Abstract
Objectives
Our aims were to assess risks of early rebleeding after successful endoscopic hemostasis for Forrest oozing (FIB) peptic ulcer bleeding (PUB’s) compared to other stigmata of recent hemorrhage (SRH).
Design
These were post-hoc multivariable analyses of a large, international, double blind study (NCT00251979) of patients randomized to high dose intravenous (IV) esomeprazole (PPI) or placebo for 72 hours. Rebleeding rates of patients with PUB SRH treated with either PPI or placebo after successful endoscopic hemostasis were also compared.
Results
For patients treated with placebo for 72 hours after successful endoscopic hemostasis, rebleed rates by SRH were spurting arterial bleeding (FIA) 22.5%, adherent clot (FIIB) 17.7%, non-bleeding visible vessel (FIIA) 11.3%, and oozing bleeding (FIB) 4.9%. Compared to FIB patients, FIA, FIIB, and FIIA had significantly greater risks of rebleeding with odds ratios (95% CI’s) from 2.61 (1.05, 6.52) for FIIA to 6.70 (2.14, 20.26) for FIA. After hemostasis, PUB rebleeding rates for FIB patients at 72 hours were similar with esomeprazole (5.4%) and placebo (4.9%), whereas rebleed rates for all other major SRH (FIA, FIIA, FIIB) were lower for PPI than placebo, but the treatment by SRH interaction test was not statistically significant.
Conclusions
After successful endoscopic hemostasis, FIB patients had very low PUB rebleeding rates irrespective of PPI or placebo treatment. This implies that after successful endoscopic hemostasis the prognostic classification of FIB ulcers as a high risk SRH and the recommendation to treat these with high dose IV PPI’s should be re-evaluated.
INTRODUCTION
Some investigators in endoscopic studies utilize the Forrest (F) classification for risk stratification and others use descriptive terms for stigmata of recent hemorrhage (SRH) for peptic ulcer bleeding – PUB’s (1,2). The former group describes FIA (spurting or pulsatile arterial bleeding), FIB (oozing), and FIIA (non-bleeding visible vessel-NBVV) as “major SRH”, based upon reported risks of peptic ulcer rebleeding (1–4). The fact that PUB’s with both spurting bleeding and oozing are included in the first major Forrest group (I) implies that this group was perceived as having a higher risk of rebleeding than the second Forrest group (II) including FIIA or FIIB patients, and this should be used as the primary means of stratifying PUB’s for their rebleed risk (2). Others also include adherent clot (FIIB) as a major stigmata (1, 3–5).
Some PUB investigators include both FIA and FIB bleeding together as “active bleeding.” They plan studies, estimate sample sizes, and report outcomes based upon an assumption of similarity of FIA and FIB rather than a significant difference in rebleeding rates with medical and endoscopic treatments. However, FIB has been reported by some investigators to have a lower risk for PUB rebleeding than FIA (6–7).
A recent prospective cohort study with endoscopic Doppler endoscopic probe reported significantly higher rates in detection of arterial blood flow underlying FIA than FIB PUB’s, significantly higher post hemostasis rates of residual blood flow, and also significantly higher rebleed rates for PUB patients with FIA than FIB after current standard of care endoscopic hemostasis (8). Past endoscopic randomized controlled trials (RCT’s) of bleeding PUB’s also previously found a lower rebleeding risk for FIB than FIA (6, 7, 9).
In some RCT’s of medical compared to endoscopic hemostasis of PUB, FIB PUB’s not associated with a visible vessel or clot were considered to be a low risk SRH for re-bleeding. These studies therefore excluded FIB PUB patients (10 – 11). However, in other more recent RCT’s studies or a meta-analysis (12–14), a cost-effectiveness analysis (15), a consensus report (3), and a review on ulcer hemorrhage (5), PUB’s with FIB and FIA were lumped together as “active bleeding” and considered to be one high risk stigmata.
Based upon these data and classifications of SRH, there is a controversy and different interpretations about the actual rebleed risks of FIB vs. FIA PUB’s and whether these should be considered as similar or different for risk stratification, sample size determination, or clinical treatment (medically and endoscopically).
The purposes of this study were 1) to assess the risk factors and rates of early rebleeding for FIB (oozing) PUB’s compared to other SRH after successful endoscopic hemostasis in a large international RCT (in the placebo treatment group), and 2) to determine the medical treatment effect on PUB rebleeding after successful endoscopic therapy of high dose PPI vs. placebo, stratified by SRH.
METHODS
Study population
The dataset for this study was from a large, double blind, randomized, controlled, international clinical trial (NCT00251979), which was previously reported (16). In brief, that study included PUB rebleeding rates after successful endoscopic hemostasis of patients with PUB stigmata (FIA, FIB, FIIA, and FIIB) who were treated with high dose intravenous (IV) infusion of esomeprazole or placebo for 72 hours in blinded fashion and compared. Initial endoscopic hemostasis was with either monotherapies (injection of epinephrine, thermal coagulation, or hemoclipping) or combination therapies (epinephrine injection and thermal coagulation or hemoclipping) and was deemed successful before randomization onto this study. Post IV infusion of PPI vs placebo of 72 hours, all patients were treated with open label esomeprazole 40mg per day from day 4 to day 30 in this study. PUB study patients were stratified by Forrest classification at baseline, including those with FIA, FIB, FIIA, and FIIB, which were all considered to be high risk for recurrent bleeding. Patients with oozing bleeding (FIB) lacked a visible vessel (FIIA) or adherent clot (FIIB). Patients with FIIC (flat spots) or FIII (clean ulcer base) were excluded. One patient in the placebo group (total 389) was missing the Forrest classification and therefore was not included in this analysis (total 388 patients).
Outcomes of rebleeding with placebo and IV PPI
Clinically significant rebleeding episodes were defined as recurrent hematemesis or melena, with a minimum decrease of 2 gram of hemoglobin, and/or the need for transfusions of red blood cells, as detailed in the previous report (16).
To exclude the potential influence of IV proton pump inhibitor (PPI) in this analysis and to evaluate the natural history after successful hemostasis, early PUB rebleeding rates up to 72 hours in the placebo group were compared according to baseline SRH.
As another analysis for this report, the rates of PUB rebleeding up to 72 hours on placebo vs. esomeprazole were also compared for patients according to their baseline SRH. This was to assess the potential benefit of profound acid suppression after successful endoscopic hemostasis of FIB PUB’s versus other major SRH (FIA, FIIA and FIIB). We also assessed for potential interactions of SRH with type of treatment (PPI vs. placebo).
Hypothesis
Our hypotheses were that the rebleed rate of patients treated with placebo (no PPI) after successful endoscopic hemostasis of FIB PUB’s would be significantly lower than other major SRH (FIA, FIIA, FIIB) and that FIB patients would not benefit clinically from high dose IV PPI’s.
Primary and secondary analyses
Both univariable and multivariable analyses were performed to determine independent risk factors for early rebleeding on IV placebo. We stratified by FIB vs other major SRH (FIA, FIIA, and FIIB) and analyzed both background characteristics and potential risk factors for rebleeding. The statistical testing performed was Fisher’s exact test (with Bailey’s method) for univariate analyses (Table 1) and logistic regression for multivariable analyses (Table 2). For the multivariable analysis, variables with p < 0.10 from the univariable analysis were included. Fisher’s exact test was used for comparisons of treatment effects in Table 3. A two-sided P value < 0.05 was considered to be a statistically significant difference. The analyses were done using NMSP, a software package validated against SAS proc LOGISTIC (Personal Communications Tore Persson, PhD).
Table 1.
Univariable Statistics Comparing Background Characteristics for Oozing vs. All Other Major SRH Combined for Placebo Treated Patients (N = 388)
| Characteristic | Oozing (Ib) (N=163) |
Other classes (Ia+IIa+IIb) (N=225) |
P-value* |
|---|---|---|---|
| Age > 65 years | 68 (41.7%) | 110 (48.9%) | 0.10 |
| Male gender | 112 (68.7%) | 155 (68.9%) | 0.97 |
| Previous ulcer complications | 27 (16.6%) | 14 (6.2%) | 0.001 |
| Ulcer size > 2 cm | 12 (7.4%) | 28 (12.4%) | 0.13 |
| H. pylori negative | 59 (36.2%) | 78 (34.7%) | 0.76 |
| NSAID’s | 63 (38.7%) | 93 (41.3%) | 0.60 |
| Epinephrine injection only | 70 (42.9%) | 71 (31.6%) | 0.022 |
| Shock | 5 (3.1%) | 14 (6.2%) | 0.23 |
By Fisher’s exact test with Bailey’s method.
Table 2.
PUB Rebleeding risk by SRH up to 72 hours in Placebo Patients (N=388) – Multivariable Analysis
| Estimated Odds Ratio* | Lower 95% CI** | Upper 95% CI | |
|---|---|---|---|
| Spurting vs. Oozing (Forrest IA, N=40 vs. IB, N=163) | 6.66 | 2.19 | 20.26 |
| Clot vs. Oozing (Forrest IIB, N=34 vs. IB, N=163) | 4.11 | 1.27 | 13.25 |
| NBVV vs. Oozing (Forrest IIA, N=151 vs. IB, N=163) | 2.61 | 1.05 | 6.52 |
The oozing bleeding group was used as the reference and all placebo patients were included according to the baseline SRH in ulcers.
CI is confidence intervals.
Table 3.
PUB Rebleeding Rates up to 72 hours by Stigmata and Treatment
| Stigmata | PPI | Placebo | Odds ratio | 95% CI for the odds ratio | NNT |
|---|---|---|---|---|---|
| Spurting (FIA) | 3/28 (10.7%) | 9/40 (22.5%) | 0.41 | 0.10 – 1.69 | 9 |
| Clot (FIIB) | 2/42 (4.8%) | 6/34 (17.6%) | 0.23 | 0.044 – 1.24 | 8 |
| Visible Vessel (FIIA) | 8/136 (5.9%) | 17/151 (11.3%) | 0.49 | 0.21 – 1.18 | 19 |
| Oozing (FIB) | 9/166 (5.4%) | 8/163 (4.9%) | 1.11 | 0.42 – 2.95 | N/A |
| *Overall Treatment Effect | 22/372 (5.9%) | 40/388 (10.3%) | 0.55 | 0.32 – 0.94 | 23 |
| **FIA, FIIA and FIIB combined | 13/206 (6.3%) | 32/225 (14.2%) | 0.41 | 0.21 – 0.80 | 13 |
NNT is the number needed to treat.
Overall Treatment Effect is for all SRH including FIA, FIB, FIIA, and FIIB.
FIB (oozing) PUB’s were excluded and other major SRH were included.
RESULTS
Rebleeding in the placebo group according to endoscopic stigmata
For cumulative PUB rebleeding rates up to 72 hours in the placebo treated group (N=388) according to baseline SRH, refer to figure 1. These are shown in decreasing order from highest to lowest rebleeding rates.
Figure 1.
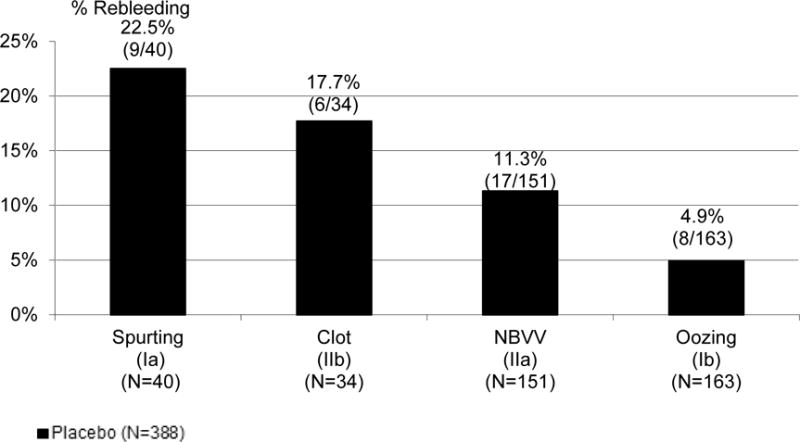
PUB Rebleeding Rates After Endoscopic Hemostasis, at 72 hrs in Placebo Treated Patients
For a comparison of baseline demographic characteristics for FIB as the reference vs. other major SRH (FIA, FIIA, FIIB), refer to Table 1. The two significant differences at baseline on this univariable analysis were a higher rate of epinephrine injection alone for hemostasis and a higher rate of previous ulcer complications. Paradoxically these differences might have been expected to increase rebleed risk of FIB patients, but that was not seen (Figure 1). The multivariable analysis with oozing as the reference SRH for early rebleeding are shown in table 2 with the estimated odds ratios and confidence intervals. These are in descending order of odds ratios. All major SRH (FIA, FIIA, FIIB) had significantly higher risks of rebleeding than FIB with odds ratios (and 95% confidence intervals) increasing from 2.61 (1.05; 6.52) for FIIA (NBVV) to a high of 6.66 (2.19;20.26) for FIA (spurting).
Rebleeding in the placebo vs. the high-dose esomeprazole groups
The comparisons of early PUB rebleeding rates within 72 hours according to different SRH and medical treatments (placebo vs. esomeprazole) are shown in Table 3. As previously reported for the RCT, there was a significantly lower rebleeding rate for all PUB patients treated with esomeprazole than placebo by 45% (16). In the current analysis, all SRH groups except oozing (FIB) had a lower rate of PUB rebleeding with PPI than placebo. For the large FIB group of 329 patients (or 43% of all study patients), the rebleeding rates at 72 hours were 5.4 % (9/166) for esomeprazole and 4.9% (8/163) for placebo treatment groups (Odds ratio 1.11, 95% CI – 0.42 – 2.95).
In contrast, high dose PPI reduced rebleeding rates at 72 hours by 5.4% (FIIA) to 12.9% (FIIB) in comparison to placebo in each of the other major stigmata subgroups (FIA, FIIA, and FIIB) with the greatest reduction in clot (FIIB) PUB’s. The NNT’s were 8 for clot, 9 for spurting, and 19 for non-bleeding visible vessel. See Table 3.
In the original RCT of 760 patients (16), the overall treatment effect of PPI vs. placebo for 72 hours had an odds ratio of 0.55 (CI – 0.32 – 0.94). However, the effects of PPI on rebleeding were diluted by including the oozing patients, who had no apparent benefit from PPI infusion. See Table 3. If only the high risk patients with major SRH (FIA, FIIA, FIIB) were included (431 patients), the treatment effect of PPI would have been greater with odds ratio of 0.41 (CI – 0.21 – 0.80). Similarly, the NNT would have been lower than it was with the large oozing group included –13 vs. 23 – table 3. The implication of this reassessment is that for a study of high risk patients that excluded FIB (oozing) patients, there could have been a reduction in enrollment by more than 40%, with a resultant increase in overall treatment effect with odds ratio reduction from 0.55 to 0.41 and a reduction in the overall number needed to treat from 23 to 13.
From the logistic regression model assessing treatment and stigmata effect, the overall treatment effect was significant (p = 0.0237) as was the stigmata effect (p = 0.0415). However, the interaction between PPI treatment and individual stigmata was not significant (p = 0.3632) in this analysis. The PPI interaction with oozing compared to the other major SRH combined (FIA, FIIA, FIIB) was also evaluated and the p value was lower but not significant – p = 0.097. The difference between the two p values was mainly due to the small size of the FIA and FIIB groups which makes the estimates of interaction uncertain there.
DISCUSSION
PUB patients with oozing bleeding (FIB) treated with IV placebo after successful endoscopic hemostasis had a significantly reduced risk of rebleeding compared to other major SRH (FIA, FIIA, FIIB). When FIB as the reference group was compared to each of the other major SRH (FIA, FIIA, and FIIB) in a multivariable analysis of placebo treated patients, all other major SRH had a significantly higher risk of rebleeding. The odd ratios varied from 2.62 (NBVV – FIIA), to 4.12 (clot – FIIB), to 6.7 (spurt – FIA) – table 2.
After successful endoscopic hemostasis in this study, patients with baseline major stigmata (FIA, FIIA, FIIB) had lower rebleeding rates with high dose IV PPI’s for 72 hours than placebo treated patients. In contrast, FIB (oozing) PUB patients on either IV placebo or high dose PPI infusion displayed very low rebleeding rates. These differences between post-hemostasis rebleeding rates with IV PPI or placebo indicate a clinically relevant reduction in rebleeding rates of 5.4 to 12.9% for each major stigmata except FIB. The original RCT was under powered to analyze treatment effect for individual SRH. However, the rebleeding rate for FIB after endoscopic hemostasis and placebo treatment was very low (4.9%), similar to FIB patients treated with PPI (5.4%). Since the rebleeding rates of FIB after endoscopic hemostasis were so low, it was unlikely that PPI could provide any additional clinical benefit.
The possible pathophysiologic reason why FIB PUB’s might be less likely to rebleed after successful endoscopic hemostasis than other Forrest PUB’s (FIA, FIIA, and FIIB) probably relates to smaller underlying arteries in FIB ulcers. The invisible arteries and their blood flow under SRH can now be detected by Doppler endoscopic probe (8, 17). Recent endoscopic Doppler probe studies of patients with FIB PUB’s vs. other major SRH have reported significantly lower detection rates of underlying arterial flow than FIA, both before and after endoscopic treatment (8). Specifically, the detection rate of arterial flow underlying for FIB PUB’s before any endoscopic treatment was significantly lower at 47% compared to FIA PUB’s which were 100% Doppler probe positive. Furthermore, after standard visually guided multipolar electrocoagulation (MPEC) or hemoclipping for ulcer hemostasis of these SRH, residual blood flow was detected by Doppler probe in 0 % for FIB PUB’s, but was still present in 35% of FIA PUB’s. Most clinically relevant to explaining the current study results was that the rebleeding rate in this prospective study was significantly lower for FIB than FIA (0% vs 28.6%), in spite of the different PPI therapy which was high dose IV PPI infusion for FIA patients vs. oral PPI for FIB patients after successful visually guided hemostasis (8).
Other confirmatory evidence that oozing (FIB) bleeding (not associated with a visible vessel or adherent clot) has a lower risk of rebleeding and emergency surgery than spurting (FIA) comes from past randomized controlled trials (RCT’s) (6, 7). The first was a RCT of epinephrine injection vs. medical treatment alone of PUB patients with active bleeding, stratified as FIA and FIB (6). All patients with rebleeding had emergency surgery instead of repeat endoscopic hemostasis. For the medical groups (not treated endoscopically), rebleeding rates and surgical intervention in FIA were clinically much higher than the FIB patients −70% vs. 29% respectively. A subsequent RCT by the same investigators compared epinephrine injection alone vs. combination epinephrine injection and heater probe coagulation for ulcer hemostasis of patients stratified for by FIA or FIB PUB’s (7). There were significantly higher rebleeding (22.2% vs. 6.5%) and emergency surgery rates (29.6% vs. 6.5%) in the FIA spurting arterial bleeding PUB patients treated with epinephrine alone vs. combination therapy. However, no significant differences were seen between treatments for the much larger PUB group with FIB in whom rebleeding (6.5% vs. 2.9%) and emergency surgery rates (6.5% vs. 5.7%) were very low for the epinephrine group vs. the combination hemostasis group (7). Current guidelines now recommend that epinephrine not be used alone for hemostasis of PUB’s with SRH (3,4).
These cohort study and RCT results implied to the investigators that smaller blood vessels underlay oozing PUB’s compared to other major SRH with spurting arterial bleeding or visible vessels (6–8). Also, FIB PUB’s were more easily and effectively treated with endoscopic hemostasis and had lower rebleeding rates either with medical treatment or endoscopic hemostasis than PUB’s with other major (FIA, FIIA, FIIB) SRH (6–8,9).
When PUB’s are encountered by the endoscopist that have both oozing bleeding and either a visible vessel or adherent clot, there may be differences of how these are classified and treated, particularly if the Forrest classification is used (1, 8). There is recent evidence that such patients with both oozing and another major SRH (such as a clot or visible vessel) would have a higher risk of rebleeding, similar to those patients with visible vessel or clot without oozing (18). In such cases, our recommendation is to classify them not as FIB but rather as visible vessel (FIIA) or adherent clot (IIB) and manage them accordingly.
These results are very relevant to the clinical management of patients with PUB’s. Since a large proportion of PUB patients often exhibit oozing ulcer bleeding compared to other high risk SRH, placing FIB patients on oral PPI’s after successful endoscopic hemostasis, and eliminating the 72 hours of high dose intravenous PPI treatment has the potential of reducing health care expenditures without increasing PUB rebleeding rates. In our previously reported study, the FIB PUB’s were the largest subgroup, comprising 43% of all patients randomized (16). As further evidence from another recent study, oral PPI’s instead of high dose IV PPI’s were utilized after successful visually guided endoscopic hemostasis in patients with FIB (oozing) PUB’s and 0% (0/15) had rebleeding (8).
Our results also have implications for understanding risk, planning and reporting of future PUB clinical trials, or assessing conclusions of recent meta-analyses (8). Making the assumption that FIA and FIB are both high risk SRH with high rebleeding rates if treated medically and/or endoscopically could lead to an overestimation in the risk of PUB rebleeding when performing sample size calculations with the consequent risk of under powering the study. Indeed, larger differences in rebleed rates would be assumed and lower sample size estimates than actually required to show significant differences would be planned. However, inclusion of a large proportion of PUB’s with FIB (oozing) could also significantly increase the size and expense of an RCT while reducing the treatment effect of PPI, as presented in the current results section which analyzed our own previously reported RCT (16). Also, grouping PUB FIA and IB together as “active bleeding” could cause potential flaws in study design and could invalidate the interpretation of PUB rebleeding and other outcomes for these SRH.
Our study has some potential limitations in that it is a post-hoc analysis and the numbers of patients with FIA and IIB ulcers were considerably lower than in the other two ulcer subgroups (FIB and FIIA). Additionally, despite the inclusion of training of investigators before the study and quality control measures during the study (19), there may have been some variations in ulcer classification due to the large size of the study and its multicenter design (16). However, when considered in the light of other published data, our results provide an important, consistent, and compelling message about oozing PUB bleeding (6,7,8,9,17,18).
The conclusions from our study are that after successful endoscopic hemostasis:
In a multivariable analysis for early rebleeding on placebo treatment, patients with other major SRH (FIA, FIIA, FIIB) had a significantly higher rebleeding risk than FIB (oozing) PUB patients.
The rate of rebleeding in FIB patients was very low and was not influenced positively by high dose IV PPI treatment.
Based upon the very low early rebleeding rates of PUB patients, FIB oozing bleeding should be separated from FIA (spurting bleeding) patients and not considered as a similar high risk SRH and thus may not require subsequent medical treatment with high dose IV PPI’s after successful endoscopic hemostasis.
What is already known about the subject
After successful endoscopic hemostasis, high dose IV PPI’s reduce PUB rebleeding rates in high risk patients and are recommended in current GI treatment guidelines.
Current guidelines also recommend endoscopic hemostasis and post hemostasis high dose PPI therapy for both Forrest IA (spurting) and IB (oozing) PUB’s.
However, past endoscopic randomized controlled trials (RCT’s) and recent Doppler probe studies of bleeding PUB’s report a significantly higher rebleeding risk for Forrest IA than Forrest IB PUB’s.
What are the new findings
The risk of rebleeding of placebo treated patients was significantly lower for Forrest IB PUB’s when compared to other high risk major stigmata (FIA, FIIA, FIIB) in a multivariable analysis.
PPI therapy did not reduce the rate of rebleeding among patients with Forrest IB PUB’s after successful endoscopic hemostasis.
How might it impact on clinical practice in the foreseeable future?
Based upon very low rates of rebleeding following successful endoscopic therapy and lack of additional benefits for PPI’s, persons with Forrest IB PUB’s may not require high dose intravenous PPI therapy.
Acknowledgments
The analysis and RCT were supported by AstraZeneca. Dr. Jensen is supported by a VA Clinical Merit Review grant (CLIN-013-07F) and NIH-NIDDK CURE: DDRC grant DK 41301 (Human Studies Core). The authors thank Jeffrey Gornbein DrPH (Biomathematics Dept. UCLA, Los Angeles) for assistance with additional biostatistical analyses.
References
- 1.Savides TS, Jensen DM. GI Bleeding. In: Feldman M, Friedman LS, Brandt LJ, Sleisenger and Fordtran’s, editors. Gastrointestinal and Liver Disease. Pathophysiology/Diagnosis/Management. Tenth. Elsevier Saunders Philadelphia; 2015. pp. 297–335. [Google Scholar]
- 2.Forrest JAH, Finlayson NDC, Shearman DJC. Endoscopy of upper gastrointestinal bleeding. Lancet. 1974;ii:394–7. doi: 10.1016/s0140-6736(74)91770-x. [DOI] [PubMed] [Google Scholar]
- 3.Barkun A, Bardou M, Kuipers EJ, et al. International Consensus: Recommendations on the management of patients with non-variceal gastrointestinal bleeding. Ann Intern Med. 2010;152:101–13. doi: 10.7326/0003-4819-152-2-201001190-00009. 39:843–57. [DOI] [PubMed] [Google Scholar]
- 4.Laine L, Jensen DM. Management of patients with ulcer bleeding. Am J Gastroenterol. 2012;107:345–360. doi: 10.1038/ajg.2011.480. [DOI] [PubMed] [Google Scholar]
- 5.Gralnek IM, Barkun AN, Bardou M. Management of acute bleeding from a peptic ulcer. N Engl J Med. 2008;359:928–37. doi: 10.1056/NEJMra0706113. [DOI] [PubMed] [Google Scholar]
- 6.Chung SCS, Leung JWC, Steele RJC, et al. Endoscopic injection of adrenaline for actively bleeding ulcers: a randomized trial. Br Med J. 1988;296:1631–33. doi: 10.1136/bmj.296.6637.1631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chung SCS, Lau JY, Sung JJ, et al. Randomized comparison between adrenaline injection alone and adrenaline injection plus heat probe treatment for actively bleeding ulcers. BMJ. 1997;314:1307–11. doi: 10.1136/bmj.314.7090.1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jensen DM, Ohning GV, Kovacs TOG, Ghassemi KA, Jutabha R, Dulai GS, Machicado GA. Doppler Endoscopic Probe as a Guide to Risk Stratification and Definitive Hemostasis of Peptic Ulcer Bleeding. Gastrointest Endosc. 2016;83:129–36. doi: 10.1016/j.gie.2015.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Swain CP, Bown SG, Storey DW, et al. Controlled trial of argon laser photocoagulation in bleeding peptic ulcers. Lancet. 1981:1313–16. doi: 10.1016/s0140-6736(81)91340-4. [DOI] [PubMed] [Google Scholar]
- 10.Jensen DM. Heat probe for hemostasis of bleeding peptic ulcers: Techniques and results of randomized controlled trials. Gastrointest Endosc. 1990;36:S42–S49. Supplement to. [PubMed] [Google Scholar]
- 11.Gralnek I, Jensen DM, Kovacs TOG, Jutabha R, Jensen ME, Cheng S, Gornbein J, the CURE Hemostasis Research Group An economic analysis of patients with active ulcer hemorrhage treated with endoscopic heater probe, injection sclerosis, or surgery in a randomized trial. Gastrointest Endosc. 1997;46:105–112. doi: 10.1016/s0016-5107(97)70056-7. [DOI] [PubMed] [Google Scholar]
- 12.Sung JJ, Tsoi KK, Lai LH, Wu JC, Lau JY. Endoscopic clipping versus injection and thermo-coagulation in the treatment of non-variceal upper gastrointestinal bleeding: a meta-analysis. Gut. 2007;56:1364–73. doi: 10.1136/gut.2007.123976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cipoletta L, Bianco MA, Rotondado G, et al. Prospective comparison of argon plasma coagulator and heater probe in the endoscopic treatment of major peptic ulcer bleeding. Gastrointest Endosc. 1998;48:191–5. doi: 10.1016/s0016-5107(98)70163-4. [DOI] [PubMed] [Google Scholar]
- 14.Lin HJ, Tseng GY, Perng CL, Lee FY, Chang FY, Lee SD. Comparison of adrenaline injection and bipolar electrocoagulation for the arrest of peptic ulcer bleeding. Gut. 1999;44:715–19. doi: 10.1136/gut.44.5.715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barkun A, Herba K, Adam V, Kennedy W, Fallone CA, Bardou M. High-dose intravenous proton pump inhibition following endoscopic therapy in the acute management of patients with bleeding peptic ulcers in the USA and Canada: a cost-effectiveness analysis. Aliment Pharmacol Ther. 2004;19:591–600. doi: 10.1046/j.1365-2036.2004.01808.x. [DOI] [PubMed] [Google Scholar]
- 16.Sung JJ, Barkun A, Kuipers EJ, Mössner J, Jensen DM, Stuart R, Lau JY, Ahlbom H, Kilhamn J, Lind T, the Peptic Ulcer Bleed Study Group Intravenous esomeprazole for prevention of recurrent peptic ulcer bleeding: A randomized trial. Ann Intern Med. 2009;50:455–464. doi: 10.7326/0003-4819-150-7-200904070-00105. [DOI] [PubMed] [Google Scholar]
- 17.Wong RC. Endosopic Doppler US probe for acute peptic ulcer hemorrhage. Gastrointest Endosc. 2004;60:804–12. doi: 10.1016/s0016-5107(04)02046-2. [DOI] [PubMed] [Google Scholar]
- 18.Jensen DM, Stuart R, Ahlbom H, Eklund S. Inter-observer agreement on assessment of photodocumentation in bleeding peptic ulcer. Gastrointest Endosc. 2009;69:AB 186 (S1491). [Google Scholar]
- 19.Sung JJY, Mossner J, Barkun A, Kuipers EJ, Lau J, Jensen D, Stuart R, Junghard O, Olsson G, on behalf of the PUB Study Group Intravenous esomeprazole for prevention of peptic ulcer re-bleeding: Rationale/design of the peptic ulcer bleed study. Aliment Pharmacol Ther. 2008;27:666–77. doi: 10.1111/j.1365-2036.2008.03631.x. [DOI] [PubMed] [Google Scholar]


