1. Introduction
Even though the elimination of congenital syphilis has been on the maternal and child health (MCH) agenda for over a decade, elimination has not yet been achieved; what, then, are the factors currently facilitating the elimination of mother-to-child transmission (MTCT) of syphilis?
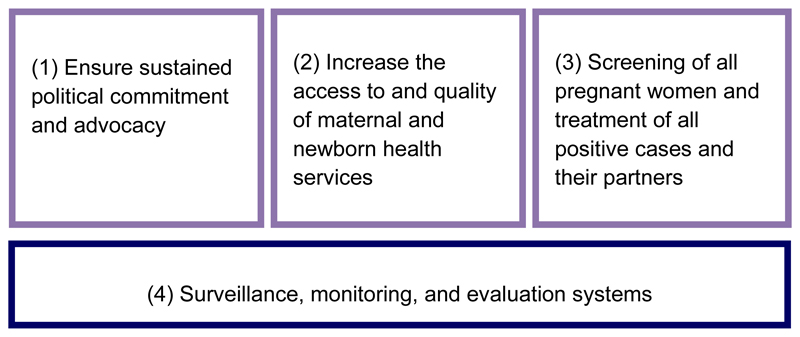
In the decade since the 2004 Bulletin of the World Health Organization special issue on maternal and congenital syphilis, with its compelling editorial emphasizing an urgent need for new approaches to address congenital syphilis prevention, substantial progress has been made on many fronts [1]. In 2007, WHO released the Global Elimination of Congenital Syphilis: Rationale and Strategy for Action [2], which was developed in consultation with experts and regional disease control officials from around the world. This pivotal strategy calls for action in four distinct “pillars”, namely: (1) ensuring sustained political commitment and advocacy; (2) increasing the access to and quality of maternal and newborn health services; (3) screening of all pregnant women and treatment of all positive cases and their partners; and (4) establishing an underlying foundation of surveillance, monitoring, and evaluation for the elimination of congenital syphilis (Figure 1) [2]. Since the launching of the strategy, many advances have now made the elimination of congenital syphilis an attainable goal for every country. The papers in this Supplement describe examples of the progress and achievements toward elimination, as well as a description of the remaining challenges.
Figure 1.
The four pillars for the elimination of congenital syphilis.
2. Taking opportunities for integration
The global MCH community has united around several new initiatives strengthening the underlying antenatal care platform (the first and second pillars of the global strategy for elimination of congenital syphilis) [3–5]. As a result, the median proportion of pregnant women receiving at least one antenatal care visit is now 90% in 58 reporting countries [6]. Further, syphilis testing in pregnancy is now part of the essential package of antenatal care services. Strategies that improve the access to and quality of antenatal care also support the elimination of congenital syphilis [7].
The strong global response to the HIV epidemic has introduced HIV screening and treatment into even the most remote areas [8]. Prevention of MTCT of HIV, initially introduced as a vertical program, has also been increasingly integrated into routine antenatal care. Therefore, in many countries and regions, services for the prevention of MTCT of HIV and syphilis are now delivered simultaneously; dual elimination of MTCT of HIV and syphilis is now a regional strategy in the Americas, Asia Pacific, Africa, and Europe, and at least 60 countries have integrated strategies for the prevention and elimination of MTCT of HIV and syphilis [9–12]. Herein, Swartzendruber et al. [13] show that such integration is associated with substantial increases in syphilis screening without adversely impacting HIV screening among pregnant women.
2.1. Simpler and cost-effective diagnostics
The development of rapid point-of-care diagnostics has made syphilis testing possible even in remote settings without access to traditional laboratories. These rapid diagnostic tests (RDTs) facilitate the provision of integrated services, such as the dual elimination of MTCT of HIV and syphilis, and improve the quality of MCH service delivery overall. In this Supplement, three new dual RDTs for HIV and syphilis are evaluated by Yin et al. [14], who found that all three have an excellent clinical performance and are simple to use. Further, through the modelling of data from Peru, Tanzania, and Zambia, Terris-Prestholt et al. [15] show that RDTs are more cost-effective in screening and treating syphilis than laboratory-based testing methods such as the rapid plasma reagin or venereal disease research laboratory test. Additionally, the potential application of electronic readers with RDTs to improve the quality of diagnosis and patient management, while also improving surveillance, is discussed by Wedderburn et al. [16].
2.2. Better data
In addition to improved diagnosis, the quality of data on syphilis in pregnancy has also improved. Since 2009, WHO has worked with countries and regions to encourage reporting on the MTCT of syphilis through the Global AIDS Response Progress Reporting System (GARPR) [17]. Syphilis seropositivity data obtained through GARPR have been used to generate global and regional estimates [18]. Herein, Ham et al. [19] suggest methods to improve the estimation process for syphilis in pregnancy by adjusting for diagnostic test type used, whereas Chen et al. [20] describe how GARPR data can be applied, using a simple online Excel tool (Microsoft, Redmond, WA, USA), to estimate the burden of maternal and congenital syphilis at a national or subnational level, as exemplified in India, Nigeria, and Zambia.
2.3. Country commitment to the elimination of MTCT of HIV and syphilis
Ultimately, it is country commitment that will make the dual elimination of MTCT of HIV and syphilis a reality. Overall, this Supplement of the International Journal of Gynecology and Obstetrics (IJGO) describes the activities of 11 countries in their scale-up of elimination of MTCT of HIV and syphilis programs. Additionally, Newman et al. [21] discuss work in six African countries to identify relevant and achievable action steps that can lead to progress toward elimination.
3. Challenges remain
Continuing challenges in the areas of advocacy, funding, and training remain to be addressed before the elimination of MTCT of syphilis and HIV can become a reality in all nations.
3.1. Advocacy at national and global level
The papers in this Supplement identify a clear need for better advocacy at the national level in order to implement integration policies for elimination of MTCT syphilis and HIV programs. In China, for example, MTCT of syphilis languished on China’s health policy agenda until the launch of their national triple strategy to eliminate the MTCT of HIV, syphilis, and hepatitis [22].
3.2. Adequate funding
Antenatal care programs implementing RDTs for syphilis have been successfully scaled up in several countries, but have not been universally effective; sufficient resources for test procurement are critical. For example, Dassah et al. [23] describe a program introducing syphilis RDTs that did not result in an overall increase in antenatal care screening, attributed, in part, to stockouts of the syphilis test kits. Further, a survey by Luu et al. [24], including 69 laboratories in 30 countries in the Americas, found that half of all laboratories serving antenatal care settings had a stockout of one or more essential syphilis testing supplies in the previous year (median duration of 30 days). Additionally, Baker et al. [25] identified shortages of tests as the main bottleneck for syphilis screening in both Tanzania and Uganda, despite a significantly higher availability for HIV tests. Thus, these authors suggest that comprehensive, rather than selective, financing and support are needed for antenatal care interventions [25].
3.3. Ongoing training
Adequate training and ongoing supervision are also crucial for the success of elimination of MTCT of syphilis programs. Balira et al. [26] found that, in Mwanza, Tanzania, only 25% of health workers in antenatal care services or maternity wards reported receiving training in the prevention of MTCT of both HIV and syphilis, which the authors felt could be improved through integrated care guidelines and training. In Guatemala, Smith et al. [27] found that providers feared delivering positive syphilis results and were more likely to report an indeterminate test result as negative. Moreover, treatment coverage of maternal syphilis must be improved for the elimination of MTCT of syphilis to succeed. Bonawitz et al. [28] found that only 12% of syphilis seropositive women received at least one dose of penicillin, despite no stockouts being reported during the time period assessed. Thus, adequate training is imperative for overcoming such barriers.
4. Country commitment to success
Several countries have demonstrated commitment toward using these tools to overcome congenital syphilis. For example, in 2015, following an estimation process of maternal and congenital syphilis at a subnational level, India (which has 29 million pregnant women annually and accounts for 20% of live births globally), launched a national strategy and operational guidelines for the elimination of congenital syphilis integrated into both the MCH and HIV screening platforms [29]. Moreover, India has introduced policy changes to ensure that syphilis and HIV testing are considered an essential component of the antenatal care package, allowed use of rapid syphilis testing in primary care facilities, and begun to address the procurement issues necessary for a massive programmatic scale-up [30]. In addition, a robust monitoring and evaluation system will be in place soon with review mechanisms at all levels, effective recording, reporting, analysis, and feedback systems that will help bridge the gaps in the program. This will facilitate India to move steadily toward the elimination of congenital syphilis and HIV by 2017.
Several countries in the Americas have also made important gains in the elimination of MTCT of HIV and syphilis. The Pan American Health Organization (PAHO) has established a regional committee for validation of elimination of MTCT of HIV and syphilis, and Cuba is the first country in the world to initiate a formal validation process for these diseases [31].
5. Conclusions
It is hoped that by highlighting the availability of new tools, improved opportunities, and examples of success, the public health community can now accelerate dual elimination of MTCT of HIV and syphilis programs. However, a commitment at multiple levels to advocate programs, provide appropriate resources and reliable procurement systems, and improve training and supervision will be needed to achieve this important goal.
Footnotes
Conflict of interest
The authors have no conflicts of interest to declare.
Contributor Information
James Kiarie, World Health Organization, Geneva, Switzerland.
Chandra K. Mishra, National Rural Health Mission, Ministry of Health and Family Welfare, Delhi, India
Marleen Temmerman, World Health Organization, Geneva, Switzerland.
References
- [1].Walker D, Walker G. Prevention of congenital syphilis--time for action. Bull World Health Organ. 2004;82(6):401. [PMC free article] [PubMed] [Google Scholar]
- [2].World Health Organization. Global Strategy for Elimination of Congenital Syphilis: Rationale and Strategy for Action. Geneva: WHO; 2007. http://www.who.int/reproductivehealth/publications/rtis/9789241595858/en/ [Google Scholar]
- [3].Global Strategy for Women and Children’s Health. http://www.everywomaneverychild.org/images/content/files/global_strategy/summary/201009_gswch_execsum_en.pdf.
- [4].World Health Organization, UNFPA, UNICEF, The World Bank. H4: Working Together to Provide Country Support for Accelerated Implementation of Reproductive, Maternal and Newborn Care. [Accessed April 26, 2015]; http://www.who.int/pmnch/about/steering_committee/091207_item1c_h4workplan_rev.pdf.
- [5].UNICEF, The Global Fund. Joint statement on a coordinated approach to Supporting Integrated Community Case Management. Published March 2014 http://www.mdghealthenvoy.org/wp-content/uploads/2014/03/Joint-Statement-Supporting-iCCM_UNICEF-RMNCH-GF_2014.pdf.
- [6].Countdown to 2015. Fulfilling the health agenda for women and children: the 2014 report. Coverage along the continuum of care. http://countdown2015mnch.org/documents/2014Report/The2014report/Part_2_(14-25)_final.pdf. [Google Scholar]
- [7].Partnership for Maternal, Newborn, and Child Health. Essential interventions, commodities, and guidelines for reproductive, maternal, newborn and child health. Geneva: PMNCH; 2011. http://www.who.int/pmnch/topics/part_publications/essential_interventions_18_01_2012.pdf?ua=1. [Google Scholar]
- [8].UNAIDS. Global plan towards the elimination of new HIV infections among children by 2015 and keeping their mothers alive. Geneva: Joint United Nations Programme on HIV/AIDS (UNAIDS); 2011. http://www.unaids.org/en/media/unaids/contentassets/documents/unaidspublication/2011/20110609_JC2137_Global-Plan-Elimination-HIV-Children_en.pdf. [Google Scholar]
- [9].Pan American Health Organization. Regional initiative for elimination of mother-to-child transmission of HIV and congenital syphilis in Latin America and the Caribbean. Washington, DC: PAHO; 2010. http://www.paho.org/derechoalaSSR/wp-content/uploads/Documentos/Regional-initiative-to-eliminate-mother-to-child-HIV-and-syphilis-transmission.pdf. [Google Scholar]
- [10].Asia-Pacific Prevention of Parent-to-Child Transmission Task Force. Elimination of parent-to-child transmission (EPTCT): women and children alive and free from HIV and syphilis. Bangkok: UNICEF East Asia and Pacific Regional Office (EAPRO); 2011. [Google Scholar]
- [11].World Health Organization. Strategic framework for the elimination of new HIV infections among children in Africa by 2015. Brazzaville, Congo: WHO Regional Office for Africa; 2013. http://www.afro.who.int/en/clusters-a-programmes/frh/making-pregnancy-safer/features/3898-strategicframework-for-the-elimination-of-new-hiv-infections-among-children-in-africa-by-2015.html. [Google Scholar]
- [12].World Health Organization. Global update on the health sector response to HIV, 2014. Geneva: WHO; 2014. http://apps.who.int/iris/bitstream/10665/128494/1/9789241507585_eng.pdf?ua=1. [Google Scholar]
- [13].Swartzendruber A, Steiner RJ, Adler M, Kamb M, Newman L. Introduction of rapid syphilis testing in antenatal care: A systematic review of the impact on HIV and syphilis testing uptake and coverage. Int J Gynecol Obstet. 2015 doi: 10.1016/j.ijgo.2015.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Yin Y-P, Ngige E, Anyaike C, Ijaodola G, Oyelade TA, Vaz RG, et al. Laboratory evaluation of three dual rapid diagnostic tests for HIV and syphilis in China and Nigeria. Int J Gynecol Obstet. 2015 doi: 10.1016/j.ijgo.2015.04.004. [DOI] [PubMed] [Google Scholar]
- [15].Terris-Prestholt F, Vickerman P, Torres-Rueda S, Santesso N, Sweeney S, Mallma P, et al. The cost-effectiveness of 10 antenatal syphilis screening and treatment approaches in Peru, Tanzania, and Zambia. Int J Gynecol Obstet. 2015 doi: 10.1016/j.ijgo.2015.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Wedderburn CJ, Murtagh M, Toskin I, Peeling RW. Using electronic readers to monitor progress toward elimination of mother-to-child transmission of HIV and syphilis: An opinion piece. Int J Gynecol Obstet. 2015 doi: 10.1016/j.ijgo.2015.04.006. [DOI] [PubMed] [Google Scholar]
- [17].UNAIDS. Global Aids Response Public Reporting 2015. Geneva: Joint United Nations Programme on HIV/AIDS (UNAIDS); 2015. http://www.unaids.org/sites/default/files/media_asset/JC2702_GARPR2015guidelines_en.pdf. [Google Scholar]
- [18].Newman L, Kamb M, Hawkes S, Gomez S, Say L, Seuc A, et al. Global estimates of syphilis in pregnancy and associated adverse outcomes: analysis of multinational antenatal surveillance data. PLoS Med. 2013;10(2):e1001396. doi: 10.1371/journal.pmed.1001396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Ham DC, Lin C, Newman L, Wijesooriya NS, Kamb M. Improving global estimates of syphilis in pregnancy by diagnostic test type: A systematic review and meta-analysis. Int J Gynecol Obstet. 2015 doi: 10.1016/j.ijgo.2015.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Chen X-S, Khaparde S, Prasad TP, Srinivas V, Anyaike C, Ijaodola G, et al. Estimating disease burden of maternal syphilis and associated adverse pregnancy outcomes in India, Nigeria, and Zambia in 2012. Int J Gynecol Obstet. 2015 doi: 10.1016/j.ijgo.2015.04.014. [DOI] [PubMed] [Google Scholar]
- [21].Newman Owiredu M, Newman L, Nzomo T, Conombo Kafando G, Sanni S, Shaffer N, et al. Elimination of mother-to-child transmission of HIV and syphilis: A dual approach in the African Region to improve quality of antenatal care and integrated disease control. Int J Gynecol Obstet. 2015 doi: 10.1016/j.ijgo.2015.04.010. [DOI] [PubMed] [Google Scholar]
- [22].Wu D, Hawkes S, Buse K. Prevention of mother-to-child transmission of syphilis and HIV in China: What drives political prioritization and what can this tell us about promoting dual elimination? Int J Gynecol Obstet. 2015 doi: 10.1016/j.ijgo.2015.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Dassah ET, Adu-Sarkodie Y, Mayaud P. Estimating the uptake of maternal syphilis screening and other antenatal interventions before and after national rollout of syphilis point-of-care testing in Ghana. Int J Gynecol Obstet. 2015 doi: 10.1016/j.ijgo.2015.04.013. [DOI] [PubMed] [Google Scholar]
- [24].Luu M, Ham DC, Kamb ML, Caffe S, Hoover KW, Perez F. Syphilis testing in antenatal care: Policies and practices among laboratories in the Americas. Int J Gynecol Obstet. 2015 doi: 10.1016/j.ijgo.2015.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Baker U, Okuga M, Waiswa P, Manzi F, Peterson S, Hanson C, et al. Bottlenecks in the implementation of essential screening tests in antenatal care: Syphilis, HIV, and anemia testing in rural Tanzania and Uganda. Int J Gynecol Obstet. 2015 doi: 10.1016/j.ijgo.2015.04.017. [DOI] [PubMed] [Google Scholar]
- [26].Balira R, Mabey D, Weiss H, Ross DA, Changalucha J, Watson-Jones D. The need for further integration of services to prevent mother-to-child transmission of HIV and syphilis in Mwanza City, Tanzania. Int J Gynecol Obstet. 2015 doi: 10.1016/j.ijgo.2015.04.016. [DOI] [PubMed] [Google Scholar]
- [27].Smith A, Sabidó M, Camey E, Batres A, Casabona J. Lessons learned from integrating simultaneous triple point-of-care screening for syphilis, hepatitis B, and HIV in prenatal services through rural outreach teams in Guatemala. Int J Gynecol Obstet. 2015 doi: 10.1016/j.ijgo.2015.04.009. [DOI] [PubMed] [Google Scholar]
- [28].Bonawitz RE, Duncan J, Hammond E, Hamomba L, Nambule J, Sambambi K, et al. Assessment of the impact of rapid syphilis tests on syphilis screening and treatment of pregnant women in Zambia. Int J Gynecol Obstet. 2015 doi: 10.1016/j.ijgo.2015.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].National Health Mission, National AIDS Coordination Organization, WHO SEARO. The national strategy and operational guidelines towards elimination of congenital syphilis. 2015 http://www.searo.who.int/india/publications/elimination_of_congenital_syphilis_part1.pdf.
- [30].National AIDS Control Organization. The national strategy and operational guidelines of congenital syphilis. New Delhi: Ministry of Health and Family Welfare; 2015. [Google Scholar]
- [31].Pan American Health Organization. Cuba advances toward validation of elimination of mother-to-child transmission of HIV and syphilis. PAHO press release; Apr 13, 2015. http://www.paho.org/hq/index.php?option=com_content&view=article&id=10628:cuba-avanza-hacia-la-validacion-de-la-eliminacion-de-la-transmision-madre-a-hijo-del-vih-y-la-sifilis-&Itemid=1926&lang=en. [Google Scholar]