Abstract
Study Objectives:
Deterioration in sleep quality seems to be a natural consequence of physical changes during pregnancy. It is still unclear if insomnia in pregnancy is associated with the same factors as chronic insomnia in the general population. The aim of this study was to explore the determinants of insomnia during pregnancy.
Methods:
The study included 266 women (mean age: 30.6 ± 5 years, weeks of pregnancy: 36 [interquartile range 32–38]) recruited at the Department of Gynecology and Obstetrics, Medical University of Warsaw. The assessment of variables was performed using the Athens Insomnia Scale (AIS), Beck Depression Inventory (BDI), Regestein Hyperarousal Scale (HS), Epworth Sleepiness Scale (ESS), General Practice Physical Activity Questionnaire, and a semi-structured interview about different sleep disorders.
Results:
Almost 40% of the women in our study received a diagnosis of insomnia based on AIS cutoff scores. The between-group analyses indicated that HS score, BDI score, eating at night, legs tingling, nightmares, snoring, and myoclonus differentiated the groups of individuals with insomnia from those without insomnia. Other variables were not significantly different between the groups. We divided individuals with insomnia in terms of insomnia duration: 49% developed insomnia at least 1 year before the study onset and 39.6% during pregnancy. For further analyses we used only the women in whom insomnia developed during pregnancy. Logistic regression confirmed that depressive symptoms (BDI) and eating at night were significant predictors of insomnia in pregnancy.
Conclusions:
Depressive symptoms and night eating are key factors related to insomnia developed during pregnancy.
Citation:
Wołyńczyk-Gmaj D, Różańska-Walędziak A, Ziemka S, Ufnal M, Brzezicka A, Gmaj B, Januszko P, Fudalej S, Czajkowski K, Wojnar M. Insomnia in pregnancy is associated with depressive symptoms and eating at night. J Clin Sleep Med. 2017;13(10):1171–1176.
Keywords: depression, eating at night, insomnia, pregnancy
INTRODUCTION
Sleep problems are a frequent complaint in pregnant women. The incidence of insomnia (difficulties in initiating or maintaining sleep accompanied by daytime dysfunctions) is highest in the third trimester of pregnancy.1–3 For pregnant women, chronic sleep debt is a risk factor of gestational diabetes mellitus, hypertension, and preeclampsia.4,5 Chronic sleep loss and insomnia in pregnancy increases the risk of postpartum depression.6,7 The sleep loss the mother is suffering during pregnancy is associated with fetus intrauterine growth retardation, preterm delivery, a longer duration of the delivery, and cesarean section.8–13
It is traditionally accepted that poor sleep quality and awakenings in the night are the result of pregnancy ailments such as nausea, vomiting, lower abdominal and sacral pain, nocturia, difficulty in breathing, dyspnea, or growing abdominal circumference. A growing gestational age correlates with increasing maternal weight, which may escalate the severity of unpleasant symptoms of pregnancy and thus worsen the quality of sleep. Additionally, the quality of sleep may be deteriorated by difficulty finding a comfortable sleeping position. Restless legs syndrome, with its prevalence increasing up to 23% in the third trimester of pregnancy, may also disturb sleep.1,14
BRIEF SUMMARY
Current Knowledge/Study Rationale: Insomnia in pregnancy is often explained by physiological changes in the mother's body. Other factors are underestimated and the scientific literature on the subject is sparse. The current study investigated behavioral factors (eg, depression or arousal) associated with insomnia during pregnancy.
Study Impact: Insomnia is more frequent in women in late pregnancy than in the general population, but is associated with similar factors. Based on the results of this study, we can hypothesize that analogous treatments as for chronic insomnia should be recommended.
Worsening of sleep quality in pregnancy is also related to sleep apnea. At the end of pregnancy, snoring is reported by 25% women; 11% of them suffer from sleep apnea.15 Snoring and sleep apnea are correlated with higher body mass index (BMI) before pregnancy.16
Objective polysomnography studies also confirm changes in sleep quality during pregnancy17 that worsen with its advancement.18 In the third trimester of pregnancy, the total sleep duration is shorter and there is a longer wake after sleep onset. In addition, the percentage of slow wave sleep and stage R sleep is lower, whereas the percentage of non-rapid eye movement sleep is higher than in women who are not pregnant.19 Quantitative electroencephalographic analysis during sleep showed lower power at 1.25–12.00 Hz and 13.25–16.00 Hz in the third trimester of pregnancy in comparison with women who are not pregnant. This tendency was not the result of taking naps. There are scant data available on the prevalence of sleep disorders, psychiatric comorbidities, and modifying factors such as physical activity in pregnant women in Central and Eastern Europe. Studies have shown that the prevalence of different types of insomnia in Poland is similar to that of other developed countries, but those studies did not specify a group of pregnant women.20,21 There are no reliable studies on insomnia during the pregnancy period conducted on Polish women, and it is commonly believed that poor sleep quality is simply a consequence of typical pregnancy ailments.
Establishing the factors associated with insomnia in pregnancy should help to administer appropriate treatment in order to prevent its negative consequences. Therefore, in this study we aimed to assess the prevalence of insomnia occurrence in late pregnancy and its associated factors.
METHODS
Participants
A total of 293 pregnant women with a normal course of pregnancy, who subsequently came for a routine control visit to the Department of Gynecology and Obstetrics, Medical University of Warsaw between December 2013 and July 2015, were invited to participate in the study. All subjects gave their informed written consent before completing the questionnaire. The study protocol was approved by the Bioethics Committee of the Medical University of Warsaw.
Seventeen women received a questionnaire by mistake; they were at earlier stages of pregnancy and 10 women did not complete all of the scales. The final sample included 266 women in the third trimester of pregnancy (28th–41st gestational week; mean: 35.0 ± 3.7; median: 36, interquartile range 32–38) aged 18 to 44 years (mean: 30.56 ± 4.95; median: 31, interquartile range: 27–34); 193 women (72.5%) had higher education, 60 (22.55%) had secondary education, and 13 (4.9%) had only basic professional education. Four women were pregnant with twins.
Among all participants, 196 women were married, 263 lived with family, 230 declared being professionally active, and 34 worked on night shifts. In terms of medical problems, 26 women were treated for diabetes, 14 for hypertension, 8 for asthma, and 2 for allergies.
Instruments and Procedures
We used instruments that are commonly utilized in the assessment of sleep problems, including:
Athens Insomnia Scale
The Athens Insomnia Scale (AIS) is an 8-item questionnaire based on the International Classification of Diseases, Tenth Revision criteria designed for quantitative measurement of the severity of insomnia. Each item is rated from 0 (not a problem) to 3 (a very serious problem). The total score of the scale ranges from 0 to 24. The scale was validated in Poland with 8 points as a cutoff score, and is characterized by a very good consistency (Cronbach alpha = .90) and reliability (test-retest reliability, r2 = .92).22,23 AIS is one of the most commonly used scales for diagnostic purposes as well as research on the effectiveness of insomnia treatment.24,25
Beck Depression Inventory
The Beck Depression Inventory (BDI) is a 21-item self-report scale, responses for each item are scored from 0 to 3. BDI is used to assess the severity of depressive symptoms with good internal consistency: Cronbach alpha = .85. The score ranges from 0 to 63 and the cutoff point for the Polish population is 12.26,27
Regestein Hyperarousal Scale
The Regestein Hyperarousal Scale (HS) is a 26-item scale; responses are scored from 0 to 3. HS is used to assess hyper-arousal with good consistency (Cronbach alpha = .84), the score ranges from 0 to 78 points, and is well correlated with objective measures of alertness.28 In previous studies patients with insomnia achieved high scores on the HS.29,30
Epworth Sleepiness Scale
The Epworth Sleepiness Scale (ESS) is an 8-question scale, with a range from 0 to 24 points, used to determine the level of daytime sleepiness in populations suffering from a variety of sleep disorders.31 The scale was assessed in pregnant women and is characterized by a good consistency (Cronbach alpha = .80).32
General Practice Physical Activity Questionnaire
The General Practice Physical Activity Questionnaire is a validated screening tool used to assess adult physical activity levels with a 4-level Physical Activity Index (PAI): active, moderately active, moderately inactive, and inactive.33 Among 246 women who completed the General Practice Physical Activity Questionnaire in the study sample, only 9 women (4%) met the criteria of being active, 39 women (16%) were moderately active, 43 women (17%) were moderately inactive, and 159 (63%) were inactive. The active group was too small to estimate the influence of physical activity on sleep in the study sample.
Other Procedures
In addition, a set of structured questions about different sleep disorders and symptoms was used. We asked about common symptoms of sleep disturbances, such as sleep nightmares, eating at night, snoring, tingling in the legs (a symptom of restless legs syndrome), myoclonus, duration of sleep problems, family history of insomnia, use of sleeping medication, daytime dysfunction, and sleep habits. Moreover, data on social, demographic, and current medical status were collected.
Insomnia was diagnosed according to the AIS with a cutoff score of 8 according to the Polish validation.23 Women who achieved a score of 8 points or more on the AIS were included in the insomnia group. Then, the insomnia group was divided into 2 groups: insomnia developed during pregnancy (duration of insomnia ≤ 6 months before examination) and insomnia developed before pregnancy (insomnia lasting longer than 1 year).
Statistical Analysis
The data were analyzed using SAS software (version 9.4, SAS Institute Inc., Cary, North Carolina, United States). First, we compared the groups with insomnia during pregnancy and those without insomnia in terms of age, advancement of pregnancy, weight, BMI, scores from all clinical scales (BDI, HS, ESS), different sleep disorders symptoms, coffee drinking, hypothyroidism, diabetes and hypertension, and sociodemo-graphic characteristics such as marital status, employment, education, and profession. Student t tests, Mann-Whitney U tests, or chi square tests were used depending on the quality and distribution of the data. In order to determine the most significant predictors of insomnia developed during pregnancy, statistically relevant variables (P < .05 in bivariate analyses) were entered into a logistic regression model. We calculated odds ratios (OR) and 95% confidence intervals (95% CI). Significance was set at P < .05 (two-tailed).
RESULTS
Based on structured, nonvalidated questions (yes/no) from 266 pregnant women in the third trimester of pregnancy, 224 women (84.2%) reported various sleep problems including: nighttime awakenings (n = 157; 59.0%), nonrestorative sleep (n = 66; 24.8%), problem with falling asleep (n = 62; 23.3%), early morning awakenings (n = 55; 20.7%), snoring (n = 80; 30.1%), tingling in the legs (n = 70; 26.3%), and eating at night (n = 61; 22.9%).
Based on the AIS, insomnia was diagnosed in 106 women (39.8%). In this group, 42 women reported that insomnia started during pregnancy (39.6% of insomnia group), and 52 (49%) declared insomnia longer than 1 year. Twelve remaining women could not be assigned to any of these groups, because of uncertain time of insomnia symptoms.
In the whole group 80 women reported snoring (30.1%), 70 tingling legs (26.3%), 61 eating at night (22.9%), and 54 myoclonus (20.4%).
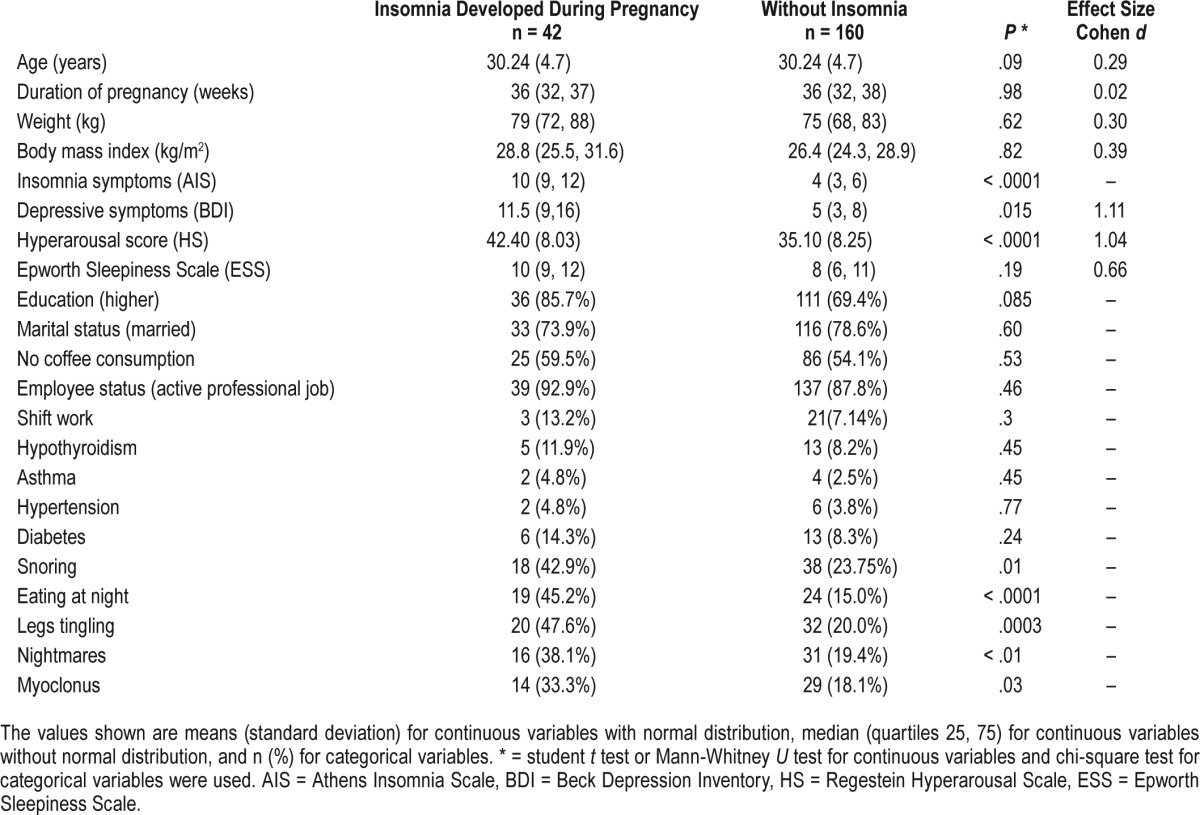
There were no significant differences between the group of pregnant women with insomnia during pregnancy (n = 42) and the group without insomnia (n = 160) with respect to age (t = −1.68, df = 200, P = 0.09), ESS score (U = 11,676.5, P = .19), education (χ2 = 4.92, df = 2, P = .085), employment (χ2 = 1.57, df = 2, P = .46), marital status (χ2 = 1.01, df = 2, P = .60), coffee drinking (χ2 = 0.40, df = 1, P = .53), hypothyroidism (well controlled; χ2 = 0.57, df = 1, P = .45), asthma (well controlled; χ2 = 0.58, df = 1, P = .45), hypertension (well controlled; χ2 = 0.085, df = 1, P = .77), diabetes (well controlled; χ2 = 1.38, df = 1, P = .24), advancement (week) of the pregnancy (U = 13,421, P = .98), body weight (U = 11,335.5, P = .62), and BMI (U = 11562.5, P = .82).
The group of women with insomnia during pregnancy (n = 42) more often woke up at night and ate (χ2 = 18.15, df = 1, P = .0001), reported more tingling in the legs (χ2 = 13.275, df = 1, P = .001), nightmares (χ2 = 6.53, df = 1, P = .01), snoring (χ2 = 6.06, df = 1, P = .01), and myoclonus (χ2 = 4.59, df = 1, P = .03); had higher depression scores (U = 11,067.5, P = .015, Cohen r = .5); and higher hyperarousal (t = 5.13, df = 200, P = .0001, Cohen r = .4) as compared to women without insomnia (Table 1).
Table 1.
Demographic and psychometric characteristics of pregnant women with insomnia that developed during pregnancy and without insomnia.
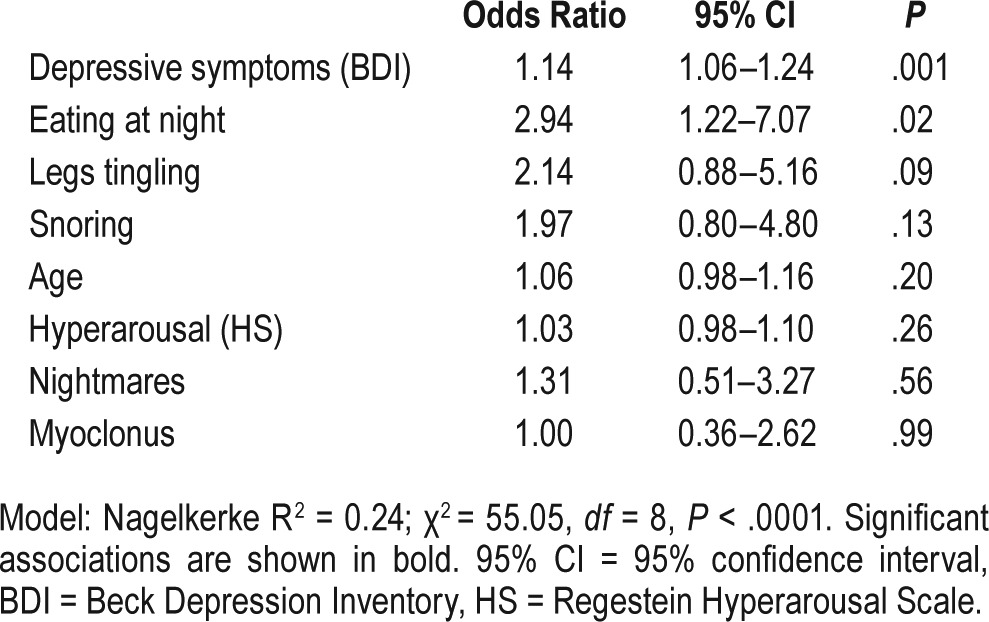
The logistic regression analysis revealed that severity of depressive symptoms (BDI score; OR = 1.14, 95% CI: 1.055–1.24, P = .001) and eating at night (OR = 2.935, 95% CI: 1.22–7.07, P = .02) were significantly associated with insomnia during pregnancy in the study group (Table 2) when controlling for all other significant factors. The model was significant (χ2 = 55.05, df = 9, P < .0001; Nagelkerke R-square = 0.24).
Table 2.
Logistic regression model for predictors of insomnia developed during pregnancy.
Comparisons of the group with insomnia developed during pregnancy and the group with insomnia before the pregnancy (lasting 1 year or longer) resulted in significant differences only with respect to nightmares (χ2 = 5.81, df = 1, P = .016) and tingling in the legs (χ2 = 5.22, df = 1, P = 0.02).
DISCUSSION
In the presented study we established the prevalence of insomnia in our sample of women in the third trimester of pregnancy. Insomnia was diagnosed in 39.8% of pregnant women participating in our study, which is a lower ratio compared to previous studies conducted on populations from different countries. In a study conducted with 2,826 Norwegian women in the 32nd week of pregnancy, primary insomnia was diagnosed in 61.5% of women according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition Text Revision criteria.6 In a Turkish questionnaire study based on answers from 486 women in the second and third trimester of pregnancy, insomnia was diagnosed in 52.2% women according to the Women's Health Initiative Insomnia Rating Scale.3 In a French study conducted with 871 women, insomnia was diagnosed in 46% of women in the first trimester of pregnancy and in 63% in the third trimester.2 The lower prevalence of insomnia in our study might result from the fact that many women complained only of selected insomnia symptoms. However, they did not reach a score of 8 on the AIS, which is the cutoff score for insomnia diagnosis according to a Polish scale validation.23 Nevertheless, our study showed that the percentage of cases with insomnia in the population of third-trimester pregnant women is much higher than in women from the Polish general population (which fluctuates around 28%).20,21
In this study snoring was reported by 30% of pregnant women, which is similar to the figures from previous studies.3,15 Almost one-fourth of subjects (22.9%) reported eating at night. To the best of our knowledge, there is no research on this phenomenon in pregnancy. The amount of women that reported eating at night was 3 times higher in women that developed insomnia in pregnancy then in pregnant women without insomnia (45% versus 15%). However, the utilized questionnaire asked only if the person got up at night and ate, and there was no thorough examination to explore the reported eating at night. We do not know whether women woke up because they felt hungry or ate because they were awake. It is widely accepted that eating at night as a sleep disorder is associated with psychiatric disorders such as depression or anxiety, as well as substance use disorders and previous eating disorders.34 Further studies in this area of pregnancy are needed.
Insomnia that developed during pregnancy represented about 40% of the total number of individuals with insomnia in our study. The group of women with insomnia that developed during pregnancy complained of waking up at night and eating, tingling in the legs, nightmares, snoring, and myoclonus, and had higher scores of depression (BDI) and hyperarousal (HS) more often than the rest of the study sample. This group did not differ from those without insomnia on many other variables, including age, ESS score, sociodemographic status, coffee intake, shift work, hypothyroidism, asthma, hypertension, or diabetes. Although it is widely accepted that sleep disorders in pregnancy are simply the result of typical problems occurring during pregnancy (such as gaining weight), we did not find an association between insomnia and body weight or the advancement of pregnancy. However, there was a narrow variance of gestational age in our study, which might account for this lack of association. Elevated scores on depressive symptoms in the group with insomnia might indicate depression, but may also suggest lower mood, which is secondary to sleep disorders. It could also indicate a common pathophysiological mechanism of both primary insomnia and depressive disorders.35
Because physically active women in our study sample were a relatively small group (4% of subjects), we could not analyze the effect of physical activity on sleep. Previous research has found that moderate physical activity may be beneficial for both the course of pregnancy and sleep quality.36
Using logistic regression we confirmed that the independent correlates of insomnia during pregnancy in our study were depressive symptoms and eating at night. The association between insomnia and depression was confirmed in several studies on groups of men and women with insomnia.37,38 Moreover, the hypothesis about a common pathophysiology of insomnia and depression may be supported by the fact that insomnia in pregnancy increases the risk of postpartum depression.12,39 In addition, we found that women with insomnia that developed during pregnancy more often suffered from nightmares and tingling in the legs in comparison with women with insomnia starting before pregnancy. Previous studies have also indicated that these symptoms are common during pregnancy, especially in its late stages.1,14,40
Our study has several limitations. The results cannot be fully generalizable because the study population included only a group of pregnant women from a single clinic, located downtown in a big city. We used only subjective self-report measures of sleep; the results would be more reliable if more objective measurement (eg, polysomnography) was used. All major sleep problems (ie, nightmares, tingling in the legs, and eating at night) were diagnosed with nonvalidated questions. We did not collect information regarding whether examined women already had children at home and how child care might affect their sleep at night. In addition, we did not directly ask about a variety of pregnancy-related complaints; our participants reported only what they perceived as disturbing for their sleep. Only 11 women with insomnia declared potential causes of sleep disorders, but as these reports were highly subjective we did not use them in further analyses.
In conclusion, our study shows that although pregnant women reported many sleep problems, insomnia during pregnancy is linked to similar factors as in other groups of people with insomnia. This suggests that treatment of insomnia in pregnancy may be the same as in chronic insomnia in other populations, especially with cognitive behavioral therapy. Also, pharmacological trials are encouraging, because recovery from insomnia is associated with a lower rate of post-partum depression.41,42 Perhaps diet modification should be implemented to prevent eating at night.
Further research on sleep in the population of pregnant women is needed because of the high prevalence of sleep problems in pregnancy and their negative effect on the health of the mother and child. It is crucial to find the actual causes of insomnia during pregnancy as it seems to be underestimated and neglected due to being commonly attributed to the physiology of pregnancy.
DISCLOSURE STATEMENT
Work for this study was performed at the Department of Psychiatry, Medical University of Warsaw, and the Department of Obstetrics and Gynecology, Medical University of Warsaw. All authors have seen and approved the manuscript. The study was financially supported by internal university funds to support research projects. The authors report no conflicts of interest.
ABBREVIATIONS
- AIS
Athens Insomnia Scale
- BDI
Beck Depression Inventory
- BMI
body mass index
- DSM
Diagnostic and Statistical Manual of Mental Disorders
- ESS
Epworth Sleepiness Scale
- HS
Regestein Hyperarousal Scale
- RLS
restless legs syndrome
- SWS
slow wave sleep
- WASO
wake after sleep onset
REFERENCES
- 1.Pien GW, Schwab RJ. Sleep disorders during pregnancy. Sleep. 2004;27(7):1405–1417. doi: 10.1093/sleep/27.7.1405. [DOI] [PubMed] [Google Scholar]
- 2.Neau JP, Texier B, Ingrand P. Sleep and vigilance disorders in pregnancy. Eur Neurol. 2009;62(1):23–29. doi: 10.1159/000215877. [DOI] [PubMed] [Google Scholar]
- 3.Kizilirmak A, Timur S, Kartal B. Insomnia in pregnancy and factors related to insomnia. ScientificWorldJournal. 2012;2012:197093. doi: 10.1100/2012/197093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haney A, Buysse DJ, Rosario BL, Chen YF, Okun ML. Sleep disturbance and cardiometabolic risk factors in early pregnancy: a preliminary study. Sleep Med. 2014;15(4):444–450. doi: 10.1016/j.sleep.2014.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hayase M, Shimada M, Seki H. Sleep quality and stress in women with pregnancy-induced hypertension and gestational diabetes mellitus. Women Birth. 2014;27(3):190–195. doi: 10.1016/j.wombi.2014.04.002. [DOI] [PubMed] [Google Scholar]
- 6.Dørheim SK, Bjorvatn B, Eberhard-Gran M. Insomnia and depressive symptoms in late pregnancy: a population-based study. Behav Sleep Med. 2012;10(3):152–166. doi: 10.1080/15402002.2012.660588. [DOI] [PubMed] [Google Scholar]
- 7.Park EM, Meltzer-Brody S, Stickgold R. Poor sleep maintenance and subjective sleep quality are associated with postpartum maternal depression symptom severity. Arch Wom Ment Health. 2013;16(6):539–547. doi: 10.1007/s00737-013-0356-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Palagini L, Gemignani A, Banti S, et al. Chronic sleep loss during pregnancy as a determinant stress: impact on pregnancy outcome. Sleep Med. 2014;15(8):853–859. doi: 10.1016/j.sleep.2014.02.013. [DOI] [PubMed] [Google Scholar]
- 9.Strange LB, Parker KP, Moore ML, Strickland OL, Bliwise DL. Disturbed sleep and preterm birth: a potential relationship? Clin Exp Obstet Gynecol. 2009;36(3):166–168. [PubMed] [Google Scholar]
- 10.Abeysena C, Jayawardana P, Seneviratne Rde A. Effect of psychosocial stress and physical activity on low birthweight: a cohort study. J Obstet Gynaecol Res. 2010;36(2):296–303. doi: 10.1111/j.1447-0756.2009.01155.x. [DOI] [PubMed] [Google Scholar]
- 11.Micheli K, Komninos I, Bagkeris E, et al. Sleep patterns in late pregnancy and risk of preterm birth and fetal growth restriction. Epidemiology. 2011;22(5):738–744. doi: 10.1097/EDE.0b013e31822546fd. [DOI] [PubMed] [Google Scholar]
- 12.Okun ML, Hanusa BH, Hall M, Wisner KL. Sleep complaints in late pregnancy and the recurrence of postpartum depression. Behav Sleep Med. 2009;7(2):106–117. doi: 10.1080/15402000902762394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Okun ML, Luther JF, Wisniewski SR. Disturbed sleep and inflammatory cytokines in depressed and nondepressed pregnant women: an exploratory analysis of pregnancy outcomes. Psychosom Med. 2013;75(7):670–681. doi: 10.1097/PSY.0b013e31829cc3e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee KA, Zaffke ME, Baratte-Beebe K. Restless legs syndrome and sleep disturbance during pregnancy: the role of folate and iron. J Womens Health Gend Based Med. 2001;10(4):335–341. doi: 10.1089/152460901750269652. [DOI] [PubMed] [Google Scholar]
- 15.Franklin KA, Holmgren PA, Jönsson F, Poromaa N, Stenlund H, Svanborg E. Snoring, pregnancy-induced hypertension, and growth retardation of the fetus. Chest. 2000;117(1):137–141. doi: 10.1378/chest.117.1.137. [DOI] [PubMed] [Google Scholar]
- 16.Sarberg M, Svanborg E, Wiréhn AB, Josefsson A. Snoring during pregnancy and its relation to sleepiness and pregnancy outcome - a prospective study. BMC Pregnancy Childbirth. 2014;14:15. doi: 10.1186/1471-2393-14-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brunner DP, Münch M, Biedermann K, Huch R, Huch A, Borbély AA. Changes in sleep and sleep electroencephalogram during pregnancy. Sleep. 1994;17(7):576–582. doi: 10.1093/sleep/17.7.576. [DOI] [PubMed] [Google Scholar]
- 18.Orff HJ, Meliska CJ, Lopez A, Martinez F, Sorenson D, Parry BL. Polysomnographic evaluation of sleep quality and quantitative variables in women as a function of mood, reproductive status, and age. Dialogues Clin Neurosci. 2012;14(4):413–424. doi: 10.31887/DCNS.2012.14.4/hjorff. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wilson DL, Barnes M, Ellett L, Permezel M, Jackson M, Crowe SF. Decreased sleep efficiency, increased wake after sleep onset and increased cortical arousals in late pregnancy. Aust N Z J Obstet Gynaecol. 2011;51(1):38–46. doi: 10.1111/j.1479-828X.2010.01252.x. [DOI] [PubMed] [Google Scholar]
- 20.Szelenberger W, Skalski M. Epidemiologia zaburzeń snu w Polsce. Doniesienie wstępne. In: Nowicki Z, Szelenberger W, editors. Zaburzenia snu. Diagnostyka i leczenie. Wybrane zagadnienia. Kraków: Biblioteka Psychiatrii Polskiej; 1999. pp. 57–63. [Google Scholar]
- 21.Kiejna A, Wojtyniak B, Rymaszewska J, Stokwiszewski J. Prevalence of insomnia in Poland — results of the National Health Interview Survey. Acta Neuropsychiatr. 2004;16(2):124–129. doi: 10.1034/j.1601-5215.2003.00011.x. [DOI] [PubMed] [Google Scholar]
- 22.Soldatos CR, Dikeos DG, Paparrigopoulos TJ. The diagnostic validity of the Athens Insomnia Scale. J Psychosom Res. 2003;55(3):263–267. doi: 10.1016/s0022-3999(02)00604-9. [DOI] [PubMed] [Google Scholar]
- 23.Fornal-Pawłowsk M, Wołyńczyk-Gmaj D, Szelenberger W. Validation of the Polish version of the Athens Insomnia Scale. Psychiatr Pol. 2011;45(2):211–221. [PubMed] [Google Scholar]
- 24.Morin CM. Measuring outcomes in randomized clinical trials of insomnia treatments. Sleep Med Rev. 2003;7(3):263–279. doi: 10.1053/smrv.2002.0274. [DOI] [PubMed] [Google Scholar]
- 25.Buysse DJ, Ancoli-Israel S, Edinger JD, Lichstein KL, Morin CM. Recommendations for standard research assessment of insomnia. Sleep. 2006;29(9):1155–1173. doi: 10.1093/sleep/29.9.1155. [DOI] [PubMed] [Google Scholar]
- 26.Beck AT, Ward CH, Mendelson M, Mock JE, Erbaugh JK. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 27.Parnowski T, Jernajczyk W. Inwentarz Depresji Becka w ocenie nastroju osób zdrowych i chorych na choroby afektywne. Psychiatr Pol. 1977;11(4):417–421. [PubMed] [Google Scholar]
- 28.Regestein QR, Dambrosia J, Hallet M, Murawski B, Paine M. Daytime alertness in patients with primary insomnia. Am J Psychiatry. 1993;150(10):1529–1534. doi: 10.1176/ajp.150.10.1529. [DOI] [PubMed] [Google Scholar]
- 29.Szelenberger W, Niemcewicz S. Severity of insomnia correlates with cognitive impairment. Acta Neurobiol Exp (Wars) 2000;60(3):373. doi: 10.55782/ane-2000-1356. [DOI] [PubMed] [Google Scholar]
- 30.Wołyńczyk-Gmaj D, Szelenberger W. Walking EEG in primary insomnia. Acta Neurobiol Exp (Wars) 2011;71(3):387–392. doi: 10.55782/ane-2011-1860. [DOI] [PubMed] [Google Scholar]
- 31.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–541. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 32.Sarberg M, Bladh M, Josefsson A, Svanborg E. Sleepiness and sleep-disordered breathing during pregnancy. Sleep Breath. 2016;20(4):1231–1237. doi: 10.1007/s11325-016-1345-9. [DOI] [PubMed] [Google Scholar]
- 33.Department of Health. The General Practice Physical Activity Questionnaire (GPPAQ) London, UK: Department of Health; 2006. [Google Scholar]
- 34.Vander Wal JS. Night eating syndrome: a critical review of the literature. Clin Psychol Rev. 2012;32(1):49–59. doi: 10.1016/j.cpr.2011.11.001. [DOI] [PubMed] [Google Scholar]
- 35.Richardson GS, Roth T. Future directions in the management of insomnia. J Clin Psychiatry. 2001;62(Suppl 10):39–45. [PubMed] [Google Scholar]
- 36.Chennaoui M, Arnal PJ, Sauvet F, Léger D. Sleep and exercise: a reciprocal issue? Sleep Med Rev. 2015;20:59–72. doi: 10.1016/j.smrv.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 37.Perlis ML, Kehr EL, Smith MT, Andrews PJ, Orff H, Giles DE. Temporal and stagewise distribution of high frequency EEG activity in patients with primary and secondary insomnia and in good sleeper controls. J Sleep Res. 2001;10(2):93–104. doi: 10.1046/j.1365-2869.2001.00247.x. [DOI] [PubMed] [Google Scholar]
- 38.Vandeputte M, de Weerd A. Sleep disorders and depressive feelings: a global survey with the Beck depression scale. Sleep Med. 2003;4(4):343–345. doi: 10.1016/s1389-9457(03)00059-5. [DOI] [PubMed] [Google Scholar]
- 39.Dørheim SK, Bjorvatn B, Eberhard-Gran M. Can insomnia in pregnancy predict postpartum depression? A longitudinal, population-based study. PLoS One. 2014;9(4):e94674. doi: 10.1371/journal.pone.0094674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tomfohr-Madsen LM, Clayborne ZM, Rouleau CR, Campbell TS. Sleeping for two: an open-pilot study of cognitive behavioral therapy for insomnia in pregnancy. Behav Sleep Med. 2017;15(5):377–393. doi: 10.1080/15402002.2016.1141769. [DOI] [PubMed] [Google Scholar]
- 41.Khazaie H, Ghadami MR, Knight DC, Emamian F, Tahmasian M. Insomnia treatment in the third trimester of pregnancy reduces postpartum depression symptoms: a randomized clinical trial. Psychiatry Res. 2013;210(3):901–905. doi: 10.1016/j.psychres.2013.08.017. [DOI] [PubMed] [Google Scholar]


