Abstract
Study Objectives:
To describe a sustainable program of teaching and implementing quality improvement (QI) in a 12-month sleep medicine fellowship.
Methods:
We created a QI curriculum based on Accreditation Council for Graduate Medical Education (ACGME) and American Board of Medical Specialty (ABMS) Part IV Maintenance of Certification (MOC) requirements for QI. Two program faculty with prior QI training volunteered to mentor fellows. Our institution's central QI office houses QI experts who teach QI across the health system. One of these experts, referred to as the “QI consultant,” helped us adapt QI teaching materials to include 4 online modules and 5 group sessions. Fellows worked in teams to complete 2 data-guided QI cycles.
Results:
The curriculum required 29 hours for fellows, 18 hours for faculty, and 55 hours for the QI consultant; now that teaching materials have been created, the QI consultant's involvement will decrease over time. Post-curriculum surveys showed that fellows' knowledge of QI concepts increased, as did their confidence performing QI activities. Fellows' QI projects objectively improved timeliness and quality of care for patients. Sleep medicine fellows and QI faculty mentors evaluated the curriculum positively. The curriculum met ACGME requirements for QI, and fellows and mentoring faculty received ABMS Part IV MOC credit upon completion of the curriculum.
Conclusions:
A QI curriculum can successfully be implemented into a 12-month sleep medicine fellowship to increase sleep medicine fellows' QI knowledge and confidence, meet ACGME and MOC requirements, and contribute to care of patients with sleep disorders.
Citation:
Shelgikar AV, Priddy C, Van Harrison R. Meeting ACGME and ABMS quality improvement requirements in a sleep medicine fellowship program. J Clin Sleep Med. 2017;13(10):1177–1183.
Keywords: education, fellowship, maintenance of certification, quality improvement, sleep disorders
INTRODUCTION
The Accreditation Council for Graduate Medical Education (ACGME) 1-year common program requirements1 include the following:
“Fellows are expected to develop skills and habits to be able to…systematically analyze practice using quality improvement methods, and implement changes with the goal of practice improvement” (IV.A.2.c)
“Fellows must demonstrate the ability to analyze the care they provide, understand their roles within health care teams, and play an active role in system improvement processes. Graduating fellows will apply these skills to critique their future unsupervised practice and effect quality improvement measures.” (VI.A.1.)
“Fellows must receive training and experience in quality improvement processes, including an understanding of health care disparities. (VI.A.1.b).(1).(a)
“Fellows must have the opportunity to participate in interprofessional quality improvement activities.” (VI.A.1.b).(3).(a)
These requirements inspired our discussion about what types of systems-based improvement experiences our fellows need during their training year. We recognized that performance improvement (PI) and quality improvement (QI) both pertain to systems-level improvement, with the main difference being that PI emphasizes human performance whereas QI highlights processes.2 QI “consists of systematic and continuous actions that lead to measurable improvement in health care services and the health status of targeted patient groups.”3 QI projects are team-based endeavors in which participants collect data to understand the current state of a process, define the gap between the process' current state and goal state, develop and implement a countermeasure to improve the process, then collect data to determine if the countermeasure achieved the goal state of the process.
BRIEF SUMMARY
Current Knowledge/Study Rationale: Continuous quality improvement (QI) in the clinical setting is a requirement for both physicians in a fellowship training program and those in practice.
Study Impact: This article describes the successful implementation of a QI curriculum into a sleep medicine fellowship. The curriculum was designed to meet QI requirements of both the Accreditation Council for Graduate Medical Education and the Multi-Specialty MOC Portfolio Program of the American Board of Medical Specialties. This article provides tips for other sleep medicine fellowship programs who seek to incorporate QI activities for their fellows.
Given that the ACGME requirements specify that fellows must have QI training and experience, we set out to create a thorough QI curriculum for our sleep medicine fellows. We wanted to ensure that our sleep medicine fellowship program teaches fellows foundational QI concepts and provides robust experience in applying this knowledge to real-life scenarios. Literature review showed that many scholarly articles detail QI curricula for residency programs,4–8 but fewer describe QI curricula in fellowship programs.9–11 Moreover, scant guidance is available on development and implementation of a QI curriculum into a single-year graduate medical education training program.
We thus set out to develop, implement, and evaluate a QI curriculum in our sleep medicine fellowship program. We recognized that our QI curriculum needs to:
Meet ACGME requirements for QI
Be practical within the 12-month fellowship program
Include QI projects that are fellow-driven
Be deliverable year after year with successive cohorts of fellows
This article describes our sleep medicine fellowship QI curriculum, which was specifically designed to encompass each of these 4 features.
METHODS
Curriculum Design
Our first step was to describe ACGME requirements for QI to our program faculty and sleep center leadership, to provide context and garner support for this new curriculum. We identified the following resources needed to create and implement a QI curriculum: time to design the curriculum; expert input to guide the content of the curriculum; time for participants (fellows and faculty mentors) to complete the curriculum; space to hold the group sessions; and time for fellows to present their projects and results to other members of our sleep disorders center.
We next reached out to the QI infrastructure within the University of Michigan Health System. Our institution's central QI office—the Performance Improvement Unit within the Quality Department—houses full-time QI experts who teach QI concepts to personnel all across our health system. One of these institutional QI teachers, referred to as the “QI consultant,” helped us adapt institutional QI teaching materials to fit the needs of our sleep medicine fellowship program.
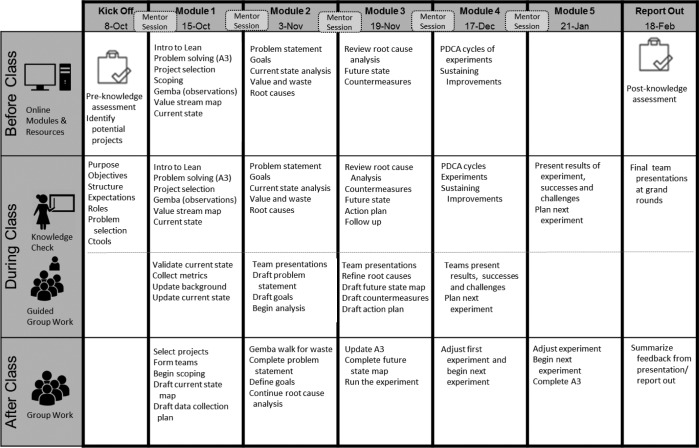
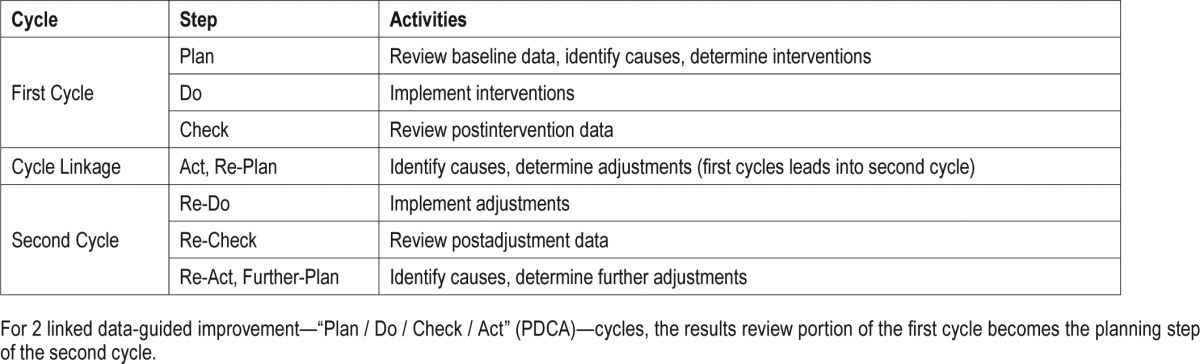
The Michigan Quality System uses Lean Thinking,12 a systematic process for continuous QI. Lean Thinking stems from the Toyota Production System13 and has been assimilated in many industries, including health care.14 A data-guided improvement cycle—“Plan / Do / Check / Act” (PDCA)—represents a basic component of QI curricula taught within our institution and elsewhere. Most project-based QI training in residency programs involves only 1 PDCA improvement cycle. We wanted our QI curriculum to provide our fellows with experience that most mirrors QI in clinical practice. We thus incorporated 2 linked PDCA cycles into our fellowship QI curriculum. For 2 linked PDCA improvement cycles, the review of results from the first PDCA cycle becomes the planning for the following cycle (Table 1).
Table 1.
Two linked cycles of data-guided quality improvement effort.
Sleep medicine fellows are held to ACGME requirements for QI during their training year. In addition, fellows who are board eligible or board certified in their primary discipline(s) must meet requirements to maintain that certification. We thus designed our QI curriculum to meet ACGME and American Board of Medical Specialties (ABMS) Maintenance of Certification (MOC) requirements for QI. The Multi-Specialty MOC Portfolio Program of the ABMS15 has approved our institution to award Part IV (practice assessment and improvement) credit to physicians who perform 2 linked cycles of data-guided QI effort. Our health care system's Quality Department has a MOC for QI Program that provides local approval and awarding of Part IV MOC. That program facilitated our ability to provide fellows and faculty QI mentors in multiple specialties the opportunity to receive MOC credit for their QI activities. This also allowed our QI curriculum to meet the MOC needs of the supervising faculty who mentored fellows' QI projects.16
We designed the curriculum to span approximately 6 months. It started nearly one-third of the way into the fellowship so that fellows would be familiar with processes in our sleep disorders center and health system. The QI consultant helped us adapt institutional materials to teach our sleep medicine fellows (1) a basic overview of QI and Lean Thinking and (2) how QI concepts directly apply to clinical care processes. The QI curriculum was based a conceptual framework of social experiential learning,17 which emphasizes the importance of teamwork in a familiar environment; fellows thus worked in groups, under guidance of a faculty mentor, and developed QI projects directly related to their clinical responsibilities.
We designed our QI curriculum using a flipped classroom approach,18,19 in which the conventional order of events is “flipped” and homework is to be completed before (not after) the classroom session. Using a flipped classroom method for our QI curriculum liberated time constraints with scheduling in-class sessions. Also, fellows tend to be self-directed learners who often engage in independent reading, so assignment of “homework” was acceptable for the fellows. Foundational QI concepts were taught via online modules, which fellows completed before each class session. These modules were interspersed throughout the curriculum and contained short instructional readings and videos. “Flipping” the didactic presentation of material gave flexibility for fellows to complete the modules.
The flipped classroom approach also allowed group time to be “hands-on” application of the didactic material. Scheduled group time corresponded to an online module and related interval of each QI project. Figure 1 shows the detailed course map, which shows the longitudinal QI curriculum including online modules, group sessions, and topics covered. Because our sleep medicine training program is a single-year fellowship, all participants are first-year sleep medicine fellows with similar schedules. We were thus able to carve out dedicated group time and held the group sessions in a conference room within our sleep disorders center.
Figure 1. Course map for the sleep medicine fellowship program quality improvement curriculum.
Gemba = location where the process/work is happening, PDCA = “Plan / Do / Check / Act”, QI = quality improvement, SIPOC = suppliers, inputs, process, outputs, and customers.
Once the curriculum was established, we met again with fellowship program faculty to request faculty to mentor fellows' QI projects. Two program faculty, both of whom had previous QI training through the institution, volunteered to mentor fellows throughout the QI curriculum. Both faculty members were shown the course map at the start and agreed to participate throughout the entire curriculum.
QI Projects
Fellows identified problems in patient care that were personally and clinically meaningful, within a reasonable scope of their direct influence, and for which 2 PDCA improvement cycles could be completed within 6 months. Fellows and faculty mentors refined these ideas into 2 projects with teams of 3 or 4 fellows working on each project. Both projects selected by the fellows involved aspects of patient care related to polysomnography; one project pertained to electrocardiograms (EKGs) and the other to inpatient sleep studies. Fellows and faculty mentors collaboratively refined the project's scope to address at least 1 of the 6 Institute of Medicine Quality Dimensions (safety, equity, timeliness, effectiveness, efficiency, patient-centeredness).20
Evaluation
Curricular planning included estimating, monitoring, and modifying program elements to minimize participants' time involvement and maximize individual fellows' knowledge and confidence, quality of the QI projects performed, and of the overall curriculum. Assessment measures included a post-curriculum test to self-assess knowledge of foundational QI concepts and fellows' self-reported confidence related to application of QI concepts.
Ethical Approval
The routine evaluation and improvement of existing educational and clinical activities using known methods is not considered research on human subjects that is regulated by an Institutional Review Board. However, the clinical leadership of our sleep disorders center approved and oversaw the educational and clinical improvement initiatives involved in the QI curriculum for sleep medicine fellows.
RESULTS
Project Participation
All 7 fellows completed the curriculum, including performing a QI project involving two PDCA cycles of data-guided improvement.
Time Involved of Various Participants
Table 2 lists the responsibilities and approximate time commitments of fellows, local faculty mentors, and the QI consultant. Overall engagement was 29 hours for fellows, 18 hours for faculty mentors, and 55 hours for the QI consultant.
Table 2.
Time commitments for participants in the sleep medicine fellowship quality improvement curriculum.
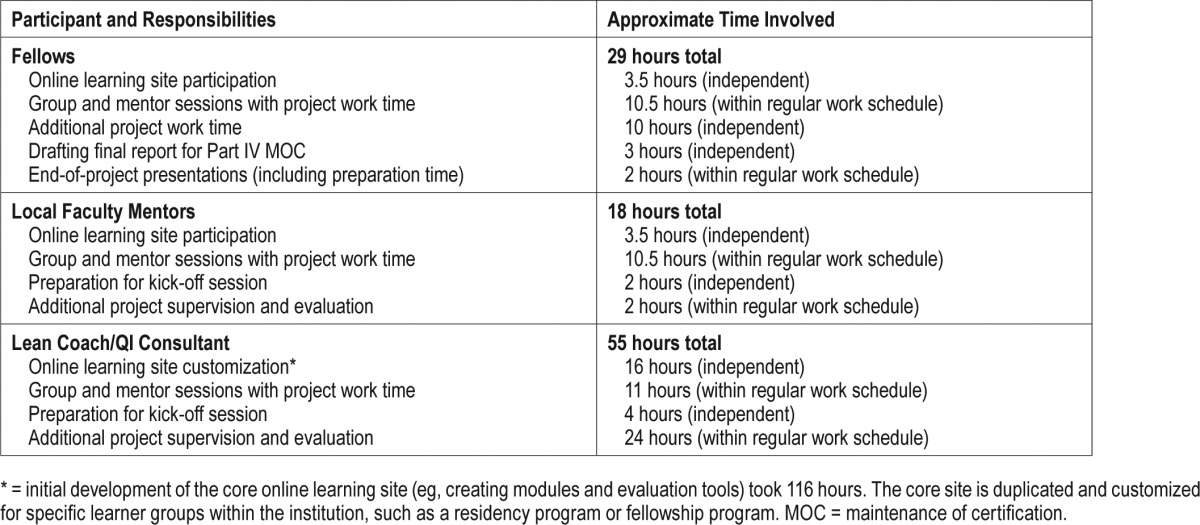
The QI consultant spent time customizing the institutional QI teaching materials so that they related directly to the curriculum designed for our sleep medicine fellowship. This process included creation of the online learning site used as part of the flipped classroom teaching method. The customization of didactic materials took the largest amount of time and represents an initial “up-front” time commitment; now that these customized materials are completed this preparation-related time will decrease drastically for future years. The QI consultant also spent time preparing for each group session and assisting program faculty with project supervision and evaluation.
The QI consultant and program faculty agreed to a 3-year approach, with the QI consultant largely developing and leading the first year, leadership shared with program faculty in the second year, and the majority of leadership transferred to program faculty in the third year and thereafter. Over this 3-year period, the QI consultant will “train the trainer” and will regularly meet with the program faculty to cultivate the trainer's expertise in structured problem solving and in teaching QI skills to other health professionals.
Individual Knowledge and Confidence
Each fellow took a postcurriculum knowledge test as a self-assessment about knowledge of foundational QI concepts. On a scale ranging from 1 to 10, with 1 equals “none” and 10 equals “very high,” fellows' retrospective self-assessment of knowledge about 11 QI concepts increased from a mean of 3.5 before training to 6.2 after training (P < .001). Fellows also took a postcurriculum self-assessment of confidence applying QI concepts to clinical care. On the same 1 to 10 scale noted previously, the fellows' retrospective self-assessment of confidence in applying 11 QI concepts increased from a mean of 3.7 before training to 6.1 after training (P < .001).
Outcomes of QI Projects
One project increased sleep study requests called directly to the fellow from 17% (n = 18) at baseline, to 59% (n = 22) postintervention, to 84% (n = 25) postadjustment (increase of 67 percentage points, P < .0001), which improved time-liness of care. The other project increased ability of sleep technologists to correctly identify electrocardiographic priorities, with calls to the on-call fellow who correctly identified electrocardiographic priority studies increasing from 70% (n = 10) at baseline, to 75% (n = 8) postintervention, to 88% (n = 8) postadjustment (small n not powered to detect increase of 18 percentage points at P < .05), which improved quality of care.
Project Presentations
Each fellow team presented its completed QI projects to sleep medicine faculty, fellows, and staff. Presentations included: reason for action, review of the current state, how a given project was selected, step-by-step explanations of their data collection, root cause analyses, countermeasure selection and implementation, results, and further recommendations.
Curriculum
On a postcurriculum survey, fellows and faculty mentors reported a positive QI curricular experience and gave suggestions for ongoing curricular refinements.
ACGME
Individual fellows' experience and the overall QI curriculum met ACGME expectations.
ABMS MOC
As fellows' QI projects met ABMS MOC Program requirements, fellows and faculty mentors received ABMS Part IV MOC credit. Each team submitted a written report of the step-by-step activities of 2 cycles of improvement and results. The reports are available at www.med.umich.edu/moc-qi/approved.htm for the fellow QI projects entitled, “Timely and Accurate Interpretation of EKGs on Polysomnograms” and “Improving Inpatient Portable Sleep Study Requests.”
DISCUSSION
The ACGME's Clinical Learning Environment Review Program21 emphasizes incorporation of coordinated QI and patient safety processes within individual programs and throughout the institution.22 The combination of QI need, interested faculty, institutional curricula that could be customized to fit our program, and opportunity to fulfill ACGME and ABMS requirements encouraged us to develop a QI curriculum in which sleep medicine fellows could use their daily clinical work to develop meaningful QI projects.
Ensuring that fellows have significant participation in QI activities can be difficult in a 1-year program. This study describes successful implementation of a QI curriculum into a single-year sleep medicine fellowship, and adds to the existing literature on incorporation of QI training into residency programs and multi-year fellowship programs.
A major challenge was scheduling the group sessions so that the QI consultant, fellows, and faculty mentors could attend without disruption of clinical responsibilities or other program didactics. Time constraints were addressed in part by (1) drawing on existing QI institutional materials and (2) using the described flipped-classroom format with online modules for delivery of didactic content. Performing the second PDCA cycle of improvement required less curricular time because learning the didactic material and how to perform the steps for the project had occurred during the first PDCA cycle.
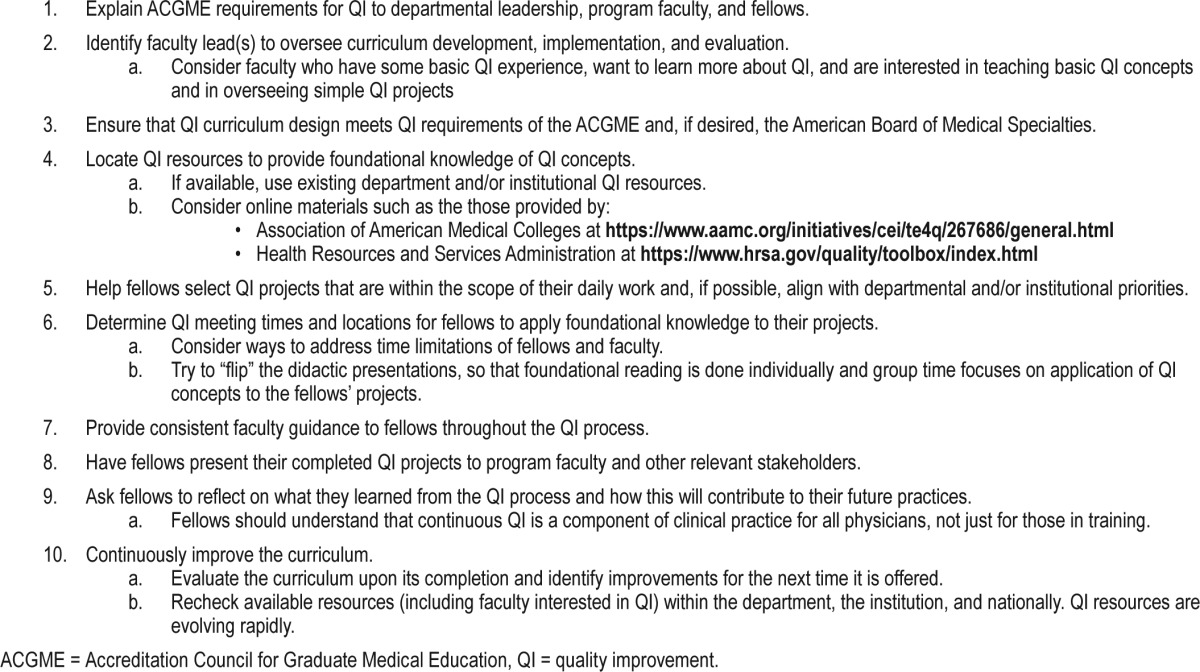
Table 3 lists tips other fellowship programs can use to guide implementation of a QI curriculum. Programs who want to build a similar QI curriculum may not currently have local faculty QI expertise. In this case, possible options include (1) collaboration with other programs that have faculty QI expertise; (2) if available, utilization of institutional QI resources to initiate and maintain a QI curriculum; and/or (3) use of publicly available online QI courses (Table 3) to provide the didactic content for a QI curriculum. The broader national interest in advancing QI within health care may give a fellowship program access to a greater number of QI resources and faculty with basic QI expertise. Also, an expanding number of institutions approved by the ABMS MOC Portfolio Program to approve local QI efforts may also translate into more support for an individual training program to implement a QI program.
Table 3.
Tips to implement a quality improvement curriculum commitment in a sleep medicine fellowship program.
The QI curriculum we described will always need to be examined for ongoing improvement. As the QI curriculum leadership transitions from the QI consultant to program faculty, the latter will need to stay current with QI concepts to lead and enhance the QI curriculum. Ongoing faculty development can be expanded to teach faculty members how to supervise fellow QI projects as a way participate in education and fulfill MOC requirements.16 The multidisciplinary nature of sleep medicine readily provides opportunities to collaborate with other training programs and enhance fellows' abilities to incorporate continuous QI into their clinical responsibilities.
CONCLUSIONS
The described sleep medicine fellowship QI curriculum integrated the fellows' education into a larger framework of improved patient care within our sleep disorders center and our institution. This experience equips fellows with skills they can incorporate into clinical practice upon graduation from fellowship. For other programs that are developing a QI curriculum, we recommend spending initial time and effort to build relationships with institutional QI units to identify resources and develop and implement a QI curriculum for fellows that links to an institutional network of QI education for all physicians, reflects how fellows will perform QI in independent practice, and prepares fellows to meet MOC requirements in independent practice.
DISCLOSURE STATEMENT
The authors report no conflicts of interest. This was not an industry-supported study.
ACKNOWLEDGMENTS
The authors wish to thank the additional faculty mentor, Helena Schotland, MD, and the sleep medicine fellows who participated in this QI training program, Hala Karnib, MD, Riaz Muhammad, MBBS, Gaurav Nigam, MBBS, Syed Qamer, MD, Wisam Sakbani, MD, Dafer Samara, MBBS, Kathryn Williams, MB BCh, along with Patricia Mullan, PhD for general advice and review of the manuscript.
ABBREVIATIONS
- ABMS
American Board of Medical Specialty
- ACGME
Accreditation Council for Graduate Medical Education
- EKG
electrocardiogram
- MOC
maintenance of certification
- PDCA
“Plan / Do / Check / Act”
- PI
performance improvement
- QI
quality improvement
REFERENCES
- 1.One-Year Common Program Requirements. Accreditation Council for Graduate Medical Education website. [Accessed July 5, 2017]. http://www.acgme.org/What-We-Do/Accreditation/Common-Program-Requirements.
- 2.Bornstein T. Quality improvement and performance improvement: different means to the same end? QA Brief. 2001;9(1):6–12. [Google Scholar]
- 3.HRSA Clinical Quality & Performance Measures Supplemental Technical Assistance. Health Resources and Services Administration website. [Accessed July 7, 2017]. https://www.hrsa.gov/quality/toolbox/index.html.
- 4.Arbuckle MR, Weinberg M, Cabaniss DL, et al. Training psychiatry residents in quality improvement: an integrated, year-long curriculum. Acad Psychiatry. 2013;37(1):42–45. doi: 10.1176/appi.ap.11120214. [DOI] [PubMed] [Google Scholar]
- 5.Buchmann RF, Deloney LA, Donepudi SK, Mitchell CM, Klein SG. Development and implementation of a systems-based practice project requirement for radiology residents. Acad Radiol. 2008;15(8):1040–1045. doi: 10.1016/j.acra.2008.02.016. [DOI] [PubMed] [Google Scholar]
- 6.Buckley JD, Joyce B, Garcia AJ, Jordan J, Scher E. Linking residency training effectiveness to clinical outcomes: a quality improvement approach. Jt Comm J Qual Patient Saf. 2010;36(5):203–208. doi: 10.1016/s1553-7250(10)36033-8. [DOI] [PubMed] [Google Scholar]
- 7.Benzer JK, Bauer MS, Charns MP, Topor DR, Dickey CC. Resident/faculty collaboration for systems-based quality improvement. Acad Psychiatry. 2013;37(6):433–435. doi: 10.1007/BF03340088. [DOI] [PubMed] [Google Scholar]
- 8.Axon RN, Penney FT, Kyle TR, et al. A hospital discharge summary quality improvement program featuring individual and team-based feedback and academic detailing. Am J Med Sci. 2014;347(6):472–477. doi: 10.1097/MAJ.0000000000000171. [DOI] [PubMed] [Google Scholar]
- 9.Callahan KE, Rogers MT, Lovato JF, Fernandez HM. A longitudinal, experiential quality improvement curriculum meeting ACGME competencies for geriatrics fellows: lessons learned. Gerontol Geriatr Educ. 2013;34(4):372–392. doi: 10.1080/02701960.2013.815179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carey WA, Colby CE. Educating fellows in practice-based learning and improvement and systems-based practice: the value of quality improvement in clinical practice. J Crit Care. 2013;28(1):112.e1–112.e5. doi: 10.1016/j.jcrc.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 11.Kashani KB, Ramar K, Farmer JC, et al. Quality improvement education incorporated as an integral part of critical care fellows training at the Mayo Clinic. Acad Med. 2014;89(10):1362–1365. doi: 10.1097/ACM.0000000000000398. [DOI] [PubMed] [Google Scholar]
- 12.Womack JP, Jones DT. Lean Thinking: Banish Waste and Create Wealth in Your Corporation. 1st ed. New York, NY: Free Press; 2003. [Google Scholar]
- 13.Liker JK. The Toyota Way: 14 Management Principles From the World's Greatest Manufacturer. New York, NY: McGraw-Hill; 2004. [Google Scholar]
- 14.Clark DM, Silvester K, Knowles S. Lean management systems: creating a culture of continuous quality improvement. J Clin Pathol. 2013;66(8):638–643. doi: 10.1136/jclinpath-2013-201553. [DOI] [PubMed] [Google Scholar]
- 15.Standards and Guidelines for Program Sponsorship. Portfolio Program of the American Board of Medical Specialties website. [Accessed August 24, 2017]. http://mocportfolioprogram.org/become-a-sponsor/sponsor-qualifications-approval-terms/. Updated December 2016.
- 16.Rosenbluth G, Tabas JA, Baron RB. What's in it for me? Maintenance of certification as an incentive for faculty supervision of resident quality improvement projects. Acad Med. 2016;91(1):56–59. doi: 10.1097/ACM.0000000000000797. [DOI] [PubMed] [Google Scholar]
- 17.Bonesso S, Gerli F, Pizzi C. The interplay between experiential and traditional learning for competency development. Front Psychol. 2015;6:1305. doi: 10.3389/fpsyg.2015.01305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Prober CG, Heath C. Lecture halls without lectures--a proposal for medical education. N Engl J Med. 2012;366(18):1657–1659. doi: 10.1056/NEJMp1202451. [DOI] [PubMed] [Google Scholar]
- 19.Bonnes SL, Ratelle JT, Halvorsen AJ, et al. Flipping the quality improvement classroom in residency education. Acad Med. 2017;92(1):101–107. doi: 10.1097/ACM.0000000000001412. [DOI] [PubMed] [Google Scholar]
- 20.Alessandrini E, Varadarajan K, Alpern ER, et al. Emergency department quality: an analysis of existing pediatric measures. Acad Emerg Med. 2011;18(5):519–526. doi: 10.1111/j.1553-2712.2011.01057.x. [DOI] [PubMed] [Google Scholar]
- 21.Weiss KB, Bagian JP, Wagner R, Nasca TJ. Introducing the CLER pathways to excellence: a new way of viewing clinical learning environments. J Grad Med Educ. 2014;6(3):608–609. doi: 10.4300/JGME-D-14-00347.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liao JM, Co JP, Kachalia A. Providing educational content and context for training the next generation of physicians in quality improvement. Acad Med. 2015;90(9):1241–1245. doi: 10.1097/ACM.0000000000000799. [DOI] [PubMed] [Google Scholar]