Abstract
This report describes a case of labial angioleiomyoma in a 52-year-old woman. The patient had noticed a slow-growing painless isolated mass in her upper lip for 6 months. The mass was surgically excised, and pathological examination was consistent with angioleiomyoma. Surgical excision was curative, and there was no recurrence at 12-month follow-up.
Keywords: Dentistry and oral medicine; Ear, nose and throat/otolaryngology; Mouth
Background
Leiomyoma is defined by the WHO as ‘circumscribed benign, often cutaneous, tumours composed of intersecting bundles of mature smooth muscle cells’.1 The tumour exists in three microscopic patterns: the solid leiomyoma, the angioleiomyoma (vascular leiomyoma) and the epithelioid leiomyoma.2
Leiomyoma accounts for approximately 5% of all benign soft tissue tumours; it mostly arises from uterine, gastrointestinal tract and smooth muscle in skin, but is exceedingly rare in the lips or oral cavity because of the paucity of smooth muscle.3 Previous studies suggested a prevalence of 0.016%–0.06%; in a series of 7748 leiomyomas from all sites, only five cases were found in the mouth, and in a retrospective search for oral leiomyoma from 76 412 pathologic specimens, only 14 cases were identified.4 5
Angioleiomyoma is the most common histological variant affecting the oral cavity, representing 64.0%–92.3% of all variants of oral leiomyoma.4–6 It occurs over a wide age range (3.5–85 years), but the peak incidence lies between the fourth and sixth decades.4 In contrast to angioleiomyoma of all sites of the body, oral angioleiomyoma has a male predilection with an estimated male to female ratio of 1.43:15 When encountered in the mouth, angioleiomyoma most frequently affects the lips, followed by the palate, buccal mucosa and the tongue; other oral sites, including jaw bones, can be affected, although less frequently.5
Mainly, oral angioleiomyoma manifests clinically as an asymptomatic slow-growing submucosal nodule, presenting an important clinical differential diagnosis.7 Here, we describe the clinical management and the differential diagnosis of angioleiomyoma presenting as a labial mass. `
Case presentation
A-52-year-old woman presented with the complaint of a mass in her upper lip. The patient first noticed the mass 6 months earlier following what she described as a blunt hit on the face. The mass grew slowly and was asymptomatic, but the patient was concerned about the appearance of her lip. The patient reported no pain, paraesthesia or discharge. Her medical history was unremarkable, and she did not smoke tobacco or drink alcohol. Clinical examination revealed the presence of a pea-sized mass occupying the central zone of the upper lip. The mass was firm, well-circumscribed, non-tender to palpation, covered by a normal vermilion mucosa and did not blanch with pressure (figure 1). No fluctuation or bruit was present, and aspiration of the lesion was negative. The patient was afebrile, and there was no cervical lymph nodes enlargement.
Figure 1.

Clinical examination revealed the presence of a pea-sized mass occupying the central zone of the upper lip. The mass was firm, well-circumscribed, non-tender to palpation, covered by normal vermilion mucosa, and did not blanch with pressure.
Investigations
Given the clinical impression of a neoplastic process, excisional biopsy was planned and performed under local anaesthesia. Macroscopic examination revealed a small mass which was well-circumscribed, light-brown in colour, firm in consistency, oval in shape and having a smooth surface (figure 2). On microscopic examination, the mass was composed of vascular channels surrounded by fascicles of concentrically arranged spindle cells with eosinophilic cytoplasm and oval nuclei showing no evidence for malignancy, with no mitotic figures and minimal pleomorphism; immunohistochemical examination revealed that the spindle cells were strongly positive for SMA (figure 3), confirming the diagnosis of angioleiomyoma.
Figure 2.

Macroscopic examination revealed a small mass which was well-circumscribed, light-brown in colour, firm in consistency, oval in shape and having a smooth surface.
Figure 3.
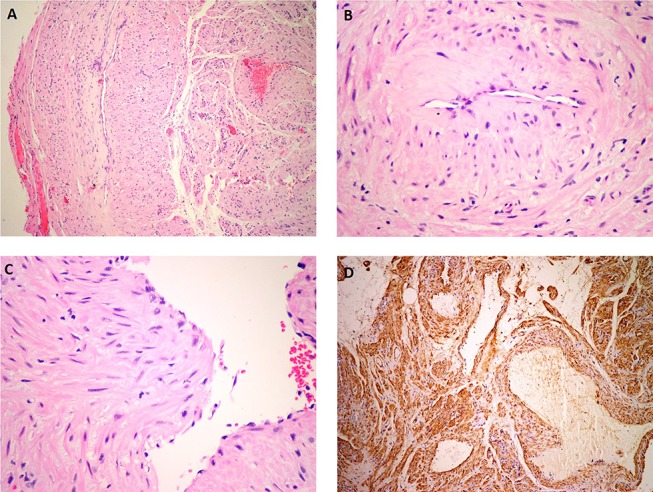
(A) Microscopic examination (H&E) revealed that the mass was well-circumscribed and composed of vascular channels. (B) The vascular channels were surrounded by fascicles of concentrically arranged spindle cells. (C) Tumour cells exhibited eosinophilic cytoplasm and oval nuclei showing no mitotic figures and a minimal degree of pleomorphism. (D) Immunohistochemical examination (SMA) revealed that the spindle cells were strongly positive for smooth muscle actin (SMA). In addition, the walls of vascular spaces were also positive for SMA.
Differential diagnosis
The clinical presentation of a slow-growing, non-ulcerated asymptomatic mass was consistent with a neoplastic process. The differential diagnosis of a slow-growing mass in the upper lip includes benign tumours arising from minor salivary glands; the most common is pleomorphic adenoma, but other less common types such as basal cell adenoma, myoepithelioma, oncocytoma and canalicular adenoma should also be considered.8 9 Other benign mesenchymal neoplasms such as lipoma, fibroma, schwannoma, neuroma, neurofibroma and fibrous histiocytoma might also affect the lips and should be considered in the differential diagnosis.10 11 Vascular malformations and neoplasms are common in the head and neck and frequently present as reddish blue submucosal lesions; however, this group of lesions was excluded from our differential diagnosis because the lesion did not blanch with pressure and needle aspiration was negative. Mucous retention and extravasation cysts are common reactive lesions in the lips and usually present as an asymptomatic submucosal bluish nodule; however, they were excluded from our differential diagnosis because needle aspiration was negative and because these lesions have a relatively rapid onset and often fluctuate in size.12 Foreign body granuloma might also occur in the lip and present similar clinical features; a history of penetrating trauma or silicone injection in the lip would suggest the diagnosis, but this was absent in our case.13 Sialoliths and phleboliths may also be considered.14 Another possible diagnosis that should not be ignored is a low-grade salivary gland malignancy such as low-grade mucoepidermoid carcinoma and low-grade adenocarcinoma which frequently presents as a slowly growing submucosal mass.15
Treatment
Complete surgical excision was performed under local anaesthesia. The mass was not adherent to the surrounding tissues and was removed in one piece (figure 4).
Figure 4.

Complete surgical excision was performed under local anaesthesia. The mass was not adherent to the surrounding tissues and was removed in one piece.
Outcome and follow-up
The patient’s postoperative recovery was uneventful, and at 12-month follow-up, there was no evidence of recurrence, and the area had healed with no complications (figure 5).
Figure 5.

At 12-month follow-up, there was no recurrence, and the area had healed without complications.
Discussion
The aetiology of leiomyoma is not entirely known, but trauma, venous stasis, hormonal changes and genetic rearrangement and translocation have been suggested.16 Our patient reported that the lesion appeared following trauma to the lip, suggesting an aetiological relationship.
The clinical presentation of oral angioleiomyoma is non-specific and might be encountered with a wide range of neoplastic and reactive oral conditions. The diagnosis of oral angioleiomyoma was, like other published cases, hardly suspected because of the rarity of the condition and the similarity with other oral lesions.7
The diagnosis of oral angioleiomyoma can only be confirmed after pathological examination which typically shows an abundance of vascular spaces surrounded by thick muscular walls composed of circumferentially arranged smooth muscle cells.5 17 18 The size of the lumena and of the muscular walls varies in different areas of tumour, and a variable mix of collagen fibres and smooth muscle fibres do exist between the vascular spaces.5 Areas of thrombosis, foci of calcification, dense hyalinisation of collagen and areas of mature fat cells are occasionally reported.7 The confirmation of smooth muscle origin can be achieved immunohistochemically with smooth muscle markers such as SMA, desmin, HHF-35, calponin and h-caldesmon.7 Our case demonstrated typical microscopic features of angioleiomyoma, and the tumour cells were strongly positive for SMA confirming the smooth muscle origin.
The pathogenesis of oral angioleiomyoma is uncertain, but it is generally believed that the tumour originates in the tunica media of blood vessels.16 Interestingly, pathological examination in our case revealed that the walls of vascular spaces stained positively with SMA, confirming that the tumour has originated from smooth muscles of blood vessels.
Most oral angioleiomyomas are, like our case, painless and characterised by a slow growth pattern; therefore, the length of time before patients seek medical attention may span months to years.5 17–21 Gueiros et al, for example, reported a case of labial angioleiomyoma with a 19-year duration.7 In very rare occasions, however, oral angioleiomyoma might present aggressively with rapid growth, pain, ulceration, paraesthesia and tooth mobility.5 22 23
Surgical excision is the treatment of choice for oral angioleiomyoma and was curative in our case. Recurrence is notably rare after complete surgical excision and, in fact, has been reported in only few cases.24 25
Importantly, there have been no reported cases of malignant transformation. Nevertheless, it is essential to distinguish leiomyomas from their malignant counterpart, the leiomyosarcoma, as both may demonstrate a similar clinical picture. Pathological features such as atypia, necrosis, pleomorphism, cellularity and mitotic activity indicate a malignant process.5
Learning points.
Angioleiomyoma is a benign smooth muscle tumour that rarely affects the oral cavity.
Angioleiomyoma of the oral cavity frequently affects the lips and present as a slow-growing, painless, firm submucosal nodule.
The clinical differential diagnosis of oral angioleiomyoma involves a wide range of reactive oral conditions and benign neoplasms.
The diagnosis of oral angioleiomyoma is confirmed by the pathological findings of variably sized vascular spaces containing concentrically arranged spindle-shaped cells that shows a strong cytoplasmic staining for smooth muscle actin.
Complete surgical excision is curative, and recurrence is extremely rare.
Footnotes
Contributors: YH treated the patient, reviewed the literature and wrote the manuscript. FS was involved in pathological diagnosis and manuscript writing. CS wrote the manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Enzinger FM, Lattes R, Torloni H. Histological typing of soft tissue tumours. Geneva: World Health Organization, 1969:30–1. [Google Scholar]
- 2.Morimoto N. Angiomyoma. A clinicopathological study. Med J Kagoshima Univ 1973;24:663–83. [Google Scholar]
- 3.Hachisuga T, Hashimoto H, Enjoji M. Angioleiomyoma. A clinicopathologic reappraisal of 562 cases. Cancer 1984;54:126–30. [DOI] [PubMed] [Google Scholar]
- 4.Baden E, Doyle JL, Lederman DA. Leiomyoma of the oral cavity: a light microscopic and immunohistochemical study with review of the literature from 1884 to 1992. Eur J Cancer B Oral Oncol 1994;30B:1–7. 10.1016/0964-1955(94)90043-4 [DOI] [PubMed] [Google Scholar]
- 5.Brooks JK, Nikitakis NG, Goodman NJ, et al. . Clinicopathologic characterization of oral angioleiomyomas. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002;94:221–7. 10.1067/moe.2002.125276 [DOI] [PubMed] [Google Scholar]
- 6.Wertheimer-Hatch L, Hatch GF, HatchB S KF, et al. . Tumors of the oral cavity and pharynx. World J Surg 2000;24:395–400. 10.1007/s002689910064 [DOI] [PubMed] [Google Scholar]
- 7.Gueiros LA, Romañach MJ, Pires-Soubhia AM, et al. . Angioleiomyoma affecting the lips: report of 3 cases and review of the literature. Med Oral Patol Oral Cir Bucal 2011;16:e482–e487. 10.4317/medoral.16.e482 [DOI] [PubMed] [Google Scholar]
- 8.Thompson LD, Bauer JL, Chiosea S, et al. . Canalicular adenoma: a clinicopathologic and immunohistochemical analysis of 67 cases with a review of the literature. Head Neck Pathol 2015;9:181–95. 10.1007/s12105-014-0560-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Daley TD. The canalicular adenoma: considerations on differential diagnosis and treatment. J Oral Maxillofac Surg 1984;42:728–30. 10.1016/0278-2391(84)90421-X [DOI] [PubMed] [Google Scholar]
- 10.Yang SW, Lin CY. Schwannoma of the upper lip: case report and literature review. Am J Otolaryngol 2003;24:351–4. 10.1016/S0196-0709(03)00065-6 [DOI] [PubMed] [Google Scholar]
- 11.Manor E, Sion-Vardy N, Joshua BZ, et al. . Oral lipoma: analysis of 58 new cases and review of the literature. Ann Diagn Pathol 2011;15:257–61. 10.1016/j.anndiagpath.2011.01.003 [DOI] [PubMed] [Google Scholar]
- 12.Sun ZJ, Zhang L, Zhang WF, et al. . Epithelioid hemangioendothelioma of the oral cavity. Oral Dis 2007;13:244–50. 10.1111/j.1601-0825.2006.01281.x [DOI] [PubMed] [Google Scholar]
- 13.Baumann LS, Halem ML. Lip silicone granulomatous foreign body reaction treated with aldara (imiquimod 5%). Dermatol Surg 2003;29:429–32. [DOI] [PubMed] [Google Scholar]
- 14.Mustapha IZ, Boucree SA. Mucocele of the upper lip: case report of an uncommon presentation and its differential diagnosis. J Can Dent Assoc 2004;70:318–21. [PubMed] [Google Scholar]
- 15.Kenny KF, Dent CD, DeBoom GW. Slowly enlarging, asymptomatic mass in the upper lip. J Am Dent Assoc 1989;118:95–7. 10.14219/jada.archive.1989.0023 [DOI] [PubMed] [Google Scholar]
- 16.Ramesh P, Annapureddy SR, Khan F, et al. . Angioleiomyoma: a clinical, pathological and radiological review. Int J Clin Pract 2004;58:587–91. 10.1111/j.1368-5031.2004.00085.x [DOI] [PubMed] [Google Scholar]
- 17.Eley KA, Alroyayamina S, Golding SJ, et al. . Angioleiomyoma of the hard palate: report of a case and review of the literature and magnetic resonance imaging findings of this rare entity. Oral Surg Oral Med Oral Pathol Oral Radiol 2012;114:e45–e49. 10.1016/j.oooo.2012.01.014 [DOI] [PubMed] [Google Scholar]
- 18.Veeresh M, Sudhakara M, Girish G, et al. . Leiomyoma: a rare tumor in the head and neck and oral cavity: report of 3 cases with review. J Oral Maxillofac Pathol 2013;17:281–7. 10.4103/0973-029X.119770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Scheper MA, Nikitakis NG, Meiller TF. A stable swelling of the hard palate. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;104:461–4. 10.1016/j.tripleo.2007.03.018 [DOI] [PubMed] [Google Scholar]
- 20.Osano H, Ioka Y, Okamoto R, et al. . Angioleiomyoma of the cheek: a case report. J Oral Sci 2015;57:63–6. 10.2334/josnusd.57.63 [DOI] [PubMed] [Google Scholar]
- 21.Arpağ OF, Damlar I, Kılıç S, et al. . Angioleiomyoma of the gingiva: a report of two cases. J Korean Assoc Oral Maxillofac Surg 2016;42:115–9. 10.5125/jkaoms.2016.42.2.115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cherrick HM, Dunlap CL, King OH. Leiomyomas of the oral cavity. review of the literature and clinicopathologic study of seven new cases. Oral Surg Oral Med Oral Pathol 1973;35:54–66. [DOI] [PubMed] [Google Scholar]
- 23.Bhatt AP, Brave VR. Angiomyoma of the mandible: a case report. J Indian Dent Assoc 1990;61:298–9. [PubMed] [Google Scholar]
- 24.Natiella JR, Neiders ME, Greene GW. Oral leiomyoma. report of six cases and a review of the literature. J Oral Pathol 1982;11:353–65. 10.1111/j.1600-0714.1982.tb00177.x [DOI] [PubMed] [Google Scholar]
- 25.Svane TJ, Smith BR, Cosentino BJ, et al. . Oral leiomyomas. review of the literature and report of a case of palatal angioleiomyoma. J Periodontol 1986;57:433–5. 10.1902/jop.1986.57.7.433 [DOI] [PubMed] [Google Scholar]


