W, Nafstad P. Effects of pre- and postnatal exposure to parental smoking on early childhood respiratory health. Am J Epidemiol. 2007;166:679–686. doi: 10.1093/aje/kwm134. [DOI] [PubMed] [Google Scholar]
- 35.Bugatto F, Fernandez-Deudero A, Bailen A, Fernandez-Macias R, Hervias-Vivancos B, Bartha JL. Second-trimester amniotic fluid proinflammatory cytokine levels in normal and overweight women. Obstet Gynecol. 2010;115:127–133. doi: 10.1097/AOG.0b013e3181c5367f. [DOI] [PubMed] [Google Scholar]
- 36.Hendler I, Blackwell SC, Mehta SH, Whitty JE, Russell E, Sorokin Y, Cotton DB. The levels of leptin, adiponectin, and resistin in normal weight, overweight, and obese pregnant women with and without preeclampsia. Am J Obstet Gynecol. 2005;193:979–983. doi: 10.1016/j.ajog.2005.06.041. [DOI] [PubMed] [Google Scholar]
- 37.Bruno A, Pace E, Chanez P, Gras D, Vachier I, Chiappara G, La Guardia M, Gerbino S, Profita M, Gjomarkaj M. Leptin and leptin receptor expression in asthma. J Allergy Clin Immunol. 2009;124:230–237. doi: 10.1016/j.jaci.2009.04.032. [DOI] [PubMed] [Google Scholar]
- 38.Bergen HT, Cherlet TC, Manuel P, Scott JE. Identification of leptin receptors in lung and isolated fetal type II cells. Am J Respir Cell Mol Biol. 2002;27:71–77. doi: 10.1165/ajrcmb.27.1.4540. [DOI] [PubMed] [Google Scholar]
- 49.Eising JB, Uiterwaal CS, Evelein AM, Visseren FL, van der Ent CK. Relationship between leptin and lung function in young healthy children. Eur Respir J. 2014;43:1189–1192. doi: 10.1183/09031936.00149613. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Directed acyclic graph of the relationship between maternal obesity and infant infections
Directed acyclic graph of the relationship between maternal obesity and infant infections including paternal BMI as a proxy for unmeasured familial confounders